Abstract
Background
Male circumcision can reduce the risk of heterosexually-acquired HIV-1 infection in men. Neonatal male circumcision (NMC) has many potential advantages over circumcision at older ages but little is known about its feasibility and safety in resource-limited settings.
Methods
We performed a randomized trial in southeastern Botswana of Mogen clamp and Plastibell, two commonly used devices for NMC. Follow-up visits occurred at six weeks and four months postpartum. Adverse events, parental satisfaction and staff impressions were recorded.
Results
Of 302 male neonates randomized, 300 (99%) underwent circumcision, 153 (51%) with Mogen clamp and 147 (49%) with Plastibell. There were no major adverse events in the Mogen clamp arm but there were two major adverse events in the Plastibell arm (both were a proximally migrated ring that had to be removed by study staff). Minor adverse events were more common with the Mogen clamp compared with the Plastibell, specifically removal of too little skin and formation of skin bridges or adhesions (12 vs. 1 and 11 vs. 3, respectively, all P<0.05). Five (3%) infants in the Mogen clamp arm and none in the Plastibell arm had minor bleeding (P=0.03). More than 94% of mothers reported being highly or completely satisfied with the procedure.
Conclusions
NMC can be performed in Botswana with a low rate of adverse events and high parental satisfaction. Although the risk of migration and retention of the Plastibell is small, the Mogen clamp may be safer for NMC in regions where immediate emergent medical attention is not available.
Introduction
Three large randomized trials have provided compelling evidence that male circumcision (MC) reduces men's risk of heterosexually-acquired HIV-1 1-3. The World Health Organization (WHO) recommends MC for HIV risk reduction, and states that “Since neonatal circumcision is a less complicated and risky procedure than circumcision performed in young boys, adolescents or adults ... countries should consider how to promote neonatal circumcision in a safe, culturally acceptable and sustainable manner”4. Systematic reviews have confirmed that the neonatal period or infancy are the safest time for MC to be performed5, 6.
Except as part of religious custom, neonatal male circumcision (NMC) is rarely performed in resource-limited settings, even in places where ritual circumcision is performed in older age groups. Previous studies in Botswana have reported, however, that self-reported acceptability of NMC among new mothers was more than 90%7. Building upon this finding, we aimed to address the question of which technique would be safest and ultimately most sustainable for programmatic scale-up of NMC in Botswana. Although specialized devices are utilized for NMC in well-resourced settings to improve the safety of the procedure, none has been carefully studied in resource-limited settings. Commonly-used devices (in circumcising regions) include the Gomco Clamp, the Mogen Clamp and the Plastibell. Based on the results of previous clinical studies regarding the respective ease of use of the devices 8, 9, we elected to evaluate Mogen clamp and Plastibell.
Methods
Study Design
This randomized clinical trial was designed to evaluate Mogen clamp and Plastibell as candidates for scale-up of NMC programs in sub-Saharan Africa. The study was approved by the Botswana Ministry of Health's Health Research and Development Committee (HRDC) and by Brigham and Women's Hospital Institutional Review Board (IRB). Written informed consent was obtained from the mothers or their legal guardians (if mothers were < 21 years, age of majority in Botswana) before neonates underwent randomization.
Subjects
Mothers and infants were enrolled between May 2009 and December 2010 at three hospitals in southeastern Botswana: Princess Marina Hospital in the capital city Gaborone, Scottish Livingstone Hospital in the village of Molepolole, and Deborah Retief Memorial Hospital in the village of Mochudi. Eligible mothers and infants were identified by study staff during visits to the maternity wards in the respective hospitals. Maternal eligibility criteria were Botswana citizenship, non-incarceration and ability to follow-up for four months. Infant eligibility criteria were male gender, gestational age ≥ 37 weeks, age ≤ 28 days of life, birth weight ≥ 2,500 grams, no evidence of neonatal sepsis or other illness requiring hospitalization, no family history of bleeding disorder, no genital or other abnormality that is a contraindication to NMC.
Randomization and Study Interventions
Infants were randomized centrally (using permuted blocks of 10 within each site) after they were brought to the study site for the procedure. Study staff performed a physical exam to exclude infants with abnormalities precluding circumcision.
All infants had approximately one gram of eutectic mixture of local anesthetic (EMLA) applied to penis and covered with an occlusive dressing10; EMLA was wiped off prior to the procedure. Infants’ upper bodies and arms swaddled, and legs restrained by an assistant. Infants had the genital area, lower abdomen and upper legs cleansed with chlorhexidine immediately prior to NMC. During the procedure, infants were given concentrated sucrose solution either by gloved finger or by syringe to augment the anesthetic effect of EMLA, as has been previously described11-13. All infants were given Vitamin K at birth, the standard of care in Botswana.
