Abstract
Plaque rupture with thrombotic occlusion without severe underlying coronary atherosclerosis is frequently observed during primary percutaneous coronary intervention (pPCI) for ST-segment elevation myocardial infarction (STEMI). These lesions are stented even if post thrombectomy mild underlying coronary artery disease (CAD) is noted. The value of mechanical thrombus aspiration alone “lone aspiration thrombectomy” (LAT) without stenting is not well studied. We present a retrospective analysis of patients receiving LAT as the only pPCI therapy for STEMI. Between January 2008 and March 2012, 202 young patients underwent pPCI for acute STEMI at our institution. From this group 10 patients had LAT as definitive therapy. LAT was favored if post thrombectomy minimal underlying CAD was noted, and concerns regarding long term treatment cost and compliance with dual antiplatelet therapy (DAPT) was an issue. All patients received ASA, clopidogrel, heparin and eptifibatide. DAPT was maintained for at least 1 month. One patient was lost to follow-up. At one month, all remaining 9 patients were free of MACE. At six weeks one patient had recurrent STEMI after abruptly discontinuing all his medications. Re-occlusion at the site of prior plaque rupture was stented, and treatment compliance was urged. Short term follow up at 2 months available for 5 patients and 2 years for 3 patients revealed no adverse consequences, the remaining patients had returned to their home countries. Conclusion: In selected young patients presenting with acute STEMI, LAT without balloon angioplasty or stenting is feasible and is associated with favorable short and long-term outcome.
Keywords: Aspiration thrombectomy, percutaneous coronary intervention, angioplasty, ST-segment elevation myocardial infarction, young patients, coronary artery disease
Introduction
Myocardial infarction in patients less than 50 years is uncommon. It usually presents as single vessel disease with thrombotic occlusion at the site of endothelial erosion or plaque rupture [1-4]. PCI is an effective and preferred method for restoring epicardial blood flow in acute MI [5,6]. Distal embolization of atherothrombotic material in the infarct related artery (IRA) before and during PCI is associated with more extensive myocardial infarction, possibility of a no reflow phenomenon and higher mortality [7]. To avert these complications manual thrombus aspiration before stenting of IRA is advised [8,9]. Following thrombosuction, however, stenting of underlying diseased coronary segment is undertaken irrespective of residual atherosclerotic disease. Randomized trials of acute MI have not addressed the question of manual thrombus aspiration without stenting. This approach is infrequently reported in literature [10-16]. and no specific guidelines are available. In recent publications [17,18]. Thrombus aspiration alone may be a viable option in patients presenting with STEMI or rescue angioplasty.
Tawam Hospital is a regional tertiary care hospital situated in Al Ain, UAE. It serves a heterogeneous population with substantial number of expatriates originating from South East Asia and the Far East. In this latter group, presentation with MI is at a significantly younger age. Predisposition for this early presentation of symptomatic CAD is not well understood. Management of these patients is affected by cost considerations, compliance issues and fragmented follow up care. Considering these socioeconomic factors, which significantly impact treatment compliance and outcome, we have managed these patients selectively with thrombus aspiration alone without stenting of IRA, if post thrombectomy minimal or no residual atherosclerotic disease was present on angiography.
In this retrospective analysis of our experience with mechanical thrombus aspiration alone in 10 patients with a mean age of 36.3 years we discuss major adverse cardiovascular events (MACE) during short term and long term follow up and the problem with treatment compliance and fragmented care.
Materials and methods
Identification of studied patients
Between January 2008 and March 2012, 202 patients younger than 50 years of age underwent primary PCI for acute STEMI at our institution. In this group 10 patients (5%) were treated with mechanical thrombus aspiration alone.
Criteria for lone thrombosuction
Lone thrombosuction was performed if residual lesion was felt by the operator to be at low risk of re-occlusion. Lesions that were deemed favorable for aspiration only were in non-tortuous and non-calcified vessels with no residual lesion or mild residual stenosis (< 40%) with smooth angiographic appearance of the vessel lumen and restoration of TIMI-3 flow. Non-infracted vessels being angiographically normal were additional reassuring information for a low total atherosclerotic burden. The decision to avoid stenting was based on preference of treating cardiologist. High-risk patients or lesions assessed to be complex, calcified or in a tortuous vessel, or more than mild stenosis post thrombus extraction were determined to be unsuitable for lone thrombosuction.
