Abstract
Background:
Keeping in view of rapid industrialization and growing Indian economy, there has been a substantial increase in the workforce in India. Currently there is no organized workplace model for promoting health of industrial workers in India.
Objective:
To develop and implement a healthy workplace model in three industrial settings of North India.
Materials and Methods:
An operations research was conducted for 12 months in purposively selected three industries of Chandigarh. In phase I, a multi-stakeholder workshop was conducted to finalize the components and tools for the healthy workplace model. NCD risk factors were assessed in 947 employees in these three industries. In phase II, the healthy workplace model was implemented on pilot basis for a period of 12 months in these three industries to finalize the model.
Findings:
Healthy workplace committee with involvement of representatives of management, labor union and research organization was formed in three industries. Various tools like comprehensive and rapid healthy workplace assessment forms, NCD work-lite format for risk factors surveillance and monitoring and evaluation format were developed. The prevalence of tobacco use, ever alcoholics was found to be 17.8% and 47%, respectively. Around one-third (28%) of employees complained of back pain in the past 12 months. Healthy workplace model with focus on three key components (physical environment, psychosocial work environment, and promoting healthy habits) was developed, implemented on pilot basis, and finalized based on experience in participating industries. A stepwise approach for model with a core, expanded, and optional components were also suggested. An accreditation system is also required for promoting healthy workplace program.
Conclusion:
Integrated healthy workplace model is feasible, could be implemented in industrial setting in northern India and needs to be pilot tested in other parts of the country.
Keywords: Experience from industry, health promotion, healthy workplace
INTRODUCTION
The workplace is increasingly being used as a setting for health promotion and preventive health activities; not only to prevent occupational injury, but to assess and improve worker′s overall health.[1,2] Globally, two million people die each year as a result of occupational accidents and work-related illnesses or injuries.[3] Another 268 million non-fatal workplace accidents result in an average of three lost workdays per casualty, as well as 160 million new cases of work-related illness each year.[4] Additionally, 8% of the global burden of disease from depression is currently attributed to occupational risks.[5] The total working population of India, in 2001, stood at 402.5 million, out of which 37.1% are cultivators and agricultural laborers.[6]
Indian industrial workers had reported a high prevalence of risk factors and morbidity due to non-communicable diseases. A study in 10 Indian industrial settings among the employees and their family members has shown overall prevalence of most NCD risk factors to be high; with 50.9% of men and 51.9% of women being overweight, central obesity was observed among 30.9% of men and 32.8% of women, and 40.2% of men and 14.9% of women reported current tobacco use.[7] Another study by Confederation of Indian Industry (CII) revealed that the 11.6% employees had unhealthy habits of consuming tobacco and alcohol for more than 5 years. About 46% of the respondents in the service sector with stress had diabetes, 39% heart problems and 49% had a history of high blood pressure, and 31% showed symptoms of COPD. Women (52.4%) have higher levels of stress than men (40.1%).[8]
Focusing on healthy workplaces will have several advantages like development of a healthy and productive workforce, which is vital to a nation′s economic and social growth, offers the ideal setting for introducing health promotion programs, acknowledges the non-occupational factors that can influence workers′ health, encourages interaction with families and communities, and protects the general environment and supports sustainable development. However, there is no organized health promotion program in industrial settings in India. There is a need for developing an integrated healthy workplace model in India for promotion and prevention of health problems in industrial setting. The objective of this project was to develop a healthy workplace model and observe the feasibility of implementing this model in three industries of Chandigarh, India.
