Abstract
Background
Risk factors associated with preeclampsia in HIV-infected women remain largely unknown. Systemic angiogenic imbalance contributes to preeclampsia in HIV-uninfected women, but changes in angiogenic markers after HAART initiation have not been studied.
Methods
The Mma Bana study randomized 560 HIV-infected, HAART-naive pregnant women with CD4 counts ≥ 200 cells/mm3 between 26–34 weeks gestation to lopinavir/ritonavir/zidovudine/lamivudine or abacavir/zidovudine/lamivudine. Another 170 participants with CD4 counts < 200 cells/mm3 initiated nevirapine/zidovudine/lamivudine between 18–34 weeks gestation. Characteristics of 11 women who developed preeclampsia were compared with the remaining722 Mma Bana participants who delivered, using logistic regression. Plasma samples drawn at HAART initiation and one month later from 60 women without preeclampsia and at HAART initiation for all11 preeclamptic women were assayed for placental growth factor (PlGF) and soluble FMS toll-like tyrosine kinase-1 (sFlt-1),
Results
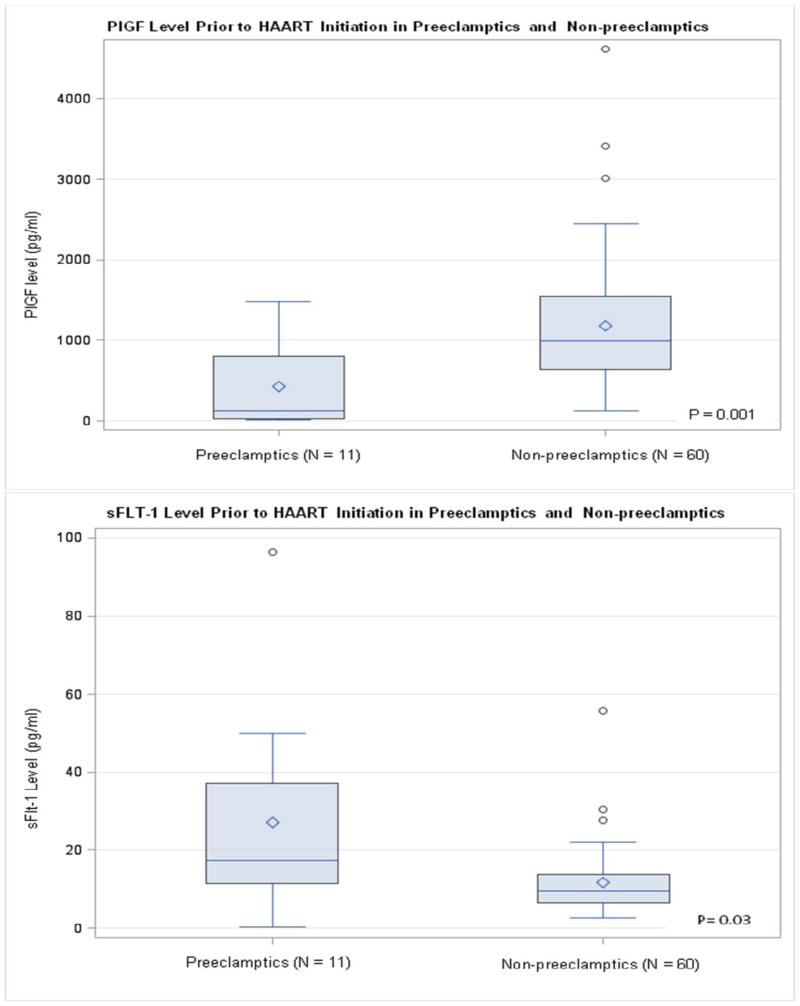
Pre-HAART viral load > 100,000 copies/ml was associated with preeclampsia (OR 5.8; 95% CI 1.8, 19.4; p = 0.004). Median pre-HAART PlGF level was lower and sFLT-1 was higher in women who developed preeclampsia versus those who did not (130 vs 992 pg/ml, p=0.001; 17.5 vs 9.4 pg/ml, p=0.03, respectively). In multivariate analysis, PlGF and viral load remained significantly associated with preeclampsia. No significant changes in angiogenic factors were noted after 1 month of HAART treatment among non-preeclamptic women.
Conclusions
Pre-HAART viral load > 100,000 copies/ml and PlGF predicted preeclampsia among women starting HAART in pregnancy. Among non-preeclamptic women, HAART treatment did not significantly alter levels of PlGF or sFlt-1 one month into treatment.
Keywords: HIV-1, viral load, pregnancy, preeclampsia, HAART
INTRODUCTION
Preeclampsia, classically characterized by the development of hypertension and proteinuria after 20 weeks gestation, affects approximately 3% of all pregnancies worldwide.1–3 Preeclampsia and its most severe forms result in increased morbidity and mortality among women and their infants, particularly in low and middle income countries.4–6 While the etiology of preeclampsia has yet to be fully elucidated, there is a body of research supporting an association between an autoimmune cascade and preeclampsia.7–10 More recent research has demonstrated that alterations in the concentrations of circulating angiogenic factors are associated with preeclampsia.11–18
Preeclampsia research among HIV-infected women has been limited. HIV-infected pregnant women in the era prior to use of Highly Active Antiretroviral Therapy (HAART) were found to be less likely to develop preeclampsia than HIV-uninfected women.19, 20 However, HIV-infected women receiving HAART appear to experience similar rates of preeclampsia as HIV-uninfected women,20–23 suggesting that HAART may restore risk of preeclampsia back to a pre-infection baseline.
