Abstract
Aneurysmal arterial disease is a vascular degenerative condition that is distinct from atherosclerotic and other occlusive arterial diseases. There is regionalization of the predisposition to aneurysm formation within the vascular tree, and the pathologic process varies with location. Infrarenal abdominal aortic aneurysm (AAA) is the most common manifestation of aneurysmal disease, and smoking is the dominant risk factor. Smoking is a much greater risk factor for AAA than for atherosclerosis. In addition to playing a role in the etiology of AAA, smoking also increases the rate of expansion and risk of rupture of established AAA. The mechanistic relationship between AAA and smoking is being established with the use of enhanced animal models that are dependent on smoke or smoke components. The mechanisms appear to involve durable alterations in vascular smooth muscle cell and inflammatory cell function. This review will examine the clinical, epidemiological and mechanistic evidence implicating smoking as a cause of aneurysms, focusing on AAA.
Aneurysmal arterial disease is clinically, histologically and mechanistically quite distinct from atherosclerosis and other occlusive arterial disease. Although atherosclerotic change may be seen in many aneurysms the relationship is not necessarily a causal one. Aneurysms are more common in some arteries than others and their etiology varies by location with, for example, hypertension dominating in cerebral arteries, genetic factors dominating in the ascending aorta and smoking dominating in the abdominal aorta. (1) Given the importance of smoking in abdominal aortic aneurysm (AAA) this review will focus on AAA. Although there is less evidence implicating smoking in other manifestations of aneurysmal disease, this does not exclude a role for smoking in the development or progression of other aneurysms.
Clinical and epidemiological studies of smoking and AAA
Smoking increases prevalence and incidence
All epidemiological studies of AAA have identified the importance of smoking as a risk factor. Smoking is a very strong risk factor for the presence of an AAA in both men and women with odds ratios ranging from 3–12.(2, 3) In the large (n=114,567) Aneurysm Detection and Management (ADAM) screening study, a history of ever smoking was associated with an odds ratio (OR) of 2.97 (95%CI 2.65, 3.32) for 3–3.9cm AAAs and 5.07 (95%CI 4.13, 6.21) for ≥4cm AAAs.(2) Smoking was considered to be responsible for 75% of the excess prevalence of AAAs ≥4cm. In a recent report of screening 22,187 Swedish men aged 65 years, 87% of men with AAA were current or ex-smokers and smoking was the dominant risk factor for AAA (OR 3.5; 95%CI 2.4, 5.1).(4)
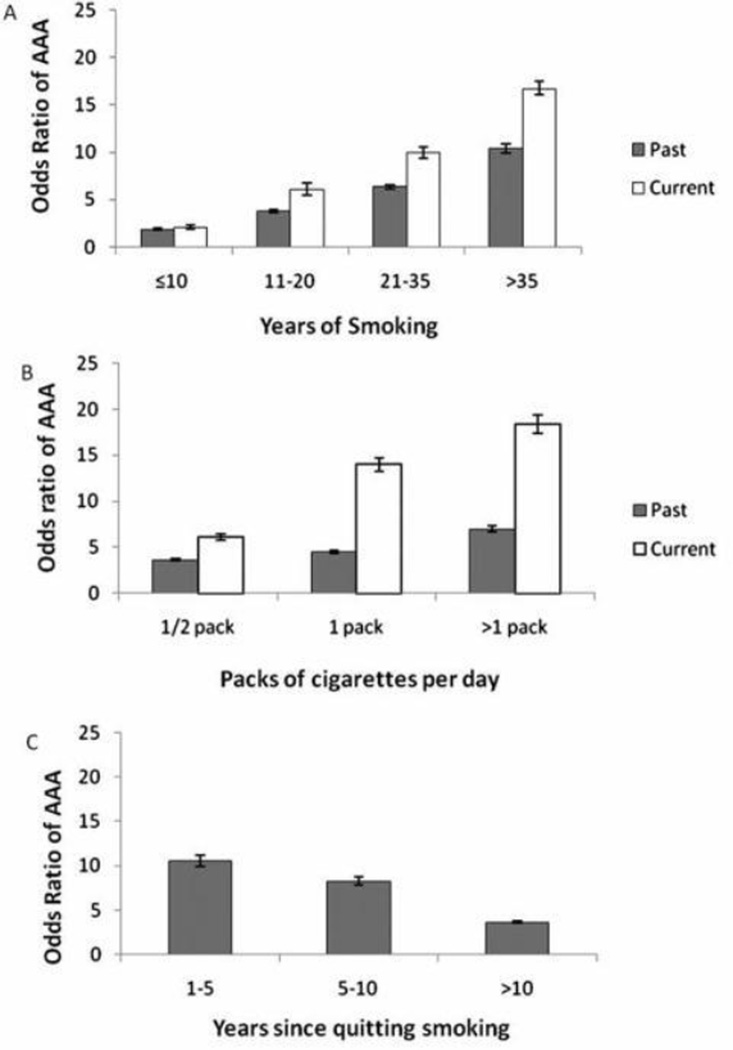
Results from a screening study of over 3 million individuals in the US showed that there was a clear relationship between prevalent AAA and both duration and amount of smoking. (Figure 1) (5) There is evidence of a strong linear dose response effect with duration of smoking.(2, 5, 6) The relationship with amount smoked is also linear in current smokers and to a lesser extent with ex-smokers.(5, 6) In ex-smokers, duration appears to be more important than level of exposure. (5, 6)
Figure 1.
