Abstract
Background
Checklists can standardize patient care, reduce errors, and improve health outcomes. For meningitis in resource-limited settings, with high patient loads and limited financial resources, CNS diagnostic algorithms may be useful to guide diagnosis and treatment. However, the cost-effectiveness of such algorithms is unknown.
Methods
We used decision analysis methodology to evaluate the costs, diagnostic yield, and cost-effectiveness of diagnostic strategies for adults with suspected meningitis in resource limited settings with moderate/high HIV prevalence. We considered three strategies: 1) comprehensive “shotgun” approach of utilizing all routine tests; 2) “stepwise” strategy with tests performed in a specific order with additional TB diagnostics; 3) “minimalist” strategy of sequential ordering of high-yield tests only. Each strategy resulted in one of four meningitis diagnoses: bacterial (4%), cryptococcal (59%), TB (8%), or other (aseptic) meningitis (29%). In model development, we utilized prevalence data from two Ugandan sites and published data on test performance. We validated the strategies with data from Malawi, South Africa, and Zimbabwe.
Results
The current comprehensive testing strategy resulted in 93.3% correct meningitis diagnoses costing $32.00/patient. A stepwise strategy had 93.8% correct diagnoses costing an average of $9.72/patient, and a minimalist strategy had 91.1% correct diagnoses costing an average of $6.17/patient. The incremental cost effectiveness ratio was $133 per additional correct diagnosis for the stepwise over minimalist strategy.
Conclusions
Through strategically choosing the order and type of testing coupled with disease prevalence rates, algorithms can deliver more care more efficiently. The algorithms presented herein are generalizable to East Africa and Southern Africa.
MESH Terms: Meningitis/DI, Meningitis/EC, Meningitis/EP, Cost Analysis, Diagnostic Techniques and Procedures/CF, Diagnosis Differential, Cryptococcal Meningitis, TB Meningitis, Bacterial Meningitis, Humans
Background
In resource-limited settings, the management of diseases is difficult due to limited diagnostic capabilities, inadequate treatment options, and overburdened staff. Checklists and treatment algorithms are an efficient way for staff with a wide range of skill sets and experience to quickly and accurately diagnose and treat patients, in a consistent manner. Although these techniques have significant advantages, their cost-effectiveness is rarely examined. Maximizing the use of limited resources is essential for long-term sustainability. Creating cost-effective algorithms and checklists is one such method to achieve this objective.
The management of central nervous system (CNS) infections is difficult across all settings due to the high mortality and morbidity rates if proper treatment is not initiated promptly. Common CNS infections include bacterial meningitis, cryptococcal meningitis (CM), tuberculosis meningitis (TBM), viral meningitis (VM), and various types of encephalitis and cerebral abscesses.1 In resource-limited settings, case management of CNS infections is extremely difficult with in-hospital mortality rates of 17–67% for bacterial meningitis, 40–69% for TBM, and 19–50% for CM in Sub-Saharan Africa.2,3 Of clinical importance is the prevalence of HIV/AIDS, and how AIDS influences disease prevalence rates and outcomes. With an estimated 9.7 to 11.5 million children and adults in Sub-Saharan Africa requiring antiretroviral therapy (ART) in 2010,4 opportunistic infections are expected to continue for the foreseeable future requiring clinical tools to enhance diagnosis and treatment of CNS infections.
In an effort to reduce patient morbidity and mortality associated with non-outbreak meningitis, a meningitis diagnostic algorithm was developed and implemented at the Mulago National Referral Hospital in Kampala, Uganda and Mbarara Regional Referral Hospital in Mbarara, Uganda, where the most common causes of death are CNS infections, pneumonia, and tuberculosis (TB).5 With high patient loads, limited financial resources, and inadequate number of clinicians, CNS treatment algorithms and diagnostic checklists could be useful tools to assist in the diagnosis and treatment of meningitis; however, the overall costs and diagnostic yield of the algorithms should be assessed. Therefore, the goal of our analysis was to evaluate the costs, diagnostic yield, and cost-effectiveness of the current CNS algorithm as well as develop and evaluate alternative algorithms that would enhance case management without draining resources.
Methods
Decision Model
We used the methods of decision analysis to evaluate the costs and diagnostic yield associated with various meningitis diagnostic algorithms. We evaluated three diagnostic strategies for HIV-infected adults : 1) comprehensive testing, 2) stepwise testing, and 3) minimalist testing. We focused on these patients because the HIV prevalence in sub-Saharan Africa is high and differential diagnosis for meningitis symptoms among HIV-infected adults is broader, often including cryptococcosis and TB. In a decision tree framework we assigned true disease status to a cohort of individuals with signs and symptoms for meningitis, based on the prevalence of four possible disease states: bacterial meningitis, CM, TBM, or ‘other’ disease. On the basis of the sensitivities and specificities of the tests used, each strategy yielded one of four final diagnoses: bacterial meningitis, CM, TBM, or ‘other meningitis’, which triggered clinical management of the diagnosed disease. The ‘other meningitis’ diagnosis includes suspicion of viral meningitis as well as individuals with negative results, with the assumption that supportive care treatment would be administered for all individuals when a definitive diagnosis was not achieved. Additionally, we assumed only one infectious etiology can occur at one time, and that all diagnostic tests are dichotomous (i.e. positive for a particular etiology or negative for that etiology) and conditionally independent. Simultaneous CM and TBM co-infection can occur but are rare (0.2%).6 CD4 counts were not incorporated into the model as the time to receipt of CD4 results varies by health center.