All circumcisions were performed by a study physician (NN) using clean, rather than sterile, techniques, as had been previously documented to be very safe14, 15. The study physician, who had no significant prior experience in performing NMC, was trained by a pediatric urologist prior to the study initiation and was deemed competent with both devices. All infants were circumcised in accordance with the WHO's “Manual for early infant male circumcision under local anaesthesia”16 and described by our group previously17. Briefly, the Mogen clamp is a reusable stainless steel device that requires a new, sterile scalpel blade for each NMC. The scalpel blades used for the study were all new (disposed after one use). The Plastibell is a disposable plastic device that comes in six sizes (1.1 – 1.7 cm diameter) and requires stainless steel scissors (the scissors may be reusable after proper disinfection). Both devices additionally require stainless steel lacrimal duct probes and hemostats. Between uses, the scissors, lacrimal duct probes, hemostats and Mogen clamps all underwent high-level disinfection. All infants had the wound dressed with gauze and Vaseline. All reusable instruments were disinfected with bleach as per WHO protocol, scrubbed with soap and water and then disinfected with Cidex Opa according to the instructions for high-level disinfection provided in the package insert.
After circumcision, infants were checked for post-procedure bleeding or other immediate complications. Mothers were asked to wait with the infant for two hours following the procedure prior to leaving the facility to ensure there was no excessive bleeding and that the infant had urinated. Mothers were given Vaseline for wound care and written post-procedure care instructions that included a phone number to reach a physician 24 hours a day, seven days a week, in case of any questions or concerns.
Follow-up and Evaluation
Post-procedure follow-up visits were planned to coincide with the national vaccination / well-baby visits at six weeks and four months of infant age. At these visits, parents were asked about complications and child outpatient cards were also reviewed for evidence of visits to non-study clinics or providers for adverse events potentially related to the procedure. At each follow-up, infants also had a physical exam, including inspection of the circumcision, by the study physician.
Outcomes
The primary study outcomes were adverse events and parental satisfaction by randomization arm. Secondary outcomes included staff impressions of the comparative safety, tolerability, and ease of use of the two techniques. We also measured the time taken to perform the procedure from the infant's diaper being removed until the time it was replaced, and recorded the number of Plastibells opened so that correct sizing could be achieved.
Adverse events that were potentially related to NMC were defined prior to study initiation and categorized as bleeding, infection, structural and other. Bleeding requiring only the application of pressure beyond the immediate post-procedure period was defined as a minor adverse event. Intervention other than pressure (e.g. suturing) was defined as a moderate adverse event. A separate clinic visit or hospitalization for bleeding from the circumcision site or need for IV fluids or blood products were categorized as major adverse events. Infection limited to the circumcision site was defined as a minor adverse event. Soft-tissue infection spreading beyond the penis (lower abdominal wall, upper legs) was defined as a moderate adverse event. Systemic infection / sepsis was defined as a major adverse event. Removal of too much or incorrect tissue; removal of too little tissue requiring repeat procedure; or structural injury to glans, urethra or shaft were defined as major adverse events, as were subsequent problems with urination or proximal migration / retention of a Plastibell ring requiring intervention for removal.
As to parental satisfaction, we asked parents to complete a structured questionnaire about their experiences with the procedure at the follow-up visits (including potential problems, and satisfaction measured by a visual analogue scale from 0 – 100%). We defined highly or completely satisfied as a score of 90% or greater. We asked whether parents would be likely to choose NMC for a future son and how likely parents would be to recommend the procedure to a relative or a friend who had a baby boy.
After all participant follow-up visits were completed, study staff were asked to fill-out a short semi-structured questionnaire of their subjective impressions of the two devices.
Statistical Analysis and Safety Monitoring
This study was designed to detect a 20% difference in parental satisfaction between the two techniques with 90% power assuming a significance level of 0.05 and two-sided statistical test. This study was not powered to detect a statistically significant difference in major adverse events between the two devices (with previously reported rates of major complications as low as 0.2% in well-resourced settings, approximately 12,750 infants per arm would be required to detect a doubling in the complication rate)14, 18. Instead, this study was designed to provide preliminary and descriptive data on the safety and sustainability of the Plastibell and Mogen clamp in Botswana that could be used to guide larger safety studies.
Differences in baseline characteristics between randomization arms were assessed using Fisher's exact test for dichotomous and categorical variables and Student's t-test for continuous variables. Analysis of primary outcomes of interest occurred only for infants who underwent circumcision. We compared parental satisfaction between randomization arms at six weeks and four months using Fisher's exact test. All statistical analyses were performed with SAS software version 9.2 (SAS Institute, Cary, NC).