Age-adjusted effects of smoking on the risk of abdominal aortic aneurysm (AAA). Reference groups are nonsmokers for all smoking variables. The vertical error bars show 95% CIs. Adapted with permission from Kent et al.5
The magnitude of risk with smoking eclipses all other modifiable risk factors for prevalent AAA. Intriguingly, smoking appears to be a substantially greater risk factor for AAA than for occlusive atherosclerotic disease. In a systematic review by Lederle et althe association between smoking and AAA was 2.5 (95%CI 2.2, 2.8) times greater than the association between smoking and coronary heart disease.(7) The divergent effect of smoking on these two vascular diseases supports the distinct pathogenesis of aneurysmal and occlusive arterial disease. The US Preventive Services Task Force considered smoking a sufficiently dominant risk factor for AAA to recommend screening men aged 65 to 75 years who have ever smoked – rather than all men of that age. (8) Kent et al have demonstrated that the efficiency of screening can be improved using algorithms based on risk factors such as smoking. (5) However, other studies have not supported selective screening based on risk factors.(9, 10)
Although AAA is less common in women, outcomes appear to be worse in women with AAA compared to men with AAA (11). There is some evidence smoking may be a greater risk factor for AAA in women than in men. In the Rotterdam Study 56% of women with AAA were current smokers compared to 38% of men. (12) In the ADAM study the OR for ever smoking was 3.8 (95%CI 1.57, 9.20) in women compared to 3.34 (95%CI 3.04, 3.67) in men. (13) It is unclear how important these differences are.
Smoking is also the dominant factor for incident AAA. In a prospective analysis of the Tromsø study there was a dose response effect with both smoking duration and quantity.(14) Even individuals who had stopped smoking 10–19 years earlier had nearly a three-fold risk of an incident AAA compared to non-smokers. This suggests that smoking has a durable influence on AAA formation. This has also been seen in recent experimental studies (see below).
Smoking increases expansion rate and rupture risk
Smoking is an important cause of progression of AAA. Continued smoking in individuals with an AAA is associated with both increased rates of expansion and the risk of rupture. In a recent meta-analysis using data from 15,475 patients with small (3–5.5cm) AAAs, current smoking was associated with an increased rate of expansion of 0.35 (95%CI 0.23, 0.48) mm/year.(15) In the UK Small Aneurysm Trial, current smoking doubled of the risk of rupture, although this was not statistically significant, with a Hazard Ratio (HR) of 2.11 (95%CI 0.95, 4.67).(16) However, this doubling of risk was confirmed as significant in a recent meta-analysis with an HR of 2.02 (95%CI 1.33–3.06) for current smoking vs ex/never smoker – an effect that was independent of aneurysmal diameter.(15)
Influence of smoking on intervention and prognosis
Smoking is relevant when patients require intervention for AAA. For patients undergoing surgical intervention for AAA, current smoking is likely to increase the risk of peri-operative death and late mortality. In the UK Small Aneurysm Trial, continued smoking one year after randomization was associated with significantly increased mortality (HR 3.23; 95%CI 1.73, 6.03).(17) Although smokers are less likely to develop an endoleak following endovascular repair (presumably due to pro-thrombotic effects), they are at increased risk of stent migration. (18)
The recently documented decline in incidence of AAA interventions and deaths and the lower than expected prevalence in screening studies has been attributed to falling rates of smoking.(4, 19, 20) Smoking cessation is associated with a decline in risk of an AAA of about 30% for each decade after quitting (Figure 1).(2, 5, 6) Nevertheless, the legacy of increased risk of AAA from smoking lasts many decades. (14)
Mechanistic studies of smoking and aneurysm formation
The most striking feature of AAA histology is the loss of normal medial arterial structure and, in particular, the near complete absence of a normal lamellar elastin matrix, a feature that it has in common with chronic obstructive pulmonary disease.(21) In the aorta, these matrix changes are attributed to three general features which are believed to be interrelated: 1) elaboration of high levels of proteases, 2) chronic inflammatory infiltration and 3) loss/dysfunction of parenchymal cells central to matrix deposition and repair.