The ‘comprehensive strategy’ mimicked the diagnostic algorithm utilized in the Cryptococcal Optimal ART Timing (COAT) trial (clinicaltrials.gov: NCT01075152), which was a randomized strategy trial to determine if early or deferred ART was optimal for 6-month survival. The comprehensive strategy’ is representative of a common “shotgun” approach many clinicians in middle and high income countries use when ruling in and ruling out disease or infection. In this strategy, all (available) diagnostic tests would be ordered simultaneously by the clinician with the laboratory running all diagnostic tests simultaneously (Supplemental_Figure1). The second, ‘stepwise strategy’ limited the number and order of diagnostic tests performed, prioritizing tests with a high sensitivity for the most prevalent diseases. Diagnostic tests were run sequentially until a diagnosis was made or all available diagnostic tests were performed (Supplemental_Figure2). The stepwise algorithm allowed for additional TB diagnostic testing (e.g. Xpert MTB/RIF) on small subset of selected high-risk patients. The ‘minimalist strategy’ used a similar sequential stepwise testing approach, except significantly limiting the number and order of diagnostic tests to high-yield tests only, eliminating tests with poor sensitivity/specificity (Supplemental_Figure3).
Model Inputs
We used data obtained from 416 HIV-infected patients screened with suspected CNS infections from November 2010 to November 2012 at Mulago national Hospital in Kampala, Uganda and Mbarara Regional Referral Hospital, Mbarara, Uganda. We estimated the underlying risk for one of four disease states: bacterial meningitis, CM, TBM, or ‘other’ disease. Of the 416 patients, 4% had suspected bacterial meningitis, 8% had probable/definite TBM, 59% had laboratory confirmed CM, and 29% had suspected viral meningitis or other (non-meningitis) diagnosis. In the sensitivity analysis, we used prevalence data from published studies conducted at GF Jooste Hospital in Cape Town, South Africa; at Queen Elizabeth Central Hospital in Blantyre, Malawi; and Harare Central and Parirenyatwa Hospitals in Harare, Zimbabwe. (Table 1).6–8 All studies had a robust sample size with a high prevalence (>75%) of HIV/AIDS.
Table 1.
Prevalence of Meningitis Etiologies in Sub-Saharan Africa
| Hospital | Country | Sample Size | HIV infected | Meningitis Prevalence | |||
|---|---|---|---|---|---|---|---|
| Bacterial/Pyogenic | Tuberculosis | Cryptococcal | Other Meningitis | ||||
| Mulago and Mbarara | Uganda | 416 | 98% | 4% | 8% | 59% | 29% |
| GF Jooste 6 | South Africa | 1,737 | 96%* | 19% | 13% | 30% | 38% |
| Queen Elizabeth Central 7 | Malawi | 263 | 77% | 20% | 17% | 43% | 20% |
| Harare Central and Parirenyatwa 8 | Zimbabwe | 200 | 90% | 16% | 12% | 45% | 28% |
| Pooled Average | 2616 | 93% | 9.3% (8.2–10.5%) | 12.7% (11–14%) | 37% (35–39%) | 41% (40–43%) | |
among bacterial, TB, and cryptococcal meningitis patients.
Pooled estimate includes weighted mean (95% confidence interval).
The meningitis diagnostic algorithms utilized the most common diagnostic tests available. The diagnostic testing probabilities (sensitivity and specificity values) varied by strategy with the dichotomous cut-off values to determine positive and negative test status being obtained from the medical literature (Table 2).9–29
Table 2.
Diagnostic Test Characteristics and Costs
| Diagnostic Test | Sensitivity | Specificity | Cost (US$) | Reference |
|---|---|---|---|---|
| Total WBC >5 cells/μL | 71–75 % | 95 % | $3.03 | 6,9 |
| Differential White Cell Count >50% (PMN/Lymph) for Bacterial Meningiits | 85–90 % | 43 % | - | 10,11 |
| CSF : Serum Glucose for Other | 100 % | unknown | $3.06 | 12 |
| CSF : Serum Glucose (Ratio <.5) | 81 % | 84 % | - | 11,12 |
| CSF Protein (>50mg/dL) | 88 % | 60 % | $2.63 | 11,12 |
| Bacterial Culture (CSF) | 92 % | 95–99% | $5.52 | 9 |
| Gram’s Stain | 92 % | 99 % | $4.30 | 13 |
| AFB stain <6mL volume for TBM 1 | 0–15 % | 100 % | $4.30 | 6,14–16 |
| AFB >6mL volume for TBM | 52–87 % | 100 % | $4.30 | 16–19 |
| Xpert MTB/RIF Assay for TBM | ~60 % (95% CI: 40–80%) | ~100% in CSF | $15.00 2 | 20–22 |
| India Ink for Cryptococcal Meningitis | 60–84 % | 99 % | $4.30 | 3,6,23–26 |
| Cryptococcal Antigen, latex agglutination | 93–99 % | 93–99 % | $4.83 3 | 27 |
| Cryptococcal Antigen, Lateral Flow Assay (LFA) | 99 % | 99 % | $2.50 | 28,29 |
AFB Ziehl-Neelsen stain for TB meningitis (TBM) estimate used in model 30% (95% CI: 10–50%) sensitivity.
GeneXpert cartridge cost is $9.98 with the $15 assay cost including shipping and estimated labor.
Cryptococcal Antigen, latex agglutination cost is ~$16 in Blantyre, Malawi and Kampala, Uganda.
