SUMMARY
Humans and other hosts acquire Toxoplasma gondii infection by ingesting tissue cysts in undercooked meat, or by food or drink contaminated with oocysts. Currently, there is no vaccine to prevent clinical disease due this parasite in humans, although, various T. gondii vaccine candidates are being developed. Mice are generally used to test the protective efficacy of vaccines because they are susceptible, reagents are available to measure immune parameters, in mice, and they are easily managed in the laboratory. In the present study, pathogenesis of toxoplasmosis was studied in mice of different strains, including Human leukocyte antigen(HLA) transgenic mice infected with different doses of T. gondii strains of different genotypes derived from several countries. Based on many experiments, the decreasing order of infectivity and pathogenicity of oocysts was: interferon gamma gene knock out (KO), HLA 3.11, HLA 2.1, HLA B7, Swiss Webster, C57/black, and BALB/c. Mice fed as few as 1 oocyst of Type I and several atypical strains died of acute toxoplasmosis within 21 days p.i. Type II, and III strains were less virulent. The model developed herein should prove to be extremely useful for testing vaccines because it is possible to accurately quantitate a challenge inoculum, test response to different strains of T. gondii using the same preparations of oocysts which are stable for up to a year, and to have highly reproducible responses to the infection.
Keywords: Toxoplasma gondii, oocysts, different genotypes, pathogenicity, different mouse strains including interferon gamma knockout and HLA transgenic mice
INTRODUCTION
Toxoplasma gondii infections are widely prevalent in animals and humans worldwide (Dubey 2010). Although most infections by this parasite are without recognized symptoms, it can cause prematurity and severe illness, eye and brain disease in congenitally infected children, and in immune-compromised individuals (Remington et al. 2006). Toxoplasma gondii is the most frequent cause of infections of the back of the eye. Severe cases of toxoplasmosis have been reported in immune-competent patients and some of these are considered to be due to infection with atypical T. gondii genotypes (Ajzenberg et al. 2004; Demar et al. 2007; Elbez-Rubinstein et al. 2009; Grigg and Sundar 2009; Delhaes et al. 2010; Pomares et al. 2011).
Humans and other hosts acquire T. gondii infection by ingesting tissue cysts in undercooked meat, or by food or drink contaminated with oocysts. Mice fed oocysts can die of acute enteritis before lesions develop in extra-intestinal organs (Dubey and Frenkel 1973). Severity of toxoplasmosis depends on many factors including dose, strain of mouse, route of inoculation, and the stage of the parasite. An oral tissue cyst mouse model has been described to study immunity and pathogenesis of orally induced toxoplasmosis (Mc Leod et al. 1984; Mc Leod et al. 1989; Brown et al. 1995; Liesenfeld et al. 1996; Buzoni-Gatel et al. 2001; Johnson et al. 2002; Liesenfeld 2002; Rachinel et al. 2004; Heimesaat et al. 2006; Dunay et al. 2008; Muñoz et al. 2009; Schreiner and Liesenfeld 2009; Dunay and Sibley 2010). After oral inoculation of 100 tissue cysts, C57BL/6 mice died of acute enteritis but BALB/c did not, and the lesions were localized to ileum. However, the number of bradyzoites in tissue cysts varies a great deal and the inoculum is not stable at room temperature. Additionally, the infectivity of free bradyzoites by the oral route in mice is low (Dubey 1997, 2001).
A non-infectious vaccine to prevent clinical disease would be a major advance to minimize suffering due this parasite in humans. Various T. gondii vaccine candidates are being developed (Cong et al. 2010, 2011). Mice are generally used to test the protective efficacy of vaccine, because they are most susceptible, reagents are available to measure immune parameters, and they are easily managed in the laboratory.
Three strains of HLA transgenic mice were used. These mice were selected because they have HLA transgenes that include HLA molecules that recognize peptide epitope supermotifs, that are present in ~90% of the human population (Cong et al. 2010, 2011). These are HLA- 2, HLA-0110 and HLA -B7 mice. Supermotifs are defined by their binding avidity to these HLA molecules with the amino acid in the second and the ninth position of the nonamer peptide critical for anchoring the peptide into the HLA molecule binding pocket (Tan et al. 2010; Cong et al. 2010, 2011).These humanized HLA transgenic mice have been very useful for defining epitopes key for protection against a number of viruses and an apicomplexan parasite, eliciting protective CD8+T cells. They have been useful also in experiments to define T.gondii eptiopes which can confer protection to parenteral challenges with luciferase expressing parasites and elicit gamma interferon from CD8+T cells when administered with adjuvants and the universal CD4T cell helper epitope PADRE (Cong et al. 2010, 2011).
The objective of the present study was to test susceptibility of different strains of mice (especially transgenic) to oral infection with oocysts of T. gondii strains with different genotypes to better understand pathogenesis of the infection by this route. This should provide a robust foundation for testing potential vaccines and new medicines.
MATERIALS AND METHODS
Toxoplasma gondii isolates used
Toxoplasma gondii strains of different genotypes were used. Details of T. gondii isolates used are given in Table 1. Because pathogenicity of T. gondii can be altered by prolonged passage in mice (Dubey 1977), we selected some strains that were recently isolated and not passaged in mice as tachyzoites or tissue cysts. Of the strains listed in Table 1, only VEG and ME49 strains had been maintained as tachyzoites or tissues cysts, before oocysts were obtained. Although, GT1, CT1, and P89 were obtained by one us (Dubey) many years ago these were maintained only as tissue cyst-oocyst stage. Strains isolated in 2004 or later had been passaged in mice to obtain oocysts, and thus represented strains circulating in nature. We also selected strains from Brazil, Colombia, USA, and Asia, because in general T. gondii strains from Brazil are more pathogenic for mice than strains from the USA (Dubey et al. 2002).
Tablel.
Details of Toxoplasma gondii strains used in this study
|
T. gondii strain |
Genotype | Host | Country | Year isolated |
References |
|---|---|---|---|---|---|
| VEG | III | Human | USA | 1989 |
Parmley et al. (1994)
Dubey et al. (1996) |
| TgGoatUS4 | III | Goat | USA | 2009 | Dubey et al. (2011b) |
| ME 49 | II | Sheep | USA | 1958 | Lunde and Jacobs (1983) |
| TgNmBr1 | II | Guinea fowl | Brazil | 2003 | Dubey et al. (2011a) |
| TgGoatUS2 | II | Goat | USA | 2009 | Dubey et al. (2011b) |
| GT- 1 | I | Goat | USA | 1978 | Dubey (1980) |
| CT1 | I | Cattle | USA | 1989 | Dubey (1992) |
| TgBbUS1 | Atypical | Bear | USA | 2009 | Dubey et al. (2010) |
| TgCatBr2 | BrI, atypical | Cat | Brazil | 2003 | Dubey et al. (2004) |
| TgCatBr1 | BrII, atypical | Cat | Brazil | 2003 | Dubey et al. (2004) |
| TgCatBr3 | BrIII, atypical | Cat | Brazil | 2003 | Dubey et al. (2004) |
| TgCatBr5 | Atypical | Cat | Brazil | 2003 | Dubey et al. (2004) |
| TgGoatUS4 | Atypical | Goat | USA | 2009 | Dubey et al. (2011b) |
| TgGoatUS6 | Atypical | Goat | USA | 2009 | Dubey et al. (2011b) |
| TgGoatUS26 | Atypical | Goat | USA | 2010 | Dubey et al. (2011b) |
| TgPigBr3 | Atypical | Pig | Brazil | 2008 | Frazão-Teixeira et al. (2011) |
| TgCkBr233 | Atypical | Chicken | Brazil | 2009 | Dubey et al. (2010) |
| TgCtPRC2 | Atypical | Cat | China | 2006 | Dubey et al. (2007) |
| TgCtPRC3 | Atypical | Cat | China | 2006 | Dubey et al. (2007) |
| TgCtPRC6 | Atypical | Cat | China | 2006 | Dubey et al. (2007) |
| TgGoatUS13 | Atypical | Goat | USA | 2009 | Dubey et al. (2011b) |
| TgPigUs15 (P89) |
Atypical | Pig | USA | 1991 |
Dubey et al. (1995) ;Velmurugan et al. (2009) |
Mouse strains used
Outbred Swiss Webster (SW) and inbred BALB/c were obtained from National Cancer Institute (NCI). Gamma interferon gene knock out (KO) mice (C57BL/6- Ifng) were obtained from Jackson Laboratories (Bar Harbor, ME, USA). HLA A021, HLA A 3.110, and HLA B07 transgenic mice were produced at Pharmexa-Epimmune (San Diego, CA, USA) and bred at the University of Chicago, Taconic (Germantown, New York) and Jackson laboratories (see Cong et al. 2010). All studies were conducted with Institutional Animal Care and Use Committee at the USDA and University of Chicago.
