Abstract
Objective
We aimed to improve pediatric inpatient surveillance at a busy referral hospital in Malawi with 2 new programs: (1) the provision of vital sign equipment and implementation of an inpatient triage program (ITAT) that includes a simplified pediatric severity-of-illness score; (2) task-shifting ITAT to a new cadre of health care workers called “Vital Sign Assistants” (VSAs).
Methods
This study, conducted on the pediatric inpatient ward of a large referral hospital in Malawi, was divided into 3 phases, each lasting 4 weeks. In Phase A, we collected baseline data. In Phase B, we provided 3 new automated vital sign poles and implemented ITAT with current hospital staff. In Phase C, VSAs were introduced and performed ITAT. Our primary outcome measures were the number of vital sign assessments performed and clinician notifications to reassess patients with high ITAT scores.
Results
We enrolled 3,994 patients who received 5,155 vital sign assessments. Assessment frequency was equal between Phases A (0.67 assessments/patient) and B (0.61 assessments/patient), but increased 3.6-fold in Phase C (2.44 assessments/patient, p<0.001). Clinician notifications increased from Phases A (84) and B (113) to Phase C (161, p=0.002). Inpatient mortality fell from Phase A (9.3%) to Phases B (5.7) and C (6.9%).
Conclusions
ITAT with VSAs improved vital sign assessments and nearly doubled clinician notifications of patients needing further assessment due to high ITAT scores, while equipment alone made no difference. Task-shifting ITAT to VSAs may improve outcomes in pediatric hospitals in the developing world.
Keywords: pulse oximetry, pediatric early warning score, task-shift, Malawi, ITAT, vital sign
Introduction
Personnel and resource shortages in sub-Saharan Africa are major obstacles to delivering quality hospital care and achieving World Health Organization (WHO) Millennium Development Goals (Liese 2004, Awases M 2003, Lozano et al. 2011). As a southern African country, Malawi exemplifies these challenges with just 1.1 doctors and 25.5 nurses per 100,000 residents and one of the highest global child mortality rates (Black et al. 2010). Emergency Triage, Assessment, and Treatment (ETAT) (Gove et al. 1999), a component of the WHO Integrated Management of Childhood Illness (IMCI) program (WHO 2005), is a validated triage tool providing simplified, symptom-based guidelines that can reduce overall hospital mortality when used at admission. ETAT is widely accepted as a centerpiece for delivering quality pediatric hospital care in developing countries (Robinson 2011, Robertson & Molyneux 2001, Molyneux et al. 2006). Despite this important contribution, many gaps remain for optimizing pediatric inpatient care.
One such gap is how to best deliver ongoing clinical monitoring throughout a patient’s hospitalization when resources are limited. Given that the clinical condition of most patients remains fluid after admission, with some responding to treatment and others not, a simple monitoring and triage tool akin to ETAT but used for the duration of hospitalization could have important implications for improving pediatric hospital outcomes. In developed countries, severity-of-illness scoring, also known as Pediatric Early Warning System (PEWS) scoring, is an effective tool to quickly identify deteriorating pediatric inpatients (Duncan et al. 2006, Monaghan 2005, Haines et al. 2006, Parshuram et al. 2009, Egdell et al. 2008, Edwards et al. 2009, Tibballs et al. 2005), resulting in substantial reductions in emergent resuscitation (Brilli et al. 2007), other clinical deterioration events (Parshuram et al. 2011), and ward respiratory arrests (Hunt et al. 2008). Adult severity-of-illness scores have been implemented in both South Africa (Rosedale et al. 2011) and Tanzania (Rylance et al. 2009), but pediatric scoring systems have not been reported in developing settings. An additional opportunity for improving inpatient surveillance is task-shifting clinical responsibilities to less costly, trained workers, thereby increasing the number of monitoring personnel on the ward. Task-shifting has been successful in the management of HIV (WHO 2006) and for routine nursing care (Thornley 2000). A simplified pediatric severity-of-illness scoring system that is incorporated into routine vital signs may lead to improved inpatient monitoring and provide an opportunity for task-shifting.
We recently developed and implemented an inpatient monitoring and triage tool for resource-limited settings based on the PEWS concept, using only a thermometer and pulse oximeter to collect routine vital signs and generate a score that identifies hospitalized children at increased risk of death (companion paper). We propose calling this system Inpatient Triage, Assessment, and Treatment (ITAT) since it builds upon key ETAT principles of triage, assessment, and treatment, but also continues these principles on the inpatient ward, after admission. Here, we address the question of how to best implement ITAT in an environment with limited human and material resources, either by equipping and training existing hospital staff or by task-shifting ITAT to a new cadre of trained health care workers, called “Vital Sign Assistants” (VSAs). We hypothesized that current hospital staffing was insufficient to effectively implement ITAT, and task-shifting to VSAs would improve vital sign collection and clinician referrals of patients with high ITAT scores
Methods
Study Population
Kamuzu Central Hospital (KCH) is a large referral hospital in Lilongwe, Malawi with over 15,000 pediatric admissions per year. Non-surgical pediatric patients are initially triaged using ETAT on admission, then admitted to one of several wards. Those with the highest urgency are sent to the acute care, malnutrition, and high-dependency wards. In 2010, KCH had a patient to nurse ratio often exceeding 100:1 (unpublished data), a pediatric HIV prevalence of 8.8%, and an inpatient child mortality rate of 7.0% (McCollum et al. 2011). Physician supervision is limited, resulting in the majority of clinical decisions being made by less-experienced personnel.
