Abstract
Background:
Permanent hypocalcaemia following thyroidectomy causes considerable morbidity. This prospective observational study aims to define the factors likely to predict hypocalcaemia following total thyroidectomy.
Materials and Methods:
Patients who were subjected to total thyroidectomy during January 2005 to December 2009 were followed up for a minimum period of 1 year. Efficacy of an intraoperative parathyroid hormone assay to predict hypocalcaemia was validated.
Results:
Overall incidence of hypocalcaemia was 23.6% (n = 190) and that of permanent hypocalcaemia was 1.61% (n = 13). Onset was delayed up to 3rd postoperative day in 13 patients. Hypocalcaemia was significantly associated with thyroidectomy for Grave's Disease (P = 0.001), Hashimoto's thyroiditis (P = 0.003), and with incidental parathyroidectomy (P = 0.006). The intraoperative assay of parathyroid hormone showed low sensitivity (0.5) and satisfactory specificity (0.9) in predicting hypocalcemia.
Conclusion:
Hypocalcemia could manifest late in the immediate postoperative period and this may explain latent hypocalcemia. High incidence of hypocalcaemia noted in Grave's Disease could be due to the autoimmunity since same feature was noted associated with Hashimoto's thyroiditis and the incidence of hypocalcaemia was not high in the subgroup with toxic nodular goiter. The incidence of hypocalcemia was not affected by age or sex.
Keywords: Grave's disease, hyperthyroidism, hypocalcemia, total thyroidectomy
INTRODUCTION
Theodore Kocher recognized recurrent laryngeal nerve injury, myxedema, and tetany as the three main postoperative complications of thyroidectomy as early as 1883. Tetany was attributed to deficiency of thyroid gland until Moussu (1898) could relieve it with an aqueous extract of parathyroid glands. Fourman and colleagues (1963) suggested persistent parathyroid insufficiency following transient hypocalcaemia.[1] They observed persistent parathyroid insufficiency in 24% of patients after thyroidectomy based on depression of serum ionized calcium level by the ethylene diaminetetraacetic acid (EDTA) infusion test. However, the issue of delayed persistent parathyroid insufficiency needs further exploration. Another study in Aberdeen Royal Infirmary noted high incidence of symptomatic patients on stress test but essentially did not correlate with serum calcium levels.[2] This feature was noted in the first 2 years following thyroidectomy.
The immediate manifestations of hypocalcaemia are mostly neuro-muscular symptoms and occasionally psychotic states. Ectodermal changes leading on to alopecia, eczema, and cataract may occur as early as 6 months after operation. Persistent hypocalcaemia may cause intracranial lesions and cardiac arrhythmias. Permanent hypocalcaemia causes substantial impact on health of patient along with considerable financial loss. Capsular dissection of thyroid lobes described in detail by Delbridge and Reeve could markedly reduce the incidences of permanent hypocalcaemia.[3] The first author reported a low incidence of 0.4% permanent hypocalcaemia in a large series 2110 operations.[4] The intraoperative assay of intact parathyroid hormone (PTH) was found to be useful in predicting hypocalcaemia after thyroidectomy and is recommended by Australian Society of Endocrine Surgeons.[5]
Large volume goiter, total thyroidectomy, recurrent goiter, retrosternal extension, advanced cancer, hyperthyroidism, and experience of the surgeons were found risk factors predisposing to post-thyroidectomy hypocalcaemia.[6,7,8] The aim of this study was to identify factors, that predispose to postoperative hypocalcaemia. We hypothesized that total thyroidectomy performed for hyperthyroidism, medistinal extension, malignancy, thyroiditis, and recurrence were associated with high incidence of hypocalcaemia.
MATERIALS AND METHODS
This observational study was conducted on patients operated for thyroid diseases during January 2005 to December 2008. Patients, who had undergone total thyroidectomy by bilateral exploration, were included in the study.
Exclusion criterions included: (1) completion thyroidectomy following hemithyroidectomy, (2) concurrent lymph node dissection, (3) patients who received calcium supplementation, (4) pre-existing hypocalcaemia, and (5) patients who underwent parathyroid auto-transplantation.
