Sir,
Ectopic thyroid tissue (ETT) is a rare congenital anomaly defined as thyroid tissue not located anterolaterally from the second to the fourth tracheal cartilage. ETT may occur anywhere along the path of descent of the thyroid. It is very unusual for two distinct foci of ETT to be present simultaneously.[1]
An 8-year-old boy presented to his physician with complaints of constipation and generalized weakness. Parents also complained about his stunted growth. His academic performance was average. Considering his history complete hormonal profile was ordered, which showed thyroid stimulating hormone value of 131 μIU/ml (Normal 0.5-5.0 μIU/ml), T3 – 110 ng/ml (Normal 80-230 ng/dl), T4 – 6.4 mcg/dl (Normal 7-14 mcg/dl). Rest of the hormonal profile was unremarkable. Neck sonography failed to reveal thyroid tissue in the pretracheal region. With this information, thyroid ectopia was suspected and so patient was referred for thyroid scan. His planar scan [Figure 1] demonstrated two foci of increased tracer uptake, one at the base of tongue (white arrow) and other in submandibular region (red arrow). There was no tracer uptake in the thyroid bed. Single photon emission tomography-computed tomography (SPECT-CT) imaging [Figure 2] localized these two distinct pertechnetate-avid foci to enhancing, hyperdense soft tissues measuring 9 × 9 mm at the base of tongue (white arrow) and other measuring 8 × 7 mm in submandibular-prehyoid region (red arrow). Considering pertechnetate avidity and enhancement on noncontrast CT, a diagnosis of dual ectopic thyroid was made. Patient had no complaints of pressure or obstruction in neck. The patient is started on thyroid hormone replacement therapy with levothyroxine and is advised regular follow-up.
Figure 1.
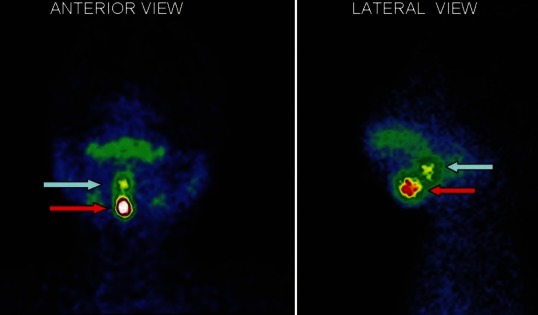
Tc-99m pertechnetate scan of an 8-year-old boy, with suspected thyroid ectopia. His planar scan (Figure 1) demonstrated two foci of increased tracer uptake, one at the base of tongue (white arrow) and other in submandibular region (red arrow). There was no tracer uptake in the thyroid bed. These features were highly suggestive of dual ectopic thyroid.
Figure 2.
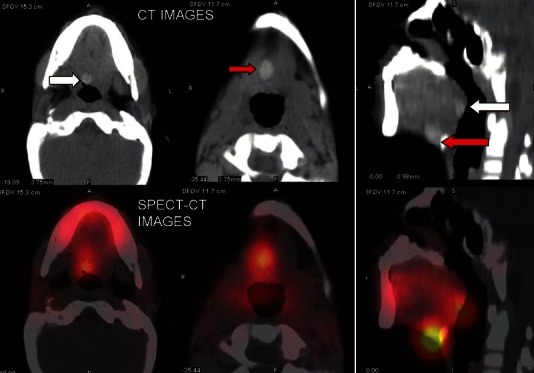
SPECT-CT images of Tc-99m pertechnetate scan. The scan localized two distinct pertechnetate-avid foci to enhancing, hyperdense soft tissues measuring 9 × 9 mm at the base of tongue (white arrow) and other measuring 8 × 7 mm in submandibular-prehyoid region (red arrow). Considering pertechnetate avidity and enhancement on noncontrast CT, a diagnosis of dual ectopic thyroid was made.
Hormone production from ETT is usually insufficient, leading either to a subclinical or clinical hypothyroid state. The incidence of clinical hypothyroidism with ETT varies from 24 to 60%. Usually the patients complain of a palpable mass, growth retardation and lump sensation in the throat. Patients may have dyspnea, stridor or cough due to intratracheal thyroid gland. Adolescents and young adults may present with slow heart rate, chronic tiredness, cold intolerance, constipation, mental fatigue, difficulty in learning, obesity, scholastic problems and delayed sexual maturation.[2]
Lifelong thyroxine therapy is required according to individual thyroid status after establishing the diagnosis. It helps in achieving the euthyroid status as well as decreasing the size of ectopic thyroid swelling by lowering the elevated TSH level.[3] Surgery is usually not done, since the ectopic thyroid may be the only functioning tissue in the body. It is indicated if the patient has pressure or obstructive symptoms, or there is suspicion of malignancy in ETT. At times ectopic thyroid of these patients are excised when they present with mass in neck region, rendering them frankly hypothyroid as against subclinical hypothyroid state that they were suffering from earlier.[4] Hence, possibility of ectopic thyroid should be kept in mind and evaluated accordingly. Dual ectopic thyroid is an extremely rare occurrence with around 30 cases reported worldwide so far. The majority of dual ectopics were shown to be in the neck and rarely away from the line of descent.[1,5]
Radionuclide studies are highly sensitive and specific in demonstrating the functional tissues in patients with ectopic thyroid.[1] Tc-99m pertechnetate scan is a well-known method for evaluating the size, distribution and activity of thyroid and distinguishing it from other tissues in the head and neck and superior mediastinum. Single photon emission tomography-computed tomography (SPECT-CT) is an example of fusion imaging where functional information of nuclear medicine and anatomical information of radiology can be evaluated together. On CT thyroid tissue has an attenuation coefficient higher than that of muscle, which is thought to be due to high iodine content in thyroid tissue.
We suggest a thyroid scan and if available SPECT/CT should be performed in all cases of suspected thyroid ectopia before any intervention is performed. Although rare, the possibility of ETT should be kept in mind whenever similar clinical scenarios are encountered.
REFERENCES
- 1.Sood A, Seam RK, Gupta M, Sharma D, Bhardwaj P. Dual ectopic thyroid: A case report with review of literature. Iran J Radiol. 2011;8:29–32. [PMC free article] [PubMed] [Google Scholar]
- 2.Dalla JS, Foley TP. Sperling MA. Pediatric Endocrinology. 3rd ed. Philadephia, PA: WB Saunders Co; 1996. Hypothyroidism; pp. 391–9. [Google Scholar]
- 3.Rovet JF. Children with congenital hypothyroidism and their siblings: Do they really differ? Pediatrics. 2005;115:e52–7. doi: 10.1542/peds.2004-1492. [DOI] [PubMed] [Google Scholar]
- 4.Sood A, Kumar R. The ectopic thyroid gland and the role of nuclear medicine techniques in its diagnosis and management. Hell J Nucl Med. 2008;11:168–71. [PubMed] [Google Scholar]
- 5.Jain A, Pathak S. Rare developmental abnormalities of thyroid gland, especially multiple ectopia: A review and our experience. Indian J Nucl Med. 2010;25:143–6. doi: 10.4103/0972-3919.78248. [DOI] [PMC free article] [PubMed] [Google Scholar]