Although considerable research with human tissue and animal models over the past two decades has begun to inform our understanding of the initiation and progression of AAA, we have yet to develop and verify an effective biologic therapeutic which will interrupt development of an AAA or halt the growth of a small AAA. However, given the importance of smoking as a risk factor, there has until recently, been very little work on the effects of smoke exposure in these models. Because of the complex make-up of tobacco smoke (TS) and the variety of intermediaries which may be involved, the effects on the vasculature could be mediated through alterations of the inflammatory response, of resident vascular smooth muscle cells (VSMC) function, or of the vessel matrix itself. Several different experimental approaches have been taken to determine the mechanisms of AAA formation related to smoking (Table).
Table.
Mechanistic Studies of Smoking Components and AAA
| Smoke Component | Study Design | Potential Mechanism | Source |
|---|---|---|---|
| Whole smoke | Circulating inflammatory markers in humans with AAA | Increased tPA in smokers which could activate proteases | 22 |
| Whole smoke | Genome-wide association study in humans | Association of smoke and AAA on 3p12.3 and epigenetic modifications | 23–25 |
| Water-soluble smoke extract | Human VSMC | Suppression of prolyl-4-hydroxylase | 27 |
| Water-soluble smoke extract | Human neutrophils, endothelial cells, and VSMC | Increased MMP production | 27,28 |
| Nicotine | VSMC and inflammatory cells | Multiple | 29 |
| Nicotine | Mouse (ApoE-deficient) model of AAA | AMP-activated protein kinase α2 | 30 |
| Nicotine | Mouse (ApoE-deficient and elastase perfusion) model of AAA | miR-21 (also associated with stabilization of aortic dilation) | 31 |
| Whole smoke | Mouse (ApoE-deficient) model of AAA | Increased MMP gene expression | 32 |
| Whole smoke | Mouse (modified elastase perfusion) model of AAA | Altered T-cell response | 33 |
AAA indicates abdominal aortic aneurysm; tPA, tissue plasminogen activator; VSMC, vascular smooth muscle cells; and MMP, matrix metalloproteinase.
Human Studies
There are many challenges to evaluating the mechanistic effects of smoking on AAA formation in humans. When looking at the associations of various circulating markers in patients with AAA, Lindholt et al came to the conclusion that smoking may activate tissue plasminogen activator (tPA).(22) Since tPA is a potent activator of elastolytic MMP, this could link smoking to aortic elastolysis. In support of this, others have shown endothelial response to serum from smokers to result in increased tPA without increased plasminogen activator inhibitor-1 or tissue factor pathway inhibitor-1.(23)
Genetic variants associated with AAA have also shown potential interactions with smoking. One genome wide association study found a variant on 3p12.3 which demonstrated that the genetic risk was significantly greater in those with a history of smoking.(24) Other studies, however, have not shown a clear relationship between smoking, genetic variants and AAA.(25) It is also possible that smoking contributes to the pathogenesis of AAA via epigenetic interactions although conclusive evidence about this is still lacking.(26)
Studies of smoke components
Since the matrix changes in the aorta bear some resemblance to those in the lung, some studies have begun with a presumption that the mechanisms are likely to be similar. Employing techniques successfully used to define similar pathologic processes induced by TS in the lung,(27–33) these studies have attempted to develop a mechanistic understanding of TS on vascular biology. Typically these studies have relied primarily on gross extracts or purified specific components of TS applied in vivo or to tissues or cells.
Using a water-soluble cigarette smoke extract (CSE) applied to VSMC in culture, the expression of a key component of prolyl-4-hydroxylase is suppressed and thereby reduces collagen production.(34) This could promote AAA development by reducing the ability of the aorta to repair medial structural damage. Others have shown that CSE can induce metalloprotease production and release in vascular cells and inflammatory cells,(35, 36) thereby promoting matrix damage.
In other studies, however, there is evidence of effects of CSE that would be contrary to what is known about AAA pathology. In VSMC, CSE appears to promote proliferation and survival.(37) This would be consistent with the enhancement of intimal hyperplasia caused by smoking, but the VSMC in AAA are typically sparse and senescent, and reproduce poorly in vitro.(38) Further, the immunomodulatory effects of TS and CSE in the acute situation varies, but it is well-described that chronic exposure effectively induces T-cell anergy,(39, 40) which appears contradictory to the chronic inflammation prominent in AAA.
