Abstract
The HSP90 inhibitor XL888 is effective at reversing BRAF inhibitor resistance in melanoma, including that mediated through acquired NRAS mutations. The present study has investigated the mechanism of action of XL888 in NRAS mutant melanoma. Treatment of NRAS mutant melanoma cell lines with XL888 led to an inhibition of growth, G2/M phase cell cycle arrest and the inhibition of cell survival in 3D spheroid and colony formation assays. In vitro, HSP90 inhibition led to the degradation of ARAF, CRAF, Wee1, Chk1 and cdc2 and was associated with decreased MAPK, AKT, mTOR and JNK signaling. Apoptosis induction was associated with increased BIM expression and a decrease in the expression of the pro-survival protein Mcl-1. The critical role of increased BIM and decreased Mcl-1 expression in the survival of NRAS mutant melanoma cell lines was demonstrated through siRNA knockdown and overexpression studies. In an animal xenograft model of NRAS mutant melanoma, XL888 treatment led to reduced tumor growth and apoptosis induction. Important differences in the pattern of client degradation were noted between the in vivo and in vitro studies. In vivo, XL888 treatment led to degradation of CDK4 and Wee1 and the inhibition of AKT/S6 signaling with little or no effect observed upon ARAF, CRAF or MAPK. Blockade of Wee1, using either siRNA knockdown or the inhibitor MK1775, was associated with significant levels of growth inhibition and apoptosis induction. Together these studies have identified Wee1 as a key target of XL888, suggesting novel therapeutic strategies for NRAS mutant melanoma.
Keywords: melanoma, NRAS, Wee1, therapy, HSP90
Introduction
Ras proteins are small molecular weight (21 kDa) GTPases that localize to the plasma membrane and function as molecular switches linking cell surface receptor tyrosine kinase activity to downstream signaling pathways (1). Approximately 25% of all cancers harbor point mutations in Ras, with the most common being position 61 mutations leading to impaired GTPase activity and position 12/13 mutations that prevent GTPase domain deactivation. In its mutant, active state Ras recruits a number of signaling cascades involved in tumor progression including the phospho-inositide 3-kinase (PI3K)/AKT pathway, the mitogen activated protein kinase (MAPK) pathway, RAL-GDS and phospholipase C (PLC)-ε (1, 2).
Recent years have seen major advances in the therapeutic management of disseminated melanomas driven through activating mutations in the serine/threonine kinase BRAF (3, 4). Despite these successes, little progress has been made towards the development of targeted therapy strategies for the 50% of all melanomas that are BRAF wild-type (5). By far the most well-characterized group of BRAF wild-type melanomas are the 15–20% of all melanomas that harbor activating position 61 mutations in NRAS (6). Emerging data shows NRAS mutant melanomas to be biologically distinct from BRAF mutant melanomas with the typical NRAS mutant melanoma patient tending to be older (>55 years old) and more likely to have a chronic history of UV-exposure (7, 8). The signaling of NRAS driven melanomas also differs from that of BRAF mutant melanomas in relying upon CRAF and phospho-diesterase IV activity to maintain MAPK signaling activity (9, 10). Unlike BRAF mutant melanomas which are highly sensitive to BRAF and MEK inhibition, responses of NRAS mutant melanomas to MEK inhibition are highly variable and it is likely that combination therapy strategies will be required (6, 11–14).
The heat shock protein (HSP)-90 family of chaperones plays a key role in maintaining the malignant potential of cancer cells by regulating the conformation, stability and function of many key receptors and kinases required for tumor initiation and maintenance (15, 16). A number of HSP90 client proteins, including CRAF, AKT, CDK4, ribosomal S6 and mutated BRAF, are known to be critical for melanoma progression, and there is now good evidence that the pharmacological inhibition of HSP90 is an excellent strategy for targeting multiple oncogenic pathways simultaneously (15, 17, 18). XL888 is a novel, orally available HSP90 inhibitor with good selectivity for HSP90α and HSP90β (IC50 - 22nM, 44nM, respectively) and little activity against a panel of 29 diverse kinases (IC50 all >3600 nM) (19). Recent studies from our lab showed XL888 to be highly effective at overcoming acquired BRAF inhibitor resistance in a panel of melanoma cell line models, including those in which resistance was mediated through mutant NRAS (20). In the current study, we show a requirement for CDK4, Wee1 and AKT inhibition in the anti-tumor effects of XL888 in NRAS mutant melanoma. Of these Wee1, is a checkpoint kinase implicated in the DNA repair response whose expression has been correlated with melanoma progression (21). Our studies support the further preclinical and clinical investigations of PI3K/AKT, CDK4 and Wee1 as well as HSP90 inhibitors in NRAS mutant melanoma.
Materials and Methods
Cell culture
The NRAS mutant cell lines WM852, WM1346, WM1361A, WM1366 and WMSbCl2, and the BRAF mutant cell line 1205Lu were a gift from Dr. Meenhard Herlyn (The Wistar Institute, Philadelphia, PA). The NRAS mutant cell lines M202, M207, M244, M245 and M318, and the BRAF mutant cell line M229 were a gift from Dr. Antoni Ribas (Jonsson Comprehensive Cancer Center, UCLA, Los Angeles, CA). Mcl-1 overexpressing cell lines WM1361A-MCL1 and WM1366-MCL1 were a gift from Dr. Andrew Aplin (Kimmel Cancer Center, Philadelphia, PA). The Coriell Institute cell identity mapping kit confirmed the identities of the Wistar cell lines. The UCLA cell line identity was confirmed by mitochondrial DNA analysis. All cell lines were verified in the past 6 months and were maintained in RPMI1640 with 5% FBS.
Proliferation Assay
Cells were plated in 96-well plates with 2.5 ×103 cells in 100uL medium per well overnight before being treated with increasing concentrations of drug. Metabolic activity was assayed after incubation with XL888 for 72 hours (XL888) or 120 hours (PD0332991, MK1775 and PI103), using Alamar Blue reagent according to manufacturers protocol (Invitrogen, Carlsbad, CA).
Cell Cycle Analysis
Cells were plated in 10cm dishes at 5.0×105 cells per dish and treated with 300nM XL888 the following day. After 24 hours, the cells were trypsinized, fixed with ethanol, stained with propidium iodide and analyzed by flow cytometry.
Apoptosis
Cells were plated in 6-well plates at 2.0 ×105 cells per well. The cells were treated with 300nM XL888 for 24–72hr before harvesting. Annexin V staining and flow cytometry analysis was performed as described in (22).
Western Blotting
Proteins were extracted and blotted for as described in (23). For mouse xenograft studies, tumor samples were harvested and immediately placed into RNAlater solution (Invitrogen) prior to protein extraction. After analysis, Western blots were stripped once and re-probed for GAPDH to confirm even protein loading. The following antibodies were obtained from Cell Signaling Technology (Beverly, MA): Akt (9272), phospho-Akt (4058), ARAF (4432), BAK (3814), BIM (2933), BRAF (9434), Cdc2 (9116), Cdc25A (3652), Chk1 (2360), CRAF (9422), p-CRAF-Ser338 (9427), ERK (9102), phospho-ERK (9101), HSP70 (4876), HSP90 (4877), Mcl1 (4572), phospho-p90RSK (9346), PARP (9542), Ral (4799), RB (9309), phospho-RB (9308), phospho-RSK2 (3556), S6 (2317), phospho-S6 (2215) and phospho-SAPK/JNK (4668). Antibodies for p21 (610233) and p27 (610241) were obtained from BD Biosciences (San Jose, CA). The antibody for p53 (OP43) was obtained from EMD Biosciences (San Diego, California). The antibody for GAPDH was obtained from Sigma Aldrich (St. Louis, MO).
Colony Formation Assay
Cells were plated in 96-well plates at 2×104 per well. Media with vehicle (DMSO) or XL888 (10, 30, 100 or 300 nM) was added the following day and replaced twice a week. After 4 weeks the plates were stained with crystal violet.
3D spheroid assays
Melanoma spheroids were prepared using the liquid overlay method (16). Spheroids were either treated for 144 hours with vehicle or 300nM XL888 before being washed and analyzed as described in (24).
RNA interference
Cells were plated in 6-well plates at 2.0 ×105 cells per well in RPMI complete media. The following day the media was replaced with 1ml Opti-MEM (Invitrogen) and the cells were transfected with 0.5ml complexes of Lipofectamine 2000 (0.5%, Invitrogen) and siRNA for either Mcl-1, BIM, BAK, Wee1 or non-targeting controls (40nM, Dharmacon On-Target Plus pools). Medium was replaced after 3–6 hours with 5% FBS in RPMI, and the cells were analyzed 120 hr after transfection. In the BIM and BAK studies, 300nM XL888 was also added 48 hours after transfection.