Preliminary work up included complete clinical examination, biochemical assay of hormone profile, and Technetium 99 thyroid scintigraphy in patients with hyperthyroidism. Ultrasound imaging of the thyroid gland and neck in general was done routinely. Aspiration cytology was performed from all solitary nodules and nodules showing suspicious features on clinical examination or ultrasound imaging. Plain helical computerized tomography was done when clinical evidences of mediastinal extension were noted. Mediastinal extension was confirmed when the lower border of goiter reached up to or beyond lower border of T4 spine. Hyperthyroidism was controlled before operation. Vocal cords were assessed by indirect laryngoscopy prior to operation.
Operation was performed by members of surgical team noted under general anesthesia. The lateral mobilization was done by the capsular dissection technique identifying parathyroid glands and laryngeal nerves. The parathyroid glands were inspected before closure for signs of ischemia. Auto-transplantation was done in the sternocleidomastoid muscle when viability was suspected by color change. Vocal cords were reassessed after extubation by direct laryngoscopy.
Serum corrected calcium was estimated before commencing operation, 6 hours after operation and at 7 AM on postoperative days till discharge. Serum intact PTH assay was done as a validation study to predict hypocalcaemia during 10 months from January 2005. The rapid immunochemiluminometric assay (ICMA) of intact PTH was done in blood drawn 10 minutes after removal of the thyroid gland (Architect).
Hypocalcaemia was diagnosed when serum corrected calcium level dropped below 8 mg/deciliter. Patients with hypocalcaemia received oral calcium supplementation (Shelcal 500 mg, Elder India, 2 tablets three times daily) along with Calcitriol (Rolsical 0.25 mg, Sun India, twice daily). Patients who developed neuromuscular symptoms received intravenous infusion of calcium gluconate, (1 mg elemental calcium/kilogram body weight/h). Patients who developed complications were reviewed monthly for 12 months or more. Serum corrected calcium was estimated on monthly visit after withholding calcium supplementation for 24 hours.
Hypocalcaemia is defined as serum corrected calcium level below 8 mg/dl. Permanent hypocalcaemia is defined as persistent hypocalcaemia after 6 months of thyroidectomy.
Statistics
The sample size was based on overall incidence of 10.6% hypocalcaemia noted following total thyroidectomy in one of our published studies.[6] Variables collected included preoperative clinical diagnosis, histological diagnosis, date of onset of hypocalcaemia, duration of calcium supplementation required and incidental parathyroidectomy. We have excluded goiter size from the final analysis since 716 (88.8%) specimens weighed over 75 g and 82 (10.17%) small sized goiters were associated with risk factors as hyperthyroidism and cancer. High risk category included patients with one or more risk factors.
SPSS version 11 was employed for statistical analysis. The Chi-square test was employed for testing statistical significance of association between two discrete variables (P = 0.05).
RESULTS
A total of 806 patients with the median age of 45 years (13-82) were included in the study. The sex ratio was 1:4.92 in favor of females. There were five instances of recurrent laryngeal nerve palsy but all of them recovered after 2 months. Eight patients reported a subjective change in quality of voice and voice fatigue but video stroboscopy or laryngeal electromyography were not done. These patients recovered when reviewed after 1 month. Four parathyroid glands were identified in 646 (80.14%) patients while only three parathyroid glands were identified in the 160 patients. There were 247 (30.6%) patients who had one or more risk factors likely to cause hypocalcaemia.
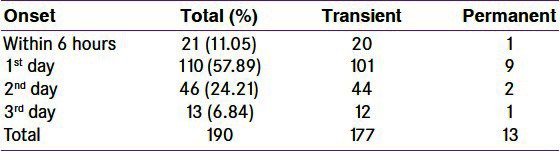
The mean value of preoperative serum corrected calcium was 8.901 mg (8-10.5) and at the time of discharge was 8.25 mg (6.1-10). The overall incidence of hypocalcaemia was 23.6% (n = 190) and that of permanent hypocalcaemia was 1.61% (n = 13). Symptomatic hypocalcaemia occurred in 10.91% (n = 88) patients. Hypocalcaemia was detected in the first 6 hours after operation in 21 patients (11.05%) and delayed up to 3rd postoperative day in 13 patients (6.84%) [Table 1]. One hundred and forty-four (75.78%) patients required calcium supplementation for 4 weeks while 2 patients required 20 weeks.
