Abstract
Background:
Deuk Laser Disc Repair® is a new full-endoscopic surgical procedure to repair symptomatic cervical disc disease.
Methods:
A prospective cohort of 66 consecutive patients underwent cervical Deuk Laser Disc Repair® for one (n = 21) or two adjacent (n = 45) symptomatic levels of cervical disc disease and were evaluated postoperatively for resolution of headache, neck pain, arm pain, and radicular symptoms. All patients were candidates for anterior cervical discectomy and fusion (ACDF) or arthroplasty. The Mann–Whitney Wilcoxon test was used to calculate P values.
Results:
All patients (n = 66) had significant improvement in preoperative symptoms with an average symptom resolution of 94.6%. Fifty percent (n = 33) had 100% resolution of all preoperative cervicogenic symptoms. Only 4.5% (n = 3) had less than 80% resolution of preoperative symptoms. Visual analog scale (VAS) significantly improved from 8.7 preoperatively to 0.5 postoperatively (P < 0.001) for the cohort. Average operative and recovery times were 57 and 52 minutes, respectively. There were no perioperative complications. Recurrent disc herniation occurred in one patient (1.5%). Average postoperative follow-up was 94 days and no significant intergroup difference in outcomes was observed (P = 0.111) in patients with <90 days (n = 52) or >90 days (n = 14, mean 319 days) follow-up. No significant difference in outcomes was observed (P = 0.774) for patients undergoing one or two level Deuk Laser Disc Repair®. Patients diagnosed with postoperative cervical facet syndrome did significantly worse (P < 0.001).
Conclusion:
Deuk Laser Disc Repair® is a safe and effective alternative to ACDF or arthroplasty for the treatment of one or two adjacent symptomatic cervical disc herniations with an overall success rate of 94.6%.
Keywords: Cervical radiculopathy, Deuk Laser Disc Repair, endoscopic spine surgery, intervertebral disc degeneration, intervertebral disc displacement, minimally invasive spine surgery
INTRODUCTION
Cervical disc diseases, including annular tears, disc bulges, contained and noncontained disc herniations, disc osteophyte complexes, degenerative disc disease, spondylosis, and stenosis are common and frequently symptomatic.[15,16,32,54] Symptoms of cervical disc disease include neck pain, arm pain, cervicogenic (originating from the cervical spine) headaches,[22,41,51] myelopathy, and radicular symptoms such as numbness, paresthesias, and weakness.[1,6,39,57] When conservative treatment modalities fail to provide adequate symptom relief in a timely fashion, surgery may be indicated.[4,8,17,23,24,26,47] The most common cervical disc surgery performed worldwide is anterior cervical discectomy and fusion (ACDF).[10,27,56] Cervical decompression and fusion is effective but has disadvantages including loss of segmental movement,[29,37] prolonged recovery, use of implants, high cost, significant risk of complications, an increased likelihood of adjacent segment disease, and inconsistent results with respect to symptom relief.[2,3,19,25,34,44,55,60] An alternative to fusion, cervical disc arthroplasty has demonstrated the potential to preserve segmental movement but shares many of the same risks as fusion,[31,36,48,49,58] in addition to heterotopic ossification, adjacent segment disease and failures.[7,38,45] Importantly, both fusion and arthroplasty require removal of the functional spinal disc. A less invasive surgical procedure that successfully treats the source of the patient's disc-related symptoms without removing the functional spinal disc could become a safe and effective alternative to cervical fusion or arthroplasty.
Deuk Laser Disc Repair® is a new minimally invasive, motion preserving, outpatient surgical procedure to endoscopically repair symptomatic cervical discs without fusion, implants, or biologics. The Deuk Laser Disc Repair® surgical technique has been previously described[11,12,13,14] and incorporates three distinct procedures including a selective partial discectomy, foraminoplasty, and annular debridement. Here we present the clinical outcomes of the first 66 consecutive patients with 1 or 2 adjacent symptomatic cervical disc(s) treated with Deuk Laser Disc Repair®.
MATERIALS AND METHODS
Patient characteristics
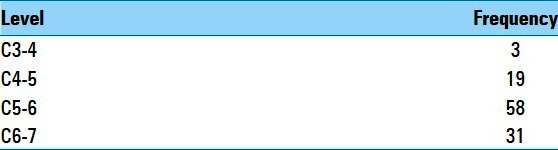
From 2008 to 2011, 66 consecutive patients meeting inclusion criteria with one (n = 21) or two (n = 45) adjacent symptomatic cervical disc(s) underwent surgical treatment with Deuk Laser Disc Repair® at their symptomatic level(s). Total number of cervical levels treated for the cohort was 111 or 1.7 levels per patient [Table 1]. All patients were included in a prospective cohort study with institutional review board approval to evaluate surgical outcomes. There were 40 female and 26 male patients aged 19-73 years (mean 40 years). All patients failed standard conservative treatment including therapy and pain management. The mean symptom duration prior to surgery for the cohort was 326 days.
Table 1.