Access to HAART in pregnancy in low and middle income countries is increasing. As HAART in pregnancy is being scaled up in developing countries, it is often done in the setting of limited access to obstetric care, including limited ability to recognize and safely manage preeclampsia. Therefore, it is of public health importance to understand any association between HAART use in pregnancy and risk of preeclampsia, as well as the mechanism underlying such an association.
Using a cohort of HIV-1 infected treatment naïve pregnant women in Botswana who initiated HAART in pregnancy, we sought to identify risk factors associated with preeclampsia. Using a smaller subset of our cohort, we explored levels of two angiogenic markers to determine if alterations in the concentration of the angiogenic markers mirrored the pattern observed in preeclamptic HIV-uninfected women. We also analyzed the change in levels of these angiogenic markers one month after HAART initiation among non-preeclamptic women.
METHODS
Study Population
The Mma Bana Study, which enrolled 730 HIV-1 infected HAART-naive pregnant women, has been described in detail previously.24 Five hundred sixty participants who had CD4+ cell counts ≥ 200 cells/mm3 and no AIDS defining illnesses at enrollment, between 26–34 weeks gestation, were randomized to receive either abacavir/zidovudine/ lamivudine co-formulated as Trizivir (GlaxoSmithKline) (TZV) twice daily or zidovudine/ lamivudine co-formulated as Combivir(CBV) (GlaxoSmithKline) with lopinavir/ritonavir co-formulated as Kaletra (Abbott) (CBV-KAL) twice daily. Another 170 women, who had a screening or previously documented CD4+ cell count of < 200 cells/mm3, were enrolled in an observational arm of the Mma Bana study between 18 weeks and 34 weeks gestation and monitored as they initiated Combivir and nevirapine (CBV-NVP), the HAART regimen specified in Botswana’s national HIV treatment guidelines. This study focuses on the 722 Mma Bana women who remained on study from enrollment through delivery.
A high rate of preeclampsia was identified while the Mma Bana study was ongoing and a sub-study was undertaken. We sought to evaluate changes in levels of placental growth factor (PlGF) and soluble FMS toll-like tyrosine kinase-1 (sFlt-1) one month after HAART initiation. Collection and storage of maternal plasma one month after HAART initiation was added in the latter half of the Mma Bana study. We obtained and stored maternal specimens until we had paired specimens (enrollment and one-month after HAAART initiation) from 60 sequentially enrolled women who had not yet delivered one month after HAART initiation, and did not experience preeclampsia (controls). These paired specimens were analyzed to determine changes in PlGF and sFlt-1 levels following a month of HAART treatment. We also compared PlGF and sFlt-1 levels from the enrollment specimens of the 60 controls with enrollment specimens from the 11 women who experienced preeclampsia, to ascertain whether HIV-infected women who later experienced preeclampsia had significantly lower levels of PlGF and higher levels of sFlt-1 prior to the onset of preeclampsia symptoms, a pattern observed among HIV-uninfected preeclamptic women. Preeclamptic women were enrolled in the Mma Bana study between 13-Sep-2006 through 10-Apr-2008, while controls (non-preeclamptics) were enrolled between 9-Jan-2008 and 12-May-2008.
Preeclampsia was defined as the presence of hypertension, as evidenced by either a systolic pressure greater than 140 mm/hg or a diastolic pressure greater than 90 mm/hg, on two occasions (separated by at least six hours), and 1+ or greater urine protein via urine dip stick as documented during a study site visit or by a non-study healthcare provider. Study participants were evaluated by a study nurse and physician at enrollment, 2 weeks post-enrollment and monthly thereafter until delivery, unless pregnancy gestational age exceeded 38 weeks and then participants were evaluated weekly until delivery. Blood pressure was measured and urine was checked for the presence of protein at every antenatal visit. Blood pressure was checked using either automated electronic equipment or manual sphygmomanometers. Any woman with a systolic and/or diastolic blood pressure meeting the definition of preeclampsia with 1+ proteinuria or greater was referred to the local hospital for definitive management of preeclampsia by the study physician.
Gestational age was calculated from an algorithm that relied upon maternal reported last menstrual period (LMP) and ultrasound performed prior to randomization. Where the estimated gestational age of a first trimester ultrasound differed by more than 1 week from the woman’s reported LMP, a second trimester ultrasound differed by more than 2 weeks, or a third trimester ultrasound differed by more than 3 weeks, ultrasound dating was employed. Otherwise the LMP was employed. Once the gestational age was ascertained utilizing this algorithm, it was not altered later in the pregnancy.
The Botswana Health Research Development Committee and the Harvard School of Public Health Human Subjects Committee approved the collection of blood and its utilization for research purposes in the Mma Bana study. Women who enrolled in the Mma Bana study provided written informed consent for their blood samples to be utilized and human subject research guidelines of Harvard School of Public Health were followed in the conduct of this clinical research.
Sample Collection and Preparation
Samples of maternal peripheral blood were obtained from HIV-infected women at enrollment and one month after HAART initiation in the parent Mma Bana study between 26 and 34 weeks gestation (for women in the randomized arms) or between 18 and 34 weeks gestation (for women in the observational arm). HAART was initiated at the enrollment visit and after the blood draw. The samples were processed and plasma was stored at −70°C, shipped frozen and kept below −60°C until time of the assay.