The 2012 costs of diagnostic testing were obtained from the South African National Health Laboratory System (NHLS). The total cost included reagents, quality controls, disposable laboratory supplies, labor, external quality assurance testing, laboratory overhead, and a margin.30 We assumed an exchange rate of 1.00 US Dollar to 8.34 South African Rand (Jan 1, 2013). Each diagnostic testing strategy included the total cost of all tests performed within that strategy. The model focused on the diagnostics cost only, without inclusion of treatment or hospitalization costs which would vary substantially by country and diagnosis.
Analysis
The model outcome values were clinical effectiveness and expected cost. Clinical effectiveness was defined as the percentage of cases for which the algorithm result matched the true disease state (i.e. correct diagnosis). Average costs were based on the summation of all tests within a given strategy. The effectiveness of each strategy was determined by the weighted average cost of the summation of all of the pathways within the model.
To determine the relative benefit obtained for additional resources spent, we calculated the incremental cost effectiveness ratios (ICERs) to determine the incremental gains in percent correct diagnosis compared to the additional costs incurred.31
The number needed to test (NNT) to prevent one missed diagnosis (and the associated adverse effects and cost) was also calculated for each strategy. NNT is helpful for understanding the relative effectiveness of the strategies and was used to measure the amount of effort required to obtain a positive change in outcome among the various diagnostic tests. NNT was calculated by dividing one over the incremental percent correct diagnosis. The decision model was analyzed in TreeAge Pro, 2013 edition (Williamstown, MA).
Sensitivity Analysis
A one-way sensitivity analysis was conducted based on the prevalence of disease across all three countries to gain an increased understanding of the impact of varying disease prevalence rates have on the expected performance of the diagnostic algorithms. Due to the highly variable performance of TB diagnostics, a probabilistic sensitivity analysis (±10% SD) among TB diagnostics and disease prevalence ((95%CI) was performed.
Results
In Uganda, the current comprehensive strategy of ordering a full diagnostic work-up to correctly identify a CNS infection resulted in 93.3% probability of a correct diagnosis at an average cost of $32.00 per patient. The stepwise strategy resulted in 93.8% probability of a correct diagnosis at an average cost of $9.72 per patient (95% CI: $5.56–$34.85), and the minimalist strategy resulted in 91.1% correct diagnoses averaging $6.17 per patient (95% CI: $2.50–$19.68). If the minimalist strategy was implemented, nearly five additional patients could be diagnosed for the same cost as one patient using the comprehensive strategy, although the percent of those diagnosed correctly would decrease by 2.2%. If the stepwise strategy was implemented, an additional 3.3 patients could be diagnosed for the same cost as one patient using the comprehensive strategy, and the expected effectiveness would increase by 0.5% (Table 3).
Table 3.
Costs and Effectiveness by Diagnostic Strategy with Disease Prevalence in Uganda
| Diagnostic Strategy | Prevalence of Disease | % Correct Diagnosis | Cost per Person |
|---|---|---|---|
| MINIMALIST STRATEGY | - | 91.1% | $6.17 |
| Bacterial Meningitis | 4% | 70.0% | $9.50 |
| Tuberculosis Meningitis | 8% | 22.4% | $11.84 |
| Cryptococcal Meningitis | 59% | 99.0% | $2.53 |
| Other | 32% | 97.3% | $11.66 |
| STEPWISE STRATEGY | - | 93.8% | $9.72 |
| Bacterial Meningitis | 4% | 90.0% | $10.89 |
| Tuberculosis Meningitis | 8% | 51.5% | $22.75 |
| Cryptococcal Meningitis | 59% | 98.4% | $5.93 |
| Other | 32% | 96.7% | $13.70 |
| COMPREHENSIVE STRATEGY | - | 93.3% | $32.00 |
| Bacterial Meningitis | 4% | 99.0%* | $32.00 |
| Tuberculosis Meningitis | 8% | 30.0%* | $32.00 |
| Cryptococcal Meningitis | 59% | 99.0% | $32.00 |
| Other | 32% | 98.9% | $32.00 |
Assumption: testing performed prior to the administration of antibiotics with increasing diagnostic yield by inclusion of bacterial culture in the comprehensive approach as well as a large volume CSF collection >6mL for AFB stain.
Within each strategy, the number of correct diagnoses varied by true disease state, with TB meningitis having the lowest percent diagnosed correctly across all strategies (22–52%) in part due to the difficulty of diagnosis. In both the minimalist and stepwise strategies, the number of correct, confirmed diagnoses for bacterial meningitis were lower (70% and 90%, respectively); however, the comparison reflects an assumption of ideal testing characteristics with the lumbar puncture being performed prior to the administration of antibiotics. In reality, in many settings, antibiotics are given prior to performing the lumbar puncture, thus there is near zero additional diagnostic yield by bacterial CSF cultures after antibiotic administration.32–34
The percent of correctly diagnosed “other meningitis” disease was high across all strategies, which can be partially attributed to the high specificity values of bacterial meningitis, TBM, and CM diagnostic tests (≥99%). The high percentage of false negative “other disease” results occurred primarily among individuals with true bacterial or TB meningitis. This can be attributed to the lower sensitivities of the diagnostic tests used to identify bacterial or TB meningitis. 14–16
The relative incremental costs of the three diagnostic testing strategies were compared to the increase in diagnostic yield. When implementing the stepwise strategy compared to the minimalist strategy, the incremental cost increase was $3.55 per person with a 2.7% improvement in diagnostic effectiveness. The increase in diagnostic yield was primarily for TBM. When the Xpert MTB/RIF Assay (Cepheid, Sunnyvale, CA) was included in the stepwise strategy, using a theoretical 60% estimated sensitivity, the number of correctly diagnosed TBM persons increased substantially from 22% to an estimated 52%. The Xpert MTB/RIF assay would be the most expensive of the diagnostic tests evaluated (~$15 total assay cost using $9.98 cartridge cost + shipping + labor) and if included in the comprehensive strategy would increase cost to $47 per patient (with identical effectiveness). By using a stepwise approach, a Xpert MTB/RIF (or similar higher tech TB diagnostics) could be included in a targeted approach for lower overall cost, yet delivering more care, when needed.
