Abstract
Thyroid hormone (TH) is known to have many beneficial effects on vital organs, but its extrapolation to be used therapeutically has been restricted by the fact that it does have concurrent adverse effects. Recent finding of various thyroid hormone receptors (TR) isoforms and their differential pattern of tissue distribution has regained interest in possible use of TH analogues in therapeutics. These findings were followed by search of compounds with isoform-specific or tissue-specific action on TR. Studying the structure–activity relationship of TR led to the development of compounds like GC1 and KB141, which preferentially act on the β1 isoform of TR. More recently, eprotirome was developed and has been studied in humans. It has shown to be effective in dyslipidemia by the lipid-lowering action of TH in the liver and also in obesity. Another compound, 3,5-diiodothyropropionic acid (DITPA), binds to both α- and β-type TRs with relatively low affinity and has been shown to be effective in heart failure (HF). In postinfarction models of HF and in a pilot clinical study, DITPA increased cardiac performance without affecting the heart rate. TR antagonists like NH3 can be used in thyrotoxicosis and cardiac arrhythmias. However, further larger clinical trials on some of these promising compounds and development of newer compounds with increased selectivity is required to achieve higher precision of action and avoid adverse effects seen with TH.
Keywords: 3, 5-diiodothyropropionic acid, eprotirome, GC-1, hypolipidemic, selective thyroid hormone receptor modulators, thyroid analogue
INTRODUCTION
For years, it is known that thyroid hormones (THs) have some actions that might be useful therapeutically, but at the same time their unwanted deleterious effects restricted their use for their beneficial effects. Potential therapeutically useful actions include those to induce weight loss and lower plasma cholesterol levels. Potential deleterious actions are those on the heart to induce tachycardia and arrhythmia, on bone to decrease mineral density causing osteoporosis and on muscle to induce wasting.[1] THs are currently used only as replacement therapy for patients with hypothyroidism, characterized by low circulating levels of endogenous hormone. All these actions are mediated by nuclear thyroid receptors (TRs). However, genetic evidence suggests that different isoforms of TR exist in different tissues and contribute to individual TH effects. This regained interest in use of TH therapeutically. Soon, it was realised that TH analogues, either tissue-selective or isoform-specific, could potentially be used to treat a large number of conditions, avoiding the unwanted side-effects of TH. This led to the development of isoform-specific TH analogues with their interesting properties. Clinical trials are still awaited, however, to verify whether these potentially promising agents will indeed prove to be of clinical therapeutic value.[2] This review summarizes recent advances in understanding the actions of TRs and some selective thyroid hormone receptor modulators and their therapeutic implications.
THYROID HORMONE RECEPTOR AND ITS BIOLOGICAL ROLE
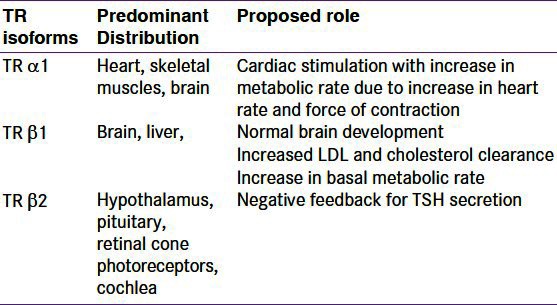
The TR belongs to the family of nuclear receptors that comprise a class of intracellular, mostly ligand-regulated, transcription factors.[3,4,5] Fundamental genes in the intestinal, skeletal and cardiac muscles and the liver and the central nervous system are regulated by THs, and influence metabolic rate, lipid levels, heart rate and mood.[6,7] There are two major subtypes of the TRs, α (TR α) and β (TR β), expressed from two different genes. Differential ribonucleic acid (RNA) processing results in the formation of several isoforms from each gene.[8] The TR α1, TR β1 and TR β2 isoforms bind THs and act as ligand-regulated transcription factors. Their predominant distribution and role is depicted in Table 1. Several other several isoforms like TR α2, TR α3, TR Δα1, TR Δα2 etc. have been found to be unable to bind any ligand. The TR β1 isoform is prevalent especially in the liver and, to a lower degree, in the heart. The TR β1 variant is the predominant systemic form, while the pituitary form is predominantly TR β2. The TR α1 isoform is also widely distributed, although its levels are generally lower than those of the TR β1 isoform. The literature suggests that most of the effects of THs on heart, particularly on heart rate and rhythm, are mediated through activation of the TRα1 isoform, while most of the actions of the hormones on the liver (e.g., lipid-lowering) and other tissues are mediated through activation of the TR β1 isoform.[9,10,11,12]
Table 1.
Thyroid receptor isoforms, location and functions
TR β SELECTIVE AGONISTS AND THEIR THERAPEUTIC IMPLICATIONS
The risk of atherosclerotic cardiovascular disease and increased low-density lipoprotein (LDL) cholesterol level is well known.[13] Statins are the current mainstay of treatment for hyperlipidemia. However, the efficacy of statins is limited,[14] and improvements for the treatment of hyperlipidemia are still desirable. Furthermore, statins are less-effective in lowering levels of other lipoproteins, such as triglycerides[15] and Lp(a) lipoprotein,[16] which are associated with the risk of atherosclerotic vascular disease. Recent reports have indicated that new drugs such as ezetimibe and torcetrapib, which have novel mechanisms of action, either have not shown an incremental reduction of secondary end points in atherosclerotic disease, such as carotid intima-media thickness,[17,18] or have had unanticipated adverse effects.