Children (age < 15 years) on the acute care and malnutrition wards at KCH from December 2010 to April 2011 were eligible for the study. Children on the surgical, high-dependency unit, and non-acute wards were excluded because they were less ill or already received closely supervised care.
ITAT Training
Nurses, clinicians and VSAs received training on vital sign collection and the ITAT score. For nurses, training consisted of a half-day lecture introducing the ITAT score and practice calculations. A 2-week introductory period followed, where nurses performed ITAT on the wards with senior nurse supervision and no data collection. For VSAs, training involved 2 days of teaching, which included a similar time spent on ITAT score calculation as well as additional training on how to obtain vital signs. VSAs also had a 2-week period of close supervision on the ward by senior nurse supervisors and the program coordinator. All trainees were tested to assess comprehension. After the introductory period, the program coordinator performed a detailed evaluation of the quality of nurse and VSA vital sign collection and ITAT score calculations to determine whether minimum competency was achieved, or whether further training was necessary.
ITAT Score
Vital signs are collected at KCH using automated vital sign poles equipped with a thermometer and pulse oximeter, while respiratory rate is determined by observation. These automated and mobile vital sign poles determine heart rate, oxygen saturation, and temperature with easy-to-use attachment sensors. At the beginning of the study, KCH had one fully operational vital sign pole available on the pediatric ward.
The ITAT score is derived from 4 vital signs: heart rate, respiratory rate, oxygen saturation, and temperature (Olson et al. 2013). A score from 0 to 2 was given for each vital sign based on the age-associated degree of abnormality, higher scores being associated with increased risk of death. The individual scores were then added to provide a cumulative ITAT score of 0 to 8.
Study Design
The study was divided into three consecutive phases (A, B, and C), each lasting six weeks with an initial two-week introductory period. A single-season design was chosen to limit potential confounders, given significant seasonal variability in the volume of hospital admissions, presenting illnesses, and staffing.
Phase A was considered a baseline data collection period and occurred prior to any ITAT training. Vital sign collection sheets (Supplementary Figure 1) were added to all patient charts upon admission. Nurses and clinicians collected and recorded all vital signs during this phase. Other hospitalization data collected from each patient chart at discharge included age, gender, weight, HIV status, discharge diagnoses, outcome, and length of hospitalization.
In Phase B, 3 new vital sign poles (WelchAllyn©, 300 series) fitted with a thermometer and pulse oximeter probe were provided, and nurses were trained as described. ITAT scoring cards were affixed to each pole and posted throughout the wards. Nurses were asked to collect vital signs and calculate ITAT scores on every inpatient twice daily, once before morning rounds and once in the afternoon. If a threshold ITAT score of 4 was surpassed, nurses were asked to immediately notify a clinician. Vital signs, ITAT scores, and clinician notifications were recorded along with hospitalization data for each patient on the admission and malnutrition wards.
In Phase C, five laypersons from the community were hired and trained as VSAs. VSAs had little or no medical background and no previous affiliation to KCH. Each VSA had finished secondary school, was literate, and was bilingual in Chichewa (local language) and English (spoken within the Malawian health care system). Similar to nursing staff in Phase B, VSAs were instructed to collect vital signs and calculate ITAT scores for all children on the admission and malnutrition wards twice daily. At a threshold score of 4, VSAs were instructed to notify a clinician to immediately evaluate the patient. VSAs were compensated by a locally appropriate salary of 850 Malawi kwacha (MWK), or US$ 5.67 USD per day at the time of the study.
Statistical Analyses
Normally-distributed data were presented with mean and standard deviation and compared with one-way ANOVA. When the global test was significant, individual between-group differences were identified with Tukey’s post-hoc test. Non-parametric data were presented with median and interquartile ranges; these data were evaluated by the Kruskal-Wallis test. Proportions were compared using Pearson chi-square tests, and when the global value was significant, individual post-hoc comparisons were made with chi-square or Fisher exact tests, using Bonferroni’s correction to adjust alpha for multiple comparisons. Alpha was similarly adjusted for variables with multiple levels.