Measurement of sFlt-1 and PlGF
Assays were performed by personnel blinded to the outcome of the pregnancy. PlGF and sFlt-1 were measured using prototype ARCHITECT immunoassays (Abbott Laboratories, Abbott Park, IL). For each woman, the two biomarkers were measured from the same banked plasma sample aliquot.
The PlGF immunoassay measures the free form of PlGF-1. The assay has a lower limit of detection of 1 pg/mL with a calibration range up to1,500 pg/mL. A 20 day imprecision study using control and panel samples ranging from 12 – 1,000 pg/mL resulted in within run covariance from 1.4 – 6.7% and total co-variance from 1.8 – 6.7%. The assay has shown acceptable dilution linearity up to 6,000 pg/mL using a 4-fold dilution for samples initially reading >1,500 pg/mL.
The sFlt-1 immunoassay measures both free and bound sFlt-1. The assay has a lower limit of detection of 0.10 ng/mL with a calibration range up to 150 ng/mL. A 10 day imprecision study using control and panel samples ranging from 5 – 100 ng/mL resulted in within run covariance from 1.8 – 3.0% and total co-variance from 2.6 – 3.8%.
Statistical Analyses
Analysis of risk factors associated with preeclampsia was conducted using univariate logistic regression. Age, gravida, enrollment CD4+ cell count (< 200 versus ≥ 200 cells/mm3), pretreatment viral load (HIV-1 RNA ≥ 100,000 vs <100,000 copies/ml), HAART regimen, and gestational age at HAART initiation were analyzed using data from all 722 women who had a recorded delivery during the Mma Bana study, including 11 women who developed preeclampsia. Among the subset of 71 women for whom angiogenic markers were assayed, including all 11 preeclamptic women, the associations of PlGF and sFlt-1 and odds of preeclampsia were analyzed using univariate logistic regression. Variables with a p-value ≤ 0.05 in univariate logistic regression were included in a multivariate logistic regression model using data from the same subset.
In the sub-study of angiogenic markers, characteristics of 60 non-preeclamptic women, for whom stored plasma specimens were available, were compared with all other women in the parent study who did not experience preeclampsia. Characteristics involving continuous and ordinal variables were compared using Wilcoxon’s rank sum test. Categorical variables were compared using Fisher’s exact or Chi Square tests. This approach was also employed to analyze differences between these 60 non-preeclamptic women and the 11 women who developed preeclampsia.
Wilcoxon’s rank sum test was used to compare s-Flt1 and PlGF levels at enrollment between non-preeclamptic women and preeclamptic women, to compare median changes in s-Flt1 and PlGF levels one month after HAART initiation among non-preeclamptic women randomized to TZV vs CBV-KAL, all of whom had enrollment CD4+ cell counts ≥ 200 cells/mm3. Moses confidence intervals were calculated for the difference in median change in the two angiogenic markers among non-preeclamptic women randomized to TZV vs CBV-KAL. Wilcoxon’s signed rank test was used to analyze the change in s-Flt1 and PlGF one month after HAART initiation in non-preeclamptic women.
All testing used a two-sided significance level of 0.05, with no correction for multiple testing. Statistical analyses were performed using SAS, version 9.3 (SAS Institute, Cary, North Carolina, USA).
RESULTS
Baseline characteristics
Of 722 Mma Bana women who delivered, 11 women developed preeclampsia. Women who developed preeclampsia had a higher median enrollment log viral load compared with non-preeclamptic women (5.05 log10 copies/ml versus 4.07 log10 copies/ml; p = 0.03) [Table 1]. Preeclamptic women also experienced significantly shorter duration of pregnancy, as would be expected, with a median gestational age at delivery of 35.1 weeks compared with 39.2 weeks among the 711 women who did not experience preeclampsia (p = 0.003). The proportion of women experiencing a stillbirth was significantly higher among preeclamptic women at 64% compared with 2% among non-preeclamptic women (p < 0.001).
Table 1.
Maternal Characteristics by Preeclamptic and Non-Preeclamptic Women
| Maternal Characteristics | Specimen Available (n=11) | Lab Specimen Unavailable (n=711) | p-value |
|---|---|---|---|
|
| |||
| Median age (years) [IQR] | 27.2 [22.2 – 31.0] | 27.2 [23.5 – 31.9] | 0.66* |
|
| |||
| Gravida Including Current Pregnancy (#, %) | 0.62* | ||
| 1 | 2 (19%) | 157 (22%) | |
| 2 | 4 (36%) | 233 (33%) | |
| 3 | 4 (36%) | 158 (22%) | |
| 4 or more | 1 (9%) | 163 (23%) | |
|
| |||
| Maternal BMI at Enrollment (kg/m2) [IQR] | 27.0 (22.6 – 28.8) | 24.6 (22.2 – 27.3) | 0.37* |
|
| |||
| Screening Labs | |||
| Median HIV-1 RNA (log10 copies/ml) [IQR] | 5.05 [3.44 – 5.60] | 4.07 [3.21–4.75] | 0.03* |
| Median CD4+ count (cells/μl) [IQR] | 345 [118 – 473] | 342 [215 – 485] | 0.44* |
|
| |||
| Gestational Age at HAART Initiation (weeks) [IQR] | 26.7 [22.3 – 29.9] | 27.0 [26.3 – 29.6] | 0.31* |
|
| |||
| Gestational Age at Delivery (weeks) [IQR] | 35.1 [30.7 – 35.7] | 39.2 [37.8–40.2] | 0.003* |
|
| |||
| HAART Regimen (#,%) | 0.06† | ||
| Combivir–Nevirapine | 6 (54%) | 160 (23%) | |
| Trizivir | 3 (28%) | 279 (39%) | |
| Combivir-Kaletra | 2 (18%) | 272 (38%) | |
|
| |||
| Stillborn Delivery | 7 (64%) | 17 (2%) | <0.001 |
p-value from Wilcoxon Rank Sums test;
p-value from a Fisher’s Exact test;
p-value from a Chi-Square test;
Risk factors Associated with Preeclampsia
Among the 722 Mma Bana study participants who experienced a delivery, only high viral load (≥ 100,000 copies/ml) was significantly associated with preeclampsia in univariate logistic regression analysis (OR 5.8; 95% CI 1.8, 19.4; p = 0.004). [Table 2] There was a trend toward association between preeclampsia and CD4+ cell count < 200 cells/mm3, as well as the type of HAART regimen initiated. However, neither reached statistical significance. High viral load remained significantly associated with preeclampsia in multivariate models adjusting separately for each of CD4+ cell count at enrollment, HAART regimen and gestational age at HAART initiation.