Table 1.
Time of onset of hypocalcaemia and relation to final outcome
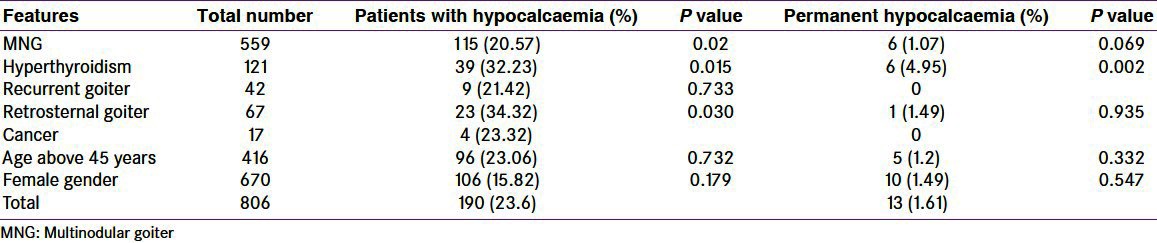
The high risk group showed an overall incidence 30.36% incidence of hypocalcaemia (n = 75; P = 0.003) and 2.4% incidence of permanent hypocalcaemia was (n = 6; P = 0.221). On analyzing various clinical situations independently, both transient and permanent hypocalcaemia were significantly associated with hyperthyroidism. Goiters with retrosternal extension showed significant incidence of transient hypocalcaemia (34.32%; P = 0.030) [Table 2].
Table 2.
Prevalence of hypocalcaemia in different clinical situations
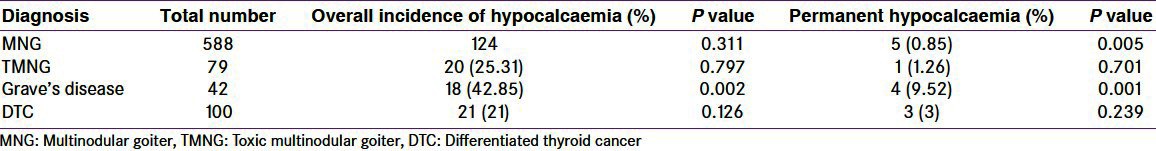
Frequency of hypocalcaemia noted in subgroups with different histological diagnosis is noted in Table 3. Thyroidectomy for Grave's disease was associated with high incidences of both transient (P = 0.002; OR = 2.581; {C.I.: 1.369-4.868}) and permanent hypocalcaemia (P = 0.001; OR = 8.830 {C.I.: 2.602-29.971}. In our series of 42 cases of Grave's disease, the sex ratio was 1:0.35 in favor of females. Permanent hypocalcaemia was noted in two patients of each group with no statistical difference (P = 0.293). Fifteen patients were above the age of 45 years and this group showed three patients with hypocalcaemia but failed to produce statistical impact (P = 0.393). Toxic nodular goiter (TNG) was not associated with significant incidence of hypocalcaemia (P = 0.797).[9]
Table 3.
Prevalence of hypocalcaemia in various pathological situations
There were 23 instances of incidental removal of parathyroid glands and hypocalcaemia occurred in 12 (52.17%) patients (P = 0.001). This subset also showed high incidence (n = 2; 8.69%) of permanent hypocalcaemia (P = 0.006; OR = 6.684; {C.I.: 1.394-32.056}) [Table 4]. On reviewing, there were 21 instances of single gland removal and 2 instances of two gland removal. On two occasions, the glands were found intra-thyroidal in location. Incidental removal of parathyroid gland had occurred in 19 instances of thyroidectomy for nontoxic nodular goiter.
Table 4.