Procedure
Access was obtained through right radial artery. Diagnostic angiography was performed with 5 French (Fr) radial TIG catheter (Terumo Medical, Somerset, NJ). JR and XB guide-catheters (Cordis Corporation Miami Lakes FL) were used for PCI. BMW guidewire (Abbott Vascular Santa Clara CA) was successfully used in all instances. Export catheters (6F) (Medtronic vascular Incorporation, Santa Rosa, CA) were used for thrombus aspiration. Intra coronary Adenosine, Nicardipine, or Nitroprusside was used in six cases to manage “slow or no reflow” due to large thrombus burden.
Adjuvant treatment
All patients received loading dose of aspirin 300 mg, clopidogrel 600 mg, heparin 5000 units bolus followed by heparin infusion and eptifibatide prior to coronary intervention.
Heparin infusion was maintained for 48 hrs targeting PTT between 50-70. Eptifibatide was infused for 18-24 hours. High dose aspirin at 300 mg daily and clopidogrel 75 mg daily was maintained for the first 4 weeks with reduction in aspirin dose to 100 mg thereafter. Other treatment included beta-blockers, high dose statin and ACE-I.
To ensure early compliance patient received first month of treatment free of any additional cost upon hospital discharge.
Follow up
Follow up information was gathered during office visit, telephone contact and review of electronic medical record. Any adverse cardiovascular event or compliance issue was appropriately documented.
Statistical analysis
All analysis was performed on Epi info version 3.5.3 software package.
Results
Baseline characteristics
Clinical characteristics are summarized in Table 1 These patients had no prior history of CAD. The mean age for the group was 36.3 years. Nine patients were male. Cigarette smoking was documented in six patients, hyperlipidemia in four, diabetes in two and hypertension in one. Hypercoaguable state due to polycythemia was diagnosed in one. Strong family history of premature coronary artery disease was present in one as shown in Table 1.
Table 1.
Baseline Characteristics of Patients
| Patients (n=10) | |
|---|---|
| Male (female) | 9 (1) |
| Age (mean ± SD) | 36.3 |
| Smoking History | 6 |
| Diabetes Mellitus | 2 |
| Family History | 1 |
| Hypercholesterolemia | 4 |
| Hypertension | 1 |
| Previous CAD | 0 |
| Polycythemia | 1 |
Routine diagnostic studies
Routine diagnostic studies revealed a moderate sized myocardial infarction. Overall LV systolic function was mildly reduced. Significant dyslipidemia was present at admission as shown in Table 2.
Table 2.
Cardiac Biomarkers, Lipids and LV Function
| Diagnostic Test | Mean Value (+/-SD) |
|---|---|
| Peak CPK | 2586.6 |
| Peak troponin (mean ± SD) | 65.1 |
| Total cholesterol mg/dl (mean ± SD) | 211.5 (+/-58.77) |
| LDL-C mg/dl (mean ± SD) | 142.3 (+/-51.04) |
| HDL-C mg/dl (mean ± SD) | 36.3 (+/-11.05) |
| Triglyceride mg/dl (mean ± SD) | 218.8 (+/-134.66) |
| LVEF (%) at discharge (mean ± SD) | 55 (+/-5.9) |
Coronary angiography
In Table 3 each patient is represented detailing age, ethnicity and BMI. Corresponding angiographic characteristic of the IRA for each patient, success following Lone thrombus aspiration and use of adjuvant intracoronary medications is detailed. Seven patients originated from South East Asia, one from Far East and two were of Middle Eastern origin. The mean BMI for the group was 25. Left anterior descending (LAD) artery was the culprit artery in five, right coronary artery (RCA) in three and left circumflex (LCX) in two patients respectively. Prior to any mechanical intervention TIMI 0 flow was noted in six patients while the rest had TIMI 2 flow in culprit vessel. Post thrombosuction TIMI 3 flow was restored in all patients. Six patients received intracoronary adenosine, Nicardipine or Nitroprusside for “slow flow phenomena”. Post thrombus aspiration all patient had either no visible lesion or less than 40% residual stenosis. The non culprit vessels were angiographically normal in nine out of ten patients with one patient having non obstructive disease in first diagonal (D1) and RCA.