The cellular effects of nicotine have been well studied, and include effects which may both promote and inhibit AAA development, as has been reviewed elsewhere.(41) Two recent studies using the Apolipoprotein E (ApoE) deficient mouse model of AAA have shown that nicotine can significantly increase aneurysm formation either with,(42) or without angiotensin II infusion.(43) A similar AAA augmentation has also been shown with nicotine infusion in the elastase-perfusion model.(42)
Activation of the AMP-activated protein kinase α2 (AMPK-α2) in VSMC may be responsible for the nicotine enhanced AAA formation,(43) consistent with increased AMPK-α2 in both smokers and in patients with AAA. In a second study, microRNA-21 (miR-21) was found to be enhanced late in aneurysm development in both ApoE-deficient and elastase-perfusion models, and was associated with stabilization of further dilatation.(42) While nicotine exposure increased miR-21 in the aneurysms and cell culture, AAA in the model was abrogated with administration of exogenous pre-miR-21. The authors did not resolve the apparent contradiction with respect to the effects of nicotine on AAA formation and miR-21.
The relationship between these two distinct mechanisms of AAA development related to nicotine exposure remain to be elucidated, although there is some data to suggest that they may be regulated similarly in response to cellular stress. Both miR-21 and AMPK are recognized to be increased in response to hypoxia. (44) There is evidence that miR-21 and AMPK can both be elevated in the context of a stress on glioma cells. (45) Further studies of the downstream effects of miR-21 and AMPK, particularly in the context of whole animal smoke exposure, will probably be necessary to better clarify the role of these molecules in nicotine-enhanced AAA.
Models incorporating in vivo smoke exposure
Although smoke component studies do offer important clues to the effects of TS on AAA development, they are often severely limited by three assumptions: First, that the toxin or limited toxin mixture applied to the cells in culture (or selected for in vivo exposure) would elicit the same effect as the in vivo response when an individual inhales cigarette smoke. Second, that the components evaluated will elicit the same response when used in a more complex mixture. Third, that TS or TS component exposure may activate known pathways of disease. None of these assumptions has been rigorously investigated or validated.
Models which examine the in vivo effects of smoking on AAA development have a critical role to play with regard to exploring the biologic response of the aorta to inhaled smoke, and in validating the mechanistic pathways defined by smoke component evaluations. Unfortunately, while exposure to smoke in the mouse has been used for years to model pulmonary disease, no aneurysm phenotype emerged. Several investigators have demonstrated smoke-enhanced AAA formation with the elastase-perfusion model or the angiotensin II treated ApoE knockout model.(46–48)
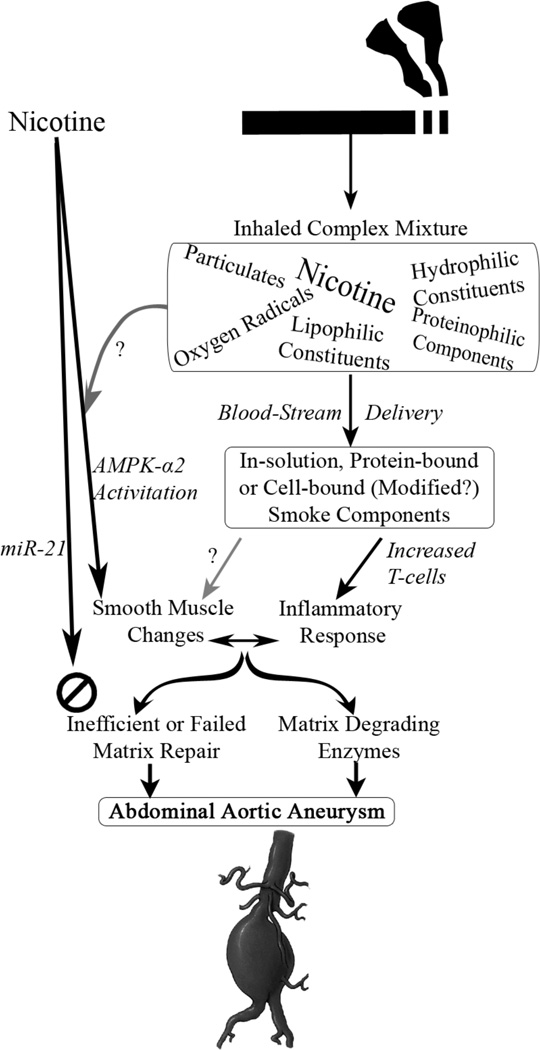
In the elastase-perfusion model, like the human disease where the increased risk of aneurysm formation persists decades after cessation of smoke exposure(14), the effects of relatively short exposure to smoke (6 weeks) results in persistently increased AAA development at least 8 weeks after smoke cessation. Somewhat surprisingly, the effects of smoke on aneurysm development are not inhibited with protease inhibitors or through genetic knockout of elastolytic enzymes.(49) The ultrastructure of the aorta is not altered by smoke exposure alone, but smoke-exposure increases the T-cell infiltrate in the aorta in response to elastase injury. Even more remarkable was the finding that adoptive transfer of leukocytes from smoke exposed animals to smoke-free animals confers the enhanced aneurysm phenotype on the recipient.(49) These results suggest that durable alterations in leukocyte function, particularly the effects on T-cells, may contribute to the enhancement of aneurysm formation by smoking. (Figure 2)
Figure 2.