MATERIALS AND METHODS
An operations research was undertaken in three industries from 2008 to 2009 in union territory of Chandigarh, the capital of Haryana and Punjab. Three industries were selected after obtaining consent from the top management. A team of experts from PGIMER School of Public health, Chandigarh, visited the decision makers/human resource managers of three industries to sensitize and emphasize the importance of healthy workplace. Healthy workplace committees were formed in each industry with participation from human resource managers, labor unions, health staff, and representatives from PGIMER, Chandigarh. Healthy workplace model was worked out based on review of existing literature and consultation with participating industries. It was finalized during a multi-stakeholder consultative workshop involving representatives from key industrial chambers, participating industries, labor unions, faculty from PGIMER and health department, Chandigarh Administration. Primary role of PGIMER, Chandigarh, was to provide technical assistance for this project, assisting in formulation of work plan, baseline assessment of risk factors and documentation of all activities. The healthy workplace committee met every month to decide the plan of action to be undertaken each month. Situation analysis was conducted in three industries to assess the prevailing situation regarding health promotion activities and service provision for employees already suffering from different diseases. Baseline assessment of NCD risk factor assessment was also carried out in these industries with trained research assistants. Standard definition as per WHO protocol of tobacco use, alcohol use, and hypertension was used for risk assessment.[9] Various tools (comprehensive and rapid situational analysis tools, NCD work-lite for NCD risk factors surveillance, monitoring tools) were developed. These tools were pilot tested in a different industry. Risk profile of 947 randomly selected employees was conducted using the NCD work-lite performa by trained research assistants initially and later on by industry staff, which is the pruned and locally adapted version of the standardized WHO NCD STEPS questionnaire.[9] The employees participating in risk profiling were from taken from randomly selected units and all were included in selected unit. The management and health staffs of the industries were also oriented regarding the concept of risk assessment and health promotion. The total duration of the project was 18 months. At the end of pilot intervention period, various parameters like written policy for physical activity promotion, smoking, alcohol, safety of physical environment, and capacity building activities were evaluated and were compared with baseline situation analysis to see the effect of intervention. The evaluation of inputs and process was done using a questionnaire as well as observation.
RESULTS
Various industries located in and around Chandigarh were contacted. Three industries who gave consent to participate were included in the study. One public sector electronic industry (with 1100 employees) and two private corporate sectors (manufacturing industry with 550 employees and an IT industry with 1000 employees, respectively) were included in the study. Sensitization of top management for benefit of such program and selection of the industries was completed in the month of May 2008.
Situation analysis
Comprehensive and rapid situational analysis proformas were used for baseline evaluation of health promotion initiatives at the industries. The comprehensive performa covers all key components for healthy workplace and took long time for completion. Pilot testing of tools showed that time is a critical factor in industrial settings as it affects their productivity, so rapid tools are required for overall assessment and risk profiling. So, keeping in view this observation, a rapid assessment tools was developed which took approximately an hour for completion. Similarly pruned version of WHO STEPS approach for NCD risk factor surveillance was used industry were finding difficult to spare their employees for half an hour. It was observed that in three industries, a full-time Medical Officer/Psychologist with outdoor facility was available. Various eye check-up camps, general health camps for employees were held from time to time. Policies on no smoking and alcohol during the official hours and premises were also found to be present in these three industries.
Risk profiling
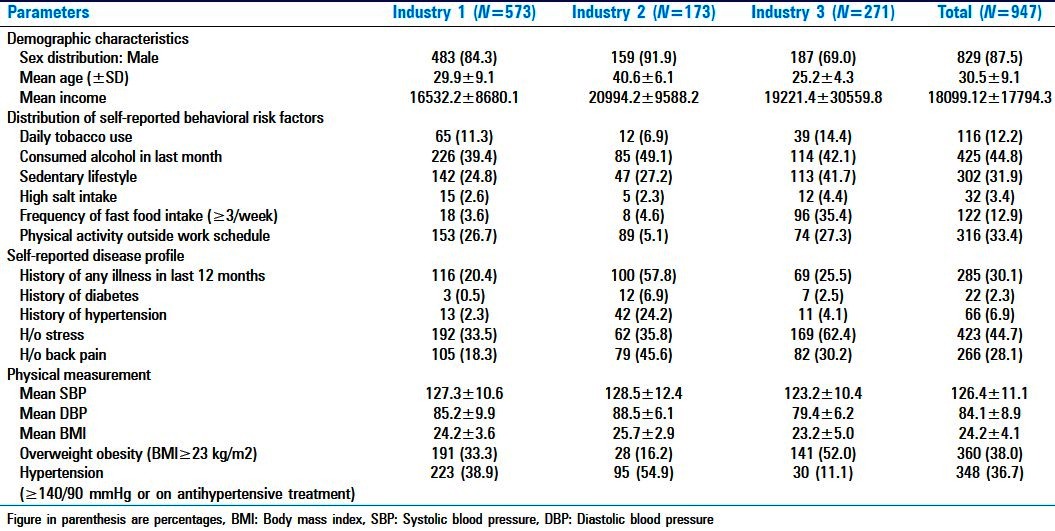
Risk assessment was carried out with a one page instrument called ′NCD Work Lite′ which is a pruned version of WHO STEPS approach for NCD risk factor surveillance. The results of the risk distribution among the workers in three industries are given in Table 1. More than one-third (36.7%) and around two-fifth (38%) of the workers were found to be hypertensives and obese during baseline assessment. Stress was observed to be a common risk factor (45%) and was very high in IT and BPO industry (62%). About one-third (28%) of employees reported to suffer from backache during the survey.