Frequency of disc levels treated with cervical Deuk Laser Disc Repair®
Inclusion criteria
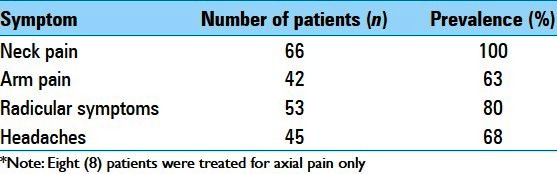
All patients aged 18 years or older undergoing Deuk Laser Disc Repair® with only one or two adjacent levels of symptomatic cervical disc disease that failed standard conservative treatments were included in this study. All patients had preoperative symptoms attributable to either one or two diseased cervical discs. Symptoms included one or more of the following: Neck pain, arm pain, cervicogenic headache, or upper extremity radicular symptoms [Table 2]. Eight patients with debilitating neck pain that failed conservative management underwent surgery for axial pain only without radicular symptoms. These patients either failed preoperative treatment for cervical facet pain or had a preoperative discogram confirming the presence of concordant discogenic pain with annular tear, which colocalized to the level(s) of disc pathology seen on preoperative magnetic resonance imaging (MRI). All patients treated in this study were candidates for ACDF and after a detailed discussion of the known potential risks and benefits of each procedure they opted for the cervical Deuk Laser Disc Repair®. Structural spinal disc abnormalities were identified preoperatively on standard MRI and/or postdiscogram computed tomography (CT) imaging. Treated symptomatic lesions included annular tears with both contained (bulging) and noncontained cervical disc herniations with or without osteophytes or foramenal stenosis seen on preoperative imaging. Patients with more than two symptomatic cervical disc herniations or inadequate follow-up were not included in this study.
Table 2.
Prevalence of preoperative symptoms in patients undergoing cervical Deuk Laser Disc Repair®
Outcome measures
Emphasis was placed on patient reported outcome measures including visual analog scale (VAS) and resolution of preoperative pain and radicular symptoms. Resolution of preoperative neck pain, arm pain, headache, and radicular symptoms for each patient treated was recorded by a medical assistant as a percentage from 0% to 100%. Operative time and recovery time were measured in minutes for each patient. Recovery time was the period from extubation to discharge home from the facility. Perioperative complications and recurrent disc herniation rates were measured for the cohort. The presence or absence of postoperative cervical facet syndrome was documented for comparative analysis with respect to outcome.
Statistical analysis
Due to the small group sample sizes and lack of data normality, nonparametric statistical methods were used. Specifically, the difference in group medians was estimated using Hodges–Lehmann methodology, while the distribution free confidence intervals (CIs) are based on Moses. The corresponding P values are based on the Mann–Whitney Wilcoxon test. Significant findings were defined by a P < 0.05.
Operative technique
All surgeries were performed by a single neurosurgeon with the patient under general endotracheal anesthesia. Patients were ASA class 1 or 2 and received appropriate preoperative medical clearance. The cervical Deuk Laser Disc Repair® technique has been described in a prior publication.[11] In brief, cervical Deuk Laser Disc Repair® is an anterior, full endoscopic, transdiscal, laser-assisted surgery during which a selective partial discectomy, foraminoplasty, and annular debridement are performed under direct visualization of the local anatomy [Figure 1]. The entire procedure is performed without the use of implants, biologics, or fusion.
Figure 1.
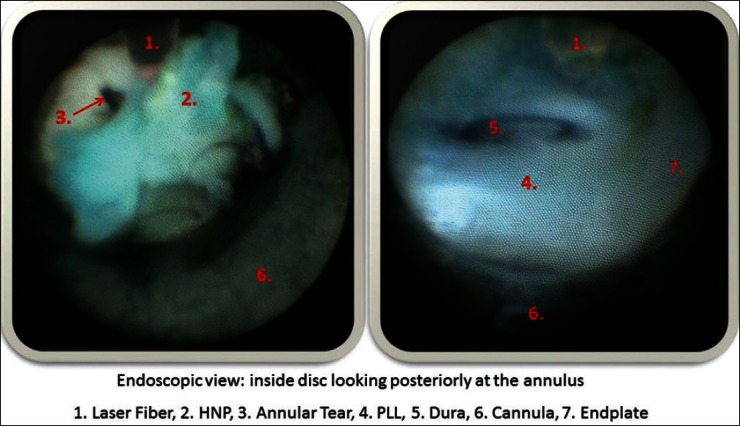
Cervical Deuk Laser Disc Repair® intraoperative endoscopic view demonstrating herniated disc fragments, annular tear, PLL and dura of the spinal cord-nerve root
RESULTS
Operative metrics
Mean operative time for the cohort was 57 minutes. Average operative blood loss was less than 5 ml. Average recovery time until discharge home was 52 minutes. There were no overnight stays.
Resolution of preoperative symptoms
All patients (n = 66) had significant improvement in their preoperative complaints including neck pain, headache, arm pain, and radicular symptoms (numbness, weakness, and paresthesias) [Figure 2]. Overall, the mean preoperative symptom resolution for the entire cohort was 94.6%. Fifty percent of the patients (n = 33) had 100% resolution of all preoperative symptoms. Only 4.5% of the patients (n = 3) had less than 80% resolution of all their preoperative symptoms. Eight patients with only axial pain achieved an average of 92.3% resolution of preoperative neck pain, including three patients with 100% resolution of pain.
Figure 2.