Real time Reverse transcription PCR
Cells were plated at 5.0×105 cells in 10cm dishes and treated the following day with 300 nM XL888. After 48 hours, total RNA was isolated using Qiagen’s RNeasy mini kit. The RNA levels were analyzed using TaqMan Gene Expression Assays primer/probes: Hs00197982_m1 (BIM), Hs01050896_m1 (MCL-1), P/N 4319413E (18S), and Hs99999905_m1 (GAPDH). The BIM and Mcl1 expression levels were normalized to 18S and GAPDH. Quantitative reverse transcriptase PCR (qRT-PCR) reactions were carried out as previously described (22).
Xenograft experiments
BALB SCID mice (Jackson Laboratory, Bar Harbor, ME) were subcutaneously injected with 2.5×106 cells in 150uL medium (L-15 with 10uM HEPES and 24% Matrigel). Tumors were grown to approximately 150–200mm3 prior to treatment. Mice were treated with 125mg/kg XL-888 or vehicle (10mM HCl) 3 times/week by oral gavage, and mouse weights and tumor volumes (L × W2/2) were measured at every treatment. Mice were gavaged a final time on day 18, and sacrificed the following day. Tumor biopsies were processed for LC-MRM analysis, western blotting and detection of apoptosis by TUNEL staining (Millipore), according to the manufacturer’s protocol.
Liquid chromatography - multiple reaction monitoring mass spectrometry (LC-MRM)
Proteins were extracted as described for Western Blotting. Sample processing and LC-MRM analysis was performed as described in (25). Data were then normalized to the pretreatment (cell lines) or vehicle controls (tissue) and plotted to show the changes in expression after drug treatment. Gene names for the UniPROT assignations of the HSP proteins are given in Supplemental Table 1.
Statistical analysis
Data show the mean of at least three independent experiments ± the S.E.M., unless stated otherwise. Statistically significant results were considered where P≤0.05.
Results
XL888 induces apoptosis and cell cycle arrest in NRAS mutant melanoma cell lines
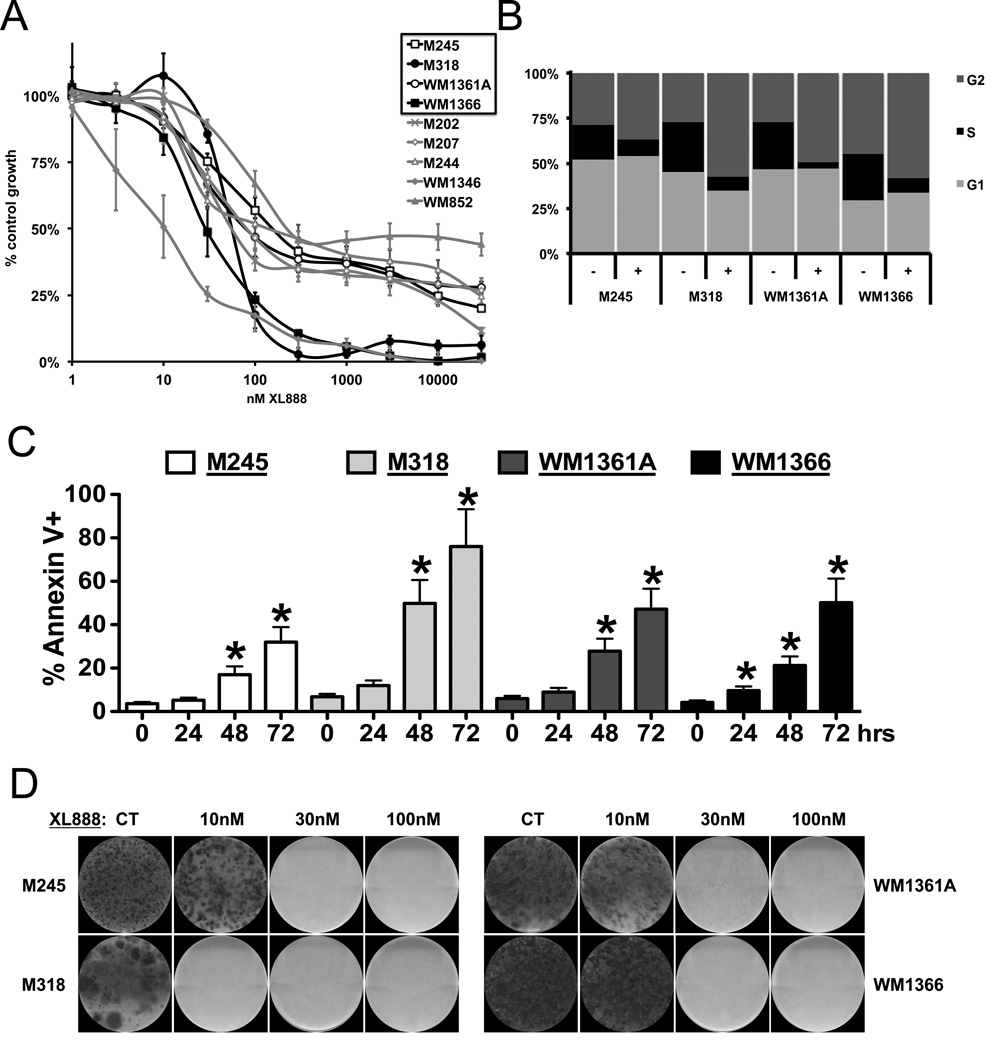
Treatment of a panel of nine NRAS mutant human melanoma cell lines with XL888 (Figure 1) was associated with concentration-dependent decreases in cell growth (Figure 2A). Four NRAS mutant cell lines (M245, M318, WM1361A, WM1366) that were representative of the larger cell line panel (2 sensitive and 2 less sensitive) were used for all subsequent experiments. The growth inhibitory effects of XL888 were associated with the induction of a G2/M phase cell cycle arrest (Figure 2B), and robust levels of apoptosis by 72 hours (Figure 2C). No colony formation was observed for any of the four cell lines following chronic XL888 (Figure 2D), with complete eradication of all M318 cells being observed at XL888 concentrations as low as 10nM (Figure 2D). The tumor selectivity of XL888 was confirmed through the lack of growth inhibitory/pro-apoptotic activity upon normal human fibroblast cell lines (20).
Figure 1.
The chemical structure of the HSP90 inhibitor XL888
Figure 2. The HSP90 inhibitor XL888 blocks the growth and survival of NRAS mutant melanoma cell lines.
A: Cells were treated with increasing concentrations of XL888 (1nM – 30 µM: 72 hrs) before analysis with the Alamar Blue assay. B: Cell cycle effects of XL888 (300 nM: 24 hrs) upon NRAS mutant melanoma lines. C: XL888 induces apoptosis in NRAS mutant melanoma cell lines. Cells were treated for 24, 48 and 72 hrs with XL888 (300 nM) followed by Annexin-V staining and flow cytometry. D: (Upper) Colony formation assay showing the long-term effectiveness of XL888. Cell lines were treated with 300nM XL888 for 4 weeks before being fixed and stained with crystal violet.