Table 1.
Distribution of risk factors in the three north Indian industries, 2008-09
Formation of healthy workplace committee and healthy workplace model
Each industry was requested to constitute a healthy workplace committee by involving key stakeholders like top management, human resource manager, and representative of labor unions. Various action plans were laid out through a consultative process through the healthy workplace committee. Healthy workplace model was developed by review of literature and was discussed in healthy workplace committees of participating industries. The model was further discussed and finalized in a stakeholder workshop including industry chamber, labor unions, health department, and academic institutions before being implemented. After piloting in participating industries, it was further modified and finalized. The healthy work place model is given in Figures 1 and 2. Healthy workplace model focused on improvement in physical work environment, promoting healthy practices, and psychosocial work environment. Physical work environment aims at improving the quality of work environment. The following points were emphasized; workplace hygiene, safety and cleanliness in facility, availability of healthy canteen with healthier options of food with proper hygiene, proper lighting, ventilation and provision of gymnasium or fitness centers on campus. In promoting healthy practices among employees, healthy diets, physical activity, hygiene, substance abuse, tobacco and alcohol cessation, information on safer sex, access to health services, yoga, and relaxation techniques were emphasized. Psychosocial work environment is third key component which examines organizational culture with emphasis on stress management, employee recognition, supportive workforce, and staff involvement in decision-making.
Figure 1.
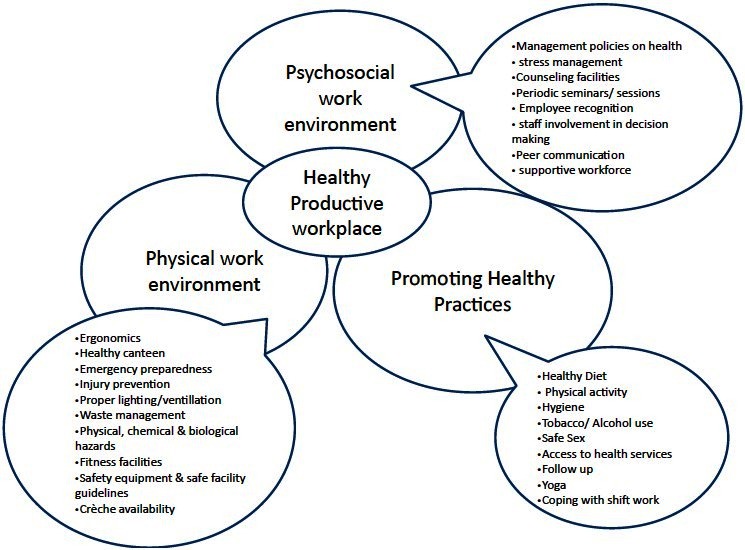
Model for healthy workplace in industrial setting in northern India
Figure 2.