An independent Data Safety Monitoring Committee (DSMC) was responsible for analyzing adverse events at an interim analysis after the 100th baby circumcised had been seen in follow-up.
Results
Study Participants
Between May 2009 and December 2010 there were a total of 1,200 eligible mother / son pairs in the three maternity wards. Working within daily time constraints, our staff invited 808 mothers to participate in the study; 547 (68%) agreed to complete the initial questionnaire and 506 (93%) said they would want NMC. Of these 506, 302 (60%) brought their neonate for NMC and provided written informed consent for the procedure (100/129 [78%] in Mochudi, 102/163 [63%] in Molepolole and 100/255 [39%] in Gaborone).
All 302 infants were enrolled and randomized: 155 to Mogen clamp and 147 to Plastibell. Demographic and clinical characteristics between the randomized groups were well balanced (Table 1). The maternal self-reported HIV status matched national prevalence rates for Botswana19. Overall, 166 (55%) mothers chose to have NMC before hospital discharge and 136 (45%) chose to return from home for NMC.
Table 1.
Baseline Characteristics of Study Population by Randomization Arm
| Mogen (N = 155) N (%)a | Plasti Bell (N = 147) N (%)a | |
|---|---|---|
| Maternal Age (years), median (IQR) | 28 (24 – 33) | 28 (25 – 32) |
| Mothers married and / or cohabitating | 37 (23.9%) | 43 (29.3) |
| Maternal self-reported HIV infected | 62/155 (41.1%) | 51/147 (35.4) |
| Mother on ARVs | 37/62 (60%) | 26/51 (51%) |
| Neonatal Gestational Age at delivery (weeks), median (IQR) | 39 (38-41) | 39 (38-39) |
| Neonatal Birth Weight (kilograms), median (IQR) | 3.2 (2.9-3.5) | 3.2 (3.0 – 3.6) |
| Neonatal Age (days) at circumcision, median (IQR) | 4 (2-11) | 2 (2-5) |
| Site | ||
| Gaborone | 50 (32.3%) | 50 (34.0%) |
| Mochudi | 51 (32.9%) | 49 (33.3%) |
| Molepolole | 54 (34.8%) | 48 (32.7%) |
Column % unless otherwise noted
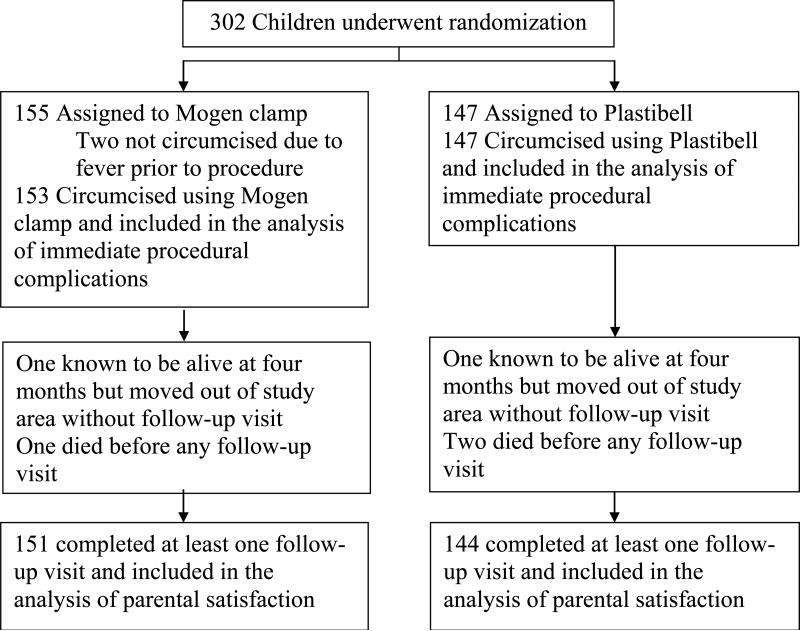
Two neonates, randomized to Mogen clamp, were not circumcised because they developed fever after randomization making them ineligible for the procedure. Therefore, 300 infants were circumcised (153 by Mogen, 147 by Plastibell). All infants were evaluated for immediate complications. A total of 295 (98%) infants had at least one subsequent follow-up visit and 258 (86%) infants completed both scheduled study visits (87% of Mogen clamp arm and 85% of Plastibell arm, P=0.6). Of the five infants with no follow-up after the immediate post-procedure assessment, two moved out of the study area (mothers reported by phone that babies were well) and three died (Figure 1). Of these, two died of gastroenteritis and one died of suspected neonatal sepsis on his second day of life, with the death reviewed by the study DSMC, Botswana HRDC and Brigham and Women's Hospital IRB and not thought to be procedure-related.