When implementing the stepwise strategy, the number needed to test to accurately identify the disease state of one person through improved diagnostic testing was 37.5 persons with a cost per additional diagnosis being $133. When implementing the stepwise strategy instead of the comprehensive strategy, the incremental cost savings was $22.28 per patient, with an additional 0.5% increase in effectiveness by focusing additional resources for selective TB testing. Thus, the stepwise strategy dominated the comprehensive strategy (Table 4).
Table 4.
Incremental Cost Effectiveness of Strategies in Uganda
| Diagnostic Strategy | Cost per person (95% CI) | % Correct Diagnosis (95% CI) | Incremental % Correct Diagnosis | NNT | ICER |
|---|---|---|---|---|---|
| Minimalist Strategy | $6.17 ($2.50–19.68) | 91.1% (88.5–93.3%) | Ref | Ref | Ref |
| Stepwise Strategy | $9.72 ($5.56–34.85) | 93.8% (92.0–95.3%) | 2.7% | 37.5 | $133 |
| Comprehensive Strategy | $32.00 ($32–32) | 93.3% (90.8–95.7%) | 2.2% | 44.6 | $1,153 |
NNT = Number Needed to Test per additional correct diagnosis; ICER = Incremental Cost Effectiveness Ratio
Similar results were found when we used the prevalence rates from Malawi, South Africa, or Zimbabwe in that the minimalist approach had the lowest diagnostic yield and lowest expected cost; the stepwise had the highest diagnostic yield; and the comprehensive approach had highest expected cost per patient tested (Table 5).
Table 5.
Cost and Effectiveness by Diagnostic Strategy in Various Sub-Saharan Countries
| Diagnostic Strategy | Malawi Prevalence7 | South Africa Prevalence6 | Uganda Prevalence | Zimbabwe Prevalence8 | ||||
|---|---|---|---|---|---|---|---|---|
| % Correct Diagnosis | Average Cost | % Correct Diagnosis | Average Cost | % Correct Diagnosis | Average Cost | % Correct Diagnosis | Average Cost | |
| Minimalist | 79.8% | $7.33 | 82.8% | $8.54 | 91.1% | $6.17 | 84.8% | $7.29 |
| Stepwise | 88.4% | $11.34 | 90.1% | $12.01 | 93.8% | $9.72 | 91.0% | $10.89 |
| Comprehensive | 87.3% | $32.00 | 90.0% | $32.00 | 93.3% | $32.00 | 90.7% | $32.00 |
Note: The primary reason for the poor performance of the models is in the definitive diagnosis of TB meningitis.
Assuming a six-month survival rate of ~40% for bacterial, TB, and cryptococcal meningitis,2,35–38 the cost in diagnostics per life saved in Uganda for using algorithms compared to the minimalist strategy would be $333 plus treatment costs when utilizing the stepwise and $2,882 plus treatment costs for the comprehensive. Treatment costs vary by disease from $3 for meningococcal meningitis with 2g ceftriaxone intramuscularly once to $15 for five days of ceftriaxone for pneumococcal meningitis plus hospitalization cost.39 Amphotericin-based treatment of cryptococcal meningitis costs $218-$402 per WHO guidelines.2
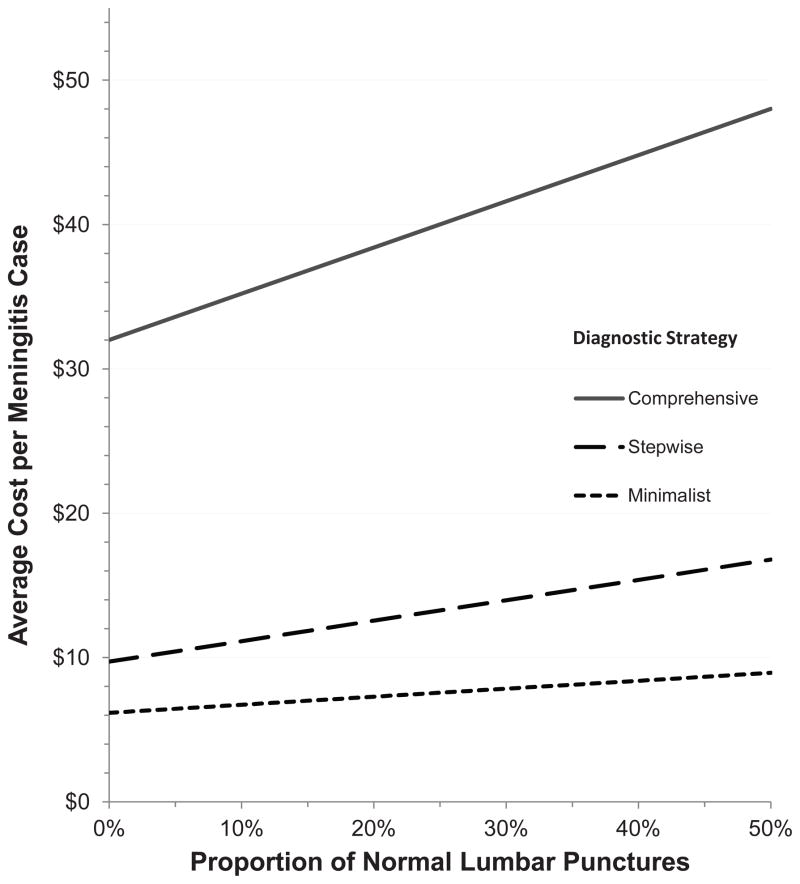
Not all initial clinically suspected meningitis cases will ultimately have meningitis infection. Based on local institutional medical practice as well as patient acceptance rates of lumbar punctures (LPs), the prevalence of negative diagnostic LPs may range up to 50% or more (i.e. persons receiving a diagnostic LP who do not have any meningitis).6,7,40 To examine the impact of the prevalence of non-meningitis individuals, we modeled the costs of LP diagnostics for these individual without meningitis within each diagnostic strategy. As the prevalence of persons without meningitis increased, the diagnostic testing costs increased such that when prevalence of no meningitis reached 50%, costs increased to $8.95 in the minimalist strategy, to $16.80 in the stepwise strategy, and to $48 in the comprehensive strategy per actual meningitis case (Figure1).