Table 2.
Univariate Logistic Regression Comparing Characteristics of Preeclamptics to Non-Preeclamptics
| Analyzed Risk Factors | Preeclamptic Women (n= 11) | Non-Preeclamptic Women (n = 711) | Odds Ratio (CI) | p-value |
|---|---|---|---|---|
| Maternal Age (median, IQR) | 27.2 (22.2 – 31.0) | 27.2 (23.5 – 31.9) | 0.97 (0.87 – 1.09) | 0.63 |
|
| ||||
| Number of Pregnancies‡ (#,%) | ||||
| 1 | 2 (1.3%) | 157 (98.7%) | Ref | 0.76 |
| 2 or more | 9 (1.6%) | 554 (98.4%) | 1.27 (0.27 – 5.96) | |
|
| ||||
| CD4+ Cell Count at Enrollment (#,%) | ||||
| < 200 cells/mm3 | 5 (3.3%) | 149 (96.7%) | Ref | 0.06 |
| ≥200 ells/mm3 | 6 (1.1%) | 562 (98.9%) | 0.32 (0.10 – 1.06) | |
|
| ||||
| Log Viral Load at Enrollment (#,%) | ||||
| < 100,000 copies/mL | 5 (0.8%) | 587 (99.2%) | Ref | 0.004 |
| ≥100,000 copies/mL | 6 (4.7%) | 121 (95.3%) | 5.8 (1.8 – 19.4) | |
|
| ||||
| Randomized HAART Regimen (#,%) | ||||
| Combivir-Nevirapine | 6 (3.6%) | 160 (96.4%) | Ref | 0.07 |
| Trizivir | 3 (1.1%) | 279 (98.9%) | 0.29 (0.07 – 1.16) | |
| Combivir-Kaletra | 2 (0.7%) | 272 (99.3%) | 0.20 (0.04 – 0.98) | |
|
| ||||
| Gestational Age at HAART Initiation (median/IQR) | 26.7 (22.3 – 29.9) | 27.0 (26.3 – 29.6) | 0.87 (0.74 – 1.04) | 0.13 |
|
| ||||
| BMI at enrollment (median, IQR) | 27.0 (22.6 – 28.8) | 24.6 (22.2 – 27.3) | 1.05 (0.94 – 1.18) | 0.41 |
Number of pregnancies includes all pregnancies of 20 weeks or greater, including the current pregnancy
Comparison of PlGF and sFlt-1in Preeclamptic Women with Non-preeclamptic Women
Pre-HAART P1GF and sFlt-1 levels were measured in all 11 women who developed preeclampsia and in a subset of 60 women who did not (see Methods). There was no significant difference between the characteristics of the 60 non-preeclamptic women in this subset and the 711 non-preeclamptic women in the overall study population with respect to median age, number of pregnancies, median enrollment CD4+ cell count and viral load, HAART treatment regimen, median gestational age at HAART initiation and at delivery and other socioeconomic characteristics.
The median PlGF level at study enrollment, on the day of HAART initiation, was 130 pg/ml among the 11 women who later developed preeclampsia compared with 992 pg/ml for 60 women who did not experience preeclampsia (p = 0.001) [Figure 1]. The median sFlt-1 level at study enrollment for women who later developed preeclampsia was 17.5 pg/ml compared with 9.4 pg/ml for women who did not experience preeclampsia (p = 0.03) [Figure 1].
Figure 1.
Analyzing the subset of 71 women using univariate logistic regression, viral load ≥ 100,000 copies/ml was a significant predictor of preeclampsia as found in the overall study population. In univariate analyses of the association of preeclampsia with angiogenic markers, every 100 pg/ml decrease in PlGF was associated with a 34% increased odds of preeclampsia (OR 1.34; 95% CI 1.13, 1.69; p = 0.004), while every 2 pg/ml increase in sFlt-1 was associated with a 15% increased odds of preeclampsia (OR 1.15; 95% CI 1.03, 1.28; p = 0.02). In multivariate logistic regression, only PlGF (AOR 1.28 per 100 pg/ml decrease; 95% 1.05, 1.66; p = 0.04) and enrollment viral load of ≥ 100,000 copies/ml (AOR 7.15; 95% CI 1.35, 45.01; p = 0.02) remained significantly associated with preeclampsia after adjustment for sFlt-1 (which was not significant, p=0.18).