ITAT score accuracy was monitored in 2 ways. First, nursing supervisors directly monitored and audited vital sign collection by nurses and VSAs to ensure proper skill performance. Second, nurse/VSA-calculated ITAT scores were compared to SAS-derived ITAT scores to measure correct score tabulation. The scores for each of the four individual measures (range: 0–2) were summed to calculate each individual’s total risk score (range: 0–8) (companion paper). Simple and weighted Kappa statistics were calculated in SAS to estimate agreement between the total risk score calculation and the nurse-or VSA-entered total risk score (-1=perfect disagreement; 0=agreement expected by chance; 1=perfect agreement), excluding missing values. Kappa statistics were estimated for the time period before and after the VSAs were hired (March 23, 2011) to compare accuracy of entered scores by nurses versus VSAs. The weighted Kappa statistic gives credit for partial agreement.
All statistical analyses were performed using IBM SPSS Statistics version 20 (IBM Corporation, Armonk, NY) and SAS version 9.2 (SAS Institute, Cary, North Carolina, USA).
IRB Review
The study was approved by the University of North Carolina Internal Review Board (IRB Study #10-2020) and the Malawi National Health Sciences Research Committee (Protocol #786). Vital signs are a routine component of patient care and do not require individual patient consent. Information pamphlets regarding the study were made available throughout the children’s wards.
Results
A total of 3,994 patients were enrolled during the three study phases (Table 1), with greater numbers admitted during Phases B and C, corresponding with a peak in malaria hospitalizations. The majority of children were admitted with an unknown HIV status. Of the 1,642 children with known HIV status, 6.9% were HIV-infected and 6.8% were HIV-exposed (defined as a child born to an HIV-infected mother and without a definitive HIV diagnosis). Malaria was the most common diagnosis, followed by sepsis and pneumonia. Baseline characteristics of children admitted during the three study phases differed with respect to incidence of malaria, pneumonia, diarrhea/dehydration, convulsions, nutritional status, and age.
Table 1.
Characteristics of study population
| Characteristic | Phase A Dec 2- Jan 19 (n=1040) |
Phase B Feb 9 - Mar 9 (n =1499) |
Phase C Mar 23 - Apr 20 (n =1455) |
P-value |
|---|---|---|---|---|