Prevalence of hypocalcaemia in special situations
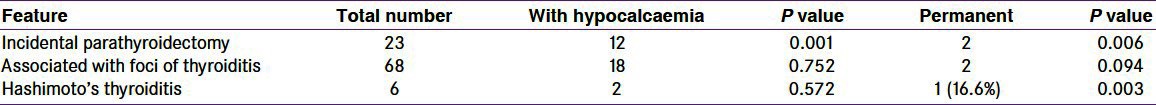
There were 6 patients with classic form of Hashimoto thyroiditis and 68 patients with foci of lymphocytic thyroiditis without extensive fibrosis or destruction of follicles. Permanent hypocalcaemia was significantly high in patients with classic Hashimoto's thyroiditis.[Table 4].
The intraoperative PTH assay was done in 155 patients as a validation study. Hypocalcaemia was noted in 33 patients (21.3%) and 4 (2.6%) patient of this subset developed permanent hypocalcaemia. The mean value of PTH was 32.1732 pg/ml, (1.20-65). 17 patients had PTH levels below 10 pg/ml. Low PTH levels correlated well with hypocalcaemia (P = 0.006) as well as permanent hypocalcaemia (P = 0.011). The sensitivity of the test was found to be 0.5, while specificity was 0.9. Also, the positive predictive value was 0.1176, while the negative predictive value was 0.9855.
DISCUSSION
Recent population studies showed 12% prevalence of palpable goiter in Kerala State, India.[10] Institutional statistics showed 76% of thyroid operations are for benign diseases which encompass large volume nodular goiters, recurrent nodular goiters, goiters with retrosternal extension, hyperthyroidism, and nodules with suspicious cytology.
Few observational studies had noted up to 50% of transient and 4% permanent hypocalcaemia after thyroidectomy.[11,12] Incidence of permanent hypocalcaemia noted in our series appears high compared to some other comparable series.[13,14] We did not appreciate significant association of hypocalcaemia with female gender or with advancing age unlike some previous observation.[15,16] Total thyroidectomy coupled with central compartment dissection was associated with high incidence of hypocalcaemia.[17,18] Inferior parathyroid glands are at risk of inadvertent removal or vascular damage during clearance of para-tracheal and pre-tracheal nodes in the central neck.[19] American Thyroid Association had revised the recommendation for central compartment dissection and suggested prophylactic dissection in selected cases only.[20]
The onset of hypocalcaemia was within 6 hours in 11.05% (n = 21) patients and was delayed up to 3rd post-operative day in 6.84% (n = 13) patients. It is interesting to note that one patient of each group developed permanent hypocalcaemia. The patient who developed permanent hypocalcaemia of the second group was operated for Grave's disease. There are reports of late onset hypocalcaemia following thyroidectomy for Grave's disease.[21] We presume that late onset hypocalcaemia may be delayed onset during the immediate postoperative period.
Operations for recurrent goiters did not cause significantly high incidences of hypocalcaemia unlike few previous studies.[22,23] Thyroidectomy for retrosternal goiters resulted in significant incidence of transient hypocalcaemia agreeing with one recent observation[24] Hypocalcaemia is relatively more common following thyroidectomy for hyperthyroidism. This feature was observed by Miche and colleagues as early as 1965.[2] There were 121 cases of hyperthyroidism which included 42 patients of Grave's disease and 79 patients of TNG. Hypocalcaemia was significantly associated with Grave's disease as noticed in some earlier studies.[21,25] In our series of 42 cases of Grave's disease incidences of hypocalcaemia was not related to sex but showed a trend toward age group >45 years.
Etiology of hypocalcaemia following thyroidectomy for Grave's Disease is still uncertain. Hyperthyroidism may lead on to loss of bone mineral density.[26] Transient hypocalcaemia may be related to osteodystrophy seen in hyperthyroidism. But thyroidectomy for TNG was not associated with significant high incidences of transient or permanent hypocalcaemia. Thrombosis of the parathyroid arteries following manipulations during surgical procedures may cause ischemic damage. Surgical procedure may induce thrombosis of parathyroid vessels due to autoimmune background of Grave's disease.[13] But we did not appreciate significant association of hypocalcaemia when thyroidectomy was performed for nodular goiter or differentiated thyroid cancer (DTC) expressing areas of lymphocytic thyroiditis. But hypocalcaemia was significantly high in a small subset of classic Hashimoto thyroiditis unlike one previous observation.[27] High incidence of hypocalcaemia in both subsets may be related to the autoimmunity associated with both conditions. The observation that concurrent active orbitopathy was found to potentiate the chance of post-operative hypocalcaemia in Grave's disease[28] underlines the above postulation.