XL888 decreases the expression of key NRAS mutant melanoma signaling proteins
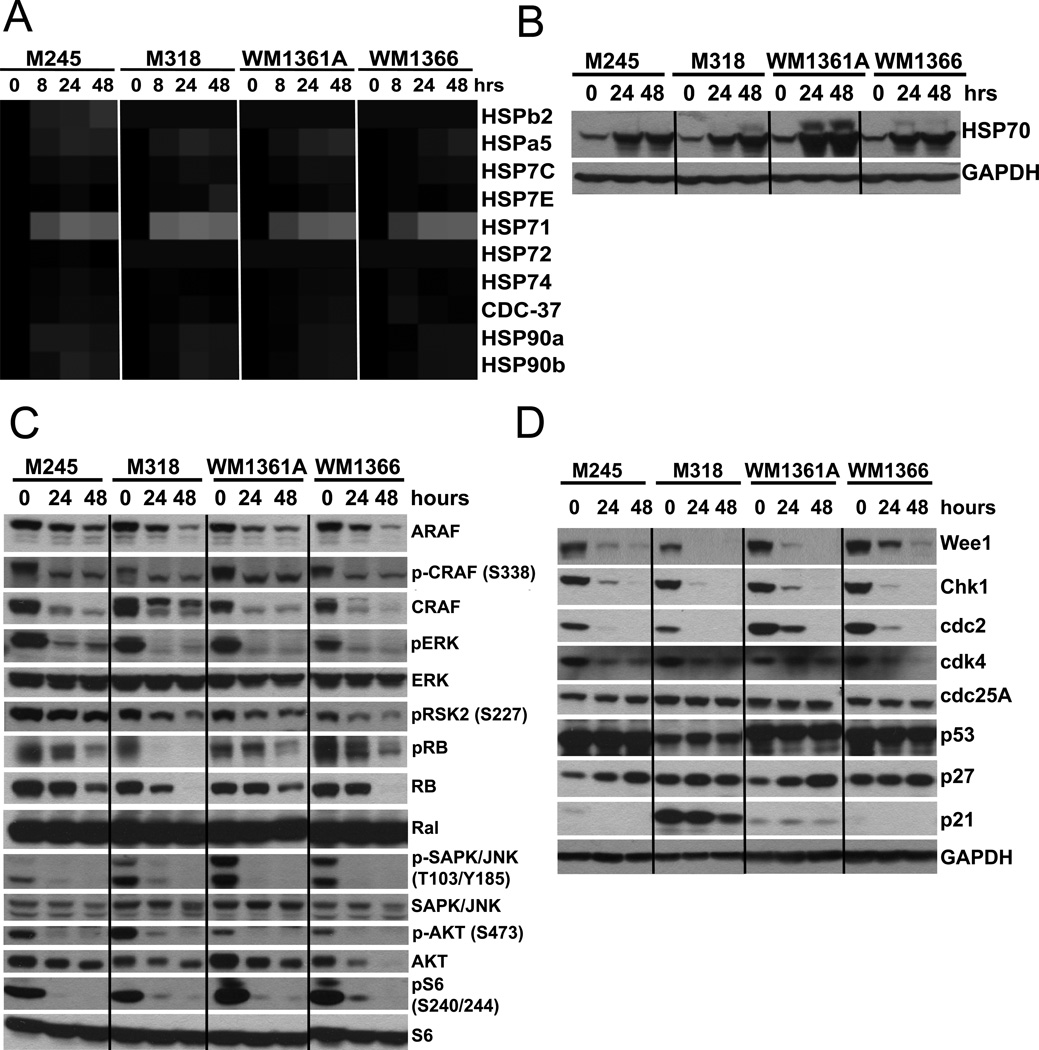
Mass spectrometry (LC-MRM) and Western blot studies showed the treatment of the NRAS mutant melanoma cell line panel with XL888 to be associated with the rapid (<8 hours) increase in the expression of the chaperone HSP70 isoform 1 (Figure 3A,B). XL888 also led to the decreased expression of many HSP client proteins including ARAF CRAF, CDK4, Wee1, CHK1, RB and cdc2 (Figures 3C,D). Together, the decreased expression of these HSP90 clients was associated with the abrogation of key melanoma signaling pathways, such as decreased phosphorylation of CRAF, ERK, AKT, RSK2 and S6 and the increased expression (in some cell lines) of p27KIP1 (Figure 3D). Little change in the expression of Ral, p53 or cdc25 was observed (Figures 3C,D).
Figure 3. XL888 increases HSP70 expression and degrades proteins involved in melanoma growth and survival.
A: Heatmap showing XL888-mediated increase in HSP70 isoform 1 (HSP71). B: Western blot confirming the LC-MRM data from panel A in four NRAS mutant melanoma cell lines. C: XL888 (300nM, 24 and 48 hrs) decreases ARAF, CRAF and AKT expression and inhibits pCRAF (Ser338), pAKT, pERK and pS6 in 4 NRAS mutant melanoma cell lines. D: XL888 mediated degradation of important cell cycle proteins. Treatment with XL888 (300nM, 24 and 48hrs) is associated with decreased expression of Wee1, Chk1, cdc2 and CDK4.
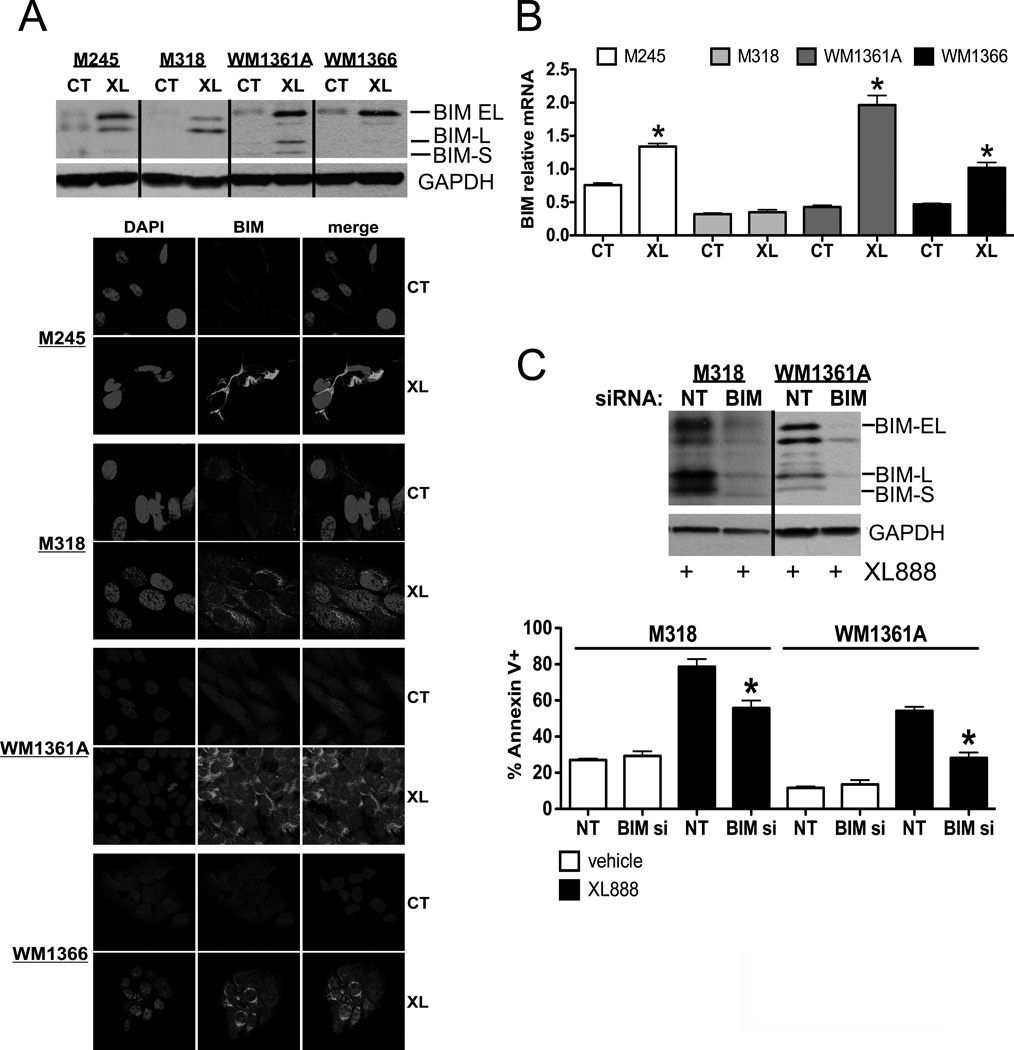
Increased expression of BIM is required for XL888-mediated apoptosis
In line with the ability of the HSP90 inhibitor to block pERK signaling (Figure 3C), XL888 also increased BIM protein expression (Figure 4A). Quantitative RT-PCR experiments revealed XL888 to increase expression of BIM mRNA in the M245, WM1361A and the WM1366 cell lines but not the M318 (Figure 4B). In the WM1361A and WM1366 cell lines, increased BIM mRNA expression was associated with nuclear relocalization of FOXO3a (Supplemental Figure 1). The knockdown of BIM expression using siRNA significantly reduced the extent of XL888-mediated apoptosis induction in the M318 and WM1361A cell lines (Figure 4C).
Figure 4. HSP90 inhibition is associated with BIM-mediated apoptosis in NRAS mutant melanoma cell lines.
(Upper) Western blot showing XL888-mediated (XL: 48 hrs, 300nM) BIM expression relative to control (CT) (Lower) Immunofluorescence experiment showing that XL888 (XL:300nM, 48 hrs) induces BIM (light gray) expression. B: XL888 (XL: 300 nM, 48 hrs) increases the expression of BIM at the mRNA level relative to control (CT). C: siRNA knockdown of XL888-mediated (300 nM, 48hrs) BIM expression significantly decreases apoptosis in two NRAS mutant melanoma cell lines (M318 and WM1361A) compared to non-targeting (NT) control. * Indicates a statistically significant difference where P<0.05.