Figure 1.
Study Schema of Randomization and Follow-Up
Procedures
No adverse events were associated with the EMLA / sucrose anesthesia. The median duration of EMLA cream application was 73 minutes, absolute range 10 – 286 minutes.
NMC with Mogen clamp required significantly less time than with Plastibell (P<0.0001). The Mogen clamp required a mean of 5.5 minutes (95% confidence interval [CI] 5.1 – 5.8); median of 5 minutes (IQR 4-6), total range 2 – 18 minutes versus Plastibell which required a mean of 7.2 minutes (95% CI 6.9 – 7.5); median 7 minutes (IQR 6-8) total range 4 – 17. The time required for the provider to perform an individual procedure did not change in either arm over the course of the study.
In 86 (59%) of Plastibell cases, only one device was opened to complete the procedure correctly with the appropriately-sized bell. In 58 (40%) of cases two Plastibells were opened and in three cases (2%) three Plastibells were opened for a total of 211 devices opened to complete 147 procedures.
Parents reported a median of seven days until the Plastibell ring fell off (IQR 5-8), with a range from 2-14 days.
Adverse Events
We observed 34 adverse events among 30 infants (10%), with four having two adverse events (Table 2). Two of the 30 experienced a major adverse event from Plastibells that migrated proximally to the corona. In each of these cases the ring had to be removed by the study staff (Figure 2), one at day 14and one at day 17. Neither infant suffered sequelae from the ring retention.
Table 2.
Complications by Randomization Arm
| Mogen (=153) N (%)a | Plastibell (N=147) N (%) | Pb | |
|---|---|---|---|
| Bleeding | 5 (3.2) | 0 | 0.03 |
| Minor | 5 | 0 | |
| Moderate / Severe | 0 | 0 | |
| Infection | 0 | 0 | |
| Too Little Skin Removed | 23 (14.7) | 4 (2.7) | < 0.01 |
| < ½ glans visible | 12 (7.6) | 1 (0.7) | <0.01 |
| Adhesion / Skin Bridge | 11 (7.0) | 3 (2.0) | 0.03 |
| Too Much Skin Removed | 0 | 0 | |
| Plastibell proximal migration | N/A | 2 (1.3) |
Column % unless otherwise noted
Chi square
Figure 2.
Plastibell ring that has migrated and lodged proximal to the corona being removed with ring cutter
The most common adverse event was removal of too little skin (27 cases), as defined by incomplete visualization of the glans (< ½ glans visible) (13 cases), or formation of adhesion / skin bridge (14 cases). Each of these minor adverse events was significantly more common with Mogen clamp than with Plastibell (Table 2). Five (3.2%) infants in the Mogen clamp arm, but none in the Plastibell arm, had minor bleeding immediately after the procedure (all controlled with local pressure) (P=0.03). No other bleeding episodes were reported.
No local or systemic infections were reported, and there were no cases in which too much skin (defined as > ½ shaft denuded) was removed, nor were there other structural complications. As noted earlier, none of the three infant deaths was judged to be procedure-related.
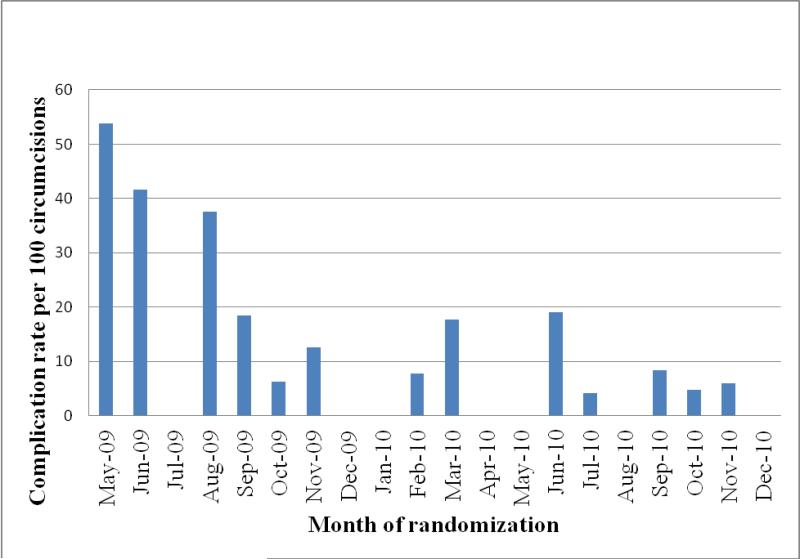
The rate of complications declined over the study period by approximately 0.88 complications / 100 procedures per month (P=0.0004) (Figure 3).