In patients on statin alone, who are unable to achieve the desired therapeutic goal of lipid control or develop intolerable side-effects, need addition of other hypolipidemic drugs to achieve improved cardiovascular outcome.[19,20]
It is known that TRs regulate body weight, adiposity and cholesterol levels. Long back in 1930, the cholesterol-lowering effect of TH in patients with hypothyroidism was described.[21] LDL is the principal lipoprotein that is reduced. This reduction is caused by increased hepatic clearance[22] due to increased expression of the hepatic LDL-receptor gene.[23,24,25] In rodents, thyromimetic compounds also accelerate clearance of cholesterol by the liver by increasing the high-density lipoprotein (HDL) receptor called scavenger receptor B1(SR-B1),[26] increasing the activity of cholesterol 7α-hydroxylase,[25,27] and increasing fecal excretion of cholesterol and bile acids.[27] Previous attempts to mimic these actions with TH metabolites[28,29] and analogues[27,30,31,32] have confirmed their cholesterol-lowering properties.
The burden of obesity and metabolic syndrome is increasing dramatically, and it is one of the major risk factors for cardiovascular diseases. Today, only limited treatment options for obesity are available, and most strategies are focused on appetite suppression.[33] Multiplestudies have demonstrated the ability of excess TH treatment to cause more weight loss than that which can be achieved by dieting alone. However, once the excess TH is stopped and the excess weight loss is usually regained.[34] One of the actions for weight loss of TH is by causing uncoupling of oxidative phosporylation in brown adipose tissue for which TR β is predominantly responsible, while both TR α and TR β are essential for synergism between TH and adrenergic signals for lipolysis.[35] These properties of TH can be used for the treatment of obesity, but, unfortunately, they cause large changes in metabolic rate and direct cardiac acceleration due to the TR α action on heart, making it unacceptable for treatment.
As discussed earlier, TR α regulates heart rate while TR β regulates lipid levels, which implies that drugs that target TR β or exhibit tissue-selective uptake may improve plasma lipid levels while sparing the heart.
NOVEL THYROID HORMONE ANALOGUES
kb-141
A recent structure–activity relationship has revealed several TR β selective thyromimetics such as KB-141. The reason for its TR β1 selectivity is most probable the difference in the single amino acid in the ligand-binding pocket. In studies of cholesterol-fed rats, KB-141 increased metabolic rate with a 10-fold selectivity and lowered cholesterol with a 27-fold selectivity as compared with tachycardia.[8] In primates, KB-141 caused significant cholesterol, Lp(a) and body weight reduction after 1 week of treatment, without tachycardia or cardiac hypertrophy, unlike TH (T3).[32] This data suggests that selective TR β agonists may represent a novel class of drugs for the treatment of obesity, hypercholesterolemia and elevated Lp(a), which may make them useful therapeutics for patients with metabolic syndrome.
GC1 [3,5-dimethyl-4-(4-hydroy-3-isopropylbenzyl)-phenoxy acetic acid]
Another thyroid analogue called GC-1 (sobetirome)] exhibited TR β1 selectivity in the range of seven to 18–times,[36,37] and a cellular transcription assay of the compounds was also performed that showed more than 10-fold preference for TR β1 in transactivation.[36] Its selective tissue uptake may also play a role in its TR β1 selectivity.[38]
Experiments on euthyroid mice to observe the effect of TH on cholesterol and triglyceride metabolism have shown that GC-1 treatment reduced serum cholesterol levels by 25% and serum triglycerides by 75% in chow-fed mice and also attenuated diet-induced hypercholesterolemia. GC-1 reduced plasma HDL cholesterol levels and increased expression of the hepatic HDL receptor.[26] Collectively, these results suggest that GC-1 stimulates important steps in reverse cholesterol transport. Use of TR β and tissue uptake-selective agonists such as GC-1 should be further explored as a strategy to improve lipid metabolism in dyslipoproteinemia.
Another study compared the effects of a 6-week treatment of equimolar doses of triiodothyronine with GC-1 on different metabolic parameters in adult female rats. It is seen that both T3 and GC-1 treatment promoted decrease in fat. However, the mass of individual skeletal muscles was negatively affected by T3, but only barely by GC-1.[39] These findings suggested the potential use of GC-1 for the treatment of obesity and the metabolic syndrome.