Table 3.
Age, Ethnicity, BMI and Vessel Characteristics Pre and Post PCI
| Patient No | Age (years) | Asian Race | BMI (mean 24.98) | IRA | Stenosis before/after Lone Thrombus Aspiration | other vessels | TIMI flow before PCI | TIMI flow after PCI | Intracoronary adenosine NicardipineNitroprusside |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 35 | South East | 24.3 | LAD | 80/20% | Normal | 2 | 3 | 0 |
| 2 | 30 | South East | 25.3 | LAD | 70/40% | Normal | 2 | 3 | 1 |
| 3 | 39 | South East | 21.4 | OM | 100/40% | Normal | 0 | 3 | 1 |
| 4 | 41 | South East | 19.8 | LCX | 100/40% | D1/RCA | 0 | 3 | 1 |
| 5 | 38 | South East | 27.1 | LAD | 90/30% | Normal | 2 | 3 | 1 |
| 6 | 41 | South East | 28.9 | RCA | 100/mild | Normal | 0 | 3 | 1 |
| 7 | 30 | South East | 21.4 | LAD | 100/30% | Normal | 0 | 3 | 1 |
| 8 | 29 | Middle East | 24.8 | RCA | 100/40% | Normal | 0 | 3 | 0 |
| 9 | 48 | Far East | 23.9 | LAD | 100/10% | Normal | 0 | 3 | 0 |
| 10 | 32 | Middle East | 32.9 | RCA | 90/0% | Normal | 2 | 3 | 0 |
Clinical outcome
One patient did not return for specified follow up at 4 weeks. No MACE was noted in the other 9 patients at 4 weeks. Patient #8 (29 years old smoker), underwent pre discharge coronary CT angiogram, which showed moderate (50-69%) residual stenosis. He stopped all medications five weeks post discharge and presented a week thereafter with STEMI. Re-occlusion of RCA at the same site of previous plaque rupture was confirmed on angiogram. The culprit lesion was stented and he was re-counseled regarding treatment compliance. Repeat invasive angiography for chest pain in patient #9, 6 weeks after initial hospitalization confirmed vessel patency with minimal residual lesion and TIMI 3 flow as shown in Figure 1. Subsequent follow up was available in 5 patients (three patients returned to their home countries) at two months and in 3 patients at 1 year and 2 years after their index MI as presented in Figure 2.
Figure 1.
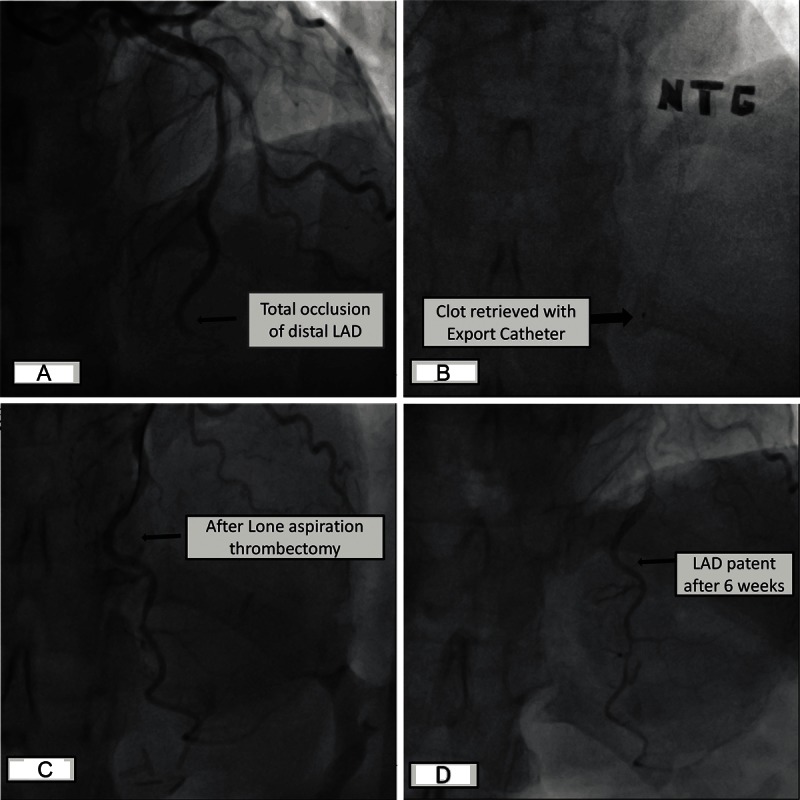
A: Total occlusion of LAD; B: Clot retrieved by export catheter; C: Post LAT angiogram shows less than 40% stenosis; D: Angiogram 6 weeks later confirms vessel patency.