Figure 3.
Complication rate / 100 procedures by month of the study
Parental Satisfaction
Of 278 infants completing the six-week follow-up visit, 96% of mothers whose neonate was circumcised with the Mogen clamp and 95% of those whose neonates were circumcised with the Plastibell reported being highly or completely satisfied with the procedure (P=0.5). Of 278 mothers completing the four-month follow-up visit, 95% of those whose neonate was circumcised with the Mogen clamp and 99% of those whose neonates were circumcised with the Plastibell reported being highly or completely satisfied with the procedure (P=0.04). Regardless of randomization arm, between 96% and 99% of mothers stated they would recommend highly or completely the procedure to a friend or relative. Regardless of randomization arm, at least 97% of mothers reported that they would want NMC for another neonate should they have one.
Sixteen fathers whose neonate was circumcised with Mogen clamp responded to the four-month questionnaire: 16 (100%) were highly or completely satisfied and would recommend NMC to a friend or relative; 15 (94%) would circumcise a future son. Eleven fathers whose neonate was circumcised with Plastibell responded to the four-month questionnaire: all 11 (100%) were highly or completely satisfied, would recommend NMC to a friend or relative and would circumcise a future son.
Mothers whose infants had experienced a complication were significantly less likely to be highly or completely satisfied at six weeks (24/28 versus 242/250, P=0.006) and at four months (24/30 versus 246/248, P<0.0001). Both mothers whose infant had a Plastibell retained were 100% satisfied at four months.
Staff Impressions
The physician who performed all NMCs and the five nurses and three recruiters who assisted him in the procedures all completed a questionnaire regarding their impressions. All nine staff members reported a subjective impression that the Mogen clamp was better tolerated by the baby based on length of the procedure and their impression of infant distress. Six of nine staff considered the Mogen procedure as easier to perform, one believed that the Plastibell was easier, and two felt that the two devices were similarly easy to use. Five staff thought the Plastibell was safer than the Mogen clamp; three thought the Mogen clamp was safer; and one thought the two were equally safe. Five staff thought the neonate's family preferred the Mogen; one thought the Plastibell was preferred; and three thought there was no difference in family preference. When asked which device they would want used for their own child, four would choose Plastibell; two would choose Mogen clamp; and three had no preference. When asked which device should be used for program scale-up, four would choose Mogen clamp; three would choose Plastibell; and one had no preference.
Discussion
We performed the first randomized study of Mogen clamp and Plastibell for NMC in a resource limited setting using clean techniques and found the procedure to have a low rate of adverse events. Reported acceptability of the procedure was high (93% of those interviewed) and although actual uptake of the procedure in our study (55% of all study participants) was higher than that previously reported in sub-Saharan settings (11%)20, more must be learned about barriers to uptake for scale-up to be successful. Parents reported a high level of satisfaction with NMC and it is possible that, with increased knowledge about and experience with NMC in this setting, parents will be more likely to choose the procedure for their sons.
Although this study was not powered to detect a statistically significant difference in adverse events, several important differences were found between the Mogen clamp and the Plastibell. The rate of major adverse events was low overall and was limited to circumcisions done with the Plastibell. Because of the potential for serious morbidity and even mortality if a neonate with a retained Plastibell is not brought quickly to medical attention, we defined a retained Plastibell as a major adverse event. Potential complications of a retained Plastibell include, but are not limited to, urinary retention, bladder rupture and necrosis of the glans 21, 22. Almost all potential complications with the Mogen happen during or immediately following the procedure, while migration and retention of the Plastibell is a late complication and would depend on caregiver recognition and subsequent management by local (sometimes remote) health facilities. Therefore, the Plastibell might not be a good choice for use in areas with low medical literacy or poor access to emergency medical services.
We observed more minor adverse events with the Mogen clamp compared to the Plastibell, the most frequent one was too little skin being removed. This complication became less common as the study progressed and as the provider became more comfortable with the instrument and better able to gauge how much tissue to remove. The use of a surgical pen, recommended for NMC by the WHO, to mark the corona and delineate landmarks prior to the procedure, could reduce the frequency of this complication 16. This study was conducted prior to the publication of WHO guidelines and a surgical pen was not used. We would strongly recommend the use of a surgical pen for all NMC procedures to avoid the problem of removing too little skin; if not enough foreskin is removed, the protective effect of male circumcision against HIV and other sexually transmitted infectious could be reduced.