Eprotirome
Eprotirome (KB2115), which contains two bromides, has minimal uptake in nonhepatic tissues as compared with triiodothyronine. It has a modestly higher affinity for the triiodothyronine receptor TR β isoform.[15] This compound was evaluated in humans. In a 2-week clinical trial, eprotirome was reported to reduce the levels of serum total and LDL cholesterol and apolipoprotein B without evident side-effects.[40]
In another placebo-controlled trial, eprotirome was associated with further reductions in serum LDL cholesterol levels in patients who are already receiving statins. Eprotirome also has potent properties for lowering levels of apolipoprotein B, triglycerides and Lp(a) lipoprotein, and it not associated with adverse effects on the heart or bone.[41] Lowered HDL cholesterol has been observed in patients on eprotirome, which has been associated with cardiovascular risk, but it is unclear whether these treatment-induced changes would impact cardiovascular disease incidence. Recently in Feb 2012 Karo Bio has decided to discontinue the phase III development program for eprotirome after one of the long term animal studies on dogs demonatrated cartilage damage in high as well as low dose groups.[42]
Tiratricol
Tiratricol is also known as TRIAC or triiodothyroacetic acid. Due to its well proven ability to suppress TSH, it is indicated in the management of thyroid hormone resistance syndrome and is used, in combination with levothyroxine in patients with thyroid cancer. It has been widely marketed for weight loss drug but with FDA warning for adverse effects including heart attacks and strokes.[43]
DIMIT (3,5- dimethyl-3-isopropyl-L-thyronine)
Maternal administration of DIMIT results in significant enhancement of fetal lung phospholipid synthesis and accelerated lung maturity. Study in rabbit fetal lungs demonstrated that short-term maternal administration of DIMIT in pregnant diabetic rabbits not only promotes fetal lung phospholipid synthesis, but also appears to ameliorate maternal hyperglycemia.[44]
Mb07811
As site of beneficial action of thyroid hormone analogues is mostly liver, liver specific delivery is needed. One of the approach is by phosphonic acied linked prodrug MB07811, which after selectively entering hypatocytes is cleaved into TRβ agonist MB07344 which has lipid lowering properties. By using several experimental approaches, Cable et al. showed that MB07811 has antisteatotic activity that is able to reduce hepatic triglyceride levels in both normal and metabolically-challenged animal models,.[45] But a phase II Study of MB07811 in Subjects With Hypercholesterolemia was terminated prior to initiation.[46]
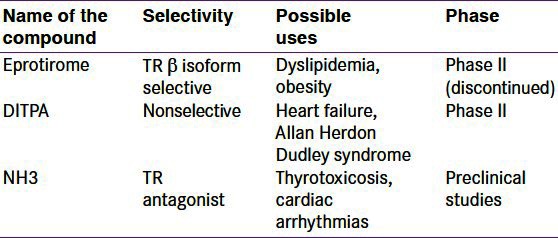
Some selective TR modulators in various phases of development are shown in Table 2.
Table 2.
Selective thyroid receptor modulators under development and their current status
TR β selectivity of the above two compounds, KB-141 and GC-1, is very less. The data suggest that even moderate TR β1-selective agonists can be useful in the development of antiobesity and lipid-lowering drugs with heart-sparing properties. Therefore, there is a need for a compound with further increase in selectivity. Some of the newly developed compounds showed high TR β1 selectivity with proposed low cardiovascular side effects.[8]
Nonselective thyroid analogues
HF is a syndrome resulting from the inability of the heart to pump sufficient blood for the body's peripheral requirements oxygen and cell nutrients, at rest and during effort. The prevalence and incidence of congestive heart failure (CHF) increases as the population ages.
Despite the reduction in mortality and morbidity with the use of angiotensin-converting enzyme inhibitors, Angiotensin II receptor blockers, β blockers and aldosterone antagonists, the prognosis of CHF remains dismal. THs and, in particular, the active form, T3, regulate the synthesis and action of various cardiac proteins, including α- and β-myosin heavy chain sarcoplasmic reticulum Ca2+ ATPase, Na+/Ca2+ exchanger, phospholamban and voltage-gated potassium channels.[47] The fundamental actions of TH on the cardiovascular system are well documented not only by the large series of experimental data[47] but also by the more recent evidence of cardiovascular alterations in the presence of minimal changes of thyroid function in humans. Changes in thyroid metabolism, characterized by a reduction in biologically active T3, have been reported in HF[47] and commonly interpreted as a compensatory mechanism. The hypothesis that this alteration is an adaptive factor minimizing catabolic phenomena of illness has been recently questioned as there is evidence of a negative prognostic impact of this syndrome in patients with heart diseases and, specifically, in patients with HF. A strong argument in favor of the hypothesis that a low T3 state may contribute to the poor prognosis of HF patients comes from data showing the benefit gained from treating patients with synthetic TH. Unfortunately, only a few studies have tested the synthetic T4 or T3 as a potentially beneficial treatment of cardiac dysfunction.[48,49] From the first observation,[50] it was clear that one of the major limitations of using T3 would have been the noncardiac effects such as increase in oxygen consumption and heart rate as well as negative effects on protein and fat metabolism. In humans, three studies evaluated the possibility of using T3 and T4 therapeutically with the purpose of improving cardiac function of HF avoiding the unwanted detrimental effects,[49,51,52] in which there was an increase in cardiac output associated with a decrease in systemic vascular resistance.[48,51] Also, in a pilot study, the improvement in the cardiovascular (and renal) hemodynamics was also associated with a progressive increase in 24-h urinary output and a reduction in noradrenaline plasma levels.