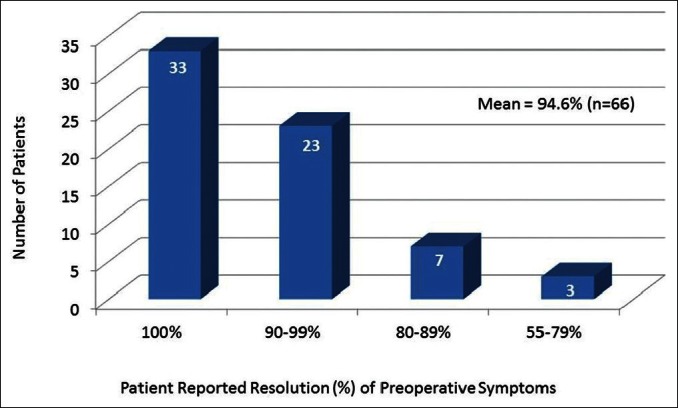
Patient reported resolution of preoperative symptoms. Average resolution of preoperative cervicogenic symptoms is 94.6%
Visual analog scale
[Figure 3] shows the improvement in VAS pain scores for the cohort after Deuk Laser Disc Repair®. Average preoperative VAS score for the cohort was 8.7. Average postoperative VAS for the cohort was 0.5. The difference is statistically significant (P < 0.001).
Figure 3.
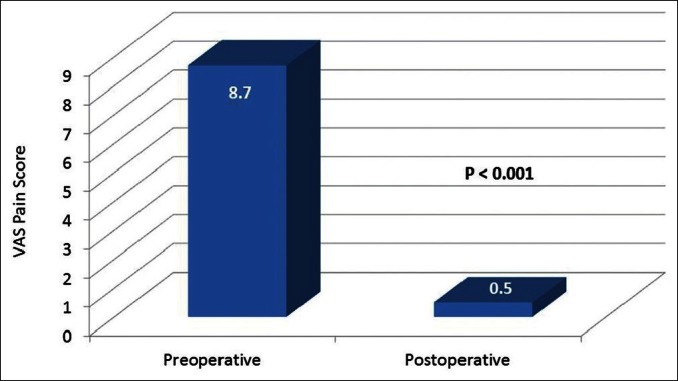
Pre- and postoperative VAS pain scores for patients that underwent cervical Deuk Laser Disc Repair®. (P< 0.001)
Perioperative complications
There were no perioperative complications in any of the patients that underwent Deuk Laser Disc Repair®. Specifically, the incidence of vascular injury, new neurological deficit or symptom, hoarseness, dysphagia, discitis, infection, hematoma, dural injury, nerve root or spinal cord injury, death, cardiovascular, or pulmonary complication was zero. There were neither hospital admissions nor emergency room visits during the 30 day postoperative period.
Recurrent disc herniation rate
Recurrent disc herniation occurred in one patient (1.5%). The patient initially underwent Deuk Laser Disc Repair® at the C5-6 and C6-7 levels with excellent relief of symptoms. He reherniated both the C5-6 and C6-7 discs 3 weeks after his initial surgery and his preoperative symptoms recurred. A second C5-6, C6-7 Deuk Laser Disc Repair® was performed 2 months after his original surgery with findings of recurrent herniations in the same locations as his original injury and the patient ultimately achieved 95% resolution of his preoperative symptoms.
Postoperative follow-up
Average postoperative follow-up for the entire group was just over 3 months. A comparative analysis of outcomes was performed between the subgroup of patients with greater than 90 days follow-up (mean 320 days, n = 14) versus those patients with less than 90 days follow-up (n = 52). No significant intergroup difference was observed with respect to resolution of preoperative symptoms (P = 0.111) [Figure 4]. No significant difference in outcomes was observed (P = 0.774) for patients undergoing one or two level Deuk Laser Disc Repair® [Figure 5].
Figure 4.
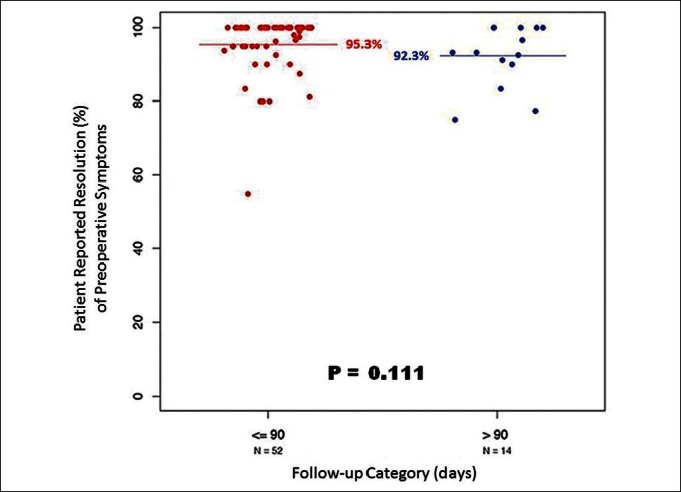
Scatter plot graph illustrates durability of cervical Deuk Laser Disc Repair® clinical outcomes over 1 year. No significant intergroup difference was observed. (P= 0.111)
Figure 5.