The occurrence of a latent, insidious form of parathyroid insufficiency was first emphasized by Fourman (1). Patients with this syndrome have calcium levels in the low normal range, but develop hypocalcaemia in response to an EDTA infusion stress test. All patients who had postoperative hypocalcaemia were followed up for 12 months but we could not appreciate delayed parathyroid insufficiency. But we did not perform the stress test.
A higher incidence of hypocalcaemia was noted in nontoxic nodular goiters but was associated with incidental parathyroidectomy. Many previous studies felt that accidental removal of parathyroid gland was not associated with postoperative hypocalcaemia.[2,29] But we noticed that incidental removal of the gland was significantly associated with hypocalcaemia. This feature was interestingly noted along with nontoxic nodular goiters without risk factors. So we feel that a refinement in the surgical technique could have improved the outcome.
Blood supply of parathyroid glands was discussed in detail by William Halsted as early as 1907.[30] The capsular dissection technique of mobilization ensures intact parathyroid glands with vascular pedicles. Thomusch et al. noted lateral ligation of inferior thyroid arteries (ITA) as a strong determinant of hypocalcaemia.[31] But in one observational study, lateral ligation of the trunk of ITA did not cause significant hypocalcaemia following subtotal thyroidectomy for Grave's disease.[32] This observation indicates an additional blood supply apart from the branches of ITA, possibly from thyroid gland itself.
The intraoperative assay of intact PTH is a good tool in predicting post-operative hypocalcaemia and is recommended by AES guidelines. We noted low sensitivity but high specificity for this costly investigation. Moreover, the aim of the surgeon is to prevent complications rather than predict the possibility.
CONCLUSION
Refined surgical techniques can lower the incidence of post-thyroidectomy hypocalcaemia. Preservation of parathyroid glands is essential to avoid this complication. Thyroidectomy for Grave's disease has higher incidence of hypocalcaemia and so may be resorted to selected patients only.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Wade JS, Fourman P, Deane L. Recovery of parathyroid function in patients with transient hypoparathyroidism after thyroidectomy. Br J Surg. 1965;52:493–6. doi: 10.1002/bjs.1800520704. [DOI] [PubMed] [Google Scholar]
- 2.Michie W, Stowers JM, Frazer SC, Gunn A. Thyroidectomy and the Parathyroids. Br J Surg. 1965;52:503–14. doi: 10.1002/bjs.1800520706. [DOI] [PubMed] [Google Scholar]
- 3.Delbridge L. Total Thyroidectomy: The evolution of surgical technique. ANZ J Surg. 2003;73:761–8. doi: 10.1046/j.1445-2197.2003.02756.x. [DOI] [PubMed] [Google Scholar]
- 4.Bliss RD, Gauger PG, Delbridge LW. Surgeon's approach to thyroid gland-Anatomy and surgical technique. World J Surg. 2000;24:891–7. doi: 10.1007/s002680010173. [DOI] [PubMed] [Google Scholar]
- 5.AES Guidelines 06/01 Group. Australian Endocrine Surgeons Guidelines, AES06/01. Postoperative Parathyroid Hormone Measurement and Early Discharge after Total thyroidectomy: Analysis of Australian Data And Management Recommendation. ANZ J Surg. 2007;77:199–202. doi: 10.1111/j.1445-2197.2007.04018.x. [DOI] [PubMed] [Google Scholar]