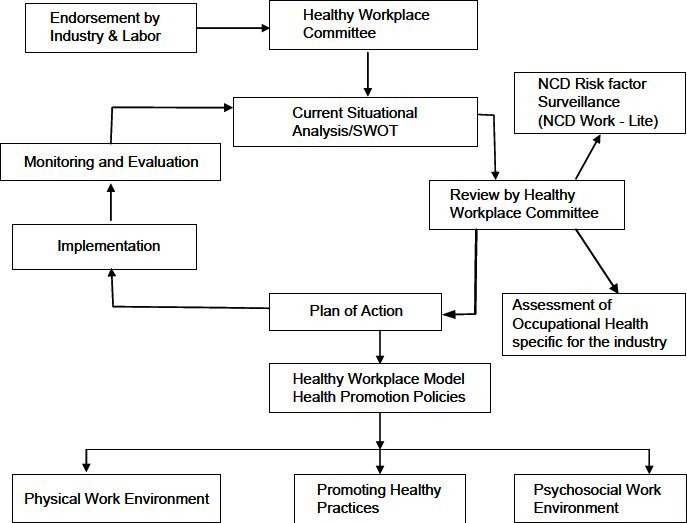
Framework for developing a healthy workplace
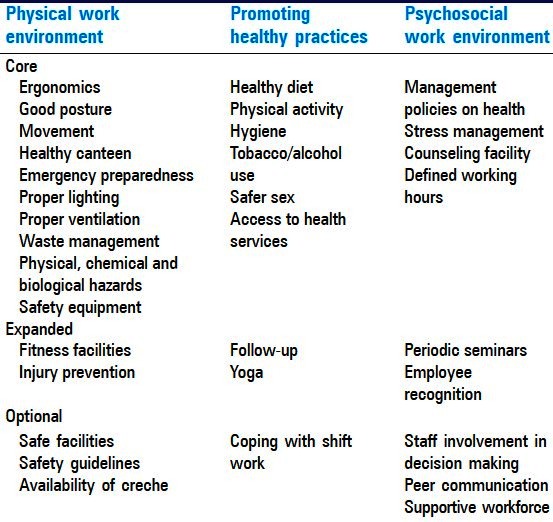
India is a mixed economy has public as well private sectors. Depending upon the availability of resources a stepwise approach is proposed having core, expanded and optional component was discussed with participating industries, in a workshop of stakeholders and is given in Table 2.
Table 2.
Stepwise approach for a healthy workplace in industry setting
Implementation of intervention
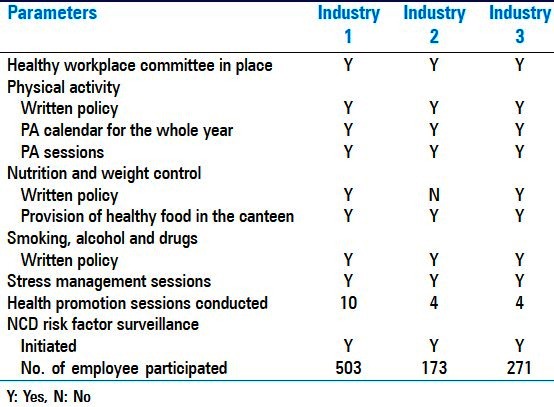
The healthy workplace model was implemented on pilot basis in the participating industries by the management of industries with supervision from healthy workplace committee and technical support from investigators. Operational problems like time constraints, effect on production, conflict in production, and human resource wing were identified, discussed in healthy workplace committee and solved with help of management. A comprehensive health promotion program focusing on healthy diet, physical activity, avoidance of tobacco and alcohol, stress, posture, personal hygiene and safety, safe water, and sex was implemented. Based on the experience, tools and integrated healthy workplace model were modified and finalized. The progress of intervention of healthy workplace program in participating industries is given in Table 3. Participating industries could set up healthy workplace committees, developed written policy for key risk factors, organized health promotion sessions, and initiated risk factor surveillance during a period of 1 year. Workplace committees met regularly every month, discussed operational issues and problems, took up difficult issues with top management, introduced healthier food options in canteens, and took practical steps for promoting physical activity and healthy life style. It also facilitated consensus and team building.