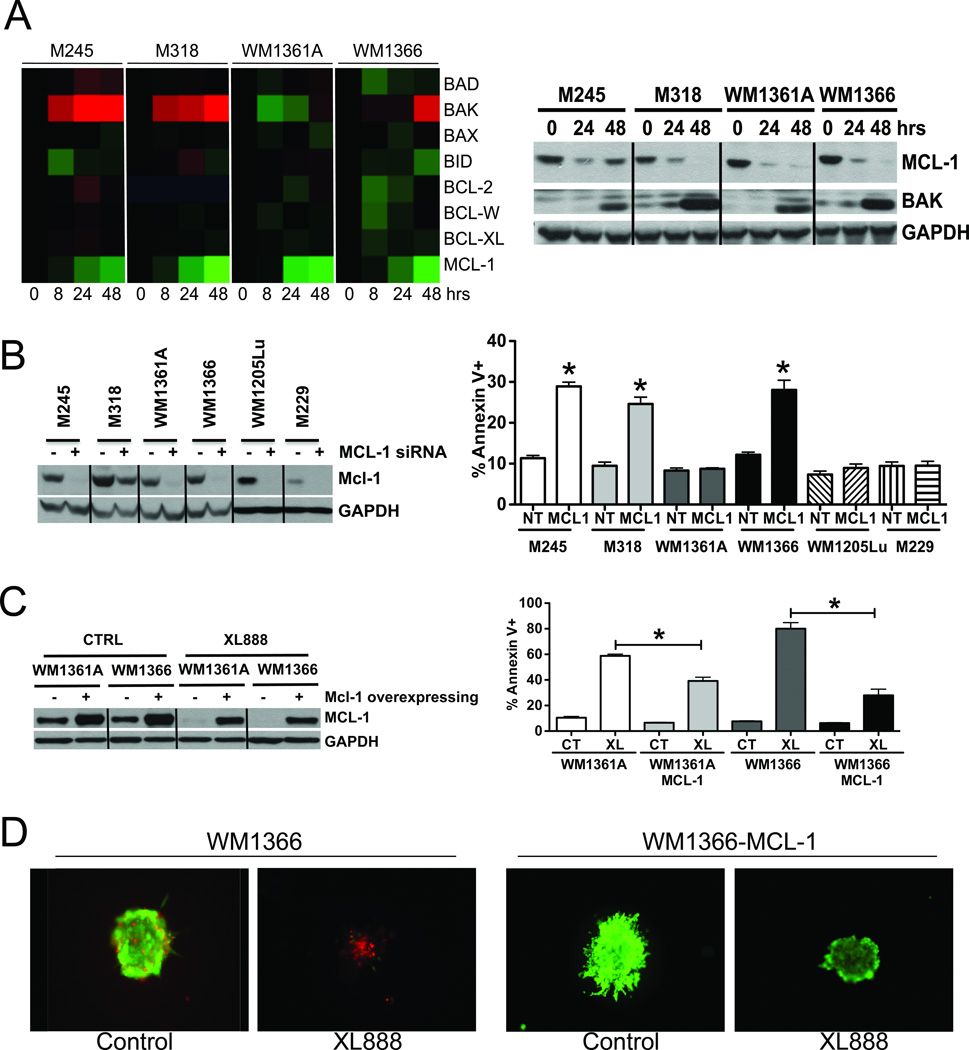
An LC-MRM screen identifies Mcl-1 as a key mediator of XL888-mediated apoptosis in NRAS mutant melanoma cell lines
As BIM knockdown only partly reversed XL888-mediated apoptosis, an LC-MRM assay was used to quantify expression of eight pro and anti-apoptotic BH3 family proteins following HSP90 inhibition. These proteomic analyses, which were confirmed by Western Blot, revealed XL888 to increase the expression of the pro-apoptotic protein BAK in three of the four cell lines in our panel (M245, M318 and WM1366), and to inhibit the mRNA and protein expression of the anti-apoptotic Mcl-1 protein in all four cell lines (Figure 5A and Supplemental Figure 2). In contrast, little change was seen in the levels of BAD, BAX, BID, Bcl-2, BCL-w and Bcl-XL. The role of increased BAK expression in XL888-mediated apoptosis was investigated by its siRNA knockdown followed by XL888 treatment (300 nM, 48 hours). Although good levels of BAK knockdown were observed in all four NRAS mutant cell lines, little effect was observed upon the level of HSP90-mediated apoptosis (Supplemental Figure 3).
Figure 5. Decreased Mcl-1 expression is required for XL888-mediated apoptosis.
A: (Left) Heatmap of LC-MRM screen shows XL888 to increase Bak expression and to decrease Mcl-1 expression in NRAS mutant melanoma cell lines. (Right) Western blot validation of the decreased Mcl-1 expression and increased Bak expression following XL888 (300nM, 48 hrs). B: siRNA knockdown of Mcl-1 increases apoptosis in NRAS mutant melanoma cells but not 2 BRAF mutant melanoma cell lines. (Left) Western blot shows the efficiency of the Mcl-1 knockdown. (Right) Mcl-1 knockdown increases apoptosis in the M245, M318 and WM1366 NRAS mutant melanoma cell lines. Apoptosis was measured by Annexin-V binding and flow cytometry. C: Mcl-1 attenuates XL888 induced apoptosis. (Left) Western blot showing increased expression of Mcl-1 in WM1366 and WM1361A cell lines following lentiviral infection. (Right) Mcl-1 overexpression attenuates XL888-mediated (XL) apoptosis as measured by Annexin-V binding as compared to control (CT). * Indicates a significant difference from control where P<0.05. D: Mcl-1 prevents XL888-induced cell death in 3D culture. Control and Mcl-1 overexpressing WM1366 spheroids were treated with either vehicle or XL888 (300nM) for 5 days before being treated with Live/Dead stain. Green: live cells and Red: dead cells.
The role of Mcl-1 the survival of NRAS mutant melanoma was confirmed in siRNA knockdown experiments, where depletion of the protein led to apoptosis in the M245, M318 and WM1366 cell lines (Figure 5B). In contrast, knockdown of Mcl-1 was associated with very little apoptosis in two melanoma cell lines harboring BRAF V600E mutations (1205Lu and M229: Figure 5B). We next addressed whether overexpression of Mcl-1 conveyed protection to XL888-mediated apoptosis by generating two isogenic NRAS mutant melanoma cell lines that stably overexpressed Mcl-1 (WM1366 MCL-1 and WM1361A MCL-1). It was noted that whereas XL888 treatment degraded Mcl-1 in the parental cell lines, Mcl-1 expression was maintained in the overexpressing cell lines (Figure 5C). The importance of Mcl-1 degradation in the cytotoxic activity of XL888 was demonstrated by the ability of Mcl-1 overexpression to significantly attenuate levels of apoptosis and to enhance cell survival in a 3D collagen implanted spheroid model (Figures 5C,D). XL888 treatment also enhanced the effects of the BH3 family protein antagonist ABT-737 (which does not impact Mcl-1) in the WM1366 and WM131A cell lines in both apoptosis and 3D spheroid assays (Supplemental Figures 4,5).
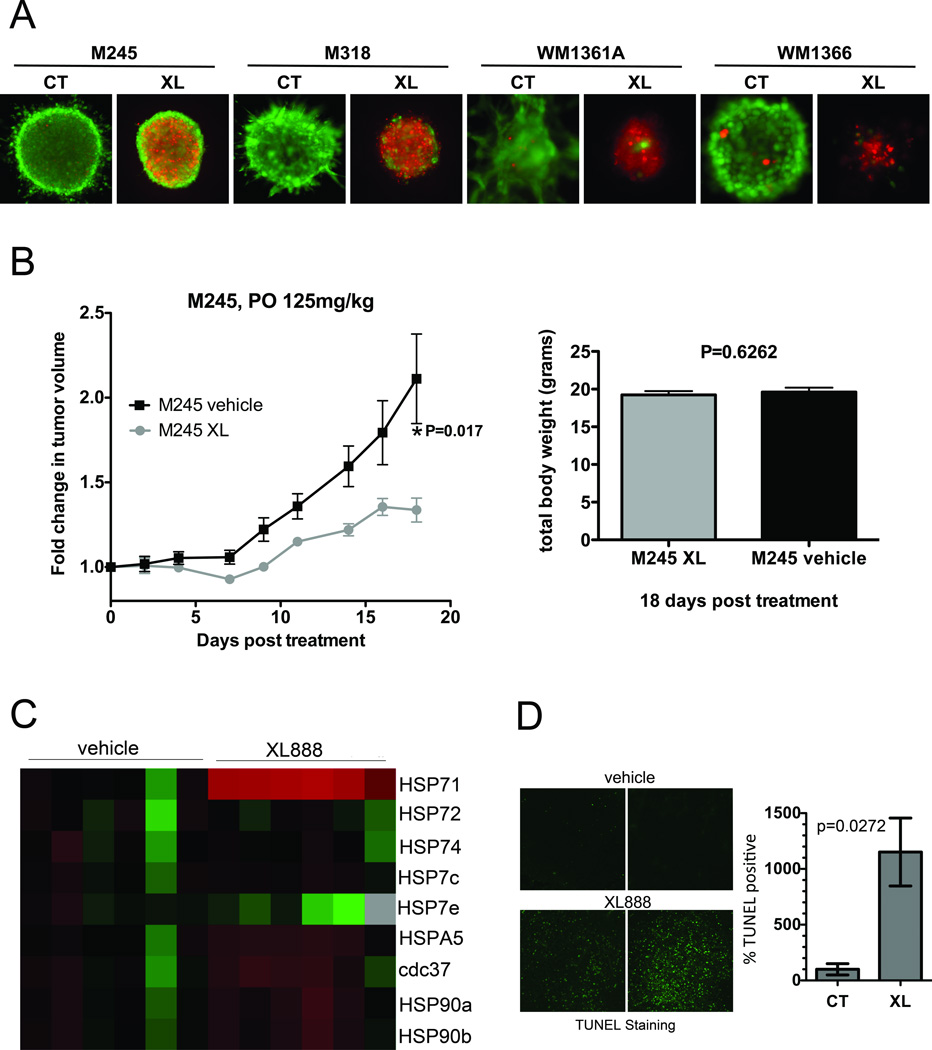
XL888 is cytotoxic against NRAS mutant melanoma cell xenografts through a mechanism involving the degradation of Wee1, CDK4 and decreased AKT/mTOR signaling
In 3D cell culture, XL888 reduced the survival of all of the NRAS mutant melanoma cell lines evaluated (Figure 6A). The trend of sensitivity across the panel of four cell lines was similar to that observed in the apoptosis experiments, with M245 being less sensitive than the other cell lines (Figures 2C, 6A). Of the four NRAS mutant melanoma cell lines evaluated, only the M245 formed xenografts in SCID mice. Treatment of the established M245 tumors with XL888 (125mg/kg 3× week) led to a significant slowing of tumor growth (P=0.017) without any effect upon animal weights (Figures 6A,B). Analysis of xenograft specimens by LC-MRM showed a marked increase in intratumoral HSP70 expression following XL888 treatment (Figure 6C). Mechanistically, XL888 was noted to induce apoptosis, as shown by an increase in TUNEL staining (Figure 6D).