Although we did not observe any injury to the glans in our study, partial amputation of the glans has been reported with the Mogen clamp23-25. We did not observe excess bleeding with the Plastibell, but this too has been reported16.
One drawback to both techniques is that, other than the disposable Plastibell and a disposable scalpel blade, all instruments require high-level disinfection or sterilization between successive uses. Another logistic complexity that must be considered with the Plastibell is the importance of having all six sizes available at all times: bells that are too large or too small for the child may be more likely to result in complications such as proximal migration and retention, highlighting the importance of supply-chain management. This is especially crucial for NMC programs because successful scale-up will depend on providing the services at local health facilities where women either deliver or bring babies for vaccinations. Remote health facilities would have to be able to maintain an adequate supply chain to ensure safety.
Staff involved in the study universally thought the Mogen clamp was better tolerated by the baby than the Plastibell (and indeed the procedure duration was significantly shorter with the Mogen clamp). The only previously published randomized study of Mogen clamp and Plastibell, which was conducted in the United States, reported that the Mogen clamp was “associated with less pain and discomfort [for the infant]”26.
Finally, the issue of neonatal mortality must be addressed. In many parts of sub-Saharan Africa neonatal mortality rates continue to be unacceptably high and may be slow to decline. Where diagnostic capabilities are limited, it can be difficult to make a definitive diagnosis as to the cause of a neonate's death. Therefore, we would strongly recommend that if a provider detects any sign of neonatal illness, that the NMC procedure be postponed until the neonate is deemed clinically well. Although NMC has been shown to be very safe in resource-rich settings14, 18 and should be equally safe in resource-limited settings, it is important that providers perform NMC only when the risks of the procedure can be absolutely minimized, and that the public be educated about the safety of NMC so that neonatal deaths are not erroneously attributed to the procedure.
Limitations
The study was small and therefore unable to detect all potential adverse events that might occur with programmatic scale-up of NMC. Programmatic monitoring and evaluation of uptake, outcomes and complications will be necessary as the procedure is taken to scale to ascertain true rates of adverse events.
Also, in order to study the devices themselves while reducing other variables that could influence outcomes, one trained physician performed all the NMCs, therefore our results may not be applicable to settings where non-physicians would be performing the procedure. Furthermore, our procedures were performed in on the premises of district hospitals and our findings may not be generalizable to lower-resourced clinical settings.
Although fathers can be important decision makers with regard to MC27, 28, few fathers participated in our study; at the time of delivery less than 30% of women were married to or cohabitating with a partner. Furthermore, in Botswana there is a traditional period of confinement for mothers and infants during which fathers are discouraged from visiting. This may have reduced the availability of fathers to participate in the follow-up visits.
Conclusions
Neonatal male circumcision conducted under clean, rather than sterile, conditions can be performed safely in Botswana. We observed only two major adverse events, both being a proximally migrated, retained Plastibell ring that had to be removed by study staff. In areas with limited access to emergency medical care, we consider the Mogen clamp to be a safer choice than the Plastibell for public sector scale up in HIV-prevention programs. Innovative devices for NMC that would improve the safety and reduce the complexity of disinfection and supply-chain management would be an important advance for use in resource-limited settings.
Acknowledgements
We would like to thank Magdeline Mabuse for her assistance in completing this study.
Funding Sources:
Supported by NIH 5K23AI084579 from the National Institutes of Allergy and Infectious Diseases (Dr. Plank). The study was supported through the President's Emergency Plan for AIDS Relief (PEPFAR) grant U2GPS000941-01, Programme No. 08-P0157. The content is solely the responsibility of the authors and does not necessarily represent the official views of PEPFAR or the National Institutes of Health.
Role of the funding source
The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Footnotes
Meeting at which parts of the data were presented (interim analysis of first 100 babies circumcised):
“Neonatal Male Circumcision in Gaborone, Botswana, and Surrounding Areas: Uptake and Outcomes”, Poster 1005. 18th Conference on Retroviruses and Opportunistic Infections (CROI), February 2011, Boston, MA.
“Infant Male Circumcision in Botswana as Part of Public HIV-Prevention Efforts”, Oral Presentation. Scaling-up male circumcision programmes in the Eastern and Southern Africa Region, UNAIDS / WHO Meeting, June 2010, Arusha, Tanzania.
Financial Disclosures
None of the authors has any conflict of interest or financial disclosure pertinent to this publication.
This trial is registered with ClinicalTrials.gov with the number NCT00971958.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Rebeca M Plank, Division of Infectious Diseases, Brigham and Women's Hospital Harvard School of Public Health, Department of Immunology and Infectious Diseases Botswana-Harvard School of Public Health AIDS Initiative Partnership for HIV Research and Education 15 Francis Street, PBB-A-4 Boston, MA 02115.