Non-preeclamptic Women –Changes in PlGF and sFlt-1 One-Month after HAART Initiation
Among the 53 non-preeclamptic women from whom PlGF assay results were available at enrollment and one month after HAART initiation, the median change in PlGF was 134 pg/ml (IQR −377 to 478 pg/ml; p=0.56 for Wilcoxon signed rank test). The median change in sFlt-1 for the 49 non-preeclamptic women for whom sFlt-1 assay results were available at enrollment and one month after HAART initiation was −0.43 pg/ml (IQR −2.60 to +1.84 pg/ml; p=0.32 for Wilcoxon signed rank test).
To determine whether randomized antiretroviral regimens were associated with changes in angiogenic markers, we analyzed median change in PlGF and sFLT-1 one month after HAART initiation among non-preeclamptic women with enrollment CD4 cell counts ≥ 200 cells/ mm3 at or prior to enrollment who were randomized to TZV or CBV-KAL. The median change in PlGF one month after HAART initiation was −92 pg/ml (IQR −440 to 548 pg/ml) among women randomized to TZV compared with 80 pg/ml (IQR −386 to 211 pg/ml) for women randomized to CBV-KAL (difference in median change: 172 pg/ml, 95% CI, −403 to 336; p=0.82)). The median change in sFlt-1 one month after HAART initiation was −0.43 pg/ml (IQR −2.33 to 4.09 pg/ml) for non-preeclamptic women randomized to TZV compared with −0.30 pg/ml (IQR −2.75 to 1.85 pg/ml) for non-preeclamptic women randomized to CBV-KAL (difference in median change: 0.13 pg/ml, 95% CI, −4.4 to 2.5; p=0.85).
DISCUSSION
Among 722 HIV-1 infected women initiating HAART in pregnancy who delivered in the Mma Bana study, viral load ≥ 100,000 copies/ml at enrollment was significantly associated with increased risk of preeclampsia. Angiogenic markers known to be associated with preeclampsia in non-HIV infected women were similarly associated with preeclampsia in a subset of Mma Bana study participants. Angiogenic marker association was notable prior to the onset maternal hypertension and prior to HAART initiation. For non-preeclamptic women, angiogenic markers did not change significantly during the first month after HAART initiation.
This is the first study, of which we are aware, describing the association between higher pretreatment viral load and preeclampsia among women initiating HAART in pregnancy. In 2010, the World Health Organization revised prevention of mother-to-child HIV transmission (PMTCT) guidelines to advocate initiation of HAART as early as the 14th week of gestation for women diagnosed with HIV in pregnancy who do not require HAART for their own health.25 Whether early initiation of HAART resulting in undetectable viral load by the second half of pregnancy reduces the risk of preeclampsia in women with viral load ≥ 100,000 copies/ml warrants further investigation. Onset of preeclampsia usually occurs in the late second trimester or third trimester of pregnancy. The earliest onset of preeclampsia in our cohort occurred at 26 weeks gestational age. If HAART is found to mitigate this risk, research will also be needed to ascertain the optimal regimen to achieve rapid viral load reduction while ensuring safety to the mother and fetus.
This is also the first study to evaluate angiogenic markers associated with preeclampsia in a cohort of HIV-infected women initiating HAART in pregnancy. The results demonstrate that women who subsequently developed preeclampsia had significantly elevated sFlt-1 and decreased PlGF prior to HAART initiation and antecedent to the combined endpoint of hypertension and proteinuria during the pregnancy. The biomarker patterns observed in our population of HIV-infected women corresponds to patterns reported in cross-sectional studies of otherwise healthy, HIV-uninfected nulliparous women who subsequently developed preeclampsia11, 26,27, suggesting a common mechanism for both HIV-infected and HIV-uninfected women.
Data from prior studies have reported conflicting findings regarding HAART in pregnancy and its association with preeclampsia. Suy et al found increased risk of preeclampsia in the HAART era in their cohort of women in Barcelona, composed predominantly of Caucasians who were on HAART prior to conception.21 HAART use in pregnancy was also associated with increased preeclampsia compared with pregnancies of HIV-infected mothers not receiving HAART in a study conducted by Wimalasundera, et al in the United Kingdom.20 In these cohorts, the rate of preeclampsia among HIV-infected women on HAART did not differ significantly from that of HIV-uninfected controls, leading the authors to conclude that restoration of the immune system may play a pivotal role in restoring the risk of pre-eclampsia.20,21 However, Haeri et al found preeclampsia to be less common among HIV-infected women on HAART compared with HIV-uninfected women (6% vs 12% p = 0.04) in a cohort of women in the United States.28
The introduction of HAART among non-preeclamptic women did not significantly change the angiogenic marker levels one month into HAART treatment. Additionally, we did not detect any significant difference in sFlt-1 or PlGF one month after HAART initiation among non-preeclamptic women with enrollment CD4 cell counts ≥ 200 cells/mm3 when comparing a triple NRTI regimen (TZV) with a protease inhibitor-based regimen (CBV-KAL). These findings should be regarded with caution as they may not have been sufficiently powered to detect differences. Larger studies are needed to determine if specific HAART regimens, initiated during pregnancy, influence preeclampsia angiogenic markers in a significantly different manner. If HAART is associated with preeclampsia, the mechanism is not likely to cause direct adverse shifts in angiogenic markers. Rather, a restoration of a deeper underlying risk is more likely20, with the angiogenic markers remaining useful indicators of risk among the subset who later become preeclamptic.