DITPA (3,5-Diiodothyropropionic acid
An alternative approach to the treatment of CHF could be the use of selective TR modulators, like 3,5-diiodothyropropionic acid (DITPA).[53,54] The structural similarity of DITPA to T4 and other TH agonists and its demonstrated ability to bind to nuclear TR make it likely that DITPA works as a thyromimetic agent.[53] Although DITPA does not bind with high selectivity to specific TR isoforms, it differs in structure from T3 in that it lacks an outer-ring iodide and the amine in the carboxylic acid side chain. These differences would be predicted to change the interactions of DITPA with amino acid side chains in the receptor-binding pocket, thereby altering receptor conformation. Because receptor conformation affects the interactions of the bound receptor with tissue-specific cofactors, it could contribute to differences in relative tissue potencies. The increase in cardiac output and decrease in vascular resistance seen with DITPA are typical cardiovascular actions of TH. At the same time, the minimal increase in heart rate implies a different pattern of tissue-specific thyromimetic potencies. Such differences in relative potencies of tissue TH actions have been shown previously for other TH analogues, such as triiodothyroacetic acid[55] GC-1[56] and KB-141.[32] The lowering of serum total and LDL cholesterol concentrations is also consistent with significant hepatic thyromimetic activity of DITPA. The rationale for potential use of a TH analogue in the treatment of HF involves the known properties of TH with respect to the cardiovascular system, such as an increase in left ventricular systolic performance, improvement of diastolic function and a decrease in peripheral vascular resistance.[57]
In a Phase II, multicenter, randomized, placebo-controlled double blind trial of NYHA class II to class IV CHF patients, DITPA improved some hemodynamic and metabolic parameters like increased cardiac index, decreased systemic vascular resistance, serum cholesterol, LDL cholesterol and body weight, but was poorly tolerated with no evidence of symptomatic benefit.[58] Therefore, there is a need for compounds with more selective TR α action that could be more beneficial and effective in CHF.
In a recent study carried out to examine the role of DITPA in the acute phase following infarction, treatment with DITPA attenuated the acute inflammatory response and reduced myocardial infarct size. The reduction in myocardial ICAM-1, KC, and IL-6 levels in the DITPA group was associated with a decrease in macrophage and neutrophil accumulation.[59] While opposite result was declared in an animal study on mice, where DITPA increased the ventricular dimensions and decreased contractile functions of heart. DITPA treated mice exhibited higher prevalence of fatal arrhythmias with no improvement in myocardial infarction and postischemic fractional shortening.[60] In the view of such conflicting results more detailed clinical trials are needed.
Other than its action in HF, DITPA has shown its use in one of the congenital disorders of TH, as shown in animal experiments in mice.[61] This disorder, called Allan Herdon Dudley syndrome, is due to mutation in the transporter of T3 called Monocarboxylate Transporter 8 (MCT8), which is highly expressed in the brain. Patients with MCT8 mutations have severe neurological impairment and psychomotor retardation, presumably due to intracellular TH deficiency. Entry of DITPA in cells of target tissues is independent of MCT8. Thus, it could be valuable in treating these patients. Some selective TR modulators in various phases of development are shown in Table 2.
THYROID HORMONE RECEPTOR ANTAGONISTS
Apart from the available TH synthesis inhibitors and release inhibitors, progress has also been made in attempting to treat hyperthyroidism by synthesizing antagonists that block TH action at the level of the TH receptor or of the thyrotropin receptor.[62] They might be useful as potential antiarrhythmic agents, particularly TR α1-selective antagonists.
It has been observed that developing antagonists is more difficult than developing agonists. Although many TR antagonists have been reported,[63,64] little work has been done in vivo to confirm this activity. Several of the antagonists reported in the literature in vitro are not active as antagonists in vivo, and most act as TR agonists, the exact reason behind the differing action being unknown.[62] The complexity of interactions between modulators and receptor makes prediction of the activity of TR modulators in vivo more difficult.[65,66]
NH3
One of the TR antagonists evaluated in animal studies is NH3. NH3 is a TR inhibitor[64,67] in vitro and in vivo in amphibians, although some partial agonist properties were seen at higher doses. In rats, NH3 showed TR inhibition that increases up to the 924 nmol/kg/day dose, and there was a loss of these effects at higher concentrations. At high doses, it showed apparent partial agonistic activity for cholesterol, heart rate and TSH. NH3 is not TR subtype-selective in vitro, and it does not seem to be selective in rats, because both TR α- and TR β-mediated parameters were inhibited.[62]
The exact reason for this loss of antagonistic activity at high doses is not known. It may be due to true partial agonist activity or a metabolite with agonist properties may be generating this. It is also possible that increasing TSH might also increase circulating THs and, at higher concentrations, the higher levels of T4 and T3 could surmount the NH3 antagonist effects.[62]
Pharmacology of NH3 action is complicated. It requires almost 1 week to develop both agonistic action at low doses and antagonistic action at high doses. Although NH3 had no effect on TSH at either dose, it lowered cholesterol to equivalent levels at both doses, despite the great difference in the doses. Hence, it is stated that at least several days of treatment are necessary for TR antagonist effects to become apparent.[62] Therefore, if NH3 is to be evaluated in humans in the future, it should be used with caution and in proper doses.
Tetrac
Deaminated derivative of T4, tetraiodothyroacetic acid (tetrac), blocks binding and actions of T4 and T3 at the receptor on αvβ3 which is a heterodimeric structural protein of the plasma membrane that bears a cell surface receptor for thyroid hormone. Thus tetrac exerts anti-proliferative actions at the integrin thyroid hormone receptor. Tetrac has been re-formulated as a nanoparticle (nanotetrac) that acts exclusively at the αvβ3 receptor and does not enter cells. Nanotetrac disrupts expression of genes in multiple cancer cell survival pathways. Nanotetrac and tetrac inhibit the pro-angiogenic actions in vitro of vascular endothelial growth factor, basic fibroblast factor, and other growth factors.[68] The US FDA has granted Orphan Drug status for Tetrac for the purpose of suppressing TSH in association with thyroid cancer treatment.[69]
Because of the presence of possible indications, development of thyroid antagonists with further improved isoform selectivity and stable activity is required.