Infection of mice with T. gondii oocysts
Oocysts were obtained by feeding infected tissues of mice to cats, sporulated in 2% sulfuric acid on a shaker for one week, and stored at 4° C until used, but not after 12 months (Dubey 1995, 2010). Most batches of oocysts had not been stored for than 6 months. Oocysts were counted in a disposable haemocytometer and diluted 10-fold from 10−1 to 10−7 to reach an end point of ≅ 1 oocyst. All ten-fold dilutions were made in 50 ml tubes with 2 % sulfuric acid (5 ml aliquot + 45 ml sulfuric acid), and dilutions were stored at 4° C, to avoid variability in inocula preparation. For inoculation of mice, oocysts from the designated dilution were neutralized with 3.3% sodium hydroxide with neutral red as indicator (approximately the same volume as the inoculum). The resultant mixture was inoculated orally into 5 mice for each dilution (unless indicated otherwise) via a gastric needle with a blunt bulb (22 gauge, 50 mm long, Cadence Science catalogue no. 7920), without washing to avoid variability of the inocula during washing procedure. All mice in a given experiment were inoculated at the same time. In most instances, oocysts from the last dilution were also inoculated orally into KO mice, because these mice are highly susceptible to toxoplasmosis and do not survive the infection, irresepective of the strain of T. gondii. All orally inoculated mice were housed in autoclavable rodent cages with biohazard signs to incinerate bedding and food for 10 days to avoid spread of T. gondii because some oocysts pass unexcysted in mouse feces (Dubey and Frenkel 1973).
Bioassay of T. gondii in mice
Mice were observed daily for eight weeks. All mice were examined for T. gondii infection. Impression smears of tissues (usually mesenteric lymph nodes or lungs) were examined microscopically for tachyzoites. Survivors were bled six to eight weeks later and 1:25 dilution of their sera were examined for T. gondii antibodies using the modified agglutination test (MAT) as described (Dubey and Desmonts 1987).The last infective dilution was considered to have 1 viable organism for data presentation. The inoculated mice were considered infected with T. gondii when tachyzoites or tissue cysts were found in tissues. Seroconversion at 6 weeks was considered as indication of the presence of live parasites in the inocula. However, brains of all mice that survived 6 weeks were examined for tissue cysts, irrespective of serological results (Dubey 2010). With the strains of T. gondii used here, tissue cysts are found in all seropositive mice.
Tissue cysts were enumerated in mice that survived 8 weeks p.i. For this, whole mouse brain was homogenized with 1 ml of saline (0.85% NaCl) and tissue cysts were counted microscopically in 50 μl of the homogenate, and the count was multiplied by 20 to obtain the number of tissue cysts per brain. If cysts were not found, another 50 μl was examined in the same manner.
Experimental design
Table 2 summarizes information on T. gondii infections in mice.
Table 2.
Experimental design
|
T. gondii strain |
Genotype | Histology-high doses |
Infectivity and mortality 1 to 100,000 oocysts |
||
|---|---|---|---|---|---|
| Outbred | Inbred | Transgenic | |||
| VEG | III | Detailed | Yes | Yes | Yes |
| TgGoatUS4 | III | No | Yes | No | No |
| ME 49 | II | Detailed | Yes | Yes | Yes |
| TgNmBrl | II | Detailed | Yes | Yes | Yes |
| TgGoatUS2 | II | No | Yes | No | No |
| GT- 1 | I | Detailed | Yes | Yes | Yes |
| CT1 | I | Limited | Yes | Yes | Yes |
| TgBbUS1 | Atypical | Limited | Yes | Yes | Yes |
| TgCatBr2 | BrI, atypical | No | Yes | Yes | Yes |
| TgCatBr1 | BrII, atypical | Detailed | Yes | Yes | Yes |
| TgCatBr3 | BrIII, atypical | Detailed | Yes | Yes | Yes |
| TgCatBr5 | Atypical | No | Yes | Yes | Yes |
| TgGoatUS4 | Atypical | No | Yes | Yes | Yes |
| TgGoatUS6 | Atypical | Limited | Yes | No | No |
| TgGoatUS26 | Atypical | Limited | Yes | No | No |
| TgPigBr3 | Atypical | Detailed | Yes | Yes | Yes |
| TgCkBr233 | Atypical | Detailed | Yes | No | No |
| TgCtPRC2 | Atypical | Limited | Yes | Yes | Yes |
| TgCtPRC3 | Atypical | Limited | Yes | Yes | Yes |
| TgCtPRC6 | Atypical | Limited | Yes | Yes | Yes |
| TgGoatUS13 | Atypical | Limited | Yes | No | No |
| TgPigUs15 (P89) |
Atypical | No | Yes | Yes | Yes |
Pathogenesis of acute toxoplasmosis in mice
Histogenesis of lesions and parasitism in mice orally inoculated with oocysts was studied herein using different strains of T. gondii, and different strains of mice (Table 3). Most mice were inoculated orally using 100,000 or more oocysts. The primary objective was to document the development of early lesions, particularly in the small intestine. As mentioned in introduction, after oral inoculation of 100 tissue cysts, C57BL/6 mice died of acute enteritis but BALB/c did not, and the lesions were localized to ileum. However, it is not known if early lesions developed in other parts of small intestine of C57BL/6 mice after feeding approximately 100 tissues cysts that might contain 100,000 bradyzoites. Actually, early lesions were not seen in SW mice inoculated orally with millions of T. gondii bradyzoites (Dubey 1997). Therefore, an unusually high dose of oocysts was selected to study early events in small intestine.
Table 3.
Histological study of mouse tissues fed large doses of Toxoplasma gondii.oocysts.
|
T. gondii strain |
Genetic type |
Strain of mouse | Times euthanized |
|---|---|---|---|
| VEG | III | BALB/c | |
| HLA-311 | 6 hours, 1, 2, 3, 4, 5 days | ||
| SW | |||
| TgGoatUS4 | III | SW | 4,8 days |
| TgNmBrl | II | SW | 1, 2, 3, 4, 5 days |
| ME49 | II | BALB/c | 6 hours, 1, 2, 3, 4, 5, 6, 7, 8, 9,10 days |
| SW | 6 hours, 1, 2, 3, 4, 5, 6 days | ||
| KO | 6 hours, 1, 2, 3, 4, 5 days | ||
| HLA-311 | 5,6 days | ||
| HLA 2.1 | 6 hours, 1, 2, 3, 4, 5, 6, 7 days | ||
| GT-1 | I | SW | 7 days, 8 days |
| HLA-B7HBM | 1, 2, 3, 4, 5, 6, 7, 8, 13 days | ||
| HLA 311 | 6 hours, 1, 2, 3, 4, 5 days | ||
| HLA 21 | 1, 2, 3, 4, 5 days | ||
| BALB/c | 6 hours, 1, 2, 3, 4, 5, 6, 7 days | ||
| CT1 | I | SW | 5 days |
| TgBrUsl | Atypical | SW | 7 days |
| TgCkBr233 | Atypical | SW | 3, 4, 5,, 6, 10 days |
| TgCatBrl | Atypical | SW | 5, 6 , 7, 8, 9, 12, 14 days |
| TgCatBr3 | Atypical | SW | 6 hours, 1, 2, 3, 4, 5, 6, 7, 8 days |
| TgPigUS15 | Atypical | HLA311 | 5 days |
| TgCtPRC2 | Atypical | HLA311 | 5 days |
| TgCtPRC3 | Atypical | HLA311 | 5 days |
| TgCtPRC6 | Atypical | HLA311 | 5 days |
| TgGoatUS13 | Atypical | HLA311 | 5 days |
| TgGoatUS6 | Atypical | SW | 4,7 days |
| TgGoatUS26 | Atypical | SW | 4 days |
In the present study, detailed observations were made using 3 strains of T. gondii (VEG, Type III, ME49, Type II, and GT1, Type I), in SW, BALB/c, and transgenic mice (Table 4). Additionally, data on 14 other strains of T. gondii were added to show the pattern of lesion; not all time points were examined for each strain of T. gondii in each strain of mouse. Subsequently, data on transgenic mice (HLAA.311, HLA B7) orally inoculated with 1-100 oocysts were added (Table 4). Mice were euthanized starting 6 h post inoculation (p.i.) and up to 14 days p.i.. The entire intestine was studied histologically. For this, the small intestine (approximately 25 cm) was stretched on a paper towel, and divided into five equal portions (nos. 1-5). The large intestine constituted the sixth segment (Table 3). Samples from the remaining organs, including the mesenteric lymph nodes, spleen, liver, lungs, heart, pancreas, skeletal muscle, tongue, uterus, and eyes were fixed in 10% buffered formalin along with intestines. One day later, 3 mm thick sections were processed for paraffin embedding. The intestines were embedded on end, like a tube. Virtually all portions of intestines were processed for histology. Paraffin-imbedded sections were cut at 5 μm thickness, and examined microscopically after staining with hematoxylin and eosin (HE). Immunohistochemistry for T. gondii was performed on paraffin-embedded sections using reagents and methods described previously (Dubey 2010). Lesions and T. gondii tachyzoites were graded in mice euthanized 1-14 days p.i.