While our study focused on risk factors of preeclampsia in HIV-infected pregnant women, the proportion of preeclamptic women experiencing stillbirth at 64% is alarming and warrants comment, given the overall proportion of stillbirths was 2% in the study. Preeclamptic women in the Mma Bana study were appropriately referred to a local hospital in a timely manner by study personnel. The high rate of stillbirths reflects healthcare challenges faced in resource-limited settings. WHO has set a goal for eliminating new pediatric HIV infections worldwide by 2015.29 Yet, the stillborn rate experienced by our preeclamptic women highlights the critical need for comprehensive and integrated health services in resource-limited settings for HIV-infected women and their infants, including emergency obstetric and neonatal care. Comprehensive healthcare will not only contribute to the elimination of pediatric HIV infections worldwide, but will optimize maternal-child health.
Our study had some limitations. Because women with baseline CD4+ cell counts < 200 cells/mm3 were eligible for NVP-based HAART initiation as early as the 18th week of gestation, while women with CD4+ cell counts ≥ 200 cell/mm3 initiated CBV-KAL or TZV after the 26th week of gestation, the Mma Bana trial design introduced potential confounding between maternal baseline CD4+ cell count, baseline viral load, gestational age at HAART initiation, and HAART treatment regimen. We separately controlled for CD4 cell count, HAART regimen, and gestational age at HAART initiation with viral load, and did not detect confounding or collinearity. However, future preeclampsia studies controlling for these possible confounders are needed.
We lacked serial measurements of sFlt-1, PlGF or CD4+ cell counts. This precludes analysis of the contribution of HAART to the outcome of preeclampsia among women who had angiogenic marker profiles consistent with the evolution of preeclampsia. Further studies characterizing baseline sFlt-1 and PlGF prior to HAART initiation and serial changes in both angiogenic biomarkers and CD4+ cell counts thereafter would allow for quantitative description of HAART’s contribution to these markers.
In conclusion, women enrolling in the Mma Bana cohort with a baseline viral load ≥ 100,000 copies/ml faced 7-fold higher risk of preeclampsia, after adjusting for two angiogenic markers predictive of preeclampsia. Data from existing large observational studies should be used to validate the association between high viral load and increased risk of preeclampsia. If the association is noted in other studies, it would be of public health importance to determine whether viral load reduction earlier in pregnancy mitigates the risk of preeclampsia. Our results demonstrate that sFlt-1 levels are elevated and PlGF levels are low antecedent to the onset of preeclampsia among HIV-infected women, in a manner comparable with prior studies involving HIV-uninfected women. Among women who did not develop preeclampsia, the analysis did not detect a statistically significant change in the levels of PlGF and sFlt-1 from baseline to 1 month after HAART initiation. Considering the conflicting findings regarding HAART’s association with preeclampsia, larger studies are needed to determine the potential mechanism for preeclampsia risk restoration among women receiving HAART. Finally, the striking rate of stillbirths in our cohort of preeclamptic women speaks to the importance of proactively managing preeclampsia to ensure optimal maternal and infant outcomes.
Acknowledgments
Sources of Funding:
Mma Bana study was supported by a grant (U01-AI066454) from the National Institute of Allergy and Infectious Diseases. Funding support from Brigham and Women’s Global Women’s Health Fellowship supported KMP’s salary during the Mma Bana study and MN’s salary during manuscript preparation. KMP received salary support from Harvard University CFAR grant (P30 AI060354) and NICHD Grant (1K23HD070774-01A1) during the period of manuscript preparation. The Fogarty AITRP grant (D43 TW000004) provided funding for AO and SM. Mma Bana study drugs were provided by Abbott Pharmaceuticals, GlaxoSmithKline, and the government of Botswana.
We are indebted to the women and infants who participated in the Mma Bana study, the Mma Bana study team staff, as well as the administration and staff at Scottish Livingston, Deborah Retief Memorial, Athlone and Princess Marina Hospitals and the staff at the referring health clinics. We are grateful to Abbott Pharmaceuticals, GlaxoSmithKline, and the government of Botswana for the provision of study drugs.