| Age, median months ± IQR | 25.9 (12.2−53.6) | 20.0 (8.8−41.6) | 26.0 (11.0−51.7) | <0.001‡,∥ |
| Female, n (%) | 460/1027 (44.8) | 682/1495 (45.6) | 708/1449 (48.9) | 0.086 |
| Duration of hospitalization, mean (SD) | 2.1 (2.2) | 2.2 (2.0) | 2.2 (1.9) | 0.208 |
| Weight-for-Age Z score, mean (SD)* | −1.34 (1.52) | −1.18 (1.60) | −1.17 (1.63) | 0.042§ |
| Mod/Severely Underweight, n/N* (%) | 241/732 (32.9) | 350/1263 (27.7) | 299/1130 (26.5) | 0.008‡,§ |
| Severely Underweight, n/N* (%) | 92/732 (12.6) | 160/1263 (12.7) | 143/1130 (12.7) | 0.998 |
| HIV status, n (%) | 0.577 | |||
| Exposed | 26/411 (6.3) | 47/594 (7.9) | 38/637 (6.0) | |
| Infected | 29/411 (7.1) | 36/594 (6.1) | 48/637 (7.5) | |
| Uninfected | 356/411 (86.6) | 511/594 (86.0) | 551/637 (86.5) | |
| Unknown | 629 | 905 | 818 | |
| Top diagnoses†, n (%) | ||||
| Malaria | 857 (82.4) | 1161 (77.5) | 1192 (81.9) | 0.001‡,∥ |
| Sepsis | 304 (29.2) | 405 (27.0) | 367 (25.2) | 0.084 |
| Pneumonia | 164 (15.8) | 524 (35.0) | 303 (20.8) | <0.001‡,§,∥ |
| Diarrhea/dehydration | 140 (13.5) | 111 (7.4) | 125 (8.6) | <0.001‡,§ |
| Meningitis | 79 (7.6) | 90 (6.0) | 98 (6.7) | 0.286 |
| Convulsions | 46 (4.4) | 41 (2.7) | 20 (1.4) | <0.001§,∥ |
IQR, interquartile range; SD, standard deviation
Denominators indicate children under 5 years of age with anthropomorphic data recorded
As many as 3 diagnoses per patient recorded; only diagnoses > 1% prevalence are listed
Phase A was significantly different than Phase B
Phase A was significantly different than Phase C
Phase B was significantly different than Phase C
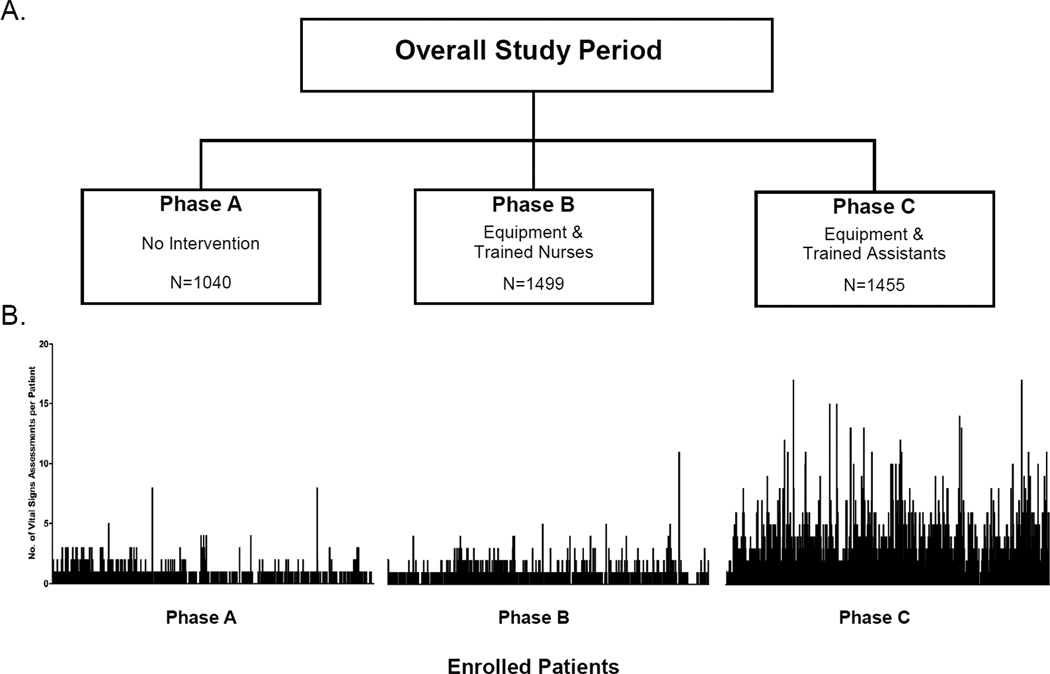
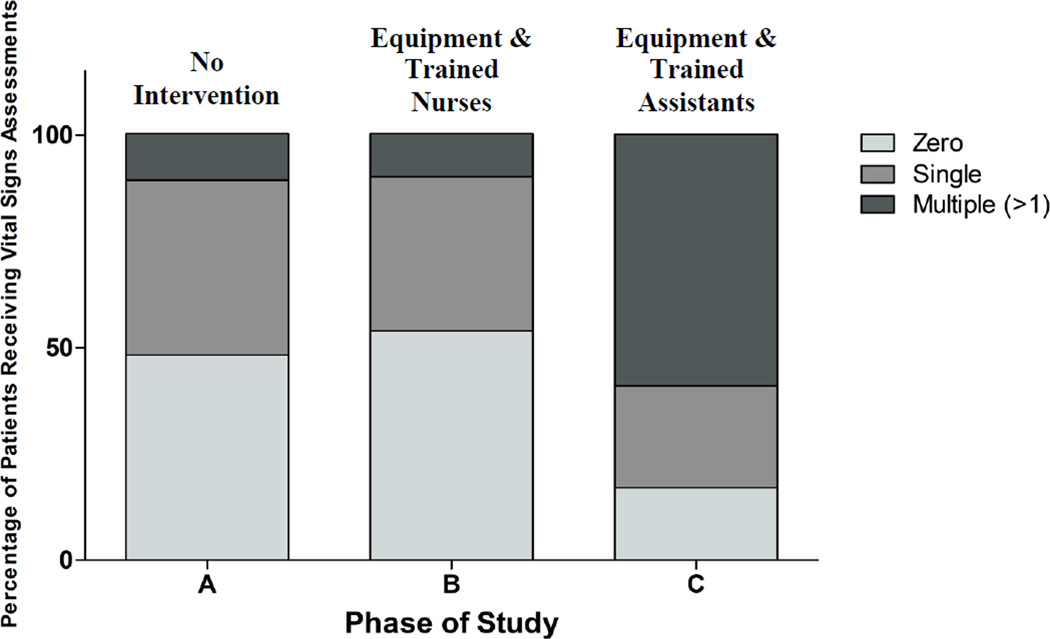
Of the 5,155 vital sign assessments obtained over the entire study period, 3,546 were performed in Phase C, averaging 2.44 assessments per patient per hospitalization, an increase from 0.67 assessments per patient per hospitalization at baseline (Phase A, p < 0.001) and 0.61 assessments per patient per hospitalization by ITAT-trained nurses using additional vital sign poles (Phase B, p < 0.001) (Table 2, Figure 1). The proportion of patients receiving multiple assessments increased almost six-fold from Phase B (10.2%) to Phase C (59.2%) (p < 0.001, Figure 2), while there was no difference between Phases A and B. Thus, the provision of equipment and ITAT-trained nurses led to no increase in the frequency of ITAT assessments, whereas the addition of both ITAT-trained VSAs and equipment led to a nearly four-fold improvement.
Table 2.