Table 4.
Histopathology of lesions of acute toxoplasmosis in BALB/c mice fed oocysts
|
T. gondii strain |
Hrs pi. |
Intestinal segmentsa | M.Lf | Other tissuesg | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | ||||
| VEG | 6 | +b | + | + | + | + | -e | + | - |
| 24 | + | + | + | + | + | - | + | - | |
| 48 | + | + | + | + | + | - | ++ | - | |
| 72 | + | + | +++d | +++ | +++ | + | +++ | Sp | |
| 96 | + | ++c | ++ | +++ | +++ | + | +++ | Sp | |
| ME 49 | 6 | + | + | + | + | + | - | - | - |
| 24 | + | + | + | + | + | - | + | - | |
| 72 | - | + | + | + | ++ | - | + | - | |
| 96 | - | - | ++ | ++ | ++ | - | ++ | Sp | |
| 120 | + | ++ | +++ | +++ | +++ | + | +++ | Sp | |
| 120 | - | + | ++ | +++ | +++ | ++ | +++ | Lu | |
| 144 | + | + | ++ | +++ | +++ | ++ | +++ | K, Li, Lu,Sp | |
| 168 | + | + | + | ++ | +++ | ++ | +++ | B.K,Li.Lu,Sp | |
| 192 | + | + | + | ++ | +++ | ++ | +++ | B,H,K,Li,Lu,M,Sp,T | |
| 216 | + | + | + | ++ | +++ | ++ | +++ | B,H,K,Li,Lu,M,Sp,T | |
| 240 | + | + | ++ | ++ | ++ | + | +++ | B,H,K,Li,Lu,M,Sp,T | |
| GT-1 | 6 | + | + | + | + | - | - | - | |
| 24 | + | + | + | + | + | - | + | - | |
| 48 | + | + | + | + | ++ | - | + | - | |
| 72 | + | + | + | ++ | +++ | - | ++ | - | |
| 96 | + | ++ | +++ | +++ | +++ | - | +++ | Sp | |
| 120 | + | ++ | +++ | +++ | +++ | - | +++ | Sp | |
| 144 | + | ++ | +++ | +++ | +++ | - | +++ | Li, Lu, Sp, St | |
| 168 | + | ++ | +++ | +++ | +++ | - | +++ | B, H, Li, Lu, Sp | |
=T. gondii not seen ,no lesion. 1-5, small intestine, 6-large intestine.
=+ Few T.gondii, no lesion,c=
=++ = T.gondii, few lesions.
d=+++ = Nearly all villi affected or severe lesions.
= no lesions, no T. gondii.
=M.L.= mesenteric lymph nodes
=B=brain, E= eye, H= heart, K=kidneys, Li=liver, Lu=lungs, , M=skeletal muscle, Sp=spleen, St=stomach,T=tongue,
Enumeration of T. gondii tachyzoites in ileum of acutely infected mice
Results of the experiment in Table 4 indicated that the terminal part of the ileum is the most heavily affected portion of the small intestine. Inorder to find whether the parasite multiplication could account for intestinal lesions, HLA 3.11 mice were orally inoculated with graded doses of oocysts of the GT1 strain, which is lethal for mice. For this, 2-3 mice (Tables 6) were euthanized 1-10 days p.i. and their ileum (terminal 10 cm) were weighed, homogenized in blender in 50 ml of saline at full speed for about 1 min, filtered through gauze (suspension A), centrifuged for 10 min at 2000 rpm (1400xg), and the supernatant discarded. The sediment was suspended in 5 ml of antibiotic saline, and this homogenate was considered 10−1 dilution (suspension B). Tachyzoites were counted in 50 μl of the 10−1 dilution in a haemocytometer. Further, 10-fold dilutions were made of the homogenate until an end point was achieved. Aliquots from different dilutions were bioassayed by subcutaneous inoculation in to 5 SW mice; bioassay data were used if the tachyzoites were not detected by microscopic examination. Data from HLA 2.1, and BALB/c mice euthanized on days 4-8 were added to supplement evidence obtained with HLA 3.211 mice (Table 6).
Table 6.
Density of Toxoplasma gondii in ileum of mice fed GT1 oocysts.
| Days pi |
Mouse strain | ||
|---|---|---|---|
| HLA 3.11 | HLA 2.1 | BALB/c | |
| 1 | 1 x103a | ND | ND |
| 2 | 1 x105a | ND | ND |
| 3 | 1.5 x107b | ND | ND |
| 4 | 1.0 x107 | ND | 1.25x107 |
| 5 | 1.0 x107 | ND | ND |
| 6 | 2.5 x107 | 3.1 x107 | ND |
| 7 | 5.0 x106 | 5.0 x106 | ND |
| 8 | 1.0 x106 | ND | 9.0 x106 |
| 9 | 1.0 x106 | ND | ND |
| 10 | 5x105 | ND | 4.5x106 |
By bioassay.
Counted.
Nd-no data.
To further study colonization of ileum by tachyzoites after feeding oocysts, 27 HLA 2.1 (Table 7) mice were orally inoculated with 3 strains of T. gondii (genotype I, II, III) and 3 mice (for each T. gondii strain) were euthanized on days 3,4, and 5, and parasites enumerated as in Table 6.
Table 7. Concentration of Toxoplasma gondii tachyzoites in ileum of HLA 2.1 mice fed three genetic Types (III,II,I) strains of oocystsa
| Day | T. gondii strain | ||
|---|---|---|---|
| p.i. | VEG | ME49 | GT1 |
| 3 | 1x107 | 4x106 | 4x106 |
| 4 | 1x107 | 1.1 x107 | 1.5 x107 |
| 5 | 4x107 | 1.5x107 | 4.25x107 |
Ten cm ileum of two mice from each group were homogenized with 50 ml saline (suspension A), centrifuged, and sediment suspended in 5 ml saline (suspension B). Organisms counted in suspension A (ileum) or suspension B.
RESULTS
Pathogenicity of different T. gondii strains in various strains of mice
Based on a 100% lethal dose, data are summarized in Table 8. The Type I strains (GT1, CT1) and six atypical strains (TgBbUs1,TgCatBr1, TgCatBr3 TgCatBr5,TgPigUS15,TgCtPr6) were lethal for all mice, irrespective of the strain and the dose; mice that received the last dilution, calculated to have no oocysts, remained healthy, did not develop antibody to T. gondii, and had no demonstrable T. gondii in their tissues. Not all atypical T. gondii strains were lethal for mice, irrespective of their country of origin. For example, the TgCatBr3 was only mildly pathogenic, whereas TgCatBr1 was highly virulent; both of these isolates are from cats from Brazil. TgBbUs1, an atypical strain from a bear from Alaska, USA, was the most virulent, irrespective of the strain of mouse.