Both nicotine infusion and experimental smoke exposure can lead to enhanced aneurysm development in murine models. Nicotine seems to directly enhance abdominal
Consolidating current experimental results of smoking on AAA
The impact of the inhalation of a complex cocktail of potential toxins in cigarette smoke on the vasculature presents a significant challenge to scientific interrogation. It must be recognized that the in vivo inhalation of TS results in episodic exposure of combustion products with a variety of bioactivities (e.g. oxygen radicals) and affinities with the circulation (e.g. lipophilic vs. hydrophilic) in the process of delivery to the tissue of interest – the aorta. Cells and enzymes in circulation may also interact with the absorbed smoke in ways that are not well understood.
Prominent components of tobacco smoke, such as nicotine are relatively easy to study in isolation with some elegant results in cell culture and animals models that can confirm our bias regarding the role of smoking on arterial disease. These studies of individual smoke components must be interpreted with caution, however. The apparent contradictory results of smoke component experiments seen in some of these studies may well be due to unique responses to the simplified exposure chosen. (Figure 2) The novel aneurysm models based on inhaled cigarette smoke exposure provide a critical means of validating the potential mechanisms related to smoke components.
Conclusion
There is little doubt that smoking is an important cause of AAA development and progression. It is, however, not the only cause of AAA with 10–15% of cases seen in individuals who have never smoked. (4) This highlights the fact that our understanding of the pathogenesis of AAA is still incomplete. The resistance of smoke-enhanced AAA models to inhibition of elastolytic proteases is an important new clue. An understanding of the unique mechanisms related to smoking is needed to shed light on new strategies to prevent or retard the growth of AAA. Although there is no direct evidence that smoking cessation prevents AAA or decreases the need for AAA intervention, health-economic modeling suggests it would be a cost effective strategy and it remains a priority for all patients with AAA.(50)
Acknowledgements
Sources of Funding
Supported by the National Health and Medical Research Council of Australia grants 458505 & 1006266 (PEN), the National Heart, Lung, and Blood Institute K08 HL84004 (JAC), Flight Attendants Medical Research Institute (JAC), the American Heart Association 0765432Z (JAC), the American College of Surgeons/Society for Vascular Surgery Foundation (JAC) the Department of Veterans Affairs (JAC), and the Peripheral Vascular Surgery Society (JAC).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
None declared
References
- 1.Norman PE, Powell JT. Site specificity of aneurysmal disease. Circulation. 2010;121:560–568. doi: 10.1161/CIRCULATIONAHA.109.880724. [DOI] [PubMed] [Google Scholar]
- 2.Lederle FA, Johnson GR, Wilson SE, Chute EP, Hye RJ, Makaroun MS, Barone GW, Bradyk D. The aneurysm detection and management study screening program. Validation cohort and final results. Arch Int Med. 2000;160:1425–1430. doi: 10.1001/archinte.160.10.1425. [DOI] [PubMed] [Google Scholar]
- 3.Jamrozik K, Norman PE, Spencer CA, Parsons RW, Tuohy R, Lawrence- Brown MM, Dickinson JA. Screening for abdominal aortic aneurysms: lessons from a population-based study. Med J Aust. 2000;173:345–350. doi: 10.5694/j.1326-5377.2000.tb125684.x. [DOI] [PubMed] [Google Scholar]
- 4.Svensjo S, Bjorck M, Gurtelschmid M, Gidlund KD, Hellberg A, Wanhainen A. Low prevalence of abdominal aortic aneurysm among 65-year-old Swedish men indicates a change in the epidemiology of the disease. Circulation. 2011;124:1118–1123. doi: 10.1161/CIRCULATIONAHA.111.030379. [DOI] [PubMed] [Google Scholar]