We wish to specifically thank BHP and HSPH Staff: Lillian Makori, Gloria Mayondi, Agnes Modise, Venice Modikwa, Ria Madison, Tlhongbotho Masoloko, Daisy Ramalekane, Molly Pretorius Holme, Heather Carey, Sara Mazzola, Carrie Kachoria, Raabya Rossenkahn, Vlad Novitsky, Chris Rowley, Jennifer Boyle, Michael Roy, Lendsey Melton, Chikezie Nwankwo, Scott Dryden Peterson, Onalenna Nthase, Norah Mawoko, Elias Woldegabriel, Kasonde Micheal, Chandan Harikrishnan, Jane Magetse, Joyce Lubinda, Tebogo Kakhu, Thena Tumediso, Modiegi Diseko, Mosetsanagape Galekhutle, Keamogetse Rebatenne, Mavis Moeng, Kebaibphe Ntalabgwe, Ditlamelo Mareme, Victoria Kgwadi, Kaone Kgati, Keitumetse Sakana, Best Mafoko, Lazarus Moremi, Jimmy Nkgau, Ilori Adewale, Banno Janet Moorad, Dipotso Arbi, Kesego Dudu Kooreng, Selebaleng Vinoliah Simon, Maggie Mosetsanagape Nkgau, Collen Rananna, Rejoice Molefe, Nametso Dimpho Lekwape, Tebogo Ncube, Eldah Kakanyo Tshotlego, Segomotso Mapote, Radinku Tshegofatso, Emmanuel Keikotlhae, William Keboutlwe, Hanqiwe Olebeng, Seleetso Ndicky Modibedi, Tshepo Silwane, Tshepiso Patricia Morupisis, Ntsholeng Kekgethile, Sydney Kgwefane, Julius Kgangetsile, Nnahurumnanya Iwe, Tseo Khudube, Malebogo Ntshimane, Maureen Gower, Nthabiseng Kgaodi, Kate Selathwe, Lorraine Phiri, Rosemary Musonda, Phillimon Segopodi, Dorcas Moses, Terence Mohammed, Dineo Mongwato, Bonolo Khumotaka, Phibeon Munyaradzi Mangwendeza, Chishamiso Mudenyanga, Matshediso Zachariah, Gertrude Ditshotlo, Alex Ntau, Poko Molwane. Botswana Ministry of Health: Khumo Seipone, Shenaaz El Halabi, Pilate Khulumani, Mary Kasule, Madisa Mine, Kgomotso Makhaola, Howard Moffat, Haruna Baba Jibril, and the PMTCT unit. Princess Marina Hospital, Gaborone: Staff of Maternity, Post natal & Children’s ward. Scottish Livingstone Hospital, Molepolole: Staff of Maternity, Post natal & Children’s ward. Deborah Retief Memorial Hospital, Mochudi: Staff of Maternity, Post natal & Children’s ward. Athlone Hospital Lobatse: Staff of Maternity, Post natal & Children’s ward. District Health Teams (Molepolole & Mochudi). City Council Clinics team (Lobatse & Gaborone). GSK: Edde Loeliger. Baylor University: Gabriel Anabwani, Elizabeth Lowenthal. Beth Israel Deaconess Medical Center: Linda Shipton. Harvard Medical School: Jennifer Chen. Oxford University: Philip Goulder, Philippa Mathews. NIH: Lynne Mofenson. DSMB Members and members of the Community Advisory Board.
Footnotes
Presented in Part:
Powis K, McErath T, Ogwu A, Souda S, Moyo S, Nadas M, Makhema J, Machakaire E, Essex M, Shapiro R. HAART initiation during pregnancy and its association with preeclampsia in HIV-1 infected women participating in the Mma Bana study, Botswana. 19th Conference on Retroviruses and Opportunistic Infections, Seattle, United States. March 5th to March 8th, 2012 [Abstract #1025].
Conflicts of Interests
MH has served as a paid DSMB member for Beohringer Ingelheim, Pfizer, Tibotec and Medicines Development.
Clinical Trials.gov Registration Number: NCT00270296
References
- 1.Dolea C, AbouZahr C. Global burden of hypertensive disorders of pregnancy in the year 2000: Evidence and Information for Policy (EIP) World Health Organization; Geneva: Jul, 2003. [Accessed 8-Oct-11]. http://www.who.int/healthinfo/statistics/bod_hypertensivedisordersofpregnancy.pdf. [Google Scholar]
- 2.Villar J, Say L, Shennan A, et al. Methodological and technical issues related to the diagnosis, screening, prevention, and treatment of preeclampsia and eclampsia. International Journal of Gynecology and Obstetrics. 2004;85(Suppl 1):S28–S41. doi: 10.1016/j.ijgo.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 3.Conde-Agudelo A, Villar J, Lindheimer M. Maternal infection and risk of preeclampsia: Systematic review and metaanalysis. American Journal of Obstetrics & Gynecology. 2008;198(1):7–22. doi: 10.1016/j.ajog.2007.07.040. [DOI] [PubMed] [Google Scholar]
- 4.Firoz T, Sanghvi H, Merialdi M, et al. Preeclampsia in low and middle income countries. Best Practices and Research Clinical Obstetrics and Gynaecology. 2011;25:537–548. doi: 10.1016/j.bpobgyn.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Khan KS, Wojdyla D, Say L, et al. WHO analysis of causes of maternal death: a systemic review. Lancet. 2006;367:1066–74. doi: 10.1016/S0140-6736(06)68397-9. [DOI] [PubMed] [Google Scholar]
- 6.Osungbade KO, Ige OK. Public Health Perspectives of Preeclampsia in Developing Countries: Implications for Health System Strengthening. Journal of Pregnancy. 2011 doi: 10.1155/2011/481095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Borchers AT, Naguwa SM, Keen CL, et al. The implications of autoimmunity and pregnancy. Journal of Autoimmunity. 2010;34:J287–J299. doi: 10.1016/j.jaut.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 8.Siddiqui AH, Irani RA, Blackwell SC, et al. Angiotensin Receptor Agonistic Autoantibody Is Highly Prevelant in Preeclampsia: Correlation With Disease Severity. Hypertension. 2010;55:386–393. doi: 10.1161/HYPERTENSIONAHA.109.140061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xia Y, Kellems RE. Receptor-activating autoantibodies and disease: preeclampsia and beyond. Expert Rev Clin Immunol. 2011;7(5):659–74. doi: 10.1586/eci.11.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wallukat G, Neichel D, Nissen E, et al. Agonistic autoantibodies directed against the angiotensin II AT1 receptor in patients with preeclampsia. Can J Physiol Pharmacol. 2003;81:79–83. doi: 10.1139/y02-160. [DOI] [PubMed] [Google Scholar]