Table 8.
Lethal dose (100%) of oocysts of various Toxoplasma gondii strains in different strains of mice *
|
T. gondii strain |
Type | SW | BALB/c | HLA | ||
|---|---|---|---|---|---|---|
| 3.11 | 2.1 | B7 | ||||
| VEG | III | 100- 1000 |
100- 1000 |
100 | 100 | 100 |
| TgGoatUS4 | III | 1000 | Not done |
100 | 100 | 100 |
| ME 49 | II | 100- 1000 |
100- 1000 |
100 | 100 | 100 |
| TgNmBr1 | II | 1000 | 1000 | 10-100 | 10-100 | 10-100 |
| CT1 | I | 1 | 1 | 1 | 1 | 1 |
| GT-1 | I | 1 | 1 | 1 | 1 | 1 |
| TgBbUs1 | Atypical | 1 | 1 | 1 | 1 | 1 |
| TgCatBr1 | Atypical, BrII | 1 | 1 | 1 | 1 | 1 |
| TgCatBr2 | Atypical, BrI | 1 | 1 | 1 | 1 | 1 |
| TgCatBr3 | Atypical, BrIII | 1000 | 10000 | 100-1000 | 100-1000 | 100-1000 |
| TgPigUS15 (P89) | Atypical | 1 | 1 | 1 | 1 | 1 |
| TgCt PRC2 | Atypical | 1 | 1 | 1 | 1 | 1 |
| TgCt PRC3 | Atypical | 1 | 1 | 1 | 1 | 1 |
| TgCt PRC6 | Atypical | 1 | 1 | 1 | 1 | 1 |
| TgCatBr5 | Atypical | 1 | 1 | 1 | 1 | 1 |
Five mice per group.
Histogenesis of lesions
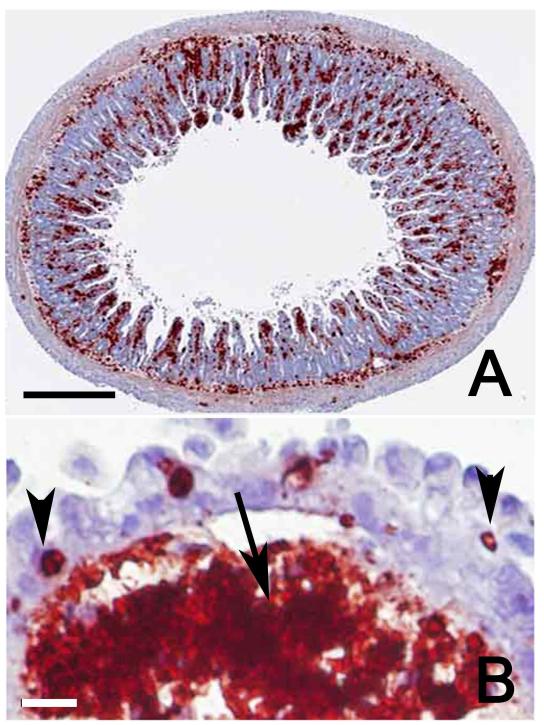
The pattern of lesions and tissue parasitisation were same, irrespective of the strain of mouse or T. gondii. An example of lesions seen in BALB/c mice after feeding VEG (Type III), ME 49 (Type II), and the GT1 (Type I) is shown in Table 5; this strain of mouse was chosen here because it is considered resistant to clinical toxoplasmosis, based on feeding 100 tissue cysts. Mice fed approximately 100,000 or more oocysts died of acute toxoplasmosis within 6 days. The last 2/5 of the small intestine was the most parasitised tissue. The extent of lesions in intestine varied with dose and the strain of T. gondii, lesions were most severe in the last 10 cm of the ileum. After feeding oocysts, T.gondii parasites were seen in histological sections of the entire small intestine, but initial multiplication was the highest in the ileum and the mesenteric lymph nodes. Mice that died day 4 after feeding oocysts did so because of severe transmural enteritis, particularly of the ileum (Fig.1). Tachyzoites multiplied in most cells in the lamina propria causing parenchymal necrosis (Fig 1B); many times the surface enterocytes were minimally affected (Fig 1B). Death was precipitated by sloughing of the contents of small intestine in to the lumen. Subsequently lesions and tachyzoites were seen in other regions of small intestine and also in the cecum and rectum, however, at any given time the ileum was most parasitized among five regions of small intestine (Table 4).Immunohistologically, tachyzoites were seen in descending order of density in intestine, mesenteric lymph nodes, spleen, lungs of mice examined 6 days p.i. Subsequently, tachyzoites were seen in the liver, heart, and brain. Mice that died of acute toxoplasmosis during the first week after infection did so because of enteritis and mesenteric lymph node necrosis. During the second and the third week p.i., mice died primarily of acute interstitial pneumonitis, with demonstrable tachyzoites.
Table 5.
Histogenesis of lesions of acute toxoplasmosis in transgenic mice fed few ME 49 (Type II) or TgGoatUS26(Atypical) oocysts
| Dose | Mouse strain |
T.gondii strain |
Day p.i. |
Intestinal segmentsa | M.Lb | Othersg | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | ||||||
| 100 | A.3.11 | ME 49 | 3 | -c | - | - | - | - | - | - | - |
| 100 | A.3.11 | ME 49 | 4 | +d | - | - | - | + | - | + | - |
| 100 | A.3.11 | ME 49 | 5 | + | + | + | + | ++e | - | ++ | Sp |
| 100 | A.3.11 | ME 49 | 6 | + | + | + | + | ++ | + | +++ | H, Li, Lu, Sp |
| 100 | A.3.11 | ME 49 | 7 | + | + | + | ++ | +++f | + | +++ | H, Li, Lu, P, Sp |
| 100 | A.3.11 | ME 49 | 9 | + | + | + | ++ | +++ | + | ++ | B, H, K, Li, Lu, Sp, T |
| 100 | A.3.11 | ME 49 | 10 | + | + | + | ++ | +++ | ++ | ++ | A, B, H, K, Li, Lu, Sp, T |
| 100 | B7 | ME 49 | 8 | + | ++ | ++ | ++ | +++ | ++ | ++ | B, H, K, Li, Lu, Sp, T |
| 100 | B7 | ME 49 | 10 | + | + | + | ++ | ++ | + | ++ | B, H, K, Li, Lu, M, P, , Sp, T,U |
| 1 | B7 | ME 49 | 12 | + | + | + | ++ | ++ | + | ++ | B,H,K, Li, Lu, M |
| 100 | A.3.11 | TgGoatUS26 | 6 | + | + | + | ++ | +++ | + | +++ | H, Li, Lu, Sp |
| 10 | A.3.11 | TgGoatUS26 | 7 | + | + | + | ++ | +++ | + | +++ | B, K ,Li, Lu, Sp, St |
| 1 | A.3.11 | TgGoatUS26 | 10 | + | + | + | + | ++ | - | ++ | B, H, K, Li, Lu, T |
| 1 | A.3.11 | TgGoatUS26 | 11 | - | + | + | + | + | - | ++ | A, K, Lu, Sp, U |
1-5. small intestine. 6-large intestine.'
Mesenteric lymph nodes.,
no lesions, no T. gondii.
Few T.gondii, no lesion..
Nearly all villi affected or severe lesions.
B=brain, E= eye, H= heart, K=kidneys, Li=liver, Lu=lungs, , M=skeletal muscle, P=Pancreas, Sp=spleen,St=stomach, T=tongue, U=uterus
Figure 1.