- 5.Kent KC, Zwolak RM, Egorova NN, Riles TS, Manganaro A, Moskowitz AJ, Gelijns AC, Greco G. Analysis of risk factors for abdominal aortic aneurysm in a cohort of more than 3 million individuals. J Vasc Surg. 2010;52:539–548. doi: 10.1016/j.jvs.2010.05.090. [DOI] [PubMed] [Google Scholar]
- 6.Wilmink TBM, Quick CRG. The association between cigarette smoking and abdominal aortic aneurysm. J Vasc Surg. 1999;30:1099–1105. doi: 10.1016/s0741-5214(99)70049-2. [DOI] [PubMed] [Google Scholar]
- 7.Lederle FA, Nelson DB, Joseph AM. Smokers' relative risk for aortic aneurysm compared with other smoking-related diseases: a systematic review. J Vasc Surg. 2003;38:329–334. doi: 10.1016/s0741-5214(03)00136-8. [DOI] [PubMed] [Google Scholar]
- 8.US Preventive Services Task Force. Screening for Abdominal Aortic Aneurysm: Recommendation statement. Ann Int Med. 2005;142:198–202. doi: 10.7326/0003-4819-142-3-200502010-00011. [DOI] [PubMed] [Google Scholar]
- 9.Vardulaki KA, Walker NM, Day NE, Duffy SW, Ashton HA, Scott RAP. Quantifying the risks of hypertension, age, sex, and smoking in patients with abdominal aortic aneurysm. Br J Surg. 2000;87:195–200. doi: 10.1046/j.1365-2168.2000.01353.x. [DOI] [PubMed] [Google Scholar]
- 10.Spencer CA, Jamrozik K, Norman PE, Lawrence-Brown MMD. The potential for a selective screening strategy for abdominal aortic aneurysm. J Med Screen. 2000;7:209–211. doi: 10.1136/jms.7.4.209. [DOI] [PubMed] [Google Scholar]
- 11.Norman PE, Powell JT. Abdominal aortic aneurysm: the prognosis is worse in women than men. Circulation. 2007;115:2865–2869. doi: 10.1161/CIRCULATIONAHA.106.671859. [DOI] [PubMed] [Google Scholar]
- 12.Pleumeekers HJCM, Hoes AW, van der Does E, van Urk H, Hofman A, de Jong PTVM, Grobbee D E. Aneurysms of the abdominal aorta in older adults. Am J Epidemiol. 1995;142:1291–1299. doi: 10.1093/oxfordjournals.aje.a117596. [DOI] [PubMed] [Google Scholar]
- 13.Lederle FA, Johnson GR ADAM Investigators. Abdominal aortic aneurysm in women. J Vasc Surg. 2001;34:122–126. doi: 10.1067/mva.2001.115275. [DOI] [PubMed] [Google Scholar]
- 14.Forsdahl SH, Singh K, Solberg S, Jacobsen BK. Risk factors for abdominal aortic aneurysms. A 7-year prospective study: the Tromso Study, 1994–2001. Circulation. 2009;119:2201–2208. doi: 10.1161/CIRCULATIONAHA.108.817619. [DOI] [PubMed] [Google Scholar]
- 15.Sweeting MJ, Thompson SG, Brown LC, Powell JT RESCAN collaborators. Meta-analysis of individual patient data to examine factors affecting growth and rupture of small abdominal aortic aneurysms. Br J Surg. 2012;99:655–665. doi: 10.1002/bjs.8707. [DOI] [PubMed] [Google Scholar]
- 16.The United Kingdom Small Aneurysm Trial Participants. Risk factors for aneurysm rupture in patients kept under ultrasound surveillance. Ann Surg. 1999;230:289–296. doi: 10.1097/00000658-199909000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The United Kingdom Small Aneurysm Trial Participants. Long-term outcomes of immediate repair compared with surveillance of small abdominal aortic aneurysms. N Eng J Med. 2002;346:1445–1452. doi: 10.1056/NEJMoa013527. [DOI] [PubMed] [Google Scholar]
- 18.Koole D, Moll FL, Buth J, Hobo R, Zandvoort H, Pasterkamp G, van Herwaarden JA EUROSTAR collaborators. The influence of smoking on endovascular abdominal aortic aneurysm repair. J Vasc Surg. 2012;55:1581–1586. doi: 10.1016/j.jvs.2011.12.018. [DOI] [PubMed] [Google Scholar]
- 19.Norman PE, Spilsbury K, Semmens JB. Falling rates of hospitalisation and mortality from abdominal aortic aneurysms in Australia. J Vasc Surg. 2011;53:274–277. doi: 10.1016/j.jvs.2010.08.087. [DOI] [PubMed] [Google Scholar]
- 20.Anjum A, von Allmen R, Greenhalgh R, Powell JT. Explaining the decrease in mortality from abdominal aortic aneurysm rupture. Br J Surg. 2012;99:637–645. doi: 10.1002/bjs.8698. [DOI] [PubMed] [Google Scholar]
- 21.Snider GL. Distinguishing among asthma, chronic bronchitis, and emphysema. Chest. 1985;87:35S–39S. doi: 10.1378/chest.87.1.35s. [DOI] [PubMed] [Google Scholar]