SUMMARY
TH is known to have a hypolididemic and weight reducing property, but this benefit could not be explored due to the deleterious effects on the heart. But, recently, isolation and study of specific receptors expressed on different tissues and development of specific ligands for these receptors have paved way for the development of specific compounds with higher affinity for tissue-specific receptors. Eprotirome is a specific TR β1 agonist shown to have a beneficial effect in dyslipidemia but devoid of the deleterious effects of TH. Similarly, DITPA has been shown to be beneficial in HF to some extent. Specific TR α agonists are difficult to synthesize as compared with specific TR β. Further structural and detailed study of receptors as well as structure–activity relationship of different ligands will provide with compounds of potential benefit.
ACKNOWLEDGMENT
The authors wish to acknowledge the help extended by Dr. Nimish Halasawadekar and Dr. Nitin Puram, Department of Pharmacology, Government Medical College, Miraj, Maharashtra.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Baxter JD, Dillmann WH, West BL, Huber R, Furlow JD, Fletterick RJ, et al. Selective modulation of thyroid hormone receptor action. J Steroid Biochem Mol Biol. 2001;76:31–42. doi: 10.1016/s0960-0760(01)00052-8. [DOI] [PubMed] [Google Scholar]
- 2.Kraiem Z. Selective agonists and antagonists to thyroid hormone action. Thyroid. 2005;15:336–9. doi: 10.1089/thy.2005.15.336. [DOI] [PubMed] [Google Scholar]
- 3.Evans RM. The steroid and thyroid hormone receptor superfamily. Science. 1988;240:889–95. doi: 10.1126/science.3283939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mangelsdorf DJ, Thummel C, Beato M, Herrlich P, Schutz G, Umesono K, et al. The nuclear receptor superfamily: The second decade. Cell. 1995;83:835–9. doi: 10.1016/0092-8674(95)90199-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ribeiro RC, Kushner PJ, Baxter JD. The nuclear hormone receptor gene superfamily. Ann Rev Med. 1995;46:443–53. doi: 10.1146/annurev.med.46.1.443. [DOI] [PubMed] [Google Scholar]
- 6.Lazar MA. Thyroid hormone receptors: Multiple forms, multiple possibilities. Endocr Rev. 1993;14:184–93. doi: 10.1210/edrv-14-2-184. [DOI] [PubMed] [Google Scholar]
- 7.Yen PM. Physiological and molecular basis of thyroid hormone action. Phys Rev. 2001;81:1097–142. doi: 10.1152/physrev.2001.81.3.1097. [DOI] [PubMed] [Google Scholar]
- 8.Malm J, Grover GJ, Färnegårdh M. Recent advances in the development of agonists selective for β1-type thyroid hormone receptor. Mini-Rev Med Chem. 2007;7:79–86. doi: 10.2174/138955707779317885. [DOI] [PubMed] [Google Scholar]
- 9.Forrest D, Vennström B. Functions of thyroid hormone receptors in mice. Thyroid. 2000;10:41–52. doi: 10.1089/thy.2000.10.41. [DOI] [PubMed] [Google Scholar]
- 10.O’shea PJ, Williams GR. Insight into the physiological actions of thyroid hormone receptors from genetically modified mice. J Endocrinol. 2002;175:553–70. doi: 10.1677/joe.0.1750553. [DOI] [PubMed] [Google Scholar]
- 11.Chatterjee VK. Resistance to thyroid hormone. Horm Res. 1997;48:43–6. doi: 10.1159/000191312. [DOI] [PubMed] [Google Scholar]
- 12.Refetoff S. Resistance to thyroid hormone: An historical overview. Thyroid. 1994;4:345. doi: 10.1089/thy.1994.4.345. [DOI] [PubMed] [Google Scholar]
- 13.Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Efficacy and safety of cholesterol-lowering treatment: Prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–78. doi: 10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 14.Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III): Final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 15.Sarwar N, Danesh J, Eiriksdottir G, Sigurdsson G, Wareham N, Bingham S, et al. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation. 2007;115:450–8. doi: 10.1161/CIRCULATIONAHA.106.637793. [DOI] [PubMed] [Google Scholar]
- 16.Bennet A, Di Angelantonio E, Erqou S, Eiriksdottir G, Sigurdsson G, Woodward M, et al. Lipoprotein(a) levels and risk of future coronary heart disease: Large-scale prospective data. Arch Intern Med. 2008;168:598–608. doi: 10.1001/archinte.168.6.598. [DOI] [PubMed] [Google Scholar]
- 17.Kastelein JJ, Akdim F, Stroes ES, Zwinderman AH, Bots ML, Stalenhoef AF, et al. Simvastatin with or without ezetimibe in familial hypercholesterolemia. N Engl J Med. 2008;358:1431–43. doi: 10.1056/NEJMoa0800742. [DOI] [PubMed] [Google Scholar]
- 18.Taylor AJ, Villines TC, Stanek EJ, Devine PJ, Griffen L, Miller M, et al. Extended-release niacin or ezetimibe and carotid intima-media thickness. N Engl J Med. 2009;361:2113–22. doi: 10.1056/NEJMoa0907569. [DOI] [PubMed] [Google Scholar]