Section of ileum of a Swiss Webster mouse, 96 hr after feeding VEG strain oocysts. Note extensive parasitisation of the lamina propria. All red stained bodies are tachyzoites. Immunohistochemical staining with rabbit T. gondii polyclonal antibodies. A. Low magnification showing cross section. Bar=250 μm. B. Higher magnification of a villus showing numerous tachyzoites and spilled antigen (arrow) in the lamina propria. A few tachyzoites (arrow heads) are present in enterocytes but the surface epithelium is intact. Bar=25 μm.
Similar pattern of lesions observed with high dose of oocysts was seen in transgenic mice (A.3.11, B7) after feeding low dose (1-100) of oocysts (Table 5). Mice fed 100 oocysts were ill 5-6 days p.i.; T. gondii was not detectable in histological sections of the mouse killed 3 day p.i., and only few parasites were seen on day 4 p.i. Tachyzoites first multiplied in small intestine and ileum was the most parasitised tissue.
Density of T. gondii in ileum of mice fed large doses of oocysts
Parasitaemia was detected in mice euthanized 6 hr pi by bioassay of blood removed from the orbital sinus (data not shown). By 3 day p.i. more than 10 million T. gondii were present in 10 cm of ileum (Table 6). The results were similar, irrespective of the strain of mouse or T. gondii genetic type (Table 7).
Mortality pattern and the number of tissue cysts in mice infected with different T. gondii strains
Examples of mortality rates are shown in Tables 9-11. With GT1 (Type I) strain, all inoculated mice died within 13 days p.i., irrespective of the dose and the mouse strain (Table 9).
Table 9.
Toxoplasma gondii GT1 strain (Type I) oocyst infectivity to various mouse strains
| Dose | Swiss Webster* |
BALB/c | HLA-3.11 | HLA-B 7 | HLA-A.21 |
|---|---|---|---|---|---|
| 10 6 | 5/5(6) | 5/5(4-5) | 5/5(5) | 5/5(4-6) | 5/5(4) |
| 10 5 | 5/5(7) | 5/5(6-7) | 5/5(6) | 5/5(6) | 5/5(5) |
| 10 4 | 5/5(9) | 5/5(-10) | 5/5(7-7) | 5/5(7-8) | 5/5(7) |
| 10 3 | 5/5(9) | 5/5(9-10) | 5/5 (7-8) | 5/5(8-10) | 5/5 (7-8) |
| 10 2 | 5/5(10-14) | 5/5(10-13) | 5/5 (7-9) | 5(9-10) | 5/5 (6) |
| 10 | 1/1(11) | 2/2(9,15) | 5/5 (10-11) | 5(10) | 5/5 (9) |
| 1 | 0/0 | 0/0 | 2/2 (11,13) | 1(11) | 2/2 (11,13) |
Five mice per group. First figure is no. of mice infected with T. gondii. Second figure is no. of mice dead.Figure in parenthesis is day of death.
Table 11.
Infectivity of low numbers of Type III (VEG, TgGoatUS4) and Type II (ME 49, TgNmBrl) strains of Toxoplasma gondii oocyst to mice
|
T. gondii strain (Type) |
Dose | No. of mice |
Mouse strains | ||||||
|---|---|---|---|---|---|---|---|---|---|
| SW | KO | HLA 3.11 |
HLA 2.1 |
HLA B7 |
C57/ Black |
BALB/c | |||
| ME 49 (II) |
100 | 25 | 25/0 (618)a |
25/25 NA |
25/25 NA |
25/21 (304) |
25/18 (128) |
23/2 (236) |
23/1 (126) |
| TgNmBr1 TypeII |
1000 | 10 | 10/0 (526) |
10/10 NA |
10/2 (785) |
10/1 (686) |
10/0 (300) |
10/0 (526) |
ND |
| TgGoatUS4 (Atypical) |
1000 | 10 | 10/1 (457) |
10/10 NA |
10/10 NA |
10/10 NA |
10/0 (364) |
9/0 (50) |
ND |
=No. of mice T. gondii infected/no. died (average no. of tissue cysts)
ND=not done, NA=not applicable, mice died.
With a relatively non-virulent atypical Brazilian strain (TgCatBr3), decreasing order of virulence were KO, HLA 3.11, SW, and BALB/c (Table 10). It is noteworthy that all KO mice fed infective dose of oocysts died within 14 days p.i. Among the mice that survived, least numbers of tissue cysts were found in BALB/c mice (Table 10).
Table 10.
TgCatBr3 (atypical) oocyst infectivity to various mouse strains.
| Dose | Swiss Webster |
BALB/c | HLA3.11 | KO MICE |
|---|---|---|---|---|
| 105 | 5/5(5-6)* | 5/5(7-11) | 5/5(6-7) | Not done |
| 104 | 5/5(7-9) | 5/5(8-20) | 5/5(7) | Not done |
| 103 | 5/2(17,18,660 -1200; 960) |
5/1(24,40- 280;170) |
5/5(10-15) | Not done |
| 102 | 5/0(860- ,1120; 1044) |
5/0(80-280; 184) |
5/4 (18-20,500) | Not done |
| 10 | 3/0(260-460; 386) |
3/0 (40-240; 120) |
5/1(19,20-220; 120) |
5/5(12-14) |
| 1 | 1/0(1200) | 0/0 | 0/0 | 0/0 |
| <1 | 0/0 | 0/0 | 0/0 | 0/0 |
Five mice per group. First figure is no. of mice infected with T. gondii. Second figure is no. of mice dead. Figure in parenthesis is day of death. Figures in bold are number of tissue cysts, range; and average per infected mouse.
In the previous experiments, 5 mice were inoculated per dose. In another experiment, 10-25 mice were inoculated using 100-1000 infective oocysts of 3 strains of T. gondii (Table 11). The infectivity of the dose was determined previously by bioassays in mice, including KO mice. Mortality and the number of oocysts are shown in Table 11. With the ME 49 strain, oocysts were most pathogenic to KO, HLA3.11, HLA 2.1, Hla B7, C57/black, BALB/c, and SW—in decreasing order of pathogenicity, the number of tissue cysts were lowest in BALB/c mice.Similar trend was with other strains of T. gondii, although not all strains were used to infect large numbers of mice.
DISCUSSION
The early events in the mouse intestine after feeding oocysts initially described in out-bred Swiss Webster mice orally inoculated with VEG strain (Dubey et al. 1997; Speer and Dubey 1998) were confirmed here using different strains of mice and T. gondii strains of different genotypes. These events are important biologically because ingestion of oocysts is a major route of transmission in animals and humans. After ingestion of oocysts, T. gondii sporozoites excyst in small intestine, and can invade entrocytes as early as 30 min p.i. (Dubey et al. 1997). Sporozoites are carried to the lamina propria by an undefined mechanism, but not by intraepithelial cells (Speer and Dubey 1998). The isolation of viable organisms as early as 4 h p.i. (Dubey et al. 1997) and 6 h (present study) from the peripheral blood of mice fed oocysts indicates that sporozoites circulate in the body early in infection but initial multiplication occurs in the mesenteric lymph nodes and the intestinal lamina propria. Toxoplasma gondii multiplies in all cell types (except red blood cells) of the lamina propria and secondarily invade surface enterocytes (Speer and Dubey 1998). Although sporozoites can excyst throughout the small intestine, they preferentially invade distal part of small intestine (Dubey et al. 1997). Similar pattern of infection was found in the present study using at least 2 other strains of T. gondii and other strains of mice. Mice died early after infection with sporozoites in association with massive infection of the intestine with intestinal necrosis. This was most prominent in the terminal ileum. The exact cause of this acute enteritis was not the focus of this research but finding of as many as 10 million tachyzoites in 10 cm (< 1g) of the terminal ileum indicates that the parasite-induced cell death is important in the oocyst model. Interferon gamma conferred some protection as seen by the greater susceptibility of the interferon gamma knock out versus the wild type BALB/c mice. Enteritis associated with an immune response to SAG 1 was described in C57/BL mice fed tissues cysts (Rachinel et al. 2004). It is of interest that the HLA transgenic mice were more susceptible than the parental C57Bl6/J and BALB/c strains but the mechanisms are not known. Whether and if so how often T. gondii infections might cause gastrointestinal symptoms in humans is unknown. Historically, enteritis was not recognized as cause of death in experimentally infected mice until the discovery of the resistant stage of T. gondii, the oocyst in late 1960. Mice fed cat feces (containing oocysts) died within 8 days p.i. but diagnosis was difficult because intestines were not examined (Hutchison et al. 1968). Subsequently, it was found that the cause of death in mice fed large numbers of oocysts was enteritis (Frenkel et al. 1970; Dubey and Frenkel 1973; Dubey et al. 1997). Initially, these studies were performed in out-bred albino mice, and now extended to inbred and transgenic mice.