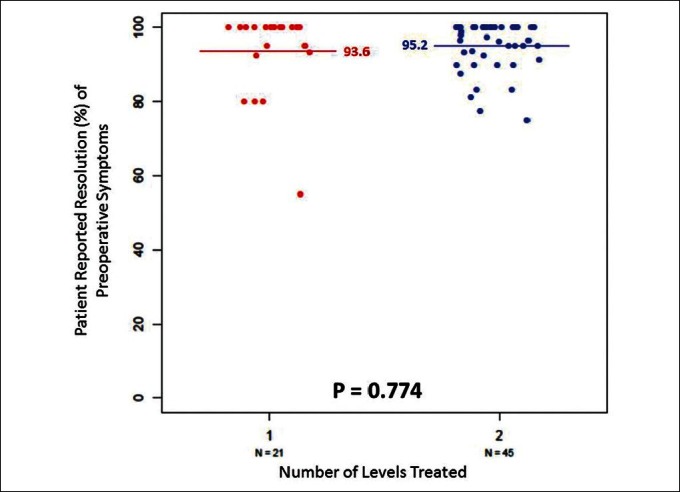
Scatter plot graph reveals no significant difference in clinical outcomes for patients undergoing one vs. two level surgery. (P = 0.774)
Cervical facet syndrome
Twelve patients in the cohort (12/66) were diagnosed with postoperative cervical facet syndrome. These patients were more likely to have residual symptoms related to the cervical spine after surgery. The mean resolution of preoperative symptoms in patients without postoperative cervical facet syndrome was 96.4%. In contrast, patients with postoperative cervical facet syndrome experienced only 86.8% resolution of their preoperative symptoms and the difference between the two groups was significant (P < 0.001) [Figure 6].
Figure 6.
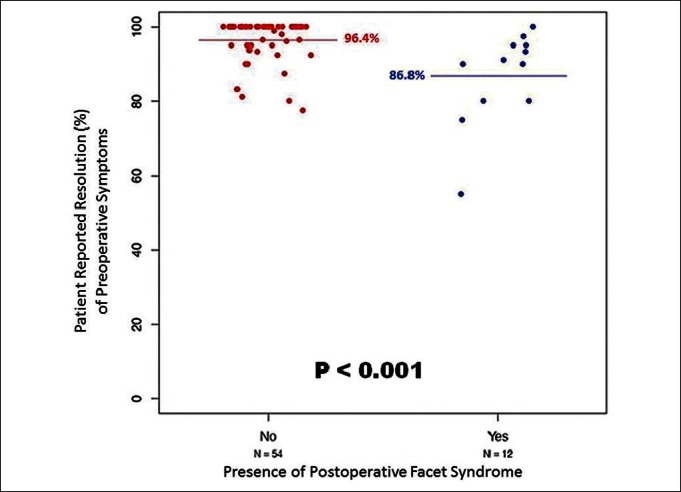
Scatter plot graph demonstrates that patients without postoperative cervical facet syndrome have significantly better clinical outcome with respect to preoperative symptom resolution. (P< 0.001)
DISCUSSION
ACDF is currently the most common surgical treatment for medically refractory symptomatic disc herniations involving one or two cervical segments.[10,27,59] The primary goal of surgery is to remove the herniated disc fragment(s) causing the patient's symptoms. To accomplish this through the anterior approach, the surgeon must remove the entire intervertebral disc to expose the offending posterior herniated disc fragment(s). The intervertebral disc provides natural load bearing support and stability to the anterior and middle spinal columns and helps maintain normal foramenal height and lordotic alignment of the motion segment. Removing the intervertebral disc to reach the herniated fragment(s) creates collateral damage including segmental instability and kyphosis. Reconstruction of the segment(s) with an interbody device-graft and stabilization with instrumented fusion or arthroplasty is necessary once the intervertebral disc is removed. A surgical procedure that preserves the intervertebral disc yet accomplishes removal of the herniated disc-osteophyte complex would maintain segmental stability and function. The concept of a selective minimal discectomy to treat symptoms of cervical disc disease is not “new” and was first described by Scoville (1981) with the posterior laminoforamenotomy-discectomy approach.[52] Though this procedure has been reported to be successful at treating radiculopathy, inherent disadvantages to his technique include limited access to only foramenal herniations precluding treatment of central and paracentral disc herniations; the technique requires removal of a substantial amount of the facet complex, which could result in destabilization of the motion segment; a more painful exposure as paraspinal muscles are divided to access the foramen; significantly greater blood loss; and other complications related to prone position surgery.