Vital sign assessments and inpatient mortality
| Characteristic | Phase A (n=1040) |
Phase B (n =1499) |
Phase C (n =1455) |
P |
|---|---|---|---|---|
| Total Assessments, n | 699 | 910 | 3546 | |
| Assessments Per Patient, mean (SD) | 0.67 (0.8) | 0.61 (0.8) | 2.44 (2.3) | <0.001†,‡ |
| Patients with Score ≥4, n (%) | -- | 71 (4.7) | 182 (12.5) | <0.001 |
| Score ≥4 Plus Notification, n (%) | -- | 42 (2.8) | 133 (9.1) | <0.001 |
| Total Clinician Notifications, n (%) | 84 | 113 | 161 | 0.002†,‡ |
| Patients with a clinician notification, % | 8.1 | 7.5 | 11.1 | |
| Clinician notifications per total ITAT score assessments, % | 12 | 12.4 | 4.5 | |
| Died, n (%) | 97 (9.3) | 85 (5.7) | 100 (6.9) | 0.002* |
| Age at Death, median months (IQR) | 20.1 (8.8 – 46.2) | 18.9 (10.2 – 36.5) | 20.3 (10.9 – 33.0) | 0.989 |
| Admission to Death, mean days (range) | 1.5 (2 – 18) | 1.6 (0 – 19) | 1.2 (0 – 11) | 0.725 |
Phase A was significantly different than Phase B
Phase A was significantly different than Phase C
Phase B was significantly different than Phase C
Figure 1.
Vital sign assessments by study phase. There were 699 assessments in Phase A, 910 assessments in Phase B, and 3946 assessments in Phase C
Figure 2.
Frequency of vital signs assessments by study phase. The frequency of patients with multiple vital sign assessments increased from Phases A (11%) and B (10%) to Phase C (59%)
ITAT score calculation accuracy also improved with the addition of VSAs compared to nurses alone. In Phase B, nursing ITAT score accuracy was only 61.9% compared to SAS-calculated scores. In Phase C, when VSAs performed the majority of ITAT assessments, accuracy was 83.4%. After chart auditing, the nursing supervisors determined that the VSAs correctly performed vital sign assessments and had no need for further training.
Next, we determined whether either intervention led to more frequent clinical re-evaluations in children triaged as higher risk for death (ITAT scores ≥ 4). In Phase C, more patients were identified as having an ITAT score of ≥ 4 and had a clinician notified for review (p < 0.001; Table 2). Although our study was not specifically powered to evaluate mortality, we found that the inpatient mortality rate decreased from 9.3% to 5.7% during Phase B and remained low in Phase C (6.9%) (p = 0.002).
Discussion
Similar to most hospitals throughout southern Africa, KCH is a busy, understaffed facility with a critically ill pediatric population that would benefit from improved inpatient monitoring and triage systems. ITAT is a pediatric inpatient monitoring and triage tool tailored specifically for low-resource settings (companion paper), but the best approach for implementing ITAT is unknown. Our data demonstrate that both the accuracy and the total number of ITAT assessments increased dramatically (3.6-fold) with the addition of equipment and VSAs (Phase C) but not with vital sign equipment and ITAT training for existing staff (Phase B). We also observed an increase in the number of patients with multiple ITAT assessments, allowing clinicians to objectively measure a patient’s clinical status during the hospital course. VSAs helped identify an increased number of patients with an ITAT score ≥ 4, which led to a greater number of clinician notifications for potential medical intervention. The composite of these findings suggests that task-shifting ITAT to VSAs from existing nurses is feasible and yields improved program indicators. A VSA-based ITAT program may also result in improved hospital outcomes if patients receive timely and appropriate interventions.
Many pediatric hospitals have implemented rapid response teams with severity-of-illness scoring systems to urgently assess patients at high risk of rapid clinical deterioration. These response teams have been shown to significantly improve patient outcomes (Tibballs & Kinney 2009, Tibballs & Kinney 2006, Hunt et al. 2008, Sharek et al. 2007, Brilli et al. 2007, Kotsakis et al. 2011). One meta-analysis of hospitals in developed countries showed a 37.7% reduction in the cardiopulmonary arrest rate outside of the intensive care unit and a 21% decrease in overall hospital mortality rate (Chan et al. 2010). A rapid response team at KCH, and most children’s hospitals in southern Africa, is not feasible given severe resource limitations. However, many clinicians and nurses are trained in traditional ETAT (5 clinicians and 24 nurses at KCH during this study (Namathanga 2011)), which includes resuscitation skills and IMCI-based treatment decisions (Molyneux et al. 2006, Robertson & Molyneux 2001, Robinson 2011). Therefore, increased clinical evaluations on the wards should also lead to improved patient mortality.