Our data demonstrate that, at least in mice, T. gondii infection can cause severe and lethal enteritis, irrespective of the genetic background. In animals, oocyst-induced infections are more severe than tissue cyst acquired infections (Dubey 2010). Schreiner and Liesenfeld (2009) reviewed reports of toxoplasmosis in many species of animals and concluded that orally induced infections can cause severe immunopathology in gut and other viscera. Whether there is a parallel disease in humans remains to be determined. Lymphadenopathy in nodes draining the terminal ileum has been confused with appendicitis, but whether there was such severe enteritis in any humans is unknown.
In the present study in mice fed high doses of oocysts, necrosis and hyperinfection of terminal ileum seems to a pathogenic hallmark of these infections for unknown reasons. Whether there is a receptor or type of cell there that causes this localization is unknown. Further, the progression of enteritis associated with early deaths there and later deaths due to pneumonia occur whether the infection is with 100 or 100,000 oocysts; parasite multiplication is responsible for atleat in part as cause of death because numerous tachyzoites can be demonstrated in smears made from intestines and lungs. Since an acutely infected cat can excrete up to 500 million oocysts in a period of few days it does not seem unreasonable to consider whether an incidental host like a mouse or human might encounter 100 or even 100,000 oocysts. Whether this happens in nature is unknown. It is of interest that more than 70 % of the mothers of children in the National Collaborative Congenital Toxoplasmosis Study in USA have antibody to oocysts (Hill et al. 2011; Boyer et al. 2011), and the source of exposure is unknown for many. Most of these mothers did not have recognized symptoms and most of the infants had moderate or severe signs of infection. Epidemics of toxoplasmosis have been linked epidemiologically to ingestion of oocysts from the environment (see Hill et al. 2011).
It is noteworthy that the introduction of the transgenes increases the susceptibility of the mice. This is reminiscent of the increased susceptibility seen in other transgenic mice earlier (Brown and McLeod 1990). Possible mechanisms are competing MHC molecules from the human transgene diminishing the response of the murine MHC which confers some protection (Brown et al., 1994, 1995; Mack et al. 1999; McLeod et al. 1989, 1993; Johnson et al. 2002a,b; Jamieson et al. 2008,2010; Lees et al., 2010; Witola et al. 2011).Alternatively the human MHC could introduce a harmful/lethal immune response because it is robust but damaging.
The data herein demonstrate that host and parasite genes interact in profoundly important and unpredictable ways in these murine models. As shown in Table 8, not all type 2 or type 1 or 3 lineage parasites behave in the same manner in these models. More than one parasite allele must be critical. Variation among alleles/epitopes in parasites of differing and the same lineages have been noted in the past.
The model developed herein should prove to be extremely useful for testing vaccines because it is possible to very accurately quantitate a consistent challenge inoculum, test response to different strains of T.gondii using the same preparations of oocysts which are stable for up to a year, and to have a very reproducible response to the infection. This should be a robust model for testing vaccine preparations in these HLA transgenic mice. This model is relevant to the human infection since CD8 T cells are protective against this infection.
ACKNOWLEDGEMENTS
This work was supported by NIAID U01AI077887 (RM, JPD) and the Dominique Cornwell and Mann Family Foundation.
REFERENCES
- Ajzenberg D, Bañuls AL, Su C, Dumètre A, Demar M, Carme B, Dardé ML. Genetic diversity, clonality and sexuality in Toxoplasma gondii. International Journal for Parasitology. 2004;34:1185–1196. doi: 10.1016/j.ijpara.2004.06.007. [DOI] [PubMed] [Google Scholar]
- Boyer K, Hill D, Mui E, Wroblewski K, Karrison, Dubey JP, Sautter M, Noble G, Withers S, Swisher CN, Heydemann PT, Hosten T, Babiarz J, Lee, McLeod R. Unrecognized ingestion of Toxoplasma gondii oocysts causes congenital toxoplasmosis and epidemics in North America. Clinical Infectious Diseases. 2011 doi: 10.1093/cid/cir667. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CR, McLeod R. Class I MHC genes and CD8+ T cells determine cyst number in Toxoplasma gondii infection. Journal of Immunology. 1990;145:3438–3441. [PubMed] [Google Scholar]
- Brown CR, David CS, Khare SJ, McLeod R. Effects of human class I transgenes on Toxoplasma gondii cyst formation. Journal of Immunology. 1994;152:4537–4541. [PubMed] [Google Scholar]
- Brown CR, Hunter CA, Estes RG, Beckmann E, Forman J, David C, Remington JS, McLeod R. Definitive identification of a gene that confers resistance against Toxoplasma cyst burden and encephalitis. Immunology. 1995;85:419–428. [PMC free article] [PubMed] [Google Scholar]
- Buzoni-Gatel D, Debbabi H, Mennechet FJD, Martin V, Lepage AC, Schwartzman JD, Kasper LH. Murine ileitis after intracellular parasite infection is controlled by producing intraepithelial lymphocytes. Gastroenterology. 2001;120:914–924. doi: 10.1053/gast.2001.22432a. [DOI] [PubMed] [Google Scholar]
- Cong H, Mui EJ, Witola WH, Sidney J, Alexander J, Sette A, Maewal A, McLeod R. Human immunome, bioinformatic analyses using HLA supermotifs and the parasite genome, binding assays, studies of human T cell responses, and immunization of HLA-A*1101 transgenic mice including novel adjuvants provide a foundation for HLA-A03 restricted CD8+T cell epitope based, adjuvanted vaccine protective against Toxoplasma gondii. Immunome Research. 2010;6 doi: 10.1186/1745-7580-6-12. doi: 10.1186/1745-7580-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cong H, Mui EJ, Witola WH, Sidney J, Alexander J, Sette A, Maewal A, McLeod R. Towards an immunosense vaccine to prevent toxoplasmosis: protective Toxoplasma gondii epitopes restricted by HLA-A*0201. Vaccine. 2011;29:754–762. doi: 10.1016/j.vaccine.2010.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delhaes L, Ajzenberg D, Sicot B, Bourgeot P, Dardé ML, Dei-Cas E, Houfflin-Debarge V. Severe congenital toxoplasmosis due to a Toxoplasma gondii strain with an atypical genotype: case report and review. Prenatal Diagnosis. 2010;30:902–905. doi: 10.1002/pd.2563. [DOI] [PubMed] [Google Scholar]
- Demar M, Ajzenberg D, Maubon D, Djossou F, Panchoe D, Punwasi W, Valery N, Peneau C, Daigre JL, Aznar C, Cottrelle B, Terzan L, Dardé ML, Carme B. Fatal outbreak of human toxoplasmosis along the Maroni River: epidemiological, clinical, and parasitological aspects. Clinical Infectious Diseases. 2007;45:e88–e95. doi: 10.1086/521246. [DOI] [PubMed] [Google Scholar]
- Dubey JP. Toxoplasma, Hammondia, Besnoitia, Sarcocystis, and other tissue cyst-forming coccidia of man and animals. In: Kreier JP, editor. Parasitic Protozoa. Vol. 3. Academic Press; New York: 1977. pp. 101–237. [Google Scholar]
