Abstract
Primary hypothyroidism is a common endocrine diseases and in recent times with increased awareness of thyroid diseases among internists, gynecologists and primary care physicians the number of patients with thyroid dysfunction seems increasing. During Ramadan, often patients find it difficult to administer levothyroxine on empty stomach since they may not wake up so early, so in this article suggestion has been given to take it at bed time. We conducted a prospective observational study during this year's holy month of Ramadan on patients enrolled from our thyroid clinic who had hypothyroidism and decided to undertake fasting. Our aim was to study the impact of bed time levothyroxine on TSH (thyroid stimulating hormone) levels.
Keywords: Hypothyroidism, levothyroxine replacement, ramadan
INTRODUCTION
Primary hypothyroidism is a common endocrine disease and in recent times, with increased awareness of thyroid diseases among internists, gynecologists, and primary care physicians, the number of patients with thyroid dysfunction seems increasing. Patients who need levothyroxine replacement are advised to take it in fasting state since it has been proved by many studies that optimal levothyroxine absorption takes place under fasting conditions.[1,2] Non-fasting regimens of levothyroxine administration are associated with higher and more variable serum TSH concentrations. Although, the study done by Bolk, et al.[3] demonstrated lower serum TSH (Thyroid stimulating hormone) concentrations when levothyroxine was taken at bedtime, and another study by Rajput, et al.[4] also proved that evening dose of levothyroxine had equal lowering effect on TSH as compared to morning dose. In contrast, a randomized crossover trial[5] in the US compared taking levothyroxine in the fasting state, with breakfast, or at bedtime in 65 patients with primary hypothyroidism and thyroid cancer, and found that fasting state is most beneficial than at other times. Bhutani, et al.[6] have also shown subjective improvement with change in timing and frequency of levothyroxine administration.
Being a minority institution, most of our patient population is Muslim by religion; during Ramadan, often patients find it difficult to administer levothyroxine on empty stomach since they may not wake up so early. In the article by Raza, et al.,[7] considering the suggestion for levothyroxine timing during Ramadan, we planned this study to assess the changes in TSH if levothyroxine is supplemented at bed time.
MATERIALS AND METHODS
We conducted a prospective observational study during holy month of Ramadan fell in July- August 2012 on patients enrolled from our thyroid clinic who had hypothyroidism and decided to undertake fasting. Our aim was to study the impact of bedtime levothyroxine supplementation on TSH levels. The week prior to Ramadan, we selected 47 patients with euthyroid status who had stable dose of levothyroxine for last 6 months. All of these patients were advised to take levothyroxine at bedtime. They were instructed to take their levothyroxine at least 2 hours after dinner. None of the patient was taking drugs such as anti-epileptics, rifampicin, cholestyramine, sucralfate, antacids, raloxifen, steroids, iron or calcium preparations. They were told to avoid soya products. We excluded those patients who had end-stage target organ diseases. Data were collected regarding the age, gender, duration of disease, thyroid peroxidase (TPO), antibodies positivity status, time interval between dinner and levothyroxine administration, concomitant illnesses and therapy. At the end of Ramadan fasting, all patients were called back for TSH measurement.
Statistical analysis
All data in the text and tables are expressed as mean ± SD. For comparison of baseline demographic and clinical characteristics in-between the groups, an unpaired Students ‘t’ test was used. All Statistical analysis was done by using the statistical package for social sciences (SPSS 15.0 version) with P < 0.05 taken as statistically significant.
RESULTS
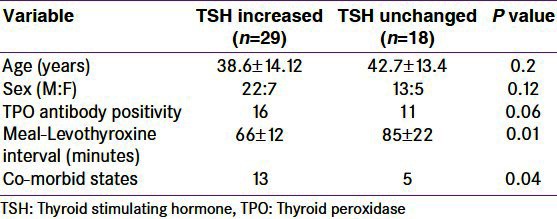
The overall variation of TSH was ranging from 0.6 to 8 (2.4 ± 2.1) miu/l. We found 29/47 patients showed higher TSH values (≥2 miu/l) while 18/47 patients had, 2 miu/l variation in TSH than their pre-Ramadan assessment. The characteristics of the patients in the two groups have been shown in Table 1. The meal-levothyroxine interval and concomitant illnesses were significantly different in two groups. The variation in TSH had significant correlation with meal-levothyroxine interval (r = -0.32, P = 0.01).