Figure 6. XL888 inhibits growth of NRAS mutant melanoma cells in 3D cell culture and a mouse xenograft model.
A: XL888 (XL: 300nM, 5 days) induces cell death 3D spheroids compared to control (CT). Green: live cells and Red: dead cells. B: XL888 inhibits the growth of M245 melanoma xenografts. Animals bearing M245 xenografts were treated with XL888 thrice per week (125 mg/kg). Data shows growth curves normalized to starting volumes, bar graph shows mean tumor volumes after 18 days of XL888 treatment. XL888 treatment led to significant levels of growth inhibition (P=0.017). C: Heatmap showing the increase in HSP70 isoform 1 (HSP71) expression in XL888 treated (15 days, 125 mg/kg) xenograft samples compared to vehicle controls. D: XL888 treatment (10 days) led to the induction of apoptosis in established M245 xenografts as measured by increased TUNEL staining (green).
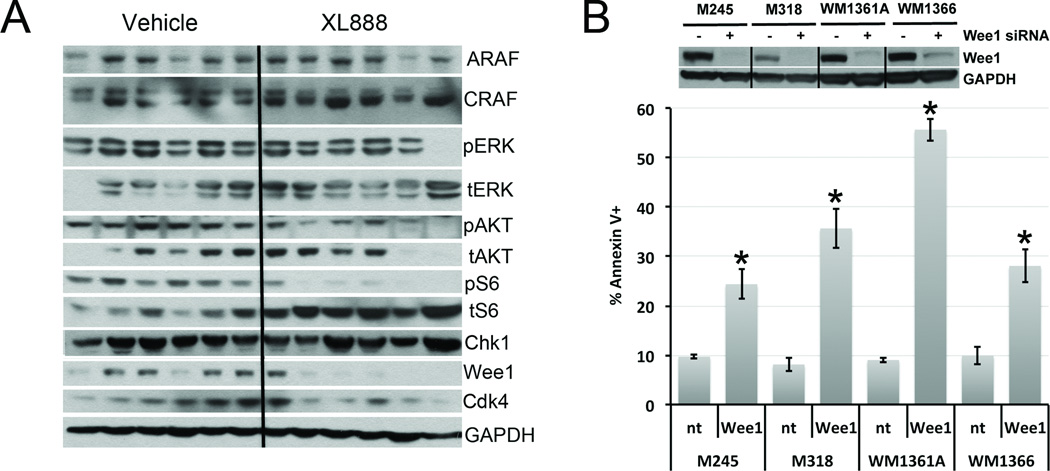
In vivo responses to XL888 are associated with degradation of Wee1 and CDK4 and inhibition of AKT/S6 signaling
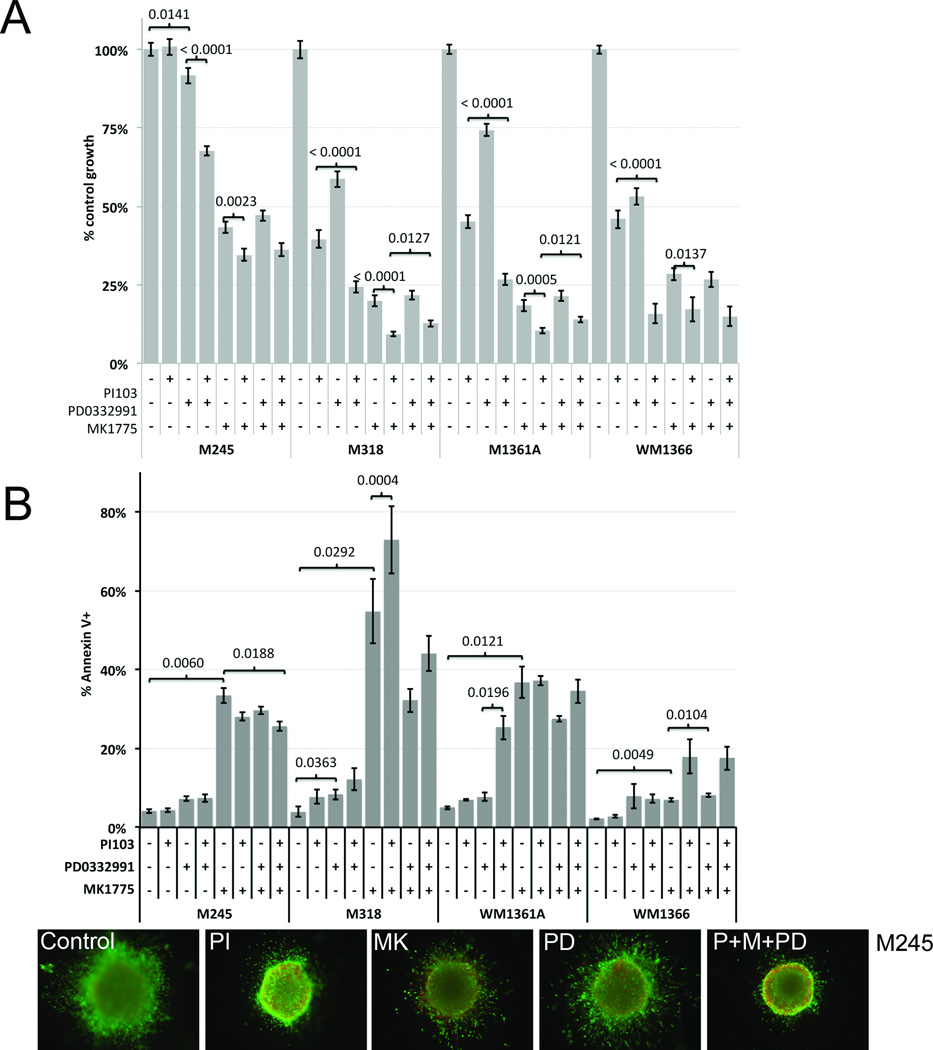
In vivo, XL888 decreased expression of CDK4, S6 and Wee1 and inhibited pAKT and pS6 signaling (Figure 7A). In contrast to the decrease of ARAF and CRAF expression and the suppression of MAPK signaling observed following XL888 treatment in the in vitro studies (Figure 3C), little change was observed in any of these signaling molecules in the xenograft specimens (Figure 7A). Inhibition of Wee1 expression using siRNA knockdown was associated with significant levels of apoptosis induction in three of the four NRAS mutant melanoma cell lines (Figure 7B). We next evaluated a panel of small molecule inhibitors of CDK4 (PD0322991), PI3K/AKT/mTOR (PI-103) and Wee1 (MK1775) on the growth and survival of NRAS mutant melanoma cell lines. Of these, MK1775 had the most potent growth inhibitory activity when used as a single agent, and the addition of PI-103 significantly enhanced these effects in all four cell lines (Figure 8A). In addition, the combination of PI-103 and PD0322991 led to significantly more growth inhibition than either agent alone in all of the cell lines (Figure 8A). With regards to apoptosis, only the Wee1 inhibitor MK1775 induced significant levels of cell death across all four cell lines when used as a single agent (Figure 8B). Some heterogeneity of response was observed when the inhibitors were combined. The combination of MK1775 and PI-103 induced more apoptosis in the WM1366 cell line compared to either agent alone. In the WM1361A cell line, the combination of PD0322991 and PI-103 was significantly more cytotoxic than each individual agent (Figure 8B). In a 3D spheroid assay, the combination of PI-103, MK1775 and PD032291 reduced invasion and survival of M245 melanoma cells compared to each agent alone (Figure 8B).