- 6.Thomusch O, Machens A, Sekulla C, Ukkat J, Lippert H, Gastinger I, et al. Multivariate analysis of risk factors for postoperative complications in benign goiter surgery: Prospective multicenter study in Germany. World J Surg. 2000;24:1335–41. doi: 10.1007/s002680010221. [DOI] [PubMed] [Google Scholar]
- 7.Zambudio AR, Rodríguez J, Riquelme J, Soria T, Canteras M, Parrilla P. Prospective study of postoperative complications after total thyroidectomy for multinodulargoiters by surgeons with experience in endocrine surgery. Ann Surg. 2004;240:18–25. doi: 10.1097/01.sla.0000129357.58265.3c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wingert DJ, Friesen SR, Iliopoulos JI, Pierce GE, Thomas JH, Hermreck AS. Post-thyroidectomy hypocalcemia. Incidence and risk factors. Am J Surg. 1986;152:606–10. doi: 10.1016/0002-9610(86)90435-6. [DOI] [PubMed] [Google Scholar]
- 9.Riju R, Jadhav S, Kanthaswamy R, Jacob P, Nair CG. Is total thyroidectomy justified in multinodulargoitre. J Indian Med Assoc. 2009;107:223–5. [PubMed] [Google Scholar]
- 10.Usha Menon V, Sundaram KR, Unnikrishnan AG, Jayakumar RV, Nair V, Kumar H. High prevalence of undetected thyroid disorders in an iodine sufficient adult in south Indian population. J Indian Med Assoc. 2009;107:72–7. [PubMed] [Google Scholar]
- 11.Shaha AR, Jaffe BM. Parathyroid preservation during thyroidectomy. Am J Otolaryngol. 1998;19:113–7. doi: 10.1016/s0196-0709(98)90106-5. [DOI] [PubMed] [Google Scholar]
- 12.Demeester-Mirkine N, Hooghe L, Van Geertruyden J, De Maertelaer V. Hypocalcemia after thyroidectomy. Arch Surg. 1992;127:854–8. doi: 10.1001/archsurg.1992.01420070118021. [DOI] [PubMed] [Google Scholar]
- 13.Delbridge L, Guinea AI, Reeve TS. Total Thyroidectomy for Bilateral Benign Multinodular Goiter, Effect of Changing Practice. Arch Surg. 1999;134:1389–93. doi: 10.1001/archsurg.134.12.1389. [DOI] [PubMed] [Google Scholar]
- 14.Reeve TS, Curtin A, Fingleton L, Kennedy P, Mackie W, Porter T, et al. Can total thyroidectomy be performed as safely by general surgeons in provincial centers as by surgeons in specialized endocrine surgical units? making the case for surgical training. Arch Surg. 1994;129:834–6. doi: 10.1001/archsurg.1994.01420320060011. [DOI] [PubMed] [Google Scholar]
- 15.Abboud B, Sargi Z, Akkam M, Sleilaty F. Risk Factors for Postthyroidectomy Hypocalcemia. J Am Coll Surg. 2002;195:456–61. doi: 10.1016/s1072-7515(02)01310-8. [DOI] [PubMed] [Google Scholar]
- 16.Bhattacharyya N, Fried MP. Assessment of the Morbidity and Complicationsof Total Thyroidectomy. Arch Otolaryngol Head Neck Surg. 2002;128:389–92. doi: 10.1001/archotol.128.4.389. [DOI] [PubMed] [Google Scholar]
- 17.Chisholm EJ, Kulinskaya E, Tolley NS. Systematic review and meta-analysis of the adverse effects of thyroidectomy combined with central neck dissection as compared with thyroidectomy alone. Laryngoscope. 2009;119:1135–9. doi: 10.1002/lary.20236. [DOI] [PubMed] [Google Scholar]
- 18.Henry JF, Gramatica L, Denizot A, Kvachenyuk A, Puccini M, Defechereux T. Morbidity of prophylactic lymph node dissection in central neck area in patients with papillary thyroid carcinoma. Langenbecks Arch Surg. 1998;383:167–9. doi: 10.1007/s004230050111. [DOI] [PubMed] [Google Scholar]