VSAs were more accurate in their ITAT score calculations than nurses, providing reassurance that task-shifting this duty to individuals with less training does not necessarily lead to less accurate triaging. Nurses have multiple other responsibilities, preventing them adequate time to carefully record and calculate each assessment. Further errors may result from variability in staffing, including locum clinicians, nurses, and students who may not have benefitted from ITAT training. Though task-shifting can improve quality of care (Dovlo 2004, Huicho et al. 2008, Chilopora et al. 2007, Haines et al. 2007, Lewin et al. 2005, Lehmann et al. 2009), some studies have demonstrated worse outcomes when tasks are shifted to inadequately trained personnel (Shutt L 1994, Ofori-Adjei & Arhinful 1996). One advantage of our ITAT program is that the skill requirements were narrow and repetitive enough that a minimal amount of training and supervision was necessary. Narrow repetitive tasks, even those requiring some level of technical skill, may be an area where task-shifting could be more successfully utilized.
With a VSA salary of 850 MWK (US$ 5.67) per day, the weekly cost for three VSAs and a nursing supervisor (including weekends) is relatively low at 18,725 MWK (US$ 124). Altogether this is similar to a full-time government nursing salary, not including costly nursing allowance packages. VSAs also provide several indirect, cost-saving benefits. Instead of performing routine vital signs, nurses are able to focus on more specialized tasks such as placing intravenous lines, administering medications, and providing blood transfusions. We also observed that VSAs take better care of the equipment compared to existing staff, perhaps because they were directly responsible for its maintenance and their jobs were made easier by it functioning properly. As the VSAs became more experienced at recognizing ill-appearing children, they began to subjectively triage hypoxemic or unwell-appearing children as higher risk even if their ITAT score did not objectively meet referral criteria. This observation suggests that the inclusion of a more subjective and potentially time consuming mental status assessment in ITAT may not be necessary. The equipment is the most expensive component of the program. However, costs could be reduced significantly by providing previously used or manual equipment, or hand-held low-cost pulse oximeters and digital thermometers with appropriate additional training. The ITAT program has remained very popular among hospital staff and continues to function 2 years after completion of the study. If the program were expanded, the current VSAs could serve as supervisors at other sites.
We observed a global decrease in the inpatient mortality rate during the study period. However, we cannot account for this mortality reduction primarily with our intervention, which only showed an increase in ITAT assessments in Phase C. Our study was implemented during a single season to avoid patient heterogeneity, but there was variability in the number of children admitted and in diagnoses for each phase. The greater incidence of malaria and decreased incidence of malnutrition in Phases B and C possibly contributed to the mortality trend. Additionally, KCH opened an auxiliary short stay unit near the end of Phase B for new admissions that would likely go home within 24 hours. These patients (15 in Phase B and 346 in Phase C) were not included in the study, and their exclusion likely led to an overestimate of mortality rate for Phase C. A better means of addressing these limitations would be to design a cluster randomized controlled trial, in which multiple large hospitals were evaluated against appropriately-matched controls over an entire year. This study design would help account for any seasonal variability in admissions and diagnoses as well as provide enough power for an analysis of mortality and other secondary outcomes.
While our VSA intervention increased clinical notifications and we assume that clinicians appropriately evaluate and treat patients per ETAT and IMCI guidelines, we were unable to verify the exact quantity and quality of clinician interventions, given poor clinician documentation. Educating all staff in ITAT likely led to increased acceptance of the program and improved clinician response, though this was also not investigated. Future evaluation of this program should include external validation of the ITAT score in a different clinical setting and investigate clinician responses to notification with enhanced data collection tools and clinician monitoring. Additionally, implementing routine vital signs may have benefits outside of direct clinician notification for threshold ITAT scores. The recorded observations that a child has remained febrile or that their score has slowly trended upwards over time may lead to a change in management without necessarily reaching a threshold ITAT score. It would also be worthwhile investigating the employment of VSAs during the night when there are fewer clinicians and a greater need for inpatient surveillance.
In conclusion, we demonstrated that the use of ITAT-trained VSAs greatly improved the delivery of ITAT services, as determined by the dramatic increase in the number and accuracy of ITAT assessments performed and the increased number of clinician notifications for review. Larger, multi-centered studies are needed to confirm whether task-shifting ITAT improves inpatient outcomes such as mortality.
Supplementary Material
Acknowledgments
We would like to thank our assistant program coordinator, Jean Nkhoma, and our Vital Sign Assistants, for their valuable contributions to the success of this program. This work was supported by a grant from Health Empowering Humanity as well as the National Institutes of Health Office of the Director, Fogarty International Center, Office of AIDS Research, National Cancer Center, National Eye Institute, National Heart, Blood, and Lung Institute, National Institute of Dental and Craniofacial Research, National Institute on Drug Abuse, National Institute of Mental Health, National Institute of Allergy and Infectious Diseases, and National Institutes of Health Office of Women’s Health and Research through the Fogarty International Clinical Research Scholars and Fellows Program at Vanderbilt University (R24 TW007988) and the American Relief and Recovery Act. The National Institutes of Health also supported this work through the National Heart Lung and Blood Institute (T32 HL072748-11).