Figure 2.
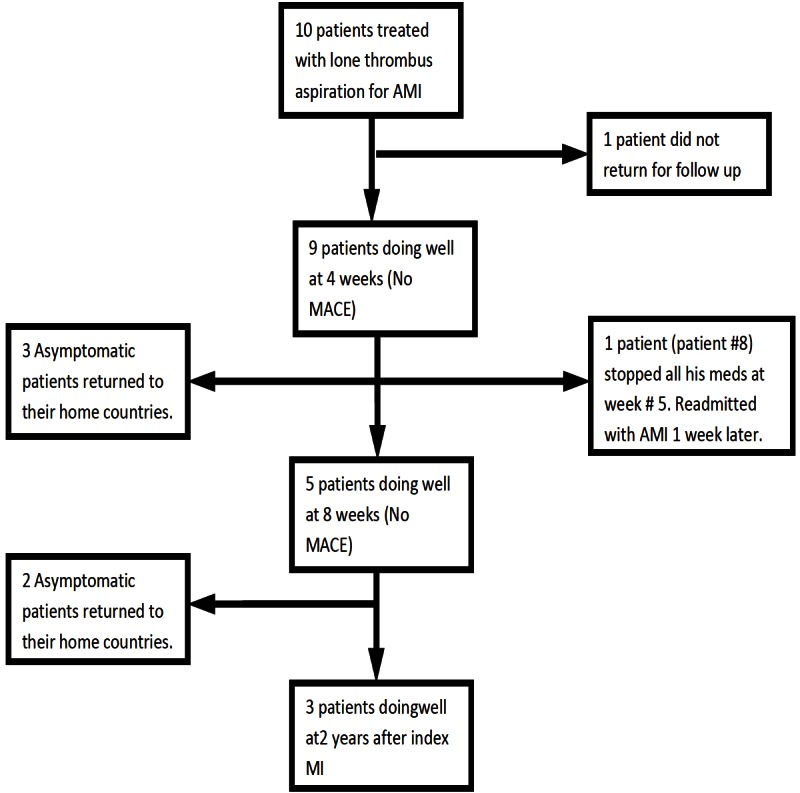
Clinical follow up and outcome.
Discussion
In acute STEMI intra-luminal thrombus is seen in 90% patients [19]. Distal embolization in STEMI occurs in approximately 15% cases and is associated with no reflow [20,21] reduced angiographic success, reduced ST segment resolution, larger infarct size and higher mortality [3]. Thrombus aspiration is an effective adjunctive therapy to prevent distal embolization and is recommended in patients with STEMI undergoing mechanical revascularization [22,23]. Despite the clinical [24], and angiographic [25,26] benefit, the response to thrombus aspiration is variable [27].
Majority of acute myocardial infarctions occur in the setting of thrombotic occlusion of coronary artery subsequent to plaque rupture and less frequently from thrombus associated with plaque erosion. The underlying atherosclerotic plaque is mostly not obstructive [28,29]. Intracoronary thrombus can be treated with embolic protection devices, mechanical thrombectomy [9]. or manual aspiration. Results were not conclusive regarding their usefulness in earlier trials and meta-analysis [24,26,30,31]. The TAPAS trial [9] brought manual thrombectomy into the mainstream, and showed mortality reduction at one-year follow-up. Thrombus aspiration in this and other studies was an effective adjunctive therapy to prevent distal embolization [22,23].