Table 1.
Clinical characteristics of study participants
DISCUSSION
We collected data on the exact interval between dinner and levothyroxine ingestion in the bedtime-dosing subjects, and we found nearly 75% patients could not keep interval of 2 hours between dinner and drug. Meal-dose intervals of greater than 2 hours may be necessary to assure an empty stomach at the time of levothyroxine ingestion, particularly when the preceding evening meal contained solid and/or fatty foods. During Ramadan, consumption of fat and fiber-rich food increases. The other reasons behind the higher TSH values may be drug interactions. Certain drugs such as oral hypoglycemic, anti-hypertensive, statins, anti-platelet drugs, proton pump inhibitors may interfere with levothyroxine absorption.
Interestingly, there was a significant subset of patients in whom the TSH concentration did not change by more than 1 miu/liter. In fact, many patients had TSH values that were within 0.1-0.2 mIU/liter of each other. For other patients, bedtime regimen resulted in considerable increase in TSH values. It is possible that such divergent results were either due to individual patient characteristics or consumption of different foods. However, it is plausible that meals with different carbohydrate, protein, or fat content are associated with different degrees of impact on LT4 absorption and TSH levels. Alternatively, there might be a subset of patients whose TSH concentrations, for other reasons, are less affected by the timing of LT4 ingestion. If either were the case, identification of these conditions or patients would be important because this may allow a less stringent LT4 timing regimen. There are many shortcomings in our study. Time interval in some patients between the TSH measurement was less than 6 weeks. We were unable to collect pharmacokinetic data. We did not take into account any symptomatology or quality of life measures.
CONCLUSION
Bedtime dose can be appropriate for hypothyroid patients during Ramadan fasting or in other times also, but there should be an interval of minimum 2 hours since the last meal. Frequent and close monitoring is needed for those who need to keep TSH in narrow range such as pregnant, elderly, and those who have osteoporosis.
Footnotes
Source of Support: Nil
Conflict of Interest: No
REFERENCES
- 1.Fish LH, Schwartz HL, Cavanaugh J, Steffes MW, Bantle JP, Oppenheimer JH. Replacement dose, metabolism and bioavailability of levothyroxine in the treatment of hypothyroidism. N Engl J Med. 1987;316:764–70. doi: 10.1056/NEJM198703263161302. [DOI] [PubMed] [Google Scholar]
- 2.Hays MT, Hays MT. Localization of human thyroxine absorption. Thyroid. 1991;1:241–8. doi: 10.1089/thy.1991.1.241. [DOI] [PubMed] [Google Scholar]
- 3.Bolk N, Visser TJ, Kalsbeek A, van Domburg RT, Berghout A. Effects of evening vs morning thyroxine ingestion on serum thyroid hormone profiles in hypothyroid patients. Clin Endocrinol (Oxf) 2007;66:43–8. doi: 10.1111/j.1365-2265.2006.02681.x. [DOI] [PubMed] [Google Scholar]
- 4.Rajput R, Chatterjee S, Rajput M. Can levothyroxine be taken as evening dose? Comparative evaluation of morning versus evening dose of levothyroxine in treatment of hypothyroidism. J Thyroid Res. 2011;2011:505239. doi: 10.4061/2011/505239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bach-Huynh TG, Nayak B, Loh J, Soldin S, Jonklaas J. Timing of levothyroxine administration affects serum thyrotropin concentration. J Clin Endocrinol Metab. 2009;94:3905–12. doi: 10.1210/jc.2009-0860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhutani S, Bhutani J, Balhara YP, Kalra S. Atypical thyroxine replacement in hypothyroidism: A clinical audit. Thyroid Res Pract. 2012;9:81–3. Available from: http://www.thetrp.net/text.asp?2012/9/3/81/99648 . [Google Scholar]
- 7.Raza SA, Ishtiaq O, Unnikrishnan AG, Khan AK, Ahmad J, Ganie MA, et al. Thyroid diseases and Ramadan. Indian J Endocrinol Metab. 2012;16:522–4. doi: 10.4103/2230-8210.98001. [DOI] [PMC free article] [PubMed] [Google Scholar]