Deuk Laser Disc Repair® was developed as a “disc preserving” surgical procedure for removing symptomatic herniated disc fragments without creating segmental kyphosis or instability. This transdiscal endoscopic technique allows preservation of the intervertebral disc and natural, unrestricted segmental motion. Herniated disc fragments are removed under direct endoscopic visualization of the posterior disc anatomy including the annular tear, posterior ligament, foramen, spinal cord, and nerve root. This is accomplished without removing the intervertebral disc by working through a 4 mm transdiscal cannula. Because the intervertebral disc is preserved with Deuk Laser Disc Repair® no interbody device, instrumentation, or fusion is necessary. The average volume of herniated disc material removed with Deuk Laser Disc Repair® was only 0.09 cm3 or an estimated 5% of a normal disc volume.[8]
Patients undergoing cervical Deuk Laser Disc Repair® had average operative and recovery times that were 57 and 52 minutes, respectively (n = 66). Operative times for ACDF have been reported in the literature to be between 40 and 240 minutes and recovery times between 20 hours and 4 days according to a recent meta-analysis.[25,56] The average blood loss for Deuk Laser Disc Repair® was less than 5 ml per patient compared with 103.8 (range 25-200) ml for ACDF.[25,27,56] ACDF has known complications including hardware failure, pseudoarthrosis, dysphagia, infection, hematoma, CSF leak, recurrent laryngeal nerve palsy, esophageal injury, and death. A recent meta-analysis of 1015 ACDF procedures demonstrated a morbidity and mortality rate of 19.3% and 0.1%, respectively.[19] Shorter operative and recovery times and reduced blood loss could result in fewer perioperative complications, lower cost of care, early return to normal activities and work, and higher patient satisfaction. In this study, there were no postoperative complications. The safety of Deuk Laser Disc Repair® is well established.[11]
The patients in this study underwent cervical Deuk Laser Disc Repair® to treat preoperative symptoms determined to be caused by one or two adjacent spinal discs. Two spinal discs were included in the treatment plan when preoperative imaging demonstrated adjacent disc pathology that correlated clinically (exam, discography, and EMG/NCS) to the patient's axial or lateralized symptoms.[5,33] The cohort achieved on average 94.6% resolution of preoperative neck and arm pain, headaches, and radicular symptoms. The average VAS pain score improved from 8.7 preoperatively to below 1 postoperatively and the change was significant (P < 0.001). One half of all treated patients (n = 33) achieved 100% resolution of all preoperative symptoms and the worst outcome was one patient with 55% resolution of their preoperative symptoms. Overall, 96% of the patients treated with cervical Deuk Laser Disc Repair® achieved 80% or higher resolution of preoperative symptoms. Patients diagnosed with “facet syndrome” in the postoperative period had significantly less resolution of preoperative symptoms (86.8%) compared with patients without this diagnosis (96.4%) (P < 0.001). Cervical Facet Syndrome is neck pain and stiffness originating from one or more inflamed zygapophyseal joints.[16,18,30] The condition is common and the clinical diagnosis is verified by medial branch block as patients will experience an immediate improvement in pain with neck rotation and extension.
Surgery was offered to eight patients with only axial pain that had failed preoperative treatments including therapy, facet injections, and epidural steroid injections. All eight of these patients had significant axial neck pain that colocalized on physical examination and/or evocative discography[30,35,56] with 1 or 2 level disc disease seen on MRI. In our view, current medical literature supports both the existence of pain originating from a diseased spinal disc (discogenic pain) as well as the use of surgery on a symptomatic spinal disc to treat neck pain when non-operative modalities fail.[8,21,43,53] In our experience, the selective use of evocative discography with postdiscogram CT in the setting of medically refractory neck pain in patients with no other significant structural abnormalities seen on MRI except for disc disease has proven an extremely effective tool for determining which patients would benefit from surgery on the symptomatic disc(s). “Discogenic pain” has been previously described by Wiberg (1949) through in vivo experiments and his results verified by Cloward (1960).[9] We believe that “discogenic pain” originates from sensitized nascent nerve fibers located in the posterior annulus surrounding symptomatic annular tears. These nerve fibers originate from branches of the sinuvertebral nerve and their growth into the posterior annulus is most likely induced by inflammatory cytokines concentrated around the symptomatic annular tear.[20,40,42,50] The Deuk Laser Disc Repair® procedure directly visualizes and addresses these painful areas of the annulus with the laser assisted debridement step of the surgery.[11]
In this study, most patients had one or two postoperative follow up visits and were discharged from care because they were doing so well. The average follow up for the entire cohort was 3 months. The authors wanted to know if the clinical effect of surgery was lost over time. An analysis of the durability of the clinical effect of Deuk Laser Disc Repair® on preoperative symptoms was performed by stratifying the entire cohort into two subgroups: Short (less than 90 days) or long-term follow up. The short-term follow up subgroup achieved 95.3% resolution of preoperative symptoms. The long-term follow up subgroup achieved a similar effect of 92.5% resolution of preoperative symptoms with a mean follow up period of 320 days. The difference in outcomes between the two subgroups was not significant (P = 0.111). Other studies have reported similar results with respect to the durability of the surgical effect for endoscopic cervical discectomy.[28,46]
In conclusion, this study has demonstrated that Deuk Laser Disc Repair® is a safe and effective treatment option for one or two adjacent level(s) of symptomatic cervical disc disease. There have been no complications to date and the surgery may be performed safely in the outpatient setting. In this study, the patients reported 94.6% resolution of their preoperative symptoms related to cervical disc disease including both contained and noncontained disc bulges and herniations, spondylosis, degenerative disc disease, stenosis, and radiculopathy. All of the patients in this study were successfully treated without fusion or spinal implants.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2013/4/1/68/112610
Disclaimer: The authors of this article have no conflicts of interest to disclose, and have adhered to SNI's policies regarding human/animal rights, and informed consent. Advertisers in SNI did not ask for, nor did they receive access to this article prior to publication
Contributor Information
Ara J. Deukmedjian, Email: deukmedjian@gmail.com.
S. T. Jason Cutright, Email: jcutright@deukspine.com.
PA-C Augusto Cianciabella, Email: acianciabella@deukspine.com.
Arias Deukmedjian, Email: adeukmedjian@deukspine.com.