The above emphasizes the concept that intracoronary thrombus, not plaque burden is the cause of vessel obstruction, and lone thrombectomy may be enough in selected cases.
In our series we show the short-term safety and feasibility of lone thrombectomy without stenting of the infarct related artery when TIMI 3 flow has been established and a non-significant residual lesion is present. Appropriate selection of patients for this approach is important, as we have previously outlined. Early compliance with prescribed treatment, in particular dual antiplatelet therapy is likely important. This approach is cost effective, avoids problems inherent with coronary stenting and the need for long-term dual antiplatelet therapy.
Study limitations
This study has the inherent limitation of a retrospective chart review. The small number of patients and inconsistent follow up influences our observations. Treatment decisions were based on angiographic appearance post thrombectomy. Additional information from Intra-vascular ultrasound (IVUS) may have confirmed our visual estimate of mild residual atherosclerosis. During follow up assessment objective reevaluation of plaque progression was not done. Functional testing or coronary CTA may have been insightful.
Conclusion
The presented cases demonstrate the effectiveness of manual thrombus aspiration in restoring TIMI 3 flow. It also confirms the safety and feasibility of thrombus aspiration alone in selected young patients with acute ST elevation myocardial infarction. Additional evaluation of plaque progression with functional testing or coronary CTA may be useful.
Disclosure of conflict of interest
None.
References
- 1.Davies MJ, Thomas A. Thrombosis and acute coronary lesions in sudden cardiac ischemic death. N Engl J Med. 1984;310:1137–1140. doi: 10.1056/NEJM198405033101801. [DOI] [PubMed] [Google Scholar]
- 2.Falk E, Shah PK, Fuster V. Coronary Plaque disruption. Circulation. 1995;92:657–671. doi: 10.1161/01.cir.92.3.657. [DOI] [PubMed] [Google Scholar]
- 3.Farb A, Burke AP, Tang AL, Liang TY, Mannan P, Smialek J, Virmani R. Coronary plaque erosion without rupture into a lipid core. A frequent cause of coronary thrombosis in sudden coronary death. Circulation. 1996;93:1354–1363. doi: 10.1161/01.cir.93.7.1354. [DOI] [PubMed] [Google Scholar]
- 4.Van der Wal AC, Becker AE, van der Loos CM, Das PK. Site of initial rupture or erosion of thrombosed coronary atherosclerotic plaques is characterized by an inflammatory process irrespective of the dominant morphology. Circulation. 1994;89:36–44. doi: 10.1161/01.cir.89.1.36. [DOI] [PubMed] [Google Scholar]
- 5.Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC Jr, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the Guidelines for the Management of Patients With Acute Myocardial Infarction) ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction) Circulation. 2004;110:588–636. doi: 10.1161/01.CIR.0000134791.68010.FA. [DOI] [PubMed] [Google Scholar]
- 6.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 7.Henriques JP, Zijlstra F, Ottervanger JP, de Boer MJ, van ‘t Hof AW, Hoorntje JC, Suryapranata H. Incidence and clinical significance of distal embolization during primary angioplasty for acute myocardial infarction. Eur Heart J. 2002;23:1112–1117. doi: 10.1053/euhj.2001.3035. [DOI] [PubMed] [Google Scholar]
- 8.Svilaas T, Vlaar PJ, van der Horst IC, Diercks GF, de Smet BJ, van den Heuvel AF, Anthonio RL, Jessurun GA, Tan ES, Suurmeijer AJ, Zijlstra F. Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med. 2008;358:557–567. doi: 10.1056/NEJMoa0706416. [DOI] [PubMed] [Google Scholar]