Figure 7. XL888 treatment leads to the degradation of CDK4, Wee1 and the AKT/S6 signaling in NRAS mutant melanoma cells in vivo.
A: Western blot analysis identifies degradation of CDK4, Wee1 and inhibition of AKT/S6 following the in vivo treatment of M245 cell xenografts with XL888. B: Wee1 expression is required for the survival of NRAS mutant melanoma cell lines. (Upper) Western blot showing the efficiency of knockdown following treatment with an siRNA against Wee1. (lower) Apoptosis induction (% Annexin V binding) following treatment with an siRNA against Wee1 for 120 hr.
Figure 8. Pharmacological inhibition of Wee1 reduces growth and induces apoptosis in NRAS mutant melanoma cell lines.
A: Inhibition of CDK4, Wee1 and PI3K/AKT inhibits growth of NRAS mutant melanoma cells. Cells were treated with PD0322991 (300 nM), PI-103 (300nM), MK1775 (1µM) or combinations of the drugs for 5 days, before being analyzed using the Alamar Blue assay. B: (Upper) The effects of CDK4, Wee1 and PI3K/AKT/mTOR inhibitors on the survival of NRAS mutant melanoma cells. Cells were treated with PD0322991 (300 nM), PI-103 (300nM), MK1775 (1µM) or combinations of the drugs for 5 days followed by Annexin-V staining and flow cytometry. (lower) Combination of PI-103 (PI), MK1775 (MK) and PD0322991 (PD) (concs as above) prevents survival and invasion of M245 melanoma spheroids. Spheres were treated with drugs for 5 days before being stained for viability and imaged.
Discussion
The current study addresses the mechanism of action of the HSP90 inhibitor XL888 in NRAS mutant melanoma. We observed that HSP90 inhibition decreased signaling through the Raf/MEK/ERK/CDK4 and PI3K/AKT pathways; two signal transduction cascades known to be important for the growth and survival of Ras mutant cell lines and tumors (26). From a mechanistic standpoint, the MEK/ERK and PI3K/AKT pathways converge at the level of cell survival through the regulation of the pro-apoptotic proteins BAD and BIM as well as cap-dependent protein translation via 4E-BP1 signaling (20, 27–29). In NRAS mutant melanoma, previous studies have shown that dual MEK and PI3K/mTOR inhibition, as well as concurrent shRNA knockdown of BRAF and PI3K, are associated with decreased cell growth and a delay in tumor formation in vivo (30, 31).
Melanoma cells are known to be particularly resistant to cell death, and typically show increased expression of anti-apoptotic proteins such as Bcl-2 and Mcl-1 as well as having constitutive activity in many signaling pathways that downregulate the expression of pro-apoptotic proteins such as BIM (32–35). In BRAF mutant melanoma cells, signaling through the MAPK pathway downregulates BIM expression through MEK/ERK mediated phosphorylation at Ser69, leading to its proteasome-mediated destruction (33). Inhibition of BRAF through use of small molecule inhibitors and siRNA knockdown induces cell death in melanoma cells in part through the binding of BIM to Bcl-2, Bcl-w, Bcl-XL, and Mcl-1, which antagonizes their pro-survival function (22, 34). In line with the known role of the MAPK pathway in regulating BIM expression, XL888 treatment led to the degradation of ARAF/CRAF expression, the inhibition of the MAPK pathway and increased BIM expression.
Mcl-1 is a pro-survival protein first identified in myeloma that exerts its anti-apoptotic activity by binding to BIM-EL and through the inhibition of pro-apoptotic Bak/Bax (36, 37). In melanoma, Mcl-1 has been implicated in the protection from anoikis; its overexpression also confers resistance to cytotoxic chemotherapy agents, radiation and the proteasome inhibitor bortezomib (38–40). Expression of Mcl-1 is regulated both at the transcriptional level through the PI3K/AKT signaling pathway and post-translationally through MEK/ERK-mediated phosphorylation at T163, which prevents its degradation by the proteasome (36, 41). An important role for Mcl-1 downregulation in the observed cytotoxic activity of XL888 was suggested by the ability of Mcl-1 siRNA knockdown to induce cell death across our NRAS mutant melanoma cell line panel and the observation that Mcl-1 overexpression reversed XL888-induced apoptosis. Further studies also showed XL888 to enhance the pro-apoptotic activity of ABT-737 (a Bcl-2/Bcl-XL antagonist with little activity against Mcl-1) in 2 NRAS mutant melanoma cell lines (42). Taken together, our results suggest that the simultaneous increase in BIM and inhibition of Mcl-1 expression underlies the potent long-lasting anti-tumor activity seen following XL888 treatment in our adherent culture system. The ability to downregulate Mcl-1 expression while increasing BIM expression would appear to be a prerequisite for any future therapy developed for NRAS mutant melanoma. Further studies will be required to determine whether NRAS mutant melanomas are uniquely dependent upon the pro-survival activity of Mcl-1.
Treatment of melanoma cells grown in vitro and in vivo with XL888 was associated with increased expression of HSP70 isoform 1, a protein often used as a biomarker of HSP90 inhibition (20). Although increased HSP70 expression has been implicated in reduced HSP90 inhibitor-mediated apoptotic responses in leukemic cells, its role in melanoma has not yet been established (43). Analysis of HSP90 client levels by Western blot revealed distinct patterns of degradation between the adherent cell culture and animal experiments. Under in vivo conditions, XL888 treatment was not associated with decreased expression of ARAF or CRAF and little inhibition of MAPK signaling was observed. Instead, it was noted that XL888 treatment led to the reduction of CDK4 and Wee1 expression and the inhibition of AKT and S6 signaling. The differences in XL888-mediated client protein degradation between the in vitro and in vivo experiments are not currently well understood. Expression of ARAF and CRAF, in particular, was not reduced despite being recently described as “strong” HSP90 clients (the 6th and 11th strongest HSP90 interactors, respectively) (44). Although there is known to be some correlation between the strength of the HSP90/kinase interaction and the likelihood of client degradation following HSP90 inhibition (e.g. strong clients are more likely to be degraded than weak clients), this is not universal and some strong clients are not degraded following HSP90 inhibitor-mediated chaperone dissociation (44). One possible explanation for the observed differences in client degradation between adherent cell culture and the in vivo model are the marked changes in the patterns of intracellular signaling seen in melanoma cells grown under different microenvironmental conditions. Previous studies from our lab have shown the MAPK signaling pathway to be differentially regulated between the same BRAF mutant melanoma cell lines grown as either 2D or 3D cell cultures (12). Whether these focal differences in signaling are reflected in altered interactions between ARAF/CRAF and the HSP chaperones remains to be determined. These observations clearly illustrate the need to screen large panels of HSP client proteins when investigating the mechanisms of action of HSP90 inhibitors.
The validity of co-targeting CDK4 and PI3K/AKT signaling simultaneously in NRAS mutant melanoma cell lines was confirmed by the significant increases in growth inhibition observed following treatment with the PI3K/mTOR inhibitor PI-103 in combination with the CDK4 inhibitor PD0322991 compared to either agent alone. Previous work has already indicated that BRAF and NRAS mutant melanoma cells are sensitive to inhibition of CDK4/6 and undergo senescence when treated with PD0322991 (45). A potential role for PI3K/AKT signaling in regulating the entry of melanocytes from BRAF-induced senescence has also been recently demonstrated (46). These data suggest that combined PI3K/CDK4 inhibition could be one strategy to induce a maximal senescence response in melanoma cells. Interestingly, the CDK4/PI3K inhibitor combination induced only limited apoptosis in three out of the four NRAS melanoma cell lines, suggesting that other mechanisms were responsible for the XL888-induced cytotoxicity observed in our xenograft model.