Table 3.
Progress of implementation of healthy workplace model in the participating industries, 2008-09
DISCUSSION
India is one of the fastest growing economies in world and undergoing rapid industrialization and development. There has been less attention paid to the health and needs of the employees in various sectors of the Indian industries. There is no existing healthy workplace model in India despite having a big working population of about 402.51 million workers and 622.74 million non-workers. Workers constitute 39.3% of India′s population as against 37.5% in 1991 census. There is no adequate OHS legislation for workers in this sector.[10]
Western countries like Canada and UK were the first to initiate healthy workplace models.[11–15] Since the needs and requirement of the healthy workforce in developed countries is different from the Indian healthy workforce, these existing models may not be applicable in Indian setting. So an effort was made to develop a healthy workplace model keeping in view Indian industrial situation, which may be suitable to other developing countries.
With the initial using of standard WHO STEPS questionnaire, a loss of productivity was observed resulting in conflict between production and administrative units, so a modified version of WHO′s STEPS performa was developed i.e., NCD- Work Lite questionnaire both in English and Hindi version. The version was self-administered after completion of shift and took 5–10 minutes. It helped to analyze the various health problems faced by the employees working in industries. Monitoring and evaluation tool was developed, which helped to assess progress of the implementation of healthy workplace program. It also helped in identifying what are the needs of the employee and whether the initiatives taken up are meeting the identified goals and what improvements are needed.
Every industry has its own set of requirements which differs from industry to industry. Therefore, a single model may not be suitable for a country like India. It was observed that public sector industry was slow in implementation as compared to corporate industries. The decision making was also slow in public sector industry and they did not want to implement complete program in one go. So it was decided to have a stepwise approach for developing healthy workplace with core, expanded, and optional components. Core component is mandatory to each and every industry irrespective of its type and can be implemented at the available resources of the company without much investment. It also include mandatory regulatory requirement under the Factory Act and other legislations. Depending upon the available resources, expanded, and optional components could be implemented in the industrial settings. We found that healthy workplace committee is the critical component in implementing the healthy workplace model and steering the industries activities toward achieving the desired goal as it acts as catalyst for innovative changes and promoting enabling environment. Industries needed motivation for considering such committee as initially they were reluctant. There were regular monthly meeting in participating industries where progress as well as operational problems were discussed. Calendar of activities, health check-up, and education sessions during the months were also finalized. It helped in empowering the industries and sustaining the program. Various local medical colleges can play an active role in functioning of healthy workplace committee in industries near their field practice areas.
At completion of project, all three industries decided to continue this program with their own resources. Once convinced of effect on productivity of healthy workforce, industries can become drivers for change as demonstrated by one of the participating industry (III) which had decided to upscale this experience globally to their 30,000 employees working in India and abroad. An independent nodal agency with involvement of ministries of industry, labor, and health with other stakeholders is required for the implementation of healthy workplace programs at National, state and district level. Mechanism of National Rural Health Mission (NRHM) and proposed National Urban Health Mission can be used for such program at state and district level. District Health Mission can implement such program through District Industry Centre, industry chambers and labor organization. There is also a need to develop an accreditation system for healthy workplaces with participation from industry. Quality Council of India (QCI) along with Industry chambers and professional associations should work out such program to run it on voluntary basis.
We started with focus on non-communicable diseases but it was observed that industries wanted a comprehensive program in a holistic way covering health promotion, communicable as well as non-communicable diseases. Therefore, an integrated model is required in developing countries like India which should cover communicable and non-communicable diseases. Experiences from western countries have proved that implementation of such healthy workplace models is beneficial to the society on whole and help to improve productivity, employee retention, and satisfaction, reduce absenteeism and medical reimbursement bills, and the dietary and lifestyle habits in industrial populations. Since three industries were selected based on their willingness to participate and giving representation to different type of industries, so there may be some element of selection bias. It can be concluded that a healthy workplace model with a stepwise approach is feasible and could be implemented in North Indian industry. It can be further pilot tested in other part of the country.