REFERENCES
- 1.Baptiste DC, Fehlings MG. Pathophysiology of cervical myelopathy. Spine J. 2006;6(6 Suppl):190–7S. doi: 10.1016/j.spinee.2006.04.024. [DOI] [PubMed] [Google Scholar]
- 2.Bolesta MJ, Rechetine GR, 2nd, Chrin AM. One and two level anterior cervical discectomy and fusion: The effect of plate fixation. Spine J. 2002;2:197–203. doi: 10.1016/s1529-9430(02)00186-9. [DOI] [PubMed] [Google Scholar]
- 3.Bolesta MJ, Rechetine GR, 2nd, Chrin AM. Three and four level anterior cervical discectomy and fusion with plate fixation: A prospective study. Spine (Phila Pa 1976) 2000;25:2040–6. doi: 10.1097/00007632-200008150-00007. [DOI] [PubMed] [Google Scholar]
- 4.Braddom RL, Buschbacher RM, Dumitru D. Physical medicine and rehabilitation. 2nd ed. Philadelphia, Pa: WB Saunders; 2000. pp. 426–9. [Google Scholar]
- 5.Cardozo MJ, Rosner MK. Multilevel cervical arthoplasty with artificial disc replacement. Neurosurg Focus. 2010;28:E19. doi: 10.3171/2010.1.FOCUS1031. [DOI] [PubMed] [Google Scholar]
- 6.Carette S, Fehlings MG. Clinical practice. Cervical radiculopathy. N Engl J Med. 2005;353:392–9. doi: 10.1056/NEJMcp043887. [DOI] [PubMed] [Google Scholar]
- 7.Cho SK, Riew KD. Adjacent segment disease following cervical spine surgery. J Am Acad Orthop Surg. 2013;21:3–11. doi: 10.5435/JAAOS-21-01-3. [DOI] [PubMed] [Google Scholar]
- 8.Cicala RS, Thoni K, Angel JJ. Long-term results of cervical epidural steroid injections. Clin J Pain. 1989;5:143–5. doi: 10.1097/00002508-198906000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Cloward RB. The clinical significance of the sinu-vertebral nerve of the cervical spine in relation to the cervical disk syndrome. J Neurol Neurosurg Psychiatry. 1960;23:321–6. doi: 10.1136/jnnp.23.4.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Denaro V, Di Martino A. Cervical spine surgery: An historical perspective. Clin Orthop Relat Res. 2011;469:639–48. doi: 10.1007/s11999-010-1752-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deukmedjian AJ, Cianciabella A, Cutright J, Deukmedjian A. Cervical Deuk laser disc repair: A novel, full-endoscopic surgical technique for the treatment of symptomatic cervical disc disease. Surg Neurol Int. 2012;3:142. doi: 10.4103/2152-7806.103884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deukmedjian AJ, Cianciabella AJ, Cutright JM. Deuk Laser Disc Repair® is an effective treatment for arm pain from cervical disc herniation. AANS. 2012 Annual Meeting, published abstract #22463. [Google Scholar]
- 13.Deukmedjian AJ, Cianciabella AJ, Cutright JM. Deuk Laser Disc Repair® is an effective treatment for neck pain from cervical disc herniation. AANS. 2012 Annual Meeting, published abstract #22468. [Google Scholar]
- 14.Deukmedjian AJ, Cianciabella AJ, Cutright JM. Deuk Laser Disc Repair® is an effective treatment for radicular symptoms from cervical disc herniation. AANS. 2012 Annual Meeting, published abstract #22469. [Google Scholar]
- 15.Ernst CW, Stadnick TW, Peeters E, Breucq C, Osteaux MJ. Cervical Spine in Symptom free Volunteers. Eur J Radiol. 2005;55:409–14. doi: 10.1016/j.ejrad.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Fei Z, Fan C, Ngo S, Xu J, Wang J. Dynamic evaluation of cervical disc herniation using kinetic MRI. J Clin Neurosci. 2011;18:232–6. doi: 10.1016/j.jocn.2010.04.035. [DOI] [PubMed] [Google Scholar]
- 17.Ferrante FM, Wilson SP, Iacobo C, Orav EJ, Rocco AG, Lipson S. Clinical classification as a predictor of therapeutic outcome after cervical epidural steroid injection. Spine (Phila Pa 1976) 1993;18:730–6. doi: 10.1097/00007632-199305000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Falco FJ, Datta S, Manchikanti L, Sehgal N, Geffert S, Singh V, et al. An updated review of the diagnostic utility of cervical facet joint injections. Pain Physicain. 2012;15:E807–38. [PubMed] [Google Scholar]
- 19.Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 2007;32:2310–7. doi: 10.1097/BRS.0b013e318154c57e. [DOI] [PubMed] [Google Scholar]
- 20.Fujimoto K, Miyagi M, Ishikawa T, Inoue G, Eguchi Y, Kamoda H, et al. Sensory and autonomic innervation of the cervical interverteboral disc in rats: The pathomechanics of chronic discogenic neck pain. Spine (Phila Pa 1976) 2012;37:1357–62. doi: 10.1097/BRS.0b013e31824ba710. [DOI] [PubMed] [Google Scholar]
- 21.Gangi A, Tsoumakidou G, buy X, Cabral JF, Garnon J. Percutaneous techniques for cervical pain of discal origin. Semin Musculoskelet Radiol. 2011;15:172–80. doi: 10.1055/s-0031-1275601. [DOI] [PubMed] [Google Scholar]