- 19.Pearson TA, Laurora I, Chu H, Kafonek S. The Lipid Treatment Assessment Project (L-TAP): A multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid-lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch Intern Med. 2000;160:459–67. doi: 10.1001/archinte.160.4.459. [DOI] [PubMed] [Google Scholar]
- 20.Pasternak RC, Smith SC, Jr, Bairey-Merz CN, Grundy SM, Cleeman JI, Lenfant C, et al. ACC/AHA/NHLBI clinical advisory on the use and safety of statins. Circulation. 2002;106:1024–8. doi: 10.1161/01.cir.0000032466.44170.44. [DOI] [PubMed] [Google Scholar]
- 21.Mason RL, Hunt HM, Hurxthal LM. Blood cholesterol values in hyperthyroidism and hypothyroidism: Their significance. N Engl J Med. 1930;203:1273–8. [Google Scholar]
- 22.Walton KW, Scott P, Dykes PW, Davies JW. The significance of alterations in serum lipids in thyroid dysfunction, II: Alterations of the metabolism and turnover of 131I low-density lipoproteins in hypothyroidism and thyrotoxicosis. Clin Sci. 1965;29:217–38. [PubMed] [Google Scholar]
- 23.Thompson GR, Soutar AK, Spengel FA, Jadhav SJ, Gavigan SJ, Myant NB. Defects of receptor-mediated low density lipoprotein catabolism in homozygous familial hypercholesterolemia and hypothyroidism in vivo. Proc Natl Acad Sci USA. 1981;78:2591–5. doi: 10.1073/pnas.78.4.2591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berkenstam A, Kristensen J, Mellstrom K, Carlsson B, Malm J, Rehnmark S, et al. The thyroid hormone mimetic compound KB2115 lowers plasma LDL cholesterol and stimulates bile acid synthesis without cardiac effects in humans. Proc Natl Acad Sci USA. 2008;105:663–7. doi: 10.1073/pnas.0705286104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gullberg H, Rudling M, Salto C, Forrestm D, Angelin B, Vennstrom B. Requirement for thyroid hormone receptor beta in T3 regulation of cholesterol metabolism in mice. Mol Endocrinol. 2002;16:1767–77. doi: 10.1210/me.2002-0009. [DOI] [PubMed] [Google Scholar]
- 26.Johansson L, Rudling M, Scanlan TS, Lundåsen T, Webb P, Baxter J, et al. Selective thyroid receptor modulation by GC-1 reduces serum lipids and stimulates steps of reverse cholesterol transport in euthyroid mice. Proc Natl Acad Sci USA. 2005;102:10297–302. doi: 10.1073/pnas.0504379102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Day R, Gebhard RL, Schwartz HL, Strait KA, Duane WC, Stone BG, et al. Time course of hepatic 3-hydroxy-3- methylglutaryl coenzyme A reductase activity and messenger ribonucleic acid, biliary lipid secretion and hepatic cholesterol content in methimazole-treated hypothyroid and hypophysectomized rats after triiodothyronine administration: Possible linkage of cholesterol synthesis to biliary secretion. Endocrinology. 1989;125:459–68. doi: 10.1210/endo-125-1-459. [DOI] [PubMed] [Google Scholar]
- 28.Sherman SI, Ringel MD, Smith MJ, Kopelen HA, Zoghbi WA, Ladenson PW, et al. Augmented hepatic and skeletal thyromimetic effects of tiratricol in comparison with levothyroxine. J Clin Endocrinol Metab. 1997;82:2153–8. doi: 10.1210/jcem.82.7.4054. [DOI] [PubMed] [Google Scholar]
- 29.Hill SR, Jr, Barker SB, McNeil JH, Tingley JO, Hibbett LL. The metabolic effects of the acetic and propionic acid analogs of thyroxine and triiodothyronine. J Clin Invest. 1960;39:523–33. doi: 10.1172/JCI104066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Strisower EH, Strisower B. The separate hypolipoproteinemic effects of dextrothyroxine and ethyl chlorophenoxyisobutyrate. J Clin Endocrinol Metab. 1964;24:139–44. doi: 10.1210/jcem-24-2-139. [DOI] [PubMed] [Google Scholar]
- 31.Underwood AH, Emmett JC, Ellis D, Flynn SB, Leeson PD, Benson GM, et al. A thyromimetic that decreases plasma cholesterol levels without increasing cardiac activity. Nature. 1986;324:425–9. doi: 10.1038/324425a0. [DOI] [PubMed] [Google Scholar]
- 32.Grover GJ, Mellström K, Ye L, Malm J, Li YL, Bladh LG, et al. Selective thyroid hormone receptor-beta activation: A strategy for reduction of weight, cholesterol, and lipoprotein(a) with reduced cardiovascular liability. Proc Natl Acad Sci USA. 2003;100:10067–72. doi: 10.1073/pnas.1633737100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grover GJ, Mellstrom K, Malm J. Therapeutic potential for thyroid hormone receptor-β selective agonists for treating obesity, hyperlipidemia and diabetes. Bentham Science Publishers. Curr Vasc Pharmacol. 2007;5:141–54. doi: 10.2174/157016107780368271. [DOI] [PubMed] [Google Scholar]
- 34.Thyroid and weight. American Thyroid Association. [accessed 2011 May 30]. Available from: http://www.thyroid.org/patients/patient_brochures/weight.html .