Figure 1.
Sensitivity analysis based on increasing proportions of lumbar punctures (LP) performed in persons with suspected meningitis, who do not have meningitis (i.e. negative LP). As the proportion of negative LPs increase, the cost per diagnostic evaluation changes differently for each regimen. For the comprehensive strategy, where every test is performed, there is a direct 1:1 linear increase in costs per each meningitis diagnosis. For the minimalist and stepwise strategies, the diagnostic algorithms stop after the first two and three tests are negative, respectively. Thus as the proportion of normal LPs approach 50%, the additional cost per meningitis diagnosis is $2.78, $7.08, and $16.00 for the minimalist, stepwise, and comprehensive strategies over the base model.
In the Ugandan setting, ceftriaxone was administered prior to lumbar puncture in 34% of 281 persons diagnosed with either CM or TBM (28% received >1 day, mean 4.9 ±3.3 days). This ineffective therapy ($2/day in 2012)41 accrued an estimated $936 in ceftriaxone expense, averaging $3.33 per person with CM or TB. Distributing this cost to the overall cohort resulted in an additional cost of $2.25 per person ($936/416).
Discussion
Our findings demonstrate the importance of evaluating the cost-effectiveness of diagnostic checklists and treatment algorithms, especially in resource limited settings. The preferred strategy is ultimately dependent on societal or a health system’s willingness (or ability) to pay for diagnostic certainty when identifying CNS infections. As the ability to pay varies across settings, understanding the health care system or the setting in which the algorithm or checklist will be implemented is essential to ensure long-term sustainability and maximal efficiency. Physicians have an ethical obligation to advocate for the highest yield testing, and formalizing a diagnostic algorithm can help achieve this as a health system’s intervention.
When identifying the ideal implementation strategy, it was important to understand that although the percentage of correctly diagnosed individuals improved as additional tests were performed, costs also rose. The clinical benefits were impacted by the sensitivity and specificity values of the diagnostic tests. The number of correctly diagnosed individuals among the bacterial, TB, and cryptococcal meningitis states was based primarily on test sensitivity whereas the “other” disease category was based primarily on the specificity of testing. Within each strategy, the diagnostic yield and costs did not substantially change with varying prevalence rates across the four sites; however, the overall cost-effectiveness of the strategy was significantly impacted when prevalence rates varied.
Depending on the weight that a clinician or health system places on diagnostic accuracy, the reduced proportion of correctly diagnosed individuals accompanied by decreased costs associated with the diagnostic tests eliminated from the algorithm, could result in substantial cost-savings. When evaluating the treatment algorithms, it is important to consider resource allocation. In the minimalist strategy, 91% of individuals were correctly diagnosed. Increasing the percentage of diagnostic certainty by 2.7% by using a stepwise algorithm increased the ratio of incremental costs to effectiveness by $133 per added diagnosis. In a resource-limited area, particularly when preemptive treatment is administered, the reduction in algorithm effectiveness may be acceptable in order to test and diagnose more of the population. Yet, simply reducing the number of diagnostic tests performed does not automatically equate to poor diagnostic efficacy if performed wisely. As can be seen through reducing the number of diagnostic tests in the comprehensive strategy to a stepwise strategy, this approach saved $22.28 per patient on average while also being able to add targeted TB testing, thereby increasing the overall effectiveness by 0.5%. By developing a stepwise algorithm based on a critical review of the literature and expert opinions, the number of missed diagnoses can be minimized and limited resources can be optimally allocated.
Understanding the impact disease prevalence and test characteristics have on treatment algorithms is crucial. When aggressively performing diagnostic LPs in populations in whom there is a high proportion of persons without meningitis (e.g. 50% negative LPs), the costs per patient can increase significantly (by $5.56 in the minimalist strategy, $14.15 in the stepwise strategy, and $32 in the comprehensive strategy) per non-meningitis patient. Furthermore, an algorithm with poor test sensitivity for diagnosis of a very common disease is not cost-effective. The prime example is India ink testing which has poor sensitivity (60–85%) for cryptococcosis, the most common etiology of meningitis in East and Southern Africa.26,42 India ink has particularly poor sensitivity for persons presenting early in cryptococcal disease course with low CSF fungal burdens. As a result, diagnoses are missed, additional diagnostic work up is pursued, and/or ineffective treatments are given, and lives are unnecessarily lost. This is true of any test with poor sensitivity when the pre-test probability is high.