Wee1 is a tyrosine kinase and HSP90 client protein that negatively regulates the G2/M checkpoint. Previous studies have shown that abrogation of Wee1 function enhances the anti-tumor activity of DNA damaging agents such as radiation and some chemotherapy drugs (47, 48). A small molecule inhibitor of Wee1, MK1775, has cytotoxic activity in a number of tumor types including sarcoma, where it induces apoptosis through inappropriate mitotic entry (48, 49). In melanoma, Wee1 expression levels increase with tumor stage, with high levels of Wee1 being correlated with greater rates of ulceration and a poorer disease free survival (21). In BRAF mutant melanoma cell lines, siRNA knockdown of Wee1 leads to a DNA damage response and apoptosis (21). Our data provide the first evidence that Wee1 inhibition, through siRNA knockdown or Wee1/HSP90 inhibition, leads to growth inhibition and apoptosis in NRAS mutant melanoma cell lines. We further show that Wee1 a is highly sensitive HSP90 client in melanoma cells grown both in vivo and under tissue culture conditions, and demonstrate that its degradation may underlie the anti-tumor activity seen to XL888.
Emerging evidence suggests that NRAS mutant melanomas show a greater diversity of response to targeted therapy agents than their BRAF mutant counterparts, and many possible combination therapy strategies have been suggested (11, 14). There is already evidence of synergy between MEK and CDK4 inhibitors in mouse and human models of NRAS mutant melanoma, although it is not yet clear what percentage of these tumors will show susceptibility to this combination (50). In the current study we demonstrate the potential utility of Wee1 inhibition and combined CDK4 and PI3K/AKT/mTOR inhibition in NRAS mutant melanoma. It is hoped that the development of rational combination therapy strategies for NRAS mutant melanoma will yield similar successes to those that have been seen in BRAF mutant melanoma.
Supplementary Material
Acknowledgements
We would like to thank Dana Aftab (Exelixis) for providing the XL888 for these studies. We also thank Laura Hall (Moffitt Molecular Biology Core) for assistance with the qRT-PCR experiments.
Grant support: K.S.M. Smalley was supported by the NIH/National Cancer Institute (R01 CA161107-01), the Harry Lloyd Trust and the Bankhead-Coley Research Program of the State of Florida (09BN-14).
Footnotes
Disclosure of conflicts of interest:
None of the authors declare any conflict of interest.
References
- 1.Downward J. Targeting RAS signalling pathways in cancer therapy. Nat Rev Cancer. 2003;3:11–22. doi: 10.1038/nrc969. [DOI] [PubMed] [Google Scholar]
- 2.Malumbres M, Barbacid M. RAS oncogenes: the first 30 years. Nature reviews Cancer. 2003;3:459–465. doi: 10.1038/nrc1097. [DOI] [PubMed] [Google Scholar]
- 3.Bollag G, Hirth P, Tsai J, Zhang J, Ibrahim PN, Cho H, et al. Clinical efficacy of a RAF inhibitor needs broad target blockade in BRAF-mutant melanoma. Nature. 2010;467:596–599. doi: 10.1038/nature09454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chapman PB, Hauschild A, Robert C, Haanen JB, Ascierto P, Larkin J, et al. Improved Survival with Vemurafenib in Melanoma with BRAF V600E Mutation. N Engl J Med. 2011 doi: 10.1056/NEJMoa1103782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smalley KSM, McArthur GA. The Current State of Targeted Therapy in Melanoma: This Time It's Personal. Seminars in Oncology. 2012;39:204–214. doi: 10.1053/j.seminoncol.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fedorenko IV, Gibney GT, Smalley KS. NRAS mutant melanoma: biological behavior and future strategies for therapeutic management. Oncogene. 2012 doi: 10.1038/onc.2012.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jakob JA, Bassett RL, Ng CS, Curry JL, Joseph RW, Alvarado GC, et al. NRAS mutation status is an independent prognostic factor in metastatic melanoma. Cancer. 2012;118:4014–4023. doi: 10.1002/cncr.26724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Devitt B, Liu W, Salemi R, Wolfe R, Kelly J, Tzen CY, et al. Clinical outcome and pathological features associated with NRAS mutation in cutaneous melanoma. Pigm Cell Melanoma R. 2011;24:666–672. doi: 10.1111/j.1755-148X.2011.00873.x. [DOI] [PubMed] [Google Scholar]
- 9.Dumaz N, Hayward R, Martin J, Ogilvie L, Hedley D, Curtin JA, et al. In Melanoma, RAS Mutations Are Accompanied by Switching Signaling from BRAF to CRAF and Disrupted Cyclic AMP Signaling. Cancer Res. 2006;66:9483–9491. doi: 10.1158/0008-5472.CAN-05-4227. [DOI] [PubMed] [Google Scholar]
- 10.Marquette A, Andre J, Bagot M, Bensussan A, Dumaz N. ERK and PDE4 cooperate to induce RAF isoform switching in melanoma. Nat Struct Mol Biol. 2011;18:584–591. doi: 10.1038/nsmb.2022. [DOI] [PubMed] [Google Scholar]
- 11.Solit DB, Garraway LA, Pratilas CA, Sawai A, Getz G, Basso A, et al. BRAF mutation predicts sensitivity to MEK inhibition. Nature. 2006;439:358–362. doi: 10.1038/nature04304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haass NK, Sproesser K, Nguyen TK, Contractor R, Medina CA, Nathanson KL, et al. The mitogen-activated protein/extracellular signal-regulated kinase kinase inhibitor AZD6244 (ARRY-142886) induces growth arrest in melanoma cells and tumor regression when combined with docetaxel. Clin Cancer Res. 2008;14:230–239. doi: 10.1158/1078-0432.CCR-07-1440. [DOI] [PubMed] [Google Scholar]
- 13.Ascierto PA, Berking C, Agarwala SS, Schadendorf D, Van Herpen C, Queirolo P, et al. Efficacy and safety of oral MEK162 in patients with locally advanced and unresectable or metastatic cutaneous melanoma harboring BRAFV600 or NRAS mutations. J Clin Oncol. 2012;30:8511. [Google Scholar]
- 14.Barretina J, Caponigro G, Stransky N, Venkatesan K, Margolin AA, Kim S, et al. The Cancer Cell Line Encyclopedia enables predictive modelling of anticancer drug sensitivity. Nature. 2012;483:603–607. doi: 10.1038/nature11003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trepel J, Mollapour M, Giaccone G, Neckers L. Targeting the dynamic HSP90 complex in cancer. Nature reviews Cancer. 2010;10:537–549. doi: 10.1038/nrc2887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taipale M, Jarosz DF, Lindquist S. HSP90 at the hub of protein homeostasis: emerging mechanistic insights. Nature reviews Molecular cell biology. 2010;11:515–528. doi: 10.1038/nrm2918. [DOI] [PubMed] [Google Scholar]
- 17.Grbovic OM, Basso AD, Sawai A, Ye Q, Friedlander P, Solit D, et al. V600E B-Raf requires the Hsp90 chaperone for stability and is degraded in response to Hsp90 inhibitors. Proc Natl Acad Sci U S A. 2006;103:57–62. doi: 10.1073/pnas.0609973103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.da Rocha Dias S, Friedlos F, Light Y, Springer C, Workman P, Marais R. Activated B-RAF is an Hsp90 client protein that is targeted by the anticancer drug 17-allylamino-17-demethoxygeldanamycin. Cancer Res. 2005;65:10686–10691. doi: 10.1158/0008-5472.CAN-05-2632. [DOI] [PubMed] [Google Scholar]
- 19.Lyman SK, Crawley SC, Gong R, Adamkewicz JI, McGrath G, Chew JY, et al. High-content, high-throughput analysis of cell cycle perturbations induced by the HSP90 inhibitor XL888. PLoS ONE. 2011;6:e17692. doi: 10.1371/journal.pone.0017692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Paraiso KHT, Haarberg HE, Wood E, Rebecca VW, Chen YA, Xiang Y, et al. The HSP90 Inhibitor XL888 Overcomes BRAF Inhibitor Resistance Mediated through Diverse Mechanisms. Clinical Cancer Research. 2012;18:2502–2514. doi: 10.1158/1078-0432.CCR-11-2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Magnussen GI, Holm R, Emilsen E, Rosnes AK, Slipicevic A, Florenes VA. High expression of Wee1 is associated with poor disease-free survival in malignant melanoma: potential for targeted therapy. PLoS ONE. 2012;7:e38254. doi: 10.1371/journal.pone.0038254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paraiso KH, Xiang Y, Rebecca VW, Abel EV, Chen YA, Munko AC, et al. PTEN loss confers BRAF inhibitor resistance to melanoma cells through the suppression of BIM expression. Cancer Res. 2011;71:2750–2760. doi: 10.1158/0008-5472.CAN-10-2954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smalley KS, Contractor R, Haass NK, Lee JT, Nathanson KL, Medina CA, et al. Ki67 expression levels are a better marker of reduced melanoma growth following MEK inhibitor treatment than phospho-ERK levels. Br J Cancer. 2007;96:445–449. doi: 10.1038/sj.bjc.6603596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smalley KS, Haass NK, Brafford PA, Lioni M, Flaherty KT, Herlyn M. Multiple signaling pathways must be targeted to overcome drug resistance in cell lines derived from melanoma metastases. Mol Cancer Ther. 2006;5:1136–1144. doi: 10.1158/1535-7163.MCT-06-0084. [DOI] [PubMed] [Google Scholar]