- 22.Lindholt J, Jorgensen B, Shi G-P, Henneberg EW. Relationships between activators and inhibitors of plasminogen, and the progression of small abdominal aortic aneurysms. Eur J Vasc Endovas Surg. 2003;25:546–551. doi: 10.1053/ejvs.2002.1872. [DOI] [PubMed] [Google Scholar]
- 23.Barua RS, Ambrose JA, Saha DC, Eales-Reynolds L-J. Smoking is associated with altered endothelial-derived fibrinolytic and antithrombotic factors. Circulation. 2002;106:905–908. doi: 10.1161/01.cir.0000029091.61707.6b. [DOI] [PubMed] [Google Scholar]
- 24.Elmore JR, Obmann MA, Kuivaniemi H, Tromp G, Gerhard GS, Franklin DP, Boddy AM, Carey DJ. Identification of a genetic variant associated with abdominal aortic aneurysms on chromosome 3p12.3 by genome wide association. J Vasc Surg. 2009;49:1525–1531. doi: 10.1016/j.jvs.2009.01.041. [DOI] [PubMed] [Google Scholar]
- 25.Gretarsdottir S, Baas AF, Thorleifsson G et al. Genome-wide association study identifies a sequence variant within the DAB2IP gene conferring susceptibility to abdominal aortic aneurysm. Nat Genet. 2010;42:692–697. doi: 10.1038/ng.622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krishna SM, Dear AE, Norman PE, Golledge J. Genetic and epigenetic mechanisms and their possible role in abdominal aortic aneurysm. Atherosclerosis. 2010;212:16–29. doi: 10.1016/j.atherosclerosis.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 27.Shapiro SD. The pathogenesis of emphysema: the elastase:antielastase hypothesis 30 years later. Proc Assoc Am Physicians. 1995;107:346–352. [PubMed] [Google Scholar]
- 28.Shapiro SD. Evolving concepts in the pathogenesis of chronic obstructive pulmonary disease. Clin Chest Med. 2000;21:621–632. doi: 10.1016/s0272-5231(05)70172-6. [DOI] [PubMed] [Google Scholar]
- 29.Shapiro SD. Proteinases in chronic obstructive pulmonary disease. Biochem Soc Trans. 2002;30:98–102. doi: 10.1042/. [DOI] [PubMed] [Google Scholar]
- 30.Finlay GA, O'Driscoll LR, Russell KJ, D'Arcy EM, Masterson JB, FitzGerald MX, O'Connor CM. Matrix metalloproteinase expression and production by alveolar macrophages in emphysema. Am J Resp Crit Care Med. 1997;156:240–247. doi: 10.1164/ajrccm.156.1.9612018. [DOI] [PubMed] [Google Scholar]
- 31.Finlay GA, Russell KJ, McMahon KJ, D'Arcy EM, Masterson JB, FitzGerald MX, O'Connor CM. Elevated levels of matrix metalloproteinases in bronchoalveolar lavage fluid of emphysematous patients. Thorax. 1997;52:502–506. doi: 10.1136/thx.52.6.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Segura-Valdez L, Pardo A, Gaxiola M, Uhal BD, Becerril C, Selman M. Upregulation of gelatinases A and B, collagenases 1 and 2, and increased parenchymal cell death in COPD. Chest. 2000;117:684–694. doi: 10.1378/chest.117.3.684. [DOI] [PubMed] [Google Scholar]
- 33.Betsuyaku T, Nishimura M, Takeyabu K, Tanino M, Venge P, Xu S, Kawakami Y. Neutrophil granule proteins in bronchoalveolar lavage fluid from subjects with subclinical emphysema. Am J Resp Crit Care Med. 1999;159:1985–1991. doi: 10.1164/ajrccm.159.6.9809043. [DOI] [PubMed] [Google Scholar]
- 34.Raveendran M, Senthil D, Utama B, Shen Y, Dudley D, Wang J, Zhang Y, Wang XL. Cigarette suppresses the expression of P4H[alpha] and vascular collagen production. Biochem Biophys Res Com. 2004;323:592–598. doi: 10.1016/j.bbrc.2004.08.129. [DOI] [PubMed] [Google Scholar]
- 35.Murphy EA, Danna-Lopes D, Sarfati I, Rao S, Cohen JR. Nicotine-stimulated elastase activity release by neutrophils in patients with abdominal aortic aneurysms. Ann Vasc Surg. 1998;12:41–45. doi: 10.1007/s100169900113. [DOI] [PubMed] [Google Scholar]
- 36.Lemaître V, Dabo AJ, D'Armiento J. Cigarette smoke components induce matrix metalloproteinase-1 in aortic endothelial cells through inhibition of mTOR signaling. Toxicological Sciences. 2011;123:542–549. doi: 10.1093/toxsci/kfr181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen Q, Edvinsson L, Xu C-B. Cigarette smoke extract promotes human vascular smooth muscle cell proliferation and survival through ERK1/2- and NF-κBdependent pathways. Scientific World J. 2010;10:2139–2156. doi: 10.1100/tsw.2010.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liao S, Curci JA, Kelley BJ, Sicard GA, Thompson RW. Accelerated replicative senescence of medial smooth muscle cells derived from abdominal aortic aneurysms compared to the adjacent inferior mesenteric artery. J Surg Res. 2000;92:85–95. doi: 10.1006/jsre.2000.5878. [DOI] [PubMed] [Google Scholar]