- 22.Haldeman S, Dagenais S. Cervicogenic headaches: A critical review. Spine J. 2001;1:31–46. doi: 10.1016/s1529-9430(01)00024-9. [DOI] [PubMed] [Google Scholar]
- 23.Heckmann JG, Lang CJ, Zöbelein I, Laumer R, Druschky A, Neundörfer B. Herniated cervical intervertebral discs with radiculopathy: An outcome study of conservatively or surgically treated patients. J Spinal Disord. 1999;12:396–401. [PubMed] [Google Scholar]
- 24.Herzog J. Use of cervical spine manipulation under anesthesia for management of cervical disk herniation, cervical radiculopathy, and associated cervicogenic headache syndrome. J Manipulative Physiol Ther. 1999;22:166–70. doi: 10.1016/S0161-4754(99)70131-4. [DOI] [PubMed] [Google Scholar]
- 25.Joo YH, Lee JW, Kwon KY, Rhee JJ, Lee HK. Comparison of fusion with cage alone and plate instrumentation in two-level cervical degenerative disease. J Korean Neurosurg Soc. 2010;48:342–6. doi: 10.3340/jkns.2010.48.4.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Judovich BD. Herniated cervical disc: A new form of traction therapy. Am J Surg. 1952;84:646–56. doi: 10.1016/0002-9610(52)90127-x. [DOI] [PubMed] [Google Scholar]
- 27.Korinth MC. Treatment of cervical degenerative disc disesase-current status and trends. Zentralbl Neurochir. 2008;69:113–24. doi: 10.1055/s-2008-1081201. [DOI] [PubMed] [Google Scholar]
- 28.Lee SH, Ahn Y, Choi WC, Bhanot A, Shin SW. Immediate pain improvement is a useful predictor of long-term favorable outcome after percutaneous laser disc decompression for cervical disc herniation. Photomed Laser Surg. 2006;24:508–13. doi: 10.1089/pho.2006.24.508. [DOI] [PubMed] [Google Scholar]
- 29.Lin HL, Cho DY, Liu YF, Lee WY, Lee HC, Chen CC. Change of cervical balance following single to multi-level interbody fusion with cage. Br J Neurosurg. 2008;22:758–63. doi: 10.1080/02688690802379134. [DOI] [PubMed] [Google Scholar]
- 30.Manchikanti L, Dunbar EE, Wargo BW, Shah RV, Derby R, Cohen SP. Systematic review of cervical discography as a diagnostic test for chronic spinal pain. Pain Physician. 2009;12:305–21. [PubMed] [Google Scholar]
- 31.McAfee PC, Reach C, Gilder K, Eisermann L, Cunningham B. A meta-analysis of comparative outcomes following arthroplasty or anterior cervical fusion: Results from four prospective multi-center randomized clinical trials and up to 1226 patients. Spine (Phila Pa 1976) 2012;37:943–52. doi: 10.1097/BRS.0b013e31823da169. [DOI] [PubMed] [Google Scholar]
- 32.Miyazaki M, Hong SW, Yoon SH, Morishita Y, Wang JC. Reliability of a magnetic resonance imaging-based grading system for cervical intervertebral disc degeneration. J Spinal Disord Tech. 2008;21:288–92. doi: 10.1097/BSD.0b013e31813c0e59. [DOI] [PubMed] [Google Scholar]
- 33.Moon HJ, Kim JH, Kim HJ, Kwon TH, Chung HS, Park YK. The effects of anterior cervical discectomy and fusion with stand-alone cages at two contiguous levels on cervical alignment and outcomes. Acta Neurochir (Wien) 2011;153:559–65. doi: 10.1007/s00701-010-0879-z. [DOI] [PubMed] [Google Scholar]
- 34.Morpeth JF, Williams ME. Vocal fold paralysis after anterior cervical diskectomy and fusion. Laryngoscope. 2000;110:43–6. doi: 10.1097/00005537-200001000-00009. [DOI] [PubMed] [Google Scholar]
- 35.Motimaya A, Arici M, George D, Ramsby G. Diagnostic value of cervical discography in the management of cervical discogenic pain. Conn Med. 2000:64395–8. [PubMed] [Google Scholar]
- 36.Mummaneni PV, Amin BY, Wu JC, Brodt ED, Dettori JR, Sasso RC. Cervical artificial disc replacement versus fusion in the cervical spine: A systematic review comparing long-term follow-up results from two FDA trials. Evid Based Spine Care J. 2012;3:59–66. doi: 10.1055/s-0031-1298610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nabhan A, Ahlhelm F, Pitzen T, Steudel WI, Jung J, Shariat K, et al. Disc replacement using Pro-Disc C versus Fusion: A prospective randomized and controlled radiographic and clinical study. Eur Spine J. 2007;16:423–30. doi: 10.1007/s00586-006-0226-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nunley PD, Jawahar A, Cavanauugh DA, Gordon CR, Kerr EJ, 3rd, Utter PA. Symtomatic adjacent segment disease after cervical total disc replacement: Re-examining the clinical and radiological evidence with established criteria. Spine J. 2013;13:5–12. doi: 10.1016/j.spinee.2012.11.032. [DOI] [PubMed] [Google Scholar]
- 39.Radhakrishnan K, Litchy WJ, O’Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994;117:325–35. doi: 10.1093/brain/117.2.325. [DOI] [PubMed] [Google Scholar]
- 40.Raj PP. Intervertebral disc: Anatomy-physiology-pathophysiology-treatment. Pain Pract. 2008;8:18–44. doi: 10.1111/j.1533-2500.2007.00171.x. [DOI] [PubMed] [Google Scholar]