- 9.Vlaar PJ, Svilaas T, van der Horst IC, Diercks GF, Fokkema ML, de Smet BJ, van den Heuvel AF, Anthonio RL, Jessurun GA, Tan ES, Suurmeijer AJ, Zijlstra F. Cardiac death and reinfarction after 1 year in the Thrombus Aspiration during Percutaneous coronary intervention in Acute myocardial infarction Study (TAPAS): a 1-year follow-up study. Lancet. 2008;371:1915–1920. doi: 10.1016/S0140-6736(08)60833-8. [DOI] [PubMed] [Google Scholar]
- 10.Talarico GP, Burzotta F, Trani C, Porto I, Leone AM, Niccoli G, Coluccia V, Schiavoni G, Crea F. Thrombus aspiration without additional ballooning or stenting to treat selected patients with ST-elevation myocardial infarction. J Invasive Cardiol. 2010;22:489–492. [PubMed] [Google Scholar]
- 11.Sakai K, Inoue K, Nobuyoshi M. Aspiration thrombectomy of a massive thrombotic embolus in acute myocardial infarction caused by coronary embolism. Int Heart J. 2007;48:387–392. doi: 10.1536/ihj.48.387. [DOI] [PubMed] [Google Scholar]
- 12.Hajek P, Alan D, Vejvoda J, Linhartova K, Shapa P. Hajsmannova Z, Veselka J, Treatment of a large Left main coronary artery thrombus by aspiration thrombectomy. J Thromb Thrombolysis. 2009;27:352–354. doi: 10.1007/s11239-008-0209-y. [DOI] [PubMed] [Google Scholar]
- 13.Kotooka N, Otsuka Y, Yasuda S, Morii I, Kawamura A, Miyazaki S. Three cases of acute myocardial infarction due to coronary embolism. Treatment using a thrombus aspiration device. Jpn Heart J. 2004;45:861–866. doi: 10.1536/jhj.45.861. [DOI] [PubMed] [Google Scholar]
- 14.Wilson AM, Ardehali R, Brinton TJ, Yeung AC, Vagelos R. Successful removal of a paradoxical coronary embolus using an aspiration catheter. Nat Clin Pract Cardiovasc Med. 2006;3:633–636. doi: 10.1038/ncpcardio0681. [DOI] [PubMed] [Google Scholar]
- 15.Fokkema ML, Vlaar PJ, Svilaas T. Thrombus aspiration as definitive mechanical intervention for ST-elevation myocardial infarction: a report of five cases. J Invasive Cardiol. 2008;20:242–244. [PubMed] [Google Scholar]
- 16.Avaramides D, Raisakis K, Matsakas E. Acute inferior ST-segment elevation myocardial infarction treated with primary angioplasty using only a Pronto aspiration catheter. J Invasive Cardiol. 2008;20:E177–9. [PubMed] [Google Scholar]
- 17.Kramer MC, Verouden NC, Li X, Koch KT, van der Wal AC, Tijssen JG, de Winter RJ. Thrombus aspiration alone during primary percutanous coronary intervention as definitive treatment in acute ST-elevation myocardial infarction. Catheter Cardiovasc Interv. 2012;79:860–867. doi: 10.1002/ccd.23214. [DOI] [PubMed] [Google Scholar]
- 18.Jamil G, Ouda H, Jamil M, Qureshi A. ‘Mechanical thrombectomy alone’ as a definite therapy for rescue angioplasty. BMJ Case Rep. 2013:2013. doi: 10.1136/bcr-2013-009002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DeWood MA, Spores J, Notske R, Mouser LT, Burroughs R, Golden MS, Lang HT. Prevalence of total coronary occlusion during the early hours of transmural myocardial infarction. N Engl J Med. 1980;303:897–902. doi: 10.1056/NEJM198010163031601. [DOI] [PubMed] [Google Scholar]
- 20.Sakuma T, Leong-Poi H, Fisher NG, Goodman NC, Kaul S. Further insights into the no-reflow phenomenon after primary angioplasty in acute myocardial infarction: the role of microthromboemboli. J Am Soc Echocardiogr. 2003;16:15–21. doi: 10.1067/mje.2003.44. [DOI] [PubMed] [Google Scholar]
- 21.Niccoli G, Burzotta F, Galiuto L, Crea F. Myocardial no-reflow in humans. J Am Coll Cardiol. 2009;54:281–292. doi: 10.1016/j.jacc.2009.03.054. [DOI] [PubMed] [Google Scholar]