Nnamdi O Ndubuka, Botswana-Harvard School of Public Health AIDS Initiative Partnership for HIV Research and Education drndubuka@gmail.com.
Kathleen E Wirth, Botswana-Harvard School of Public Health AIDS Initiative Partnership for HIV Research and Education Harvard School of Public Health, Department of Epidemiology kwirth@hsph.harvard.edu.
Janet T Mwambona, Botswana Ministry of Health janetulim@gmail.com.
Poloko Kebaabetswe, University of Botswana, School of Medicine Poloko.kebaabetswe@mopipi.ub.bw.
Barbara Bassil, Botswana Ministry of Health barbarabassil@hotmail.com.
Chiapo Lesetedi, Botswana Ministry of Health drlesetedi@yahoo.co.uk.
Fatma M Hussein, Botswana Ministry of Health fmtiro@gmail.com.
Jane Magetse, Botswana-Harvard School of Public Health AIDS Initiative Partnership for HIV Research and Education jmagetse@bhp.org.bw.
Maggie Nkgau, Botswana-Harvard School of Public Health AIDS Initiative Partnership for HIV Research and Education mnkgau@bhp.org.bw.
Joseph Makhema, Botswana-Harvard School of Public Health AIDS Initiative Partnership for HIV Research and Education jmakhema@bhp.org.bw.
Mompati Mmalane, Botswana-Harvard School of Public Health AIDS Initiative Partnership for HIV Research and Education mmmalane@bhp.org.bw.
Tracy Creek, Children's Healthcare of Atlanta Tracy.Creek@choa.org.
Kathleen M Powis, Departments of Internal Medicine and Pediatrics, Massachusetts General Hospital Harvard School of Public Health, Department of Immunology and Infectious Diseases Botswana-Harvard School of Public Health AIDS Initiative Partnership for HIV Research and Education kpowis@partners.org.
Roger Shapiro, Beth Israel Deaconess Medical Center, Division of Infectious Diseases Harvard School of Public Health, Department of Immunology and Infectious Diseases Botswana-Harvard School of Public Health AIDS Initiative Partnership for HIV Research and Education rshapiro999@gmail.com.
Shahin Lockman, Division of Infectious Diseases, Brigham and Women's Hospital Harvard School of Public Health, Department of Immunology and Infectious Diseases Botswana-Harvard School of Public Health AIDS Initiative Partnership for HIV Research and Education Shahin.Lockman@gmail.com.
References
- 1.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005 Nov;2(11):e298. doi: 10.1371/journal.pmed.0020298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007 Feb 24;369(9562):643–656. doi: 10.1016/S0140-6736(07)60312-2. [DOI] [PubMed] [Google Scholar]
- 3.Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007 Feb 24;369(9562):657–666. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- 4.WHO New Data on Male Circumcision and HIV Prevention: Policy and Programme Implications. 2007 http://www.who.int/hiv/mediacentre/MCrecommendations_en.pdf.
- 5.Weiss HA, Larke N, Halperin D, Schenker I. Complications of circumcision in male neonates, infants and children: a systematic review. BMC Urol. 2010;10:2. doi: 10.1186/1471-2490-10-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.UNAIDS . Neonatal and child male circumcision: a global review. UNAIDS; Geneva: 2010. [Google Scholar]
- 7.Plank RM, Makhema J, Kebaabetswe P, et al. Acceptability of infant male circumcision as part of HIV prevention and male reproductive health efforts in Gaborone, Botswana, and surrounding areas. AIDS Behav. 2010 Oct;14(5):1198–1202. doi: 10.1007/s10461-009-9632-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kurtis PS, DeSilva HN, Bernstein BA, Malakh L, Schechter NL. A comparison of the Mogen and Gomco clamps in combination with dorsal penile nerve block in minimizing the pain of neonatal circumcision. Pediatrics. 1999 Feb;103(2):E23. doi: 10.1542/peds.103.2.e23. [DOI] [PubMed] [Google Scholar]
- 9.Kaufman GE, Cimo S, Miller LW, Blass EM. An evaluation of the effects of sucrose on neonatal pain with 2 commonly used circumcision methods. Am J Obstet Gynecol. 2002 Mar;186(3):564–568. doi: 10.1067/mob.2002.121621. [DOI] [PubMed] [Google Scholar]