- 25.Remily-Wood ER, Liu RZ, Xiang Y, Chen Y, Thomas CE, Rajyaguru N, et al. A database of reaction monitoring mass spectrometry assays for elucidating therapeutic response in cancer. Proteomics Clinical applications. 2011;5:383–396. doi: 10.1002/prca.201000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Engelman JA, Chen L, Tan X, Crosby K, Guimaraes AR, Upadhyay R, et al. Effective use of PI3K and MEK inhibitors to treat mutant Kras G12D and PIK3CA H1047R murine lung cancers. Nat Med. 2008;14:1351–1356. doi: 10.1038/nm.1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.She QB, Solit DB, Ye Q, O'Reilly KE, Lobo J, Rosen N. The BAD protein integrates survival signaling by EGFR/MAPK and PI3K/Akt kinase pathways in PTEN-deficient tumor cells. Cancer Cell. 2005;8:287–297. doi: 10.1016/j.ccr.2005.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.She QB, Halilovic E, Ye Q, Zhen W, Shirasawa S, Sasazuki T, et al. 4E-BP1 Is a Key Effector of the Oncogenic Activation of the AKT and ERK Signaling Pathways that Integrates Their Function in Tumors. Cancer Cell. 2010;18:39–51. doi: 10.1016/j.ccr.2010.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shao Y, Aplin AE. Akt3-mediated resistance to apoptosis in B-RAF-targeted melanoma cells. Cancer Res. 2010;70:6670–6681. doi: 10.1158/0008-5472.CAN-09-4471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jaiswal BS, Janakiraman V, Kljavin NM, Eastham-Anderson J, Cupp JE, Liang Y, et al. Combined targeting of BRAF and CRAF or BRAF and PI3K effector pathways is required for efficacy in NRAS mutant tumors. PLoS One. 2009;4:e5717. doi: 10.1371/journal.pone.0005717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Greger JG, Eastman SD, Zhang VV, Bleam MR, Hughes AM, Smitheman KN, et al. Combinations of BRAF, MEK, and PI3K/mTOR Inhibitors Overcome Acquired Resistance to the BRAF Inhibitor GSK2118436 Dabrafenib, Mediated by NRAS or MEK Mutations. Molecular Cancer Therapeutics. 2012;11:909–920. doi: 10.1158/1535-7163.MCT-11-0989. [DOI] [PubMed] [Google Scholar]
- 32.Soengas MS, Lowe SW. Apoptosis and melanoma chemoresistance. Oncogene. 2003;22:3138–3151. doi: 10.1038/sj.onc.1206454. [DOI] [PubMed] [Google Scholar]
- 33.Cartlidge RA, Thomas GR, Cagnol S, Jong KA, Molton SA, Finch AJ, et al. Oncogenic BRAF(V600E) inhibits BIM expression to promote melanoma cell survival. Pigment Cell Melanoma Res. 2008;21:534–544. doi: 10.1111/j.1755-148X.2008.00491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Boisvert-Adamo K, Aplin AE. Mutant B-RAF mediates resistance to anoikis via Bad and Bim. Oncogene. 2008;27:3301–3312. doi: 10.1038/sj.onc.1211003. [DOI] [PubMed] [Google Scholar]
- 35.Ley R, Balmanno K, Hadfield K, Weston C, Cook SJ. Activation of the ERK1/2 signaling pathway promotes phosphorylation and proteasome-dependent degradation of the BH3-only protein, Bim. J Biol Chem. 2003;278:18811–18816. doi: 10.1074/jbc.M301010200. [DOI] [PubMed] [Google Scholar]
- 36.Wang JM, Chao JR, Chen W, Kuo ML, Yen JJ, Yang-Yen HF. The antiapoptotic gene mcl-1 is up-regulated by the phosphatidylinositol 3-kinase/Akt signaling pathway through a transcription factor complex containing CREB. Molecular and Cellular Biology. 1999;19:6195–6206. doi: 10.1128/mcb.19.9.6195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kozopas KM, Yang T, Buchan HL, Zhou P, Craig RW. MCL1, a gene expressed in programmed myeloid cell differentiation, has sequence similarity to BCL2. Proceedings of the National Academy of Sciences of the United States of America. 1993;90:3516–3520. doi: 10.1073/pnas.90.8.3516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boisvert-Adamo K, Longmate W, Abel EV, Aplin AE. Mcl-1 is required for melanoma cell resistance to anoikis. Mol Cancer Res. 2009;7:549–556. doi: 10.1158/1541-7786.MCR-08-0358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thallinger C, Wolschek MF, Wacheck V, Maierhofer H, Gunsberg P, Polterauer P, et al. Mcl-1 antisense therapy chemosensitizes human melanoma in a SCID mouse xenotransplantation model. The Journal of investigative dermatology. 2003;120:1081–1086. doi: 10.1046/j.1523-1747.2003.12252.x. [DOI] [PubMed] [Google Scholar]
- 40.Qin JZ, Xin H, Sitailo LA, Denning MF, Nickoloff BJ. Enhanced killing of melanoma cells by simultaneously targeting Mcl-1 and NOXA. Cancer Research. 2006;66:9636–9645. doi: 10.1158/0008-5472.CAN-06-0747. [DOI] [PubMed] [Google Scholar]
- 41.Domina AM, Vrana JA, Gregory MA, Hann SR, Craig RW. MCL1 is phosphorylated in the PEST region and stabilized upon ERK activation in viable cells, and at additional sites with cytotoxic okadaic acid or taxol. Oncogene. 2004;23:5301–5315. doi: 10.1038/sj.onc.1207692. [DOI] [PubMed] [Google Scholar]
- 42.Chen S, Dai Y, Harada H, Dent P, Grant S. Mcl-1 down-regulation potentiates ABT-737 lethality by cooperatively inducing bak activation and bax translocation. Cancer Research. 2007;67:782–791. doi: 10.1158/0008-5472.CAN-06-3964. [DOI] [PubMed] [Google Scholar]
- 43.Beere HM. "The stress of dying": the role of heat shock proteins in the regulation of apoptosis. Journal of Cell Science. 2004;117:2641–2651. doi: 10.1242/jcs.01284. [DOI] [PubMed] [Google Scholar]
- 44.Taipale M, Krykbaeva I, Koeva M, Kayatekin C, Westover KD, Karras GI, et al. Quantitative analysis of hsp90-client interactions reveals principles of substrate recognition. Cell. 2012;150:987–1001. doi: 10.1016/j.cell.2012.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Anders L, Ke N, Hydbring P, Choi YJ, Widlund HR, Chick JM, et al. A Systematic Screen for CDK4/6 Substrates Links FOXM1 Phosphorylation to Senescence Suppression in Cancer Cells. Cancer Cell. 2011;20:620–634. doi: 10.1016/j.ccr.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vredeveld LC, Possik PA, Smit MA, Meissl K, Michaloglou C, Horlings HM, et al. Abrogation of BRAFV600E-induced senescence by PI3K pathway activation contributes to melanomagenesis. Gene Dev. 2012;26:1055–1069. doi: 10.1101/gad.187252.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hallstrom TMKA, Jaamaa S, Monkkonen M, Peltonen K, Andersson LC, Medema RH, et al. Human prostate epithelium lacks Wee1A-mediated DNA damage-induced checkpoint enforcement. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:7211–7216. doi: 10.1073/pnas.0609299104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rajeshkumar NV, De Oliveira E, Ottenhof N, Watters J, Brooks D, Demuth T, et al. MK-1775, a Potent Wee1 Inhibitor, Synergizes with Gemcitabine to Achieve Tumor Regressions, Selectively in p53-Deficient Pancreatic Cancer Xenografts. Clinical Cancer Research. 2011;17:2799–2806. doi: 10.1158/1078-0432.CCR-10-2580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kreahling JM, Gemmer JY, Reed D, Letson D, Bui M, Altiok S. MK1775, a selective Wee1 inhibitor, shows single-agent antitumor activity against sarcoma cells. Molecular Cancer Therapeutics. 2012;11:174–182. doi: 10.1158/1535-7163.MCT-11-0529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kwong LN, Costello JC, Liu H, Jiang S, Helms TL, Langsdorf AE, et al. Oncogenic NRAS signaling differentially regulates survival and proliferation in melanoma. Nature Medicine. 2012 doi: 10.1038/nm.2941. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.