- Dubey JP. Mouse pathogenicity of Toxoplasma gondii isolated from a goat. American Journal of Veterinary Research. 1980;41:427–429. [PubMed] [Google Scholar]
- Dubey JP. Isolation of Toxoplasma gondii from a naturally infected beef cow. Journal of Parasitology. 1992;78:151–153. [PubMed] [Google Scholar]
- Dubey JP. Duration of immunity to shedding of Toxoplasma gondii oocysts by cats. Journal of Parasitology. 1995;81:410–415. [PubMed] [Google Scholar]
- Dubey JP. Bradyzoite-induced murine toxoplasmosis: stage conversion, pathogenesis, and tissue cyst formation in mice fed bradyzoites of different strains of Toxoplasma gondii. Journal of Eukaryotic Microbiology. 1997;44:592–602. doi: 10.1111/j.1550-7408.1997.tb05965.x. [DOI] [PubMed] [Google Scholar]
- Dubey JP. Oocyst shedding by cats fed isolated bradyzoites and comparison of infectivity of bradyzoites of the VEG strain Toxoplasma gondii to cats and mice. Journal of Parasitology. 2001;87:215–219. doi: 10.1645/0022-3395(2001)087[0215:OSBCFI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Dubey JP. Toxoplasmosis of Animals and Humans. Second Edition CRC Press; Boca Raton. Florida: 2010. p. 313p. [Google Scholar]
- Dubey JP, Desmonts G. Serological responses of equids fed Toxoplasma gondii oocysts. Equine Veterinary Journal. 1987;19:337–339. doi: 10.1111/j.2042-3306.1987.tb01426.x. [DOI] [PubMed] [Google Scholar]
- Dubey JP, Frenkel JK. Experimental Toxoplasma infection in mice with strains producing oocysts. Journal of Parasitology. 1973;59:505–512. [PubMed] [Google Scholar]
- Dubey JP, Graham DH, Blackston CR, Lehmann T, Gennari SM, Ragozo AMA, Nishi SM, Shen SK, Kwok OCH, Hill DE, Thulliez P. Biological and genetic characterisation of Toxoplasma gondii isolates from chickens (Gallus domesticus) from São Paulo, Brazil: Unexpected findings. International Journal for Parasitology. 2002;32:99–105. doi: 10.1016/s0020-7519(01)00364-2. [DOI] [PubMed] [Google Scholar]
- Dubey JP, Lunney JK, Shen SK, Kwok OCH, Ashford DA, Thulliez P. Infectivity of low numbers of Toxoplasma gondii oocysts to pigs. Journal of Parasitology. 1996;82:438–443. [PubMed] [Google Scholar]
- Dubey JP, Navarro IT, Sreekumar C, Dahl E, Freire RL, Kawabata HH, Vianna MCB, Kwok OCH, Shen SK, Thulliez P, Lehmann T. Toxoplasma gondii infections in cats from Paraná, Brazil: seroprevalence, tissue distribution, and biologic and genetic characterization of isolates. Journal of Parasitology. 2004;90:721–726. doi: 10.1645/GE-382R. [DOI] [PubMed] [Google Scholar]
- Dubey JP, Passos LMF, Rajendran, Ferreira LR, Gennari SM, Su C. Isolation of viable Toxoplasma gondii from feral guinea fowl (Numida meleagris) and domestic rabbits (Oryctolagus cuniculus) from Brazil. Journal of Parasitology. 2011a doi: 10.1645/GE-2728.1. In Press. [DOI] [PubMed] [Google Scholar]
- Dubey JP, Rajendran C, Ferreira LR, Kwok OCH, Sinnett D, Majumdar D, Su C. A new atypical highly mouse virulent Toxoplasma gondii genotype isolated from a wild black bear in Alaska. Journal of Parasitology. 2010;96:713–716. doi: 10.1645/GE-2429.1. [DOI] [PubMed] [Google Scholar]
- Dubey JP, Rajendran, Ferreira LR, Martins J, Kwok OCH, Hill DE, Villena I, Zhou H, Su C, Jones JL. High prevalence and genotypes of Toxoplasma gondii isolated from goats from a retail meat store destined for human consumption in the USA. International Journal for Parasitology. 2011b;41:827–833. doi: 10.1016/j.ijpara.2011.03.006. [DOI] [PubMed] [Google Scholar]
- Dubey JP, Speer CA, Shen SK, Kwok OCH, Blixt JA. Oocyst-induced murine toxoplasmosis: life cycle, pathogenicity, and stage conversion in mice fed Toxoplasma gondii oocysts. Journal of Parasitology. 1997;83:870–882. [PubMed] [Google Scholar]
- Dubey JP, Thulliez P, Powell EC. Toxoplasma gondii in Iowa sows: comparison of antibody titers to isolation of T. gondii by bioassays in mice and cats. Journal of Parasitology. 1995;81:48–53. [PubMed] [Google Scholar]
- Dubey JP, Zhu XQ, Sundar N, Zhang H, Kwok OCH, Su C. Genetic and biologic characterization of Toxoplasma gondii isolates of cats from China. Veterinary Parasitology. 2007;145:352–356. doi: 10.1016/j.vetpar.2006.12.016. [DOI] [PubMed] [Google Scholar]
- Dunay IR, DaMatta RA, Fux B, Presti R, Greco S, Colonna M, Sibley LD. Gr1+ (Ly6C+) inflammatory monocytes are required for mucosal resistance to the pathogen Toxoplasma gondii. Immunity. 2008;29:306–317. doi: 10.1016/j.immuni.2008.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunay IR, Sibley LD. Monocytes mediate mucosal immunity to Toxoplasma gondii. Current Opinion in Immunology. 2010;22:461–466. doi: 10.1016/j.coi.2010.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbez-Rubinstein A, Ajzenberg D, Dardé ML, Cohen R, Dumètre A, Yera H, Gondon E, Janaud JC, Thulliez P. Congenital toxoplasmosis and reinfection during pregnancy: case report, strain characterization, experimental model of reinfection, and review. Journal of Infectious Diseases. 2009;199:280–285. doi: 10.1086/595793. [DOI] [PubMed] [Google Scholar]
- Frazão-Teixeira E, Sundar N, Dubey JP, Grigg ME, de Oliveira FCR. Multi-locus DNA sequencing of Toxoplasma gondii isolated from Brazilian pigs identifies genetically divergent strains. Veterinary Parasitology. 2011;175:33–39. doi: 10.1016/j.vetpar.2010.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frenkel JK, Dubey JP, Miller NL. Toxoplasma gondii in cats: fecal stages identified as coccidian oocysts. Science. 1970;167:893–896. doi: 10.1126/science.167.3919.893. [DOI] [PubMed] [Google Scholar]
- Grigg ME, Sundar N. Sexual recombination punctuated by outbreaks and clonal expansions predicts Toxoplasma gondii population genetics. International Journal for Parasitology. 2009;39:925–933. doi: 10.1016/j.ijpara.2009.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heimesaat MM, Bereswill S, Fischer A, Fuchs D, Struck D, Niebergall J, Jahn HK, Dunay IR, Moter A, Gescher DM, Schumann RR, Göbel UB, Liesenfeld O. Gram-negative bacteria aggravate murine small intestinal Th1-type immunopathology following oral infection with Toxoplasma gondii. Journal of Immunology. 2006;177:8785–8795. doi: 10.4049/jimmunol.177.12.8785. [DOI] [PubMed] [Google Scholar]
- Hill D, Coss C, Dubey JP, Wroblewski K, Sautter M, Hosten T, Muñoz-Zanzi C, Mui E, Withers S, Boyer K, Hermes G, Coyne J, Jagdis F, Burnett A, McLeod P, Morton H, Robinson D, McLeod R. Identification of a sporozoite-specific antigen from Toxoplasma gondii. Journal of Parasitology. 2011;97:328–337. doi: 10.1645/GE-2782.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchison WM, Dunachie JF, Work K. Brief report. The faecal transmission of Toxoplasma gondii. Acta Pathologica et Microbiologica Scandinavica. 1968;74:462–464. doi: 10.1111/j.1699-0463.1968.tb03501.x. [DOI] [PubMed] [Google Scholar]