ACKNOWLEDGMENTS
We are really thankful to the participating industries to become a partner in this project and implementing the model on pilot basis. We are also thankful to WHO, India country office in general and Dr. Cherian Verghese, Cluster Focal point, NMH for providing financial and technical support. We are also thankful to Confederation of Indian Industry (CII), Northern regional and Central office for facilitating in organizing the stakeholder workshop.
Footnotes
Source of Support: Government of India-WHO India collaborative programme 2007-08
Conflict of Interest: None declared.
REFERENCES
- 1.World Health Organization 2010. Healthy workplaces: A model for action: For employers, workers, policymakers and practitioners. [Last accessed on 2010 Jun 15]. Available From: http://www.whoindia.org/LinkFiles/NMH_Resources_Healthy_Workplaces_a_model_for_action.pdf .
- 2.The Bangkok Charter for Health promotion in a globalized world. [Last accessed on 2010 Jun 15]. Available From: http://www.who.int/healthpromotion/conferences/6gchp/hpr_050829_%20BCHP.pdf .
- 3.International Labour Organization. Facts on safety at work. 2005. Apr, [Last accessed on 2010 Jul 15]. Available From: http://www.ilo.org/wcmsp5/groups/public/dgreports/dcomm/documents/publication/wcms_067574.pdf .
- 4.Number of work-related accidents and illnesses continues to increase: ILO and WHO join in call for prevention strategies. International Labour Organisation/World Health Organisation Joint Press Release; 28 April 2005. [Google Scholar]
- 5.Prüss-Ustün A, Corvalan C. Preventing disease through health environments: Towards an estimate of the environmental burden of disease. Geneva: World Health Organisation; 2006. [Google Scholar]
- 6.Census of India. 2001. [Last accessed on 2010 Jul 1]. Available From: http://censusindia.gov.in/
- 7.Reddy KS, Prabhakaran D, Chaturvedi V, Jeemon P, Thankappan KR, Ramakrishan L, et al. Methods for establishing a surveillance system for cardiovascular diseases in Indian industrial populations. Bull World Health Organ. 2006;84:461–9. doi: 10.2471/blt.05.027037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahuja R. Healthy workplace in corporate sector, India. Confederation of Indian Industry, Feb 2007. [Last accessed on 2010 Jul 1]. Available From: http://whoindia.org/EN/Section20/Section29_1414.htm .
- 9.The World Health Organisation stepwise approach to surveillance of noncommunicable diseases. [Last accessed on 2010 Jul 15]. Available http://www.searo.who.int/LinkFiles/Regional_Tobacco_Surveillance_System_SI_risk.pdf .
- 10.Chaudhuri RN. Occupational health problems among agriculture and plantation workers. J Indian Med Assoc. 2000;98:439–45. [PubMed] [Google Scholar]
- 11.National Quality Institute. The Canadian Healthy Workplace Criteria. Toronto: National Quality Institute; 1998. [Last accessed on 2010 Jul 15]. Available from http://nqi.ca . [Google Scholar]
- 12.Leka S, Cox T, Griffiths A. Workplace health promotion at Nottingham: A systems approach. Glob Occup Health Network. 2003;5 [Google Scholar]
- 13.Robson L. Healthy Workplace Scorecard. Institute for Work and Health Internal Plenary session. 2003 Mar 4; [Google Scholar]
- 14.Burton J. Creating Healthy Workplaces-Industrial Accident Prevention Association. 2004. [Last accessed on 2010 Jul 15]. Available http://www.iapa.ca/pdf/2004_HWP_Healthy_Workplace_FINAL.pdf .
- 15.Health Canada, Corporate Health Model: A Guide to Developing and Implementing the Workplace Health System in Medium and Large Businesses. Health Canada, Catalogue No H39-225/1991. [Last accessed on 2010 Jul 15]. Available From: http://www.hc-sc.gc.ca ISBN 0-662-19112-9 .