- 22.Kushner FG, Hand M, Smith SC Jr, King SB 3rd, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE Jr, Green LA, Hochman JS, Jacobs AK, Krumholz HM, Morrison DA, Ornato JP, Pearle DL, Peterson ED, Sloan MA, Whitlow PL, Williams DO. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009;54:2205–2241. doi: 10.1016/j.jacc.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 23.Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, Filippatos G, Fox K, Huber K, Kastrati A, Rosengren A, Steg PG, Tubaro M, Verheugt F, Weidinger F, Weis M ESC Committee for Practice Guidelines (CPG) Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008;29:2909–2945. doi: 10.1093/eurheartj/ehn416. [DOI] [PubMed] [Google Scholar]
- 24.Burzotta F, De Vita M, Gu YL, Isshiki T, Lefèvre T, Kaltoft A, Dudek D, Sardella G, Orrego PS, Antoniucci D, De Luca L, Biondi-Zoccai GG, Crea F, Zijlstra F. Clinical impact of thrombectomy in acute ST-elevation myocardial infarction: an individual patient-data pooled analysis of 11 trials. Eur Heart J. 2009;30:2193–2203. doi: 10.1093/eurheartj/ehp348. [DOI] [PubMed] [Google Scholar]
- 25.Burzotta F, Trani C, Romagnoli E, Mazzari MA, Rebuzzi AG, De Vita M, Garramone B, Giannico F, Niccoli G, Biondi-Zoccai GG, Schiavoni G, Mongiardo R, Crea F. Manual thrombus-aspiration improves myocardial reperfusion: the randomized evaluation of the effect of mechanical reduction of distal embolization by thrombus-aspiration in primary and rescue angioplasty (REMEDIA) trial. J Am Coll Cardiol. 2005;46:371–376. doi: 10.1016/j.jacc.2005.04.057. [DOI] [PubMed] [Google Scholar]
- 26.De Luca G, Dudek D, Sardella G, Marino P, Chevalier B, Zijlstra F. Adjunctive manual thrombectomy improves myocardial perfusion and mortality in patients undergoing primary percutaneous coronary intervention for ST-elevation myocardial infarction: a meta-analysis of randomized trials. Eur Heart J. 2008;29:3002–3010. doi: 10.1093/eurheartj/ehn389. [DOI] [PubMed] [Google Scholar]
- 27.Burzotta F, Trani C, Romagnoli E, Belloni F, Biondi-Zoccai GG, Mazzari MA, De Vita M, Giannico F, Garramone B, Niccoli G, Rebuzzi AG, Mongiardo R, Schiavoni G, Crea F. A pilot study with a new, rapid-exchange, thrombus-aspirating device in patients with thrombus-containing lesions: the Diver C. E. study. Catheter Cardiovasc Interv. 2006;67:887–893. doi: 10.1002/ccd.20713. [DOI] [PubMed] [Google Scholar]
- 28.Falk E. Plaque rupture with severe pre-existing stenosis precipitating coronary thrombosis. Characteristics of coronary atherosclerotic plaques underlying fatal occlusive thrombi. Br Heart J. 1983;50:127–134. doi: 10.1136/hrt.50.2.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vetrovec GW, Cowley MJ, Overton H, Richardson DW. Intracoronary thrombus in syndromes of unstable myocardial ischemia. Am Heart J. 1981;102:1202–1208. doi: 10.1016/0002-8703(81)90653-0. [DOI] [PubMed] [Google Scholar]
- 30.Bavery AA, Kumbhani DJ, Bhatt DL. Role of adjunctive thrombectomy and embolic protection devices in acute myocardial infarction: a comprehensive meta-analysis of randomized trials. Eur Heart J. 2008;29:2989–3001. doi: 10.1093/eurheartj/ehn421. [DOI] [PubMed] [Google Scholar]
- 31.Ali A, Cox D, Dib N, Brodie B, Berman D, Gupta N, Browne K, Iwaoka R, Azrin M, Stapleton D, Setum C, Popma J AIMI Investigators. Rheolytic thrombectomy with percutaneous coronary intervention for infarct size reduction in acute myocardial infarction: 30-day results from a multicenter randomized study. J Am Coll Cardiol. 2006;48:244–252. doi: 10.1016/j.jacc.2006.03.044. [DOI] [PubMed] [Google Scholar]