- 41.Rana MV. Managing and treating headache of cervicogenic origin. Med Clin North Am. 2013;97:267–80. doi: 10.1016/j.mcna.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 42.Rennie C, Haffajee MR, Ebrahim MA. The sinuvertebral nerves at the craniovertebral junction. A microdissection study. Clin Anat. 2013;26:357–66. doi: 10.1002/ca.22105. [DOI] [PubMed] [Google Scholar]
- 43.Riew KD, Ecker E, Dettori JR. Anterior cervical discectomy and fusion for the management of axial neck pain in the absence of radiculopathy or myelopathy. Evid Based Spine Care J. 2010;1:45–50. doi: 10.1055/s-0030-1267067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rihn JA, Kane J, Albert TJ, Vaccaro AR, Hilibrrand AS. What is the incidence and severity of dysphagia after anterior cervical surgery.? Clin Orthop Relat Res. 2011;469:658–65. doi: 10.1007/s11999-010-1731-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rhin JA, Lawrence J, Gates C, Harris E, Hilibrand AS. Adjacent segment disease after cervical spine fusion. Instr Course Lect. 2009;58:747–56. [PubMed] [Google Scholar]
- 46.Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic anterior decompression versus conventional anterior decompression and fusion in cervical disc herniations. Int Orthop. 2009;33:1677–82. doi: 10.1007/s00264-008-0684-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Saal JS, Saal JA, Yurth EF. Nonoperative management of herniated cervical intervertebral disc with radiculopathy. Spine. 1996;21:1877–83. doi: 10.1097/00007632-199608150-00008. [DOI] [PubMed] [Google Scholar]
- 48.Salari B, McAfee PC. Cervical total disk replacement: Complications and avoidance. Orthop Clin North Am. 2012;43:97–107. doi: 10.1016/j.ocl.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 49.Sasso RC, Smucker JD, Hacker RJ, Heller JG. Artificial disc versus fusion: A prospective, randomized study with 2-year follow-up on 99 patients. Spine. 2007;32:2933–40. doi: 10.1097/BRS.0b013e31815d0034. [DOI] [PubMed] [Google Scholar]
- 50.Schoeder M, Viezens L, Schaefer C, Friedrichs B, Algenstaedt P, Rutner W, et al. Chemokine profile of disc degeneration with acute or chronic pain laboratory investigation. J Neurosurg Spine. 2013 Mar 8; doi: 10.3171/2013.1.SPINE12483. [In Press] [DOI] [PubMed] [Google Scholar]
- 51.Schofferman J, Garges K, Goldthwaite N, Koestler M, Libby E. Upper cervical anterior diskectomy and fusion improves discogenic cercical headaches. Spine (Phila Pa 1976) 2002;27:2240–4. doi: 10.1097/00007632-200210150-00011. [DOI] [PubMed] [Google Scholar]
- 52.Scoville WB. Crevical disc: Classifications, indication and approaches with special reference to posterior keyhole operation. In: Dunsker, editor. Cervical Spondylosis. New York: Raven Press; 1981. pp. 155–67. [Google Scholar]
- 53.Senter BS. Cervical discogenic syndrome: A cause of chonic head and neck pain. J Miss State Med Assoc. 1995;36:231–4. [PubMed] [Google Scholar]
- 54.Shedid D, Benzel EC. Cervical spondylosis anatomy: Pathophysiology and biomechanics. Neurosurgery. 2007;60(1 Suppl 1):S7–13. doi: 10.1227/01.NEU.0000215430.86569.C4. [DOI] [PubMed] [Google Scholar]
- 55.Shen FH, Samartzis D, Khanna N, Goldberg EJ, An HS. Comparison of clinical and radiographic outcome in instrumented anterior cervical discectomy and fusion with or without direct uncovertebral joint decompression. Spine J. 2004;4:629–35. doi: 10.1016/j.spinee.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 56.Siebenrock KA, Aebi M. Crevical discography in discogenic pain syndrome and its predictive value for cervical fusion. Arch Orthop Trauma Surg. 1994;113:199–203. doi: 10.1007/BF00441832. [DOI] [PubMed] [Google Scholar]
- 57.Tanaka Y, Kokubun S, Sato T, Ozawa H. Cervical roots as origin of pain in the neck or scapular regions. Spine. 2006;31:E568–73. doi: 10.1097/01.brs.0000229261.02816.48. [DOI] [PubMed] [Google Scholar]
- 58.Tu TH, Wu JC, Fay LY, Ko CC, Huang WC, Cheng H. Vertebral body spilt fracture a single-level cervical total disc replacement. J Neurosurg Spine. 2012:16231–5. doi: 10.3171/2011.11.SPINE11210. [DOI] [PubMed] [Google Scholar]
- 59.Villavicencio AT, Pushchak E, Burneikiene S, Thramann JJ. The safety of instrumented outpatient anterior cervical discectomy and fusion. Spine J. 2007;7:148–53. doi: 10.1016/j.spinee.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 60.Wright IP, Eisenstein SM. Anterior cervical discectomy and fusion without instrumentation. Spine (Phila Pa 1976) 2007;32:722–5. doi: 10.1097/01.brs.0000258846.86537.ad. [DOI] [PubMed] [Google Scholar]