Additionally, it is important to understand the standard medical practice in the setting in which the algorithm is being implemented. For meningitis, where the majority of suspect cases receive empiric ceftriaxone treatment prior to LP,3 the large number of theoretically missed BM cases, 30% in minimalist and 10% in stepwise, reduced the effectiveness of the respective algorithms compared to the comprehensive strategy. Yet in actual use among this 416 person cohort, bacterial CSF culture was less sensitive than Gram stain and did not detect any additional cases. One problem with empiric antibiotic treatment for all meningitis cases is that a minority of persons presenting with suspected meningitis (5–20%) in Sub-Saharan Africa outside of the meningitis-belt actually have bacterial meningitis. In South Africa, the reported cases nationwide of cryptococcal meningitis exceed all causes of bacterial meningitis combined.43 The cost of ceftriaxone therapy rapidly exceeds the cost of either minimalist or stepwise diagnostic testing algorithms, and unnecessary use may propagate antibiotic resistance. The new point-of-care cryptococcal antigen (CrAg) lateral flow assay (Immy, Norman, Oklahoma),28,29 and its low cost ($2.50 real world lab cost) should change “empiric” meningitis treatment to at least a minimalist diagnostic strategy of first testing for CrAg before empiric antibiotics in high HIV prevalence settings.
Furthermore, the current practice of creating an algorithm or checklists based solely on effectiveness, without considering cost, is unsustainable over the long-term, especially in resource-limited settings where extensive testing and treatment are often unavailable. For example, the cost of the current comprehensive algorithm of $32, which was designed to optimally diagnose one patient’s condition (excluding treatment and hospitalization costs) is greater than the per capita annual health expenditure of $24 in Uganda.44 The total operating budget for Mulago hospital was $17.20 per hospital bed per day in 2010. A further challenge is the necessary change in medical culture to shift individual physician ordering to a systems-based approach, trading autonomy for gains in efficacy. This culture shift to implement a lab-centric diagnostic testing approach may be a substantial challenge requiring well-written standard operating procedures (SOPs) as well as the ability to opt-out when warranted by physician judgment.
Limitations of the study design included assuming conditional independence of diagnostic tests and assuming that only one infectious etiology could occur at one time. In reality, multiple etiologies are possible, albeit uncommon (0.2% in Cape Town).6 Categorizing all non-diseased and other disease (i.e. aseptic viral meningitis) under one category overestimated the diagnostic certainty of the other disease state. While the “other meningitis” state has many potential etiologies, such diagnostic testing is typically unavailable in most resource-limited laboratories, as is specific treatment. However, the cost implications associated with negative diagnostic LPs were accounted for in the analysis with costs increasing as the proportion of normal diagnostic LPs increased. Another limitation was that sensitivity and specificity of diagnostic tests were obtained from the literature. In practice, testing performance may have significant variability dependent on laboratory quality assurance, staffing levels, and techniques (e.g. AFB stain). In addition, while the results of this analysis are most generalizable to populations with high HIV prevalence (e.g. East and Southern Africa), this concept of using disease prevalence and diagnostic testing performance should be generalizable. In other regions, local disease prevalence should guide the stepwise ordering of testing. Understanding regional disease prevalence is important for international guidelines. For example, WHO guidelines for standardized treatment of non-epidemic bacterial meningitis in Africa (written from a West African perspective only)39 are inappropriate in Eastern and Southern Africa by completely ignoring the diagnostic possibility of M. tuberculosis and Cryptococcus.
To our knowledge, no previous studies have investigated the cost-effectiveness of diagnostic algorithms in resource-limited settings. Our findings suggest that future research should be focused on performing cost-effectiveness analyses on diagnostic algorithms and checklists for additional disease states in order to inform policy on implementation of cost-effective treatment algorithms and outcomes. Use of diagnostic algorithms in high-income countries may also be warranted to increase cost-effectiveness of diagnostic testing, but this is as yet a foreign concept. Increasing the awareness of creating cost-effective treatment algorithms and checklists will not only improve the management of patient conditions but will also ensure their long-term sustainability in resource-constrained settings.
Supplementary Material
Acknowledgments
The authors thank support from National Institutes of Health (NS065713, AI073192, AI089244). We thank input from Dr. Graeme Meintjes; Dr. Neal Wetherall for laboratory support; and Drs. Henry Nabeta, Kabanda Taseera, Radha Rajasingham, and Abdu Musubire for care of patients with meningitis in Uganda. The abstract was presented at the 2011 American Society of Tropical Medicine and Hygiene annual meeting, December 7, 2011.
Footnotes
Conflicts of Interest: The authors have no conflict of interest.
References
- 1.Somand D, Meurer W. Central nervous system infections. Emerg Med Clin North Am. 2009;27(1):89–100. ix. doi: 10.1016/j.emc.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 2.Rajasingham R, Rolfes MA, Birkenkamp KE, Meya DB, Boulware DR. Cryptococcal meningitis treatment strategies in resource-limited settings: a cost-effectiveness analysis. PLoS Med. 2012;9(9):e1001316. doi: 10.1371/journal.pmed.1001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trachtenberg JD, Kambugu AD, McKellar M, et al. The medical management of central nervous system infections in Uganda and the potential impact of an algorithm-based approach to improve outcomes. Int J Infect Dis. 2007;11(6):524–530. doi: 10.1016/j.ijid.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 4.WHO. [Accessed 15 April 2012.];Towards Universal Access: Scaling up priority HIV/AIDS interventions in the health sector 2010. 2010 Available at: http://www.who.int/hiv/pub/2010progressreport/full_report_en.pdf.