- 11.Levine RJ, Maynard SE, Qian C, et al. Circulating Angiogenic Factors and the Risk of Preeclampsia. N Engl J Med. 2004;350:672–83. doi: 10.1056/NEJMoa031884. [DOI] [PubMed] [Google Scholar]
- 12.Vaisbuch E, Whitty JE, Hassan SS, et al. Circulating angiogenic and antiangiogenic factors in women with eclampsia. Am J Obstet Gynecol. 2011;204:152e1–9. doi: 10.1016/j.ajog.2010.08.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Masuyama H, Suwaki N, Nakatsukasa H, et al. Circulating angiogenic factors in preeclampsia, gestational proteinuria, and preeclampsia superimposed on chronic glomerulonephritis. Am J Obstet Gynecol. 2006;194:551–6. doi: 10.1016/j.ajog.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 14.Robinson CJ, Johnson DD, Chang EY, et al. Evaluation of placental growth factor and soluble Fms-like tyrosine kinase 1 receptor levels in mild and severe preeclampsia. Am J Obstet Gynecol. 2006;195:255–9. doi: 10.1016/j.ajog.2005.12.049. [DOI] [PubMed] [Google Scholar]
- 15.Vatten LJ, Eskild A, Nilsen TIL, et al. Changes in circulating level of angiogenic factors from the first to second trimester as predictors of preeclampsia. Am J Obstet Gynecol. 2007;196:239. e1–239. e6. doi: 10.1016/j.ajog.2006.10.909. [DOI] [PubMed] [Google Scholar]
- 16.Yelumalai S, Muniandy S, Omar SZ, et al. Pregnancy-Induced Hypertension and Preeclampsia: Levels of Angiogenic Factors in Malaysian Women. J Clin Biochem Nutr. 2010;47:191–7. doi: 10.3164/jcbn.10-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Powers RW, Jeyabalan A, Clifton RG, et al. Soluble fms-Like Tyrosine Kinase 1 (sFlt-1), Endoglin and Placental Growth Factor (PlGF) in Preeclampsia among High Risk Pregnancies. PLoS ONE. 2010;5(10):e13263. doi: 10.1371/journal.pone.0013263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moore Simas TA, Crawford SL, Solitro MJ, Frost, et al. Angiogenic factors for the prediction of preeclampsia in high-risk women. Am J Obstet Gynecol. 2007;197:244. e1–244. e8. doi: 10.1016/j.ajog.2007.06.030. [DOI] [PubMed] [Google Scholar]
- 19.Stratton P, Tuomala RE, Abboud R, et al. Obstetric and newborn outcomes in a cohort of HIV-infected pregnant women: a report of the women and infants transmission study. J Acquir Immune Defic Syndr Hum Retrovirol. 1999;20:179–86. doi: 10.1097/00042560-199902010-00011. [DOI] [PubMed] [Google Scholar]
- 20.Wimalasundera RC, Larbalestier N, Smith JH, et al. Preeclampsia, antiretroviral therapy, and immune reconstitution. Lancet. 2002;360:1152–54. doi: 10.1016/s0140-6736(02)11195-0. [DOI] [PubMed] [Google Scholar]
- 21.Suy A, Martinez E, Coll O, et al. Increased risk of preeclampsia and fetal death in HIV-infected pregnant women receiving highly active antiretroviral therapy. AIDS. 2006;20:59–66. doi: 10.1097/01.aids.0000198090.70325.bd. [DOI] [PubMed] [Google Scholar]
- 22.Martin F, Taylor GP. The safety of highly active antiretroviral therapy for HIV-positive pregnant mother and her baby: is “the more the merrier”? Journal of Antimicrobial Chemotherapy. 2009;64:895–900. doi: 10.1093/jac/dkp303. [DOI] [PubMed] [Google Scholar]
- 23.Parekh N, Ribaudo H, Souda S, et al. Risk factors for very preterm delivery and delivery of very-small-for-gestational-age infants among HIV-exposed and HIV-unexposed infants in Botswana. International Journal of Gynecology and Obstetrics. 2011;115:20–25. doi: 10.1016/j.ijgo.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 24.Shapiro R, Hughes M, Ogwu A, et al. Antiretroviral Regimens in Pregnancy and Breast-Feeding in Botswana. N Engl J Med. 2010;362:2282–94. doi: 10.1056/NEJMoa0907736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. [Accessed 24 Nov 2012];Antiretroviral Drugs for Treating Pregnant Women and Preventing HIV Infections in Infants: Recommendations for a public health approach 2010 version. Available at: http://whqlibdoc.who.int/publications/2010/9789241599818_eng.pdf. [PubMed]
- 26.Levine RJ, Lam C, Qian C, et al. Soluble endoglin and other circulating antiangogenic factors in preeclampsia. N Engl J Med. 2006;355:992–1005. doi: 10.1056/NEJMoa055352. [DOI] [PubMed] [Google Scholar]
- 27.McKeeman GC, Ardill JE, Caldwell CM, et al. Soluble vascular endothielal growth factor receptor-1 (sflt-1) is increased throughout gestation in patients who have preeclamsia develop. Am J Obstet Gynecol. 2004;191:1240–6. doi: 10.1016/j.ajog.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 28.Haeri S, Shauer M, Dale M, et al. Obstetric and newborn infant outcomes in human immunodeficiency virus-infected women who receive highly active antiretroviral therapy. Am J Obstet Gynecol. 2009;201:315.e1–5. doi: 10.1016/j.ajog.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 29.Towards The Elimination of Mother-to-Child Transmission of HIV: Report of a WHO technical consultation – 9–11 November 2010. World Health Organization; 2011. [Accessed 30-Nov-12]. http://whqlibdoc.who.int/publications/2011/9789241501910_eng.pdf. [Google Scholar]