- 35.Miriam OR, Suzy DC, Masahiro K, James JS, Sheue-yann C, Antonio CB, et al. Expression of uncoupling protein 1 in mouse brown adipose tissue is thyroid hormone receptor-isoform specific and required for adaptive thermogenesis. Endocrinology. 2010;151:432–40. doi: 10.1210/en.2009-0667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chiellini G, Apriletti JW, Yosihhara HA, Baxter JD, Ribeiro RC, Scanlan TS. A high-affinity subtype-selective agonist ligand for the thyroid hormone receptor. Chem Biol. 1998;5:299–306. doi: 10.1016/s1074-5521(98)90168-5. [DOI] [PubMed] [Google Scholar]
- 37.Chiellini G, Nguyen NH, Apriletti JW, Baxter JD, Scanlan TS. Synthesis and biological activity of novel thyroid hormone analogues: 5’-aryl substituted GC-1 derivatives. Bioorg Med Chem. 2002;10:333–46. doi: 10.1016/s0968-0896(01)00284-x. [DOI] [PubMed] [Google Scholar]
- 38.Gloss B, Giannocco G, Swanson EA, Moriscot AS, Chiellini G, Scanlan TS, et al. Different configurations of specific thyroid hormone response elements mediate opposite effects of thyroid hormone and GC-1 on gene expression. Endocrinology. 2005;146:4926–33. doi: 10.1210/en.2005-0631. [DOI] [PubMed] [Google Scholar]
- 39.Villicev CM, Freitas FR, Aoki MS, Taffarel C, Scanlan TS, Moriscot AS, et al. Thyroid hormone receptor beta-specific agonist GC-1 increases energy expenditure and prevents fat-mass accumulation in rats. J Endocrinol. 2007;193:21–9. doi: 10.1677/joe.1.07066. [DOI] [PubMed] [Google Scholar]
- 40.Ness GC, Pendleton LC, Li YC, Chiang JY. Effect of thyroid hormone on hepatic cholesterol 7 alpha hydroxylase, LDL receptor, HMG-CoA reductase, farnesyl pyrophosphatem synthetase and apolipoprotein A-I mRNA levels in hypophysectomizedrats. Biochem Biophys Res Commun. 1990;172:1150–6. doi: 10.1016/0006-291x(90)91568-d. [DOI] [PubMed] [Google Scholar]
- 41.Ladenson PW, Kristensen JD, Ridgway EC, Olsson AG, Carlsson B, Klein I. Use of the thyroid hormone analogue eprotirome in statin-treated dyslipidemia. N Engl J Med. 2010;362:906–16. doi: 10.1056/NEJMoa0905633. [DOI] [PubMed] [Google Scholar]
- 42.Karo bio terminates the eprotirome program. [accesed on 29th March 2012]. Available from www.karobio.com .
- 43.Carvalho GA, Ramos HE. Thyroid hormone resistance syndrome. Arq Bras Endocrinol Metabol. 2004;48(1):83–92. doi: 10.1590/s0004-27302004000100010. [DOI] [PubMed] [Google Scholar]
- 44.Neufeld N, Melmed S. 3,5-dimethyl-3’- isopropyl-l-thyronine Therapy in diabetic pregnancy Stimulation of rabbit fetal lung phospholipids. J. Clin. Invest. Dec;68:19811605–1609. doi: 10.1172/JCI110417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.ARRESE M. Burning Hepatic Fat: Therapeutic Potential for Liver-Specific Thyromimetics in the Treatment of Nonalcoholic Fatty Liver Disease, Hepatology. [accesed on 28th March 2012];Study of MB07811 in subjects with hypercholesterolemia. 49(No 2):200946. doi: 10.1002/hep.22783. Available from www.clinicaltrials.gov . [DOI] [PubMed] [Google Scholar]
- 46.Study of MB07811 in subjects with hypercholesterolemia. [accesed on 28th March 2012]. Available from www.clinicaltrials.gov .
- 47.Klein I, Ojamaa K. Thyroid hormone and the cardiovascular system. N Engl J Med. 2001;344:501–9. doi: 10.1056/NEJM200102153440707. [DOI] [PubMed] [Google Scholar]
- 48.Klemperer JD, Klein I, Gomez M, Helm RE, Ojamaa K, Thomas SJ, et al. Thyroid hormone treatment after coronary-artery bypass surgery. N Engl J Med. 1995;333:1522–7. doi: 10.1056/NEJM199512073332302. [DOI] [PubMed] [Google Scholar]
- 49.Hamilton MA, Stevenson LW, Fonarow GC, Steimle A, Goldhaber JI, Child JS, et al. Safety and hemodynamic effects of intravenous triiodothyronine in advanced congestive heart failure. Am J Cardiol. 1998;81:443–7. doi: 10.1016/s0002-9149(97)00950-8. [DOI] [PubMed] [Google Scholar]
- 50.Gay RG, Graham S, Aguirre M, Goldman S, Morkin E. Effects of 10-to 12-day treatment with l-thyroxine in rats with myocardial infarction. Am J Physiol. 1988;255:801–6. doi: 10.1152/ajpheart.1988.255.4.H801. [DOI] [PubMed] [Google Scholar]
- 51.Moruzzi P, Doria E, Agostoni PG. Medium-term effectiveness of l-thyroxine treatment in idiopathic dilated cardiomyopathy. Am J Med. 1996;101:461–7. doi: 10.1016/s0002-9343(96)00281-1. [DOI] [PubMed] [Google Scholar]
- 52.Lervasi G, Emdin M, Colzani RM. Beneficial effects of longterm triiodothyronine (t3) infusion in patients with advanced heart failure and low t3 syndrome. In: Kimchi A, editor. Heart disease: New trends in research, diagnosis and treatment. Bologna: Medimond Medical Publ; 2001. pp. 549–58. [Google Scholar]