- 5.Leligdowicz A, Katwere M, Piloya T, Ronald A, Kambugu A, Katabira E. Challenges in diagnosis, treatment and follow-up of patients presenting with central nervous system infections in a resource-limited setting. Mcgill J Med. 2006;9(1):39–48. [PMC free article] [PubMed] [Google Scholar]
- 6.Jarvis JN, Meintjes G, Williams A, Brown Y, Crede T, Harrison TS. Adult meningitis in a setting of high HIV and TB prevalence: findings from 4961 suspected cases. BMC Infect Dis. 2010;10:67. doi: 10.1186/1471-2334-10-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen DB, Zijlstra EE, Mukaka M, et al. Diagnosis of cryptococcal and tuberculous meningitis in a resource-limited African setting. Trop Med Int Health. 2010;15(8):910–917. doi: 10.1111/j.1365-3156.2010.02565.x. [DOI] [PubMed] [Google Scholar]
- 8.Hakim JG, Gangaidzo IT, Heyderman RS, et al. Impact of HIV infection on meningitis in Harare, Zimbabwe: a prospective study of 406 predominantly adult patients. AIDS. 2000;14(10):1401–1407. doi: 10.1097/00002030-200007070-00013. [DOI] [PubMed] [Google Scholar]
- 9.Wallach JB. Interpretation of diagnostic tests. 8. Philadelphia: Lippincott Wiliams & Wilkins; 2007. [Google Scholar]
- 10.Tunkel AR, Hartman BJ, Kaplan SL, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004;39(9):1267–1284. doi: 10.1086/425368. [DOI] [PubMed] [Google Scholar]
- 11.Geiseler PJ, Nelson KE, Levin S, Reddi KT, Moses VK. Community-acquired purulent meningitis: a review of 1,316 cases during the antibiotic era, 1954–1976. Rev Infect Dis. 1980;2(5):725–745. doi: 10.1093/clinids/2.5.725. [DOI] [PubMed] [Google Scholar]
- 12.Lindquist L, Linne T, Hansson LO, Kalin M, Axelsson G. Value of cerebrospinal fluid analysis in the differential diagnosis of meningitis: a study in 710 patients with suspected central nervous system infection. Eur J Clin Microbiol Infect Dis. 1988;7(3):374–380. doi: 10.1007/BF01962340. [DOI] [PubMed] [Google Scholar]
- 13.Dunbar SA, Eason RA, Musher DM, Clarridge JE., 3rd Microscopic examination and broth culture of cerebrospinal fluid in diagnosis of meningitis. J Clin Microbiol. 1998;36(6):1617–1620. doi: 10.1128/jcm.36.6.1617-1620.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schutte CM. Clinical, cerebrospinal fluid and pathological findings and outcomes in HIV-positive and HIV-negative patients with tuberculous meningitis. Infection. 2001;29(4):213–217. doi: 10.1007/s15010-001-1198-3. [DOI] [PubMed] [Google Scholar]
- 15.Karstaedt AS, Valtchanova S, Barriere R, Crewe-Brown HH. Tuberculous meningitis in South African urban adults. QJM. 1998;91(11):743–747. doi: 10.1093/qjmed/91.11.743. [DOI] [PubMed] [Google Scholar]
- 16.Torok ME, Chau TT, Mai PP, et al. Clinical and microbiological features of HIV-associated tuberculous meningitis in Vietnamese adults. PLoS One. 2008;3(3):e1772. doi: 10.1371/journal.pone.0001772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kennedy DH, Fallon RJ. Tuberculous meningitis. JAMA. 1979;241(3):264–268. [PubMed] [Google Scholar]
- 18.Caws M, Thwaites GE, Duy PM, et al. Molecular analysis of Mycobacterium tuberculosis causing multidrug-resistant tuberculosis meningitis. Int J Tuberc Lung Dis. 2007;11(2):202–208. [PubMed] [Google Scholar]
- 19.Thwaites GE, Chau TT, Stepniewska K, et al. Diagnosis of adult tuberculous meningitis by use of clinical and laboratory features. Lancet. 2002;360(9342):1287–1292. doi: 10.1016/s0140-6736(02)11318-3. [DOI] [PubMed] [Google Scholar]
- 20.Teo J, Jureen R, Chiang D, Chan D, Lin R. Comparison of two nucleic acid amplification assays, the Xpert MTB/RIF assay and the amplified Mycobacterium Tuberculosis Direct assay, for detection of Mycobacterium tuberculosis in respiratory and nonrespiratory specimens. J Clin Microbiol. 2011;49(10):3659–3662. doi: 10.1128/JCM.00211-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Causse M, Ruiz P, Gutierrez-Aroca JB, Casal M. Comparison of two molecular methods for rapid diagnosis of extrapulmonary tuberculosis. J Clin Microbiol. 2011;49(8):3065–3067. doi: 10.1128/JCM.00491-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hillemann D, Rusch-Gerdes S, Boehme C, Richter E. Rapid molecular detection of extrapulmonary tuberculosis by the automated GeneXpert MTB/RIF system. J Clin Microbiol. 2011;49(4):1202–1205. doi: 10.1128/JCM.02268-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scheld WM, Whitley RJ, Marra CM. Infections of the central nervous system. 3. Philadelphia: Lippincott Williams & Wilkins; 2004. [Google Scholar]
- 24.Saha DC, Xess I, Biswas A, Bhowmik DM, Padma MV. Detection of Cryptococcus by conventional, serological and molecular methods. J Med Microbiol. 2009;58(Pt 8):1098–1105. doi: 10.1099/jmm.0.007328-0. [DOI] [PubMed] [Google Scholar]