- 39.Kalra R, Singh SP, Savage SM, Finch GL, Sopori ML. Effects of cigarette smoke on immune response: chronic exposure to cigarette smoke impairs antigenmediated signaling in T cells and depletes IP3-sensitive Ca(2+) stores. J Pharmacol Exp Ther. 2000;293:166–171. [PubMed] [Google Scholar]
- 40.Geng Y, Savage SM, Razani-Boroujerdi S, Sopori ML. Effects of nicotine on the immune response. II. Chronic nicotine treatment induces T cell anergy. J Immunol. 1996;156:2384–2390. [PubMed] [Google Scholar]
- 41.Li Z-Z, Dai Q-Y. Pathogenesis of abdominal aortic aneurysms: role of nicotine and nicotinic acetylcholine receptors. Mediators Inflamm. 2012:103120. doi: 10.1155/2012/103120. Epub 2012 Mar 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maegdefessel L, Azuma J, Toh R, Deng A, Merk DR, Raiesdana A, Leeper NJ, Raaz U, Schoelmerich AM, McConnell MV, Dalman RL, Spin JM, Tsao PS. MicroRNA-21 blocks abdominal aortic aneurysm development and nicotineaugmented expansion. Science Translational Medicine. 2012;4 doi: 10.1126/scitranslmed.3003441. 122ra22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang S, Zhang C, Zhang M, Liang B, Zhu H, Lee J, Viollet B, Xia L, Zhang Y, Zou M-H. Activation of AMP-activated protein kinase [alpha]2 by nicotine instigates formation of abdominal aortic aneurysms in mice in vivo. Nat Med. 2012;18:902–910. doi: 10.1038/nm.2711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Polytarchou C, Iliopoulos D, Hatziapostolou M, Kottakis F, Maroulakou I, Struhl K, Tsichlis PN. Akt2 regulates all Akt isoforms and promotes resistance to hypoxia through induction of miR-21 upon oxygen deprivation. Cancer Research. 2011;71:4720–4731. doi: 10.1158/0008-5472.CAN-11-0365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Godlewski J, Nowicki MO, Bronisz A, Nuovo G, Palatini J, de Lay M, van Brocklyn J, Ostrowski MC, Chiocca EA, Lawler SE. MicroRNA-451 regulates LKB1/AMPK signaling and allows adaptation to metabolic stress in glioma cells. Molecular Cell. 2010;37:620–632. doi: 10.1016/j.molcel.2010.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stolle K, Berges A, Lietz M, Lebrun S, Wallerath T. Cigarette smoke enhances abdominal aortic aneurysm formation in angiotensin II-treated apolipoprotein E-deficient mice. Toxicology Letters. 2010;199:403–409. doi: 10.1016/j.toxlet.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 47.Buckley C, Wyble CW, Borhani M, Ennis TL, Kobayashi DK, Curci JA, Shapiro SD, Thompson RW. Accelerated enlargement of experimental abdominal aortic aneurysms in a mouse model of chronic cigarette smoke exposure. J Am Coll Surg. 2004;199:896–903. doi: 10.1016/j.jamcollsurg.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 48.Bergoeing MP, Arif B, Hackmann AE, Ennis TL, Thompson RW, Curci JA. Cigarette smoking increases aortic dilatation without affecting matrix metalloproteinase-9 and-12 expression in a modified mouse model of aneurysm formation. J Vasc Surg. 2007;21:328–338. doi: 10.1016/j.jvs.2007.01.058. [DOI] [PubMed] [Google Scholar]
- 49.Arif B, Garcia-Fernandez F, Ennis TL, Jin J, Davis EC, Thompson RW, Curci JA. Novel mechanism of aortic aneurysm development in mice associated with smoking and leukocytes. Arterioscler Thromb Vasc Biol. 2012;32:2901–2909. doi: 10.1161/ATVBAHA.112.300208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mani K, Wanhainen A, Lundkvist J, Lindstrom D. Cost-effectiveness of intensive smoking cessation therapy among patients with small abdominal aortic aneurysms. J Vasc Surg. 2011;54:628–636. doi: 10.1016/j.jvs.2011.02.055. [DOI] [PubMed] [Google Scholar]