- 53.Pennock GD, Raya TE, Bahl JJ, Goldman S, Morkin E. Cardiac effects of 3,5-diiodothyropropionic acid: A thyroid hormone analog with inotropic selectivity. J Pharmacol Exp Ther. 1992;263:163–9. [PubMed] [Google Scholar]
- 54.Morkin E, Ladenson P, Goldman S, Adamson C. Thyroid hormone analogs for treatment of hypercholesterolemia and heart failure: Past, present and future prospects. J Mol Cell Cardiol. 2004;37:1137–46. doi: 10.1016/j.yjmcc.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 55.Sherman SI, Ladenson PW. Organ-specific effects of tiratricol: A thyroid hormone analog with hepatic, not pituitary, superagonist effects. J Clin Endocrinol Metab. 1992;75:901–5. doi: 10.1210/jcem.75.3.1517383. [DOI] [PubMed] [Google Scholar]
- 56.Baxter JD, Webb P, Grover G, Scanlan TS. Selective activation of thyroid Hormone signaling pathways by gc-1: A new approach to controlling Cholesterol and body weight. Trends Endocrinol Metab. 2004;15:154–7. doi: 10.1016/j.tem.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 57.Biondi B, Cooper DS. The clinical significance of subclinical thyroid Dysfunction. Endocr Rev. 2008;29:76–131. doi: 10.1210/er.2006-0043. [DOI] [PubMed] [Google Scholar]
- 58.Goldman S, McCarren M. DITPA (3,5-diiodothyropropionic acid), a thyroid hormone analog to treat heart failure: Phase II trial veterans affairs cooperative study. Circulation. 2009;119:3093–100. doi: 10.1161/CIRCULATIONAHA.108.834424. [DOI] [PubMed] [Google Scholar]
- 59.Abohashem-Aly AA, Meng X, Li J, Sadaria MR, Ao L, Wennergren J, Fullerton DA, Raeburn CD. DITPA, a thyroid hormone analog, reduces infarct size and attenuates the inflammatory response following myocardial ischemia. J Surg Res. 2011 Dec;171(2):379–85. doi: 10.1016/j.jss.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 60.Muthu Periasamy, Xie Jay L. Zweier, Mahamud Shouvik D., Mahamud, Kalyanasundaram Anuradha, Bonagura John D., Talukder M.A. Hassan, Yang Fuchun, Nishijima namesYoshinori, Chen Chun-An. Lin Detrimental effects of thyroid hormone analog DITPAacute myocardial ischemia-reperfusion in the mouse heart: increased mortality with in vivo. Am J Physiol Heart Circ Physiol. 2011;300:H702–H711. doi: 10.1152/ajpheart.00514.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Di Cosmo C, Liao XH, Dumitrescu AM, Weiss RE, Refetoff S. A thyroid hormone analogue with reduced dependence on the monocarboxylate transporter 8 (MCT8) for tissue transport. Endocrinology. 2009;150:4450–8. doi: 10.1210/en.2009-0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Grover GJ, Dunn C, Nguyen NH, Boulet J, Dong G, Domogauer J, et al. Pharmacological profile of the thyroid receptor antagonist NH3 in rats. J Pharmacol Exp Ther. 2007;322:385–90. doi: 10.1124/jpet.106.116152. [DOI] [PubMed] [Google Scholar]
- 63.Carlsson B, Singh BN, Temciuc M, Nilsson S, Li YL, Mellin C, et al. Synthesis and preliminary characterization of a novel antiarrhythmic compound (KB130015) with an improved toxicity profile compared with amiodarone. J Med Chem. 2002;45:623–30. doi: 10.1021/jm001126+. [DOI] [PubMed] [Google Scholar]
- 64.Lim W, Nguyen NH, Yang HY, Scanlan TS, Furlow JD. A thyroid hormone antagonist that inhibits thyroid hormone action in vivo. J Biol Chem. 2002;277:35665–70. doi: 10.1074/jbc.M205608200. [DOI] [PubMed] [Google Scholar]
- 65.Harvey CB, Williams GR. Mechanism of thyroid hormone action. Thyroid. 2002;12:441–6. doi: 10.1089/105072502760143791. [DOI] [PubMed] [Google Scholar]
- 66.Moore JM, Galicia SJ, McReynolds AC, Nguyen NH, Scanlan TS, Guy RK. Quantitative proteomics of the thyroid hormone receptor-coregulator interactions. J Biol Chem. 2004;279:27584–90. doi: 10.1074/jbc.M403453200. [DOI] [PubMed] [Google Scholar]
- 67.Nguyen NH, Apriletti JW, Cunha Lima ST, Webb P, Baxter JD, Scanlan TS. Rational design and synthesis of a novel thyroid hormone antagonist that blocks coactivator recruitment. J Med Chem. 2002;45:3310–20. doi: 10.1021/jm0201013. [DOI] [PubMed] [Google Scholar]
- 68.Lin HY, Cody V, Davis FB, Hercbergs AA, Luidens MK, Mousa S, Davis PJ. Identification and Functions of the Plasma Membrane Receptor for Thyroid Hormone Analogues. Discov Med. 2011 Apr;11(59):337–347. [PubMed] [Google Scholar]
- 69.King Pharmaceuticals Announces Exclusive License for Tetrac. [accesed on 29th March 2012]. Available from http://tbutton.prnewswire.com/prn/11690X04258115 .