References
- Awases GA, Nyoni J, Chatora R. DHS, B W-A, editor. Migration of Health Professionals in Six Countries: A Synthesis Report. 2003 [Google Scholar]
- Black RE, Cousens S, Johnson HL, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–1987. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- Brilli RJ, Gibson R, Luria JW, et al. Implementation of a medical emergency team in a large pediatric teaching hospital prevents respiratory and cardiopulmonary arrests outside the intensive care unit. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2007;8:236–246. doi: 10.1097/01.PCC.0000262947.72442.EA. quiz 247. [DOI] [PubMed] [Google Scholar]
- Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid Response Teams: A Systematic Review and Meta-analysis. Archives of internal medicine. 2010;170:18–26. doi: 10.1001/archinternmed.2009.424. [DOI] [PubMed] [Google Scholar]
- Chilopora G, Pereira C, Kamwendo F, et al. Postoperative outcome of caesarean sections and other major emergency obstetric surgery by clinical officers and medical officers in Malawi. Human resources for health. 2007;5:17. doi: 10.1186/1478-4491-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovlo D. Using mid-level cadres as substitutes for internationally mobile health professionals in Africa. A desk review. Human resources for health. 2004;2:7. doi: 10.1186/1478-4491-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan H, Hutchison J, Parshuram CS. The Pediatric Early Warning System score: a severity of illness score to predict urgent medical need in hospitalized children. J Crit Care. 2006;21:271–278. doi: 10.1016/j.jcrc.2006.06.007. [DOI] [PubMed] [Google Scholar]
- Edwards ED, Powell CV, Mason BW, Oliver A. Prospective cohort study to test the predictability of the Cardiff and Vale paediatric early warning system. Archives of disease in childhood. 2009;94:602–606. doi: 10.1136/adc.2008.142026. [DOI] [PubMed] [Google Scholar]
- Egdell P, Finlay L, Pedley DK. The PAWS score: validation of an early warning scoring system for the initial assessment of children in the emergency department. Emergency medicine journal : EMJ. 2008;25:745–749. doi: 10.1136/emj.2007.054965. [DOI] [PubMed] [Google Scholar]
- Gove S, Tamburlini G, Molyneux E, Whitesell P, Campbell H. Development and technical basis of simplified guidelines for emergency triage assessment and treatment in developing countries. WHO Integrated Management of Childhood Illness (IMCI) Referral Care Project. Archives of disease in childhood. 1999;81:473–477. doi: 10.1136/adc.81.6.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines A, Sanders D, Lehmann U, et al. Achieving child survival goals: potential contribution of community health workers. Lancet. 2007;369:2121–2131. doi: 10.1016/S0140-6736(07)60325-0. [DOI] [PubMed] [Google Scholar]
- Haines C, Perrott M, Weir P. Promoting care for acutely ill children-development and evaluation of a paediatric early warning tool. Intensive & critical care nursing : the official journal of the British Association of Critical Care Nurses. 2006;22:73–81. doi: 10.1016/j.iccn.2005.09.003. [DOI] [PubMed] [Google Scholar]
- Huicho L, Scherpbier RW, Nkowane AM, Victora CG. How much does quality of child care vary between health workers with differing durations of training? An observational multicountry study. Lancet. 2008;372:910–916. doi: 10.1016/S0140-6736(08)61401-4. [DOI] [PubMed] [Google Scholar]
- Hunt EA, Zimmer KP, Rinke ML, et al. Transition from a traditional code team to a medical emergency team and categorization of cardiopulmonary arrests in a children's center. Archives of pediatrics & adolescent medicine. 2008;162:117–122. doi: 10.1001/archpediatrics.2007.33. [DOI] [PubMed] [Google Scholar]
- Kotsakis A, Lobos AT, Parshuram C, et al. Implementation of a multicenter rapid response system in pediatric academic hospitals is effective. Pediatrics. 2011;128:72–78. doi: 10.1542/peds.2010-0756. [DOI] [PubMed] [Google Scholar]
- Lehmann U, Van Damme W, Barten F, Sanders D. Task shifting: the answer to the human resources crisis in Africa? Human resources for health. 2009;7:49. doi: 10.1186/1478-4491-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewin SA, Dick J, Pond P, et al. Lay health workers in primary and community health care. Cochrane database of systematic reviews. 2005:CD004015. doi: 10.1002/14651858.CD004015.pub2. [DOI] [PubMed] [Google Scholar]
- Liese BD, Gilles . The State of the Health Workforce in Sub-Saharan Africa: Evidence of Crisis and Analysis of Contributing Factors. Washington D.C.: The World Bank; 2004. [Google Scholar]
- Lozano R, Wang H, Foreman KJ, et al. Progress towards Millennium Development Goals 4 and 5 on maternal and child mortality: an updated systematic analysis. Lancet. 2011;378:1139–1165. doi: 10.1016/S0140-6736(11)61337-8. [DOI] [PubMed] [Google Scholar]