- 25.Jackson AT, Nussbaum JC, Phulusa J, et al. A phase II randomized controlled trial adding oral flucytosine to high-dose fluconazole, with short-course amphotericin B, for cryptococcal meningitis. AIDS. 2012;26(11):1363–1370. doi: 10.1097/QAD.0b013e328354b419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kisenge PR, Hawkins AT, Maro VP, et al. Low CD4 count plus coma predicts cryptococcal meningitis in Tanzania. BMC Infect Dis. 2007;7(1):39. doi: 10.1186/1471-2334-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perfect JR, Dismukes WE, Dromer F, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:291–322. doi: 10.1086/649858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rolfes MAR, Butler E, von Hohenberg M, et al. Evaluation of a novel point-of-care lateral flow assay to detect cryptococcal antigen in plasma and CSF. Abstract 953. CROI; 6 March 2012; Seattle. 2012. [Google Scholar]
- 29.Jarvis JN, Percival A, Bauman S, et al. Evaluation of a novel point-of-care cryptococcal antigen test on serum, plasma, and urine from patients with HIV-associated cryptococcal meningitis. Clin Infect Dis. 2011;53(10):1019–1023. doi: 10.1093/cid/cir613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meya DB, Manabe YC, Castelnuovo B, et al. Cost-effectiveness of serum cryptococcal antigen screening to prevent deaths among HIV-infected persons with a CD4+ cell count < or = 100 cells/microL who start HIV therapy in resource-limited settings. Clin Infect Dis. 2010;51(4):448–455. doi: 10.1086/655143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hunink MGM. Decision making in health and medicine : integrating evidence and values. Cambridge ; New York: Cambridge University Press; 2001. [Google Scholar]
- 32.Kanegaye JT, Soliemanzadeh P, Bradley JS. Lumbar puncture in pediatric bacterial meningitis: defining the time interval for recovery of cerebrospinal fluid pathogens after parenteral antibiotic pretreatment. Pediatrics. 2001;108(5):1169–1174. [PubMed] [Google Scholar]
- 33.Nigrovic LE, Malley R, Macias CG, et al. Effect of antibiotic pretreatment on cerebrospinal fluid profiles of children with bacterial meningitis. Pediatrics. 2008;122(4):726–730. doi: 10.1542/peds.2007-3275. [DOI] [PubMed] [Google Scholar]
- 34.del Rio MA, Chrane D, Shelton S, McCracken GH, Jr, Nelson JD. Ceftriaxone versus ampicillin and chloramphenicol for treatment of bacterial meningitis in children. Lancet. 1983;1(8336):1241–1244. doi: 10.1016/s0140-6736(83)92696-x. [DOI] [PubMed] [Google Scholar]
- 35.Heemskerk D, Day J, Chau TT, et al. Intensified treatment with high dose rifampicin and levofloxacin compared to standard treatment for adult patients with tuberculous meningitis (TBM-IT): protocol for a randomized controlled trial. Trials. 2011;12:25. doi: 10.1186/1745-6215-12-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS. 2009;23(4):525–530. doi: 10.1097/QAD.0b013e328322ffac. [DOI] [PubMed] [Google Scholar]
- 37.Scarborough M, Gordon SB, Whitty CJ, et al. Corticosteroids for bacterial meningitis in adults in sub-Saharan Africa. N Engl J Med. 2007;357(24):2441–2450. doi: 10.1056/NEJMoa065711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ajdukiewicz KM, Cartwright KE, Scarborough M, et al. Glycerol adjuvant therapy in adults with bacterial meningitis in a high HIV seroprevalence setting in Malawi: a double-blind, randomised controlled trial. Lancet Infect Dis. 2011;11(4):293–300. doi: 10.1016/S1473-3099(10)70317-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.WHO. WHO/CDS/EPR/2007.3. Geneva: WHO Press; 2007. Standardized treatment of bacterial meningitis in Africa in epidemic and non epidemic situations. http://www.who.int/csr/resources/publications/meningitis/WHO_CDS_EPR_2007_3/en/index.html. [Google Scholar]
- 40.Boulware DR, Bonham SC, Meya DB, et al. Paucity of initial cerebrospinal fluid inflammation in cryptococcal meningitis is associated with subsequent immune reconstitution inflammatory syndrome. J Infect Dis. 2010;202(6):962–970. doi: 10.1086/655785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Joint Medical Store. [Accessed May 31, 2012.];Product Catalogue. 2011 http://www.jms.co.ug/uploads/catalogue.pdf.
- 42.Kambugu A, Meya DB, Rhein J, et al. Outcomes of cryptococcal meningitis in Uganda before and after the availability of highly active antiretroviral therapy. Clin Infect Dis. 2008;46(11):1694–1701. doi: 10.1086/587667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.National Institute for Communicable Diseases. Group for Enteric, Respiratory and Meningeal disease Surveillance in South Africa. Govender N, Quan V, editors. [Accessed Jan 19, 2013.];GERMS-SA Annual Report 2011. 2011 http://www.nicd.ac.za/assets/files/2011%20GERMS-SA%20Annual%20report%20pub%20final.pdf.
- 44.WHO. [Accessed 15 April 2012.];World Health Statistics 2009: Table 7: Health expenditure. 2009 Available at: http://www.who.int/whosis/whostat/EN_WHS09_Table7.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.