- 10.Plank RM, Kubiak DW, Abdullahi RB, et al. Loss of anatomical landmarks with eutectic mixture of local anesthetic cream for neonatal male circumcision. J Pediatr Urol. 2012 Oct 23; doi: 10.1016/j.jpurol.2012.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taddio A. Pain management for neonatal circumcision. Paediatr Drugs. 2001;3(2):101–111. doi: 10.2165/00128072-200103020-00003. [DOI] [PubMed] [Google Scholar]
- 12.Brady-Fryer B, Wiebe N, Lander JA. Pain relief for neonatal circumcision. Cochrane Database Syst Rev. 2004;(4):CD004217. doi: 10.1002/14651858.CD004217.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blass EM, Hoffmeyer LB. Sucrose as an analgesic for newborn infants. Pediatrics. 1991 Feb;87(2):215–218. [PubMed] [Google Scholar]
- 14.Ben Chaim J, Livne PM, Binyamini J, Hardak B, Ben-Meir D, Mor Y. Complications of circumcision in Israel: a one year multicenter survey. Isr Med Assoc J. 2005 Jun;7(6):368–370. [PubMed] [Google Scholar]
- 15.Naimer SA, Trattner A. Are sterile conditions essential for all forms of cutaneous surgery? The case of ritual neonatal circumcision. J Cutan Med Surg. 2000 Oct;4(4):177–180. doi: 10.1177/120347540000400401. [DOI] [PubMed] [Google Scholar]
- 16.WHO . Manual for early infant male circumcision under local anaesthesia. WHO Document Production Services; Geneva, Switzerland: 2011. [Google Scholar]
- 17.Plank RM, Ndubuka N, Mwambona J, et al. Neonatal Male Circumcision in Gaborone, Botswana, and Surrounding Areas: Uptake and Outcomes.. 18th Conference on Retroviruses and Opportunistic Infections; Vol Boston, Massachusetts, USA. 2011. [Google Scholar]
- 18.Wiswell TE, Geschke DW. Risks from circumcision during the first month of life compared with those for uncircumcised boys. Pediatrics. 1989 Jun;83(6):1011–1015. [PubMed] [Google Scholar]
- 19.Botswana-MOH . In: Botswana AIDS Impact Survey III. Office CS, editor. Gaborone; Botswana: 2009. [Google Scholar]
- 20.Waters E, Li M, Mugisa B, et al. Acceptability and Uptake of Neonatal Male Circumcision in Lusaka, Zambia. AIDS Behav. 2012 Sep 12; doi: 10.1007/s10461-012-0297-8. [DOI] [PubMed] [Google Scholar]
- 21.Bode CO, Ikhisemojie S, Ademuyiwa AO. Penile injuries from proximal migration of the Plastibell circumcision ring. J Pediatr Urol. 2010 Feb;6(1):23–27. doi: 10.1016/j.jpurol.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 22.Cairns JT. Circumcision: A minor procedure? Paediatr Child Health. 2007 Apr;12(4):311–312. doi: 10.1093/pch/12.7.612a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Neulander E, Walfisch S, Kaneti J. Amputation of distal penile glans during neonatal ritual circumcision--a rare complication. Br J Urol. 1996 Jun;77(6):924–925. doi: 10.1046/j.1464-410x.1996.06934.x. [DOI] [PubMed] [Google Scholar]
- 24.Young MR, Bailey RC, Odoyo-June E, et al. Safety of over Twelve Hundred Infant Male Circumcisions Using the Mogen Clamp in Kenya. PLoS One. 2012;7(10):e47395. doi: 10.1371/journal.pone.0047395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pippi Salle JL, Jesus LE, Lorenzo AJ, et al. Glans amputation during routine neonatal circumcision: Mechanism of injury and strategy for prevention. J Pediatr Urol. 2012 Nov 5; doi: 10.1016/j.jpurol.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 26.Taeusch HW, Martinez AM, Partridge JC, Sniderman S, Armstrong-Wells J, Fuentes-Afflick E. Pain during Mogen or PlastiBell circumcision. J Perinatol. 2002 Apr-May;22(3):214–218. doi: 10.1038/sj.jp.7210653. [DOI] [PubMed] [Google Scholar]
- 27.Young MR, Odoyo-June E, Nordstrom SK, et al. Factors Associated With Uptake of Infant Male Circumcision for HIV Prevention in Western Kenya. Pediatrics. 2012 Jul;130(1):e175–182. doi: 10.1542/peds.2011-2290. [DOI] [PubMed] [Google Scholar]
- 28.Mavhu W, Hatzold K, Laver SM, et al. Acceptability of early infant male circumcision as an HIV prevention intervention in Zimbabwe: a qualitative perspective. PLoS One. 2012;7(2):e32475. doi: 10.1371/journal.pone.0032475. [DOI] [PMC free article] [PubMed] [Google Scholar]