- 19.Carty SE, Cooper DS, Doherty GM, Duh QY, Kloos RT, Mandel SJ, et al. Consensus statement on the terminology and classification of central neck dissection for thyroid cancer. Thyroid. 2009;19:1053–8. doi: 10.1089/thy.2009.0159. [DOI] [PubMed] [Google Scholar]
- 20.Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–214. doi: 10.1089/thy.2009.0110. [DOI] [PubMed] [Google Scholar]
- 21.Gann DS, Paone JF. Delayed hypocalcemia after thyroidectomy for Graves’ disease is prevented by parathyroid autotransplantation. Ann Surg. 1979;190:508–13. doi: 10.1097/00000658-197910000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lefevre JH, Tresallet C, Leenhardt L, Jublanc C, Chigot JP, Menegaux F. Reoperative surgery for thyroid disease. Langenbecks Arch Surg. 2007;392:685–91. doi: 10.1007/s00423-007-0201-6. [DOI] [PubMed] [Google Scholar]
- 23.Menegaux F, Turpin G, Dahman M, Leenhardt L, Chadarevian R, Aurengo A, et al. Secondary thyroidectomy in patients with prior thyroid surgery for benign disease: A study of 203 cases. Surgery. 1999;126:479–83. [PubMed] [Google Scholar]
- 24.Abboud B, Sleilaty G, Mallak N, AbouZeid H, Tabchy B. Morbidity and mortality of thyroidectomy for substernal goiter. Head Neck. 2010;32:744–9. doi: 10.1002/hed.21246. [DOI] [PubMed] [Google Scholar]
- 25.Pesce CE, Shiue Z, Tsai HL, Umbricht CB, Tufano RP, Dackiw AP, et al. Postoperative hypocalcemia after thyroidectomy for Graves’ disease. Thyroid. 2010;20:1279–83. doi: 10.1089/thy.2010.0047. [DOI] [PubMed] [Google Scholar]
- 26.Mosekilde L, Eriksen EF, Charles P. Effects of thyroid hormones on bone and mineral metabolism. Endocrinol Metab Clin North Am. 1990;19:35–63. [PubMed] [Google Scholar]
- 27.Shih ML, Lee JA, Hsieh CB, Yu JC, Liu HD, Kebebew E, et al. Thyroidectomy for Hashimoto's thyroiditis: Complications and associated cancers. Thyroid. 2008;18:729–34. doi: 10.1089/thy.2007.0384. [DOI] [PubMed] [Google Scholar]
- 28.Hassan I, Danila R, Maurer E, Osei-Agymang T, Zielke A. Severe Graves’ ophthalmopathy may be a risk factor for the development of postthyroidectomy hypocalcaemia. Exp Clin Endocrinol Diabetes. 2008;116:614–8. doi: 10.1055/s-2008-1065333. [DOI] [PubMed] [Google Scholar]
- 29.Manouras A, Markogiannakis H, Lagoudianakis E, Antonakis P, Genetzakis M, Papadima A, et al. Unintentional parathyroidectomy during total thyroidectomy. Head Neck. 2008;30:497–502. doi: 10.1002/hed.20728. [DOI] [PubMed] [Google Scholar]
- 30.Halsted WS, Evans HM. The Parathyroid Glandules. Their blood supply and their preservation in operation upon the thyroid gland. Ann Surg. 1907;46:489–506. doi: 10.1097/00000658-190710000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thomusch O, Machens A, Sekulla C, Ukkat J, Brauckhoff M, Dralle H. The impact of surgical technique on postoperative hypoparathyroidism in bilateral thyroid surgery: A multivariate analysis of 5846 consecutive patients. Surgery. 2003;133:180–5. doi: 10.1067/msy.2003.61. [DOI] [PubMed] [Google Scholar]
- 32.Araujo Filho VJ, Silva Filho GB, Brandão LG, Santos LR, Ferraz AR. The importance of the ligation of the inferior thyroid artery in parathyroid function after subtotal thyroidectomy. Rev Hosp Clin Fac Med Sao Paulo. 2000;55:113–20. doi: 10.1590/s0041-87812000000400002. [DOI] [PubMed] [Google Scholar]