- McCollum ED, Preidis GA, Golitko CL, et al. Routine inpatient human immunodeficiency virus testing system increases access to pediatric human immunodeficiency virus care in sub-Saharan Africa. The Pediatric infectious disease journal. 2011;30:e75–e81. doi: 10.1097/INF.0b013e3182103f8a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molyneux E, Ahmad S, Robertson A. Improved triage and emergency care for children reduces inpatient mortality in a resource-constrained setting. Bulletin of the World Health Organization. 2006;84:314–319. doi: 10.2471/blt.04.019505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monaghan A. Detecting and managing deterioration in children. Paediatric nursing. 2005;17:32–35. doi: 10.7748/paed2005.02.17.1.32.c964. [DOI] [PubMed] [Google Scholar]
- Namathanga A. Emergency Triage, Assessment, and Training (ETAT) 2011 Reports. Lilongwe, Malawi: Kamuzu Central Hospital; 2011. [Google Scholar]
- Ofori-Adjei D, Arhinful DK. Effect of training on the clinical management of malaria by medical assistants in Ghana. Social science & medicine. 1996;42:1169–1176. doi: 10.1016/0277-9536(95)00389-4. [DOI] [PubMed] [Google Scholar]
- Parshuram CS, Bayliss A, Reimer J, Middaugh K, Blanchard N. Implementing the Bedside Paediatric Early Warning System in a community hospital: A prospective observational study. Paediatrics & child health. 2011;16:e18–e22. doi: 10.1093/pch/16.3.e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parshuram CS, Hutchison J, Middaugh K. Development and initial validation of the Bedside Paediatric Early Warning System score. Critical care. 2009;13:R135. doi: 10.1186/cc7998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson MA, Molyneux EM. Triage in the developing world--can it be done? Archives of disease in childhood. 2001;85:208–213. doi: 10.1136/adc.85.3.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson JZA, Durand C, Nosek, Namathanga A, Milazi R, Thomas A, Mwansambo C, Kazembe PN, Torrey S. International Child Health Group, Implementation of ETAT (Emergency Triage Assessment And Treatment) in a central hospital in malawi. Arch Dis Child. 2011;96:A74–A75. [Google Scholar]
- Rosedale K, Smith ZA, Davies H, Wood D. The effectiveness of the South African Triage Score (SATS) in a rural emergency department. South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde. 2011;101:537–540. [PubMed] [Google Scholar]
- Rylance J, Baker T, Mushi E, Mashaga D. Use of an early warning score and ability to walk predicts mortality in medical patients admitted to hospitals in Tanzania. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2009;103:790–794. doi: 10.1016/j.trstmh.2009.05.004. [DOI] [PubMed] [Google Scholar]
- Sharek PJ, Parast LM, Leong K, et al. Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU in a Children's Hospital. JAMA : the journal of the American Medical Association. 2007;298:2267–2274. doi: 10.1001/jama.298.19.2267. [DOI] [PubMed] [Google Scholar]
- Shutt LMM. In: Midterm Review Of The Tanzania Family Planning Services Support (FPSS) Project (621-0173). POPTECH Report No. 94-011- 015. PROJECT, P T A, editor. Washington, DC: US Agency for International Development; 1994. [Google Scholar]
- Thornley C. A question of competence? Re-evaluating the roles of the nursing auxiliary and health care assistant in the NHS. Journal of clinical nursing. 2000;9:451–458. doi: 10.1046/j.1365-2702.2000.00398.x. [DOI] [PubMed] [Google Scholar]
- Tibballs J, Kinney S. Evaluation of a paediatric early warning tool--claims unsubstantiated. Intensive & critical care nursing : the official journal of the British Association of Critical Care Nurses. 2006;22:315–316. doi: 10.1016/j.iccn.2006.10.003. author reply 317. [DOI] [PubMed] [Google Scholar]
- Tibballs J, Kinney S. Reduction of hospital mortality and of preventable cardiac arrest and death on introduction of a pediatric medical emergency team. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2009;10:306–312. doi: 10.1097/PCC.0b013e318198b02c. [DOI] [PubMed] [Google Scholar]
- Tibballs J, Kinney S, Duke T, Oakley E, Hennessy M. Reduction of paediatric in-patient cardiac arrest and death with a medical emergency team: preliminary results. Archives of disease in childhood. 2005;90:1148–1152. doi: 10.1136/adc.2004.069401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Handbook : IMCI integrated management of childhood illness. World Health Organisation; 2005. [Google Scholar]
- WHO. Treat, Train, Retain: The AIDS and health workforce plan. Report on the consultation on AIDS and human resources for health, WHO. Geneva: World Health Organization; 2006. available at http://www.who.int/hiv/pub/meetingreports/ttr/en/index.html. Geneva: World Health Organisation. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.