- Jamieson SE, de Roubaix LA, Cortina-Borja M, Tan HK, Mui EJ, Cordell HJ, Kirisits MJ, Miller EN, Peacock CS, Hargrave AC, Coyne JJ, Boyer K, Bessieres M-H, Buffolano W, Ferret N, Franck J, Kieffer F, Meier P, Nowakowska DE, Paul M, Peyron F, Stray-Pedersen B, Prusa AR, Thulliez P, Wallon M, Petersen E, McLeod R, Gilbert RE, Blackwell JM. Genetic and epigenetic factors at COL2A1 and ABCA4 influence clinical outcome in congenital toxoplasmosis. PLoS ONE. 2008;3:e2285. doi: 10.1371/journal.pone.0002285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamieson SE, Peixoto-Rangel AL, Hargrave AC, de Roubaix LA, Mui EJ, Boulter NR, Miller EN, Fuller SJ, Wiley JS, Castellucci L, Boyer K, Peixe RG, Kirisits MJ, Elias LD, Coyne JJ, Correa-Oliveira R, Sautter M, Smith NC, Lees MP, Swisher CN, Heydemann P, Noble AG, Patel D, Bardo D, Burrowes D, McLone D, Roizen N, Withers S, Bahia-Oliveira LM, McLeod R, Blackwell JM. Evidence for associations between the purinergic receptor P2X7 (P2RX7) and toxoplasmosis. Genes and Immunity. 2010;11:374–383. doi: 10.1038/gene.2010.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson J, Suzuki Y, Mack D, Mui E, Estes R, David C, Skamene E, Forman J, McLeod R. Genetic analysis of influences on survival following Toxoplasma gondii infection. International Journal for Parasitology. 2002a;32:179–185. doi: 10.1016/s0020-7519(01)00321-6. [DOI] [PubMed] [Google Scholar]
- Johnson JJ, Roberts CW, Pope C, Roberts F, Kirisits MJ, Estes R, Mui E, Krieger T, Brown CR, Forman J, McLeod R. In vitro correlates of Ld-restricted resistance to toxoplasmic encephalitis and their critical dependence on parasite strain. Journal of Immunology. 2002b;169:966–973. doi: 10.4049/jimmunol.169.2.966. [DOI] [PubMed] [Google Scholar]
- Lees MP, Fuller SJ, McLeod R, Boulter NR, Miller CM, Zakrzewski AM, Mui EJ, Witola WH, Coyne JJ, Hargrave AC, Jamieson SE, Blackwell JM, Wiley JS, Smith NC. P2X7 receptor-mediated killing of an intracellular parasite, Toxoplasma gondii, by human and murine macrophages. Journal of Immunology. 2010;184:7040–7046. doi: 10.4049/jimmunol.1000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liesenfeld O. Oral infection of C57BL/6 mice with Toxoplasma gondii: A new model of inflammatory bowel disease? Journal of Infectious Diseases. 2002;185(Suppl 1):S96–S101. doi: 10.1086/338006. [DOI] [PubMed] [Google Scholar]
- Liesenfeld O, Kosek J, Remington JS, Suzuki Y. Association of CD4+ T cell-dependent, interferon-γ-mediated necrosis of the small intestine with genetic susceptibility of mice to peroral infection with Toxoplasma gondii. Journal of Experimental Medicine. 1996;184:597–607. doi: 10.1084/jem.184.2.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunde MN, Jacobs L. Antigenic differences between endozoites and cystozoites of Toxoplasma gondii. Journal of Parasitology. 1983;69:806–808. [PubMed] [Google Scholar]
- Mack D, Johnson JJ, Roberts F, Roberts CW, Estes RG, David C, Grumet FC, McLeod R. HLA-class II genes modify outcome of Toxoplasma gondii infection. International Journal for Parasitology. 1999;29:1351–1358. doi: 10.1016/s0020-7519(99)00152-6. [DOI] [PubMed] [Google Scholar]
- McLeod R, Estes RG, Mack DG, Cohen H. Immune response of mice to ingested Toxoplasma gondii. A model of Toxoplasma infection acquired by ingestion. Journal of Infectious Diseases. 1984;149:234–244. doi: 10.1093/infdis/149.2.234. [DOI] [PubMed] [Google Scholar]
- McLeod R, Eisenhauer P, Mack D, Brown C, Filice G, Spitalny G. Immune responses associated with early survival after peroral infection with Toxoplasma gondii. Journal of Immunology. 1989;142:3247–3255. [PubMed] [Google Scholar]
- McLeod R, Skamene E, Brown CR, Eisenhauer P, Mack DG. Genetic regulation on early survival and cyst number after peroral Toxoplasma gondii infection of AxB/ BxA recombinant inbred and B10 congenic mice. Journal of Immunology. 1989;143:3031–3034. [PubMed] [Google Scholar]
- McLeod R, Brown C, Mack D. Immunogenetics influence outcome of Toxoplasma gondii infection. Research in Immunology. 1993;144(1):61–65. doi: 10.1016/s0923-2494(05)80101-4. [DOI] [PubMed] [Google Scholar]
- Muñoz M, Heimesaat MM, Danker K, Struck D, Lohmann U, Plickert R, Bereswill S, Fischer A, Dunay IR, Wolk K, Loddenkemper C, Krell HW, Libert C, Lund LR, Frey O, Hölscher C, Iwakura Y, Ghilardi N, Ouyang W, Kamradt T, Sabat R, Liesenfeld O. Interleukin (IL)-23 mediates Toxoplasma gondii-induced immunopathology in the gut via matrixmetalloproteinase-2 and IL-22 but independent of IL-17. Journal of Experimental Medicine. 2009;206:3047–3059. doi: 10.1084/jem.20090900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parmley SF, Gross U, Sucharczuk A, Windeck T, Sgarlato GD, Remington JS. Two alleles of the gene encoding surface antigen P22 in 25 strains of Toxoplasma gondii. Journal of Parasitology. 80:293–301. [PubMed] [Google Scholar]
- Pomares C, Ajzenberg D, Bornard L, Bernardin G, Hasseine L, Dardé ML, Marty P. Toxoplasmosis and horse meat, France. Emerging Infectious Diseases. 2011;17:1327–1328. doi: 10.3201/eid1707.101642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachinel N, Buzoni-Gatel D, Dutta C, Mennechet FJ, Luangsay S, Minns LA, Grigg ME, Tomavo S, Boothroyd JC, Kasper LH. The induction of acute ileitis by a single microbial antigen of Toxoplasma gondii. Journal of Immunology. 2004;173:2725–35. doi: 10.4049/jimmunol.173.4.2725. [DOI] [PubMed] [Google Scholar]
- Remington JS, McLeod R, Thulliez P, Desmonts G. In: Toxoplasmosis. In: Infectious Diseases of the Fetus and Newborn Infant. Remington JS, Klein JS, Wilson CB, Baker CJ, editors. Elsevier Saunders; Philadelphia: 2006. pp. 947–1091. [Google Scholar]
- Schreiner M, Liesenfeld O. Small intestinal inflammation following oral infection with Toxoplasma gondii does not occur exclusively in C57BL/6 mice: review of 70 reports from the literature. Memorias do Instituto Oswaldo Cruz. 2009;104:221–233. doi: 10.1590/s0074-02762009000200015. [DOI] [PubMed] [Google Scholar]
- Speer CA, Dubey JP. Ultrastructure of early stages of infection in mice fed Toxoplasma gondii oocysts. Parasitology. 1998;116:35–42. doi: 10.1017/s0031182097001959. [DOI] [PubMed] [Google Scholar]
- Tan TG, Mui E, Cong H, Witola WH, Montpetit A, Muench SP, Sidney J, Alexander J, Sette A, Grigg ME, Maewal A, McLeod R. Identification of T. gondii epitopes, adjuvants, and host genetic factors that influence protection of mice and humans. Vaccine. 2010;28:3977–3989. doi: 10.1016/j.vaccine.2010.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velmurugan GV, Su C, Dubey JP. Isolate designation and characterization of Toxoplasma gondii isolates from pigs in the United States. Journal of Parasitology. 2009;95:95–99. doi: 10.1645/GE-1746.1. [DOI] [PubMed] [Google Scholar]
- Witola WH, Mui E, Hargrave A, Liu S, Hypolite M, Montpetit A, Cavailles P, Bisanz C, Cesbron-Delauw MF, Fournie GJ, McLeod R. NALP1 influences susceptibility to human congenital toxoplasmosis, Proinflammatory cytokine response, and fate of Toxoplasma gondii-infected monocytic cells. Infection and Immunity. 2011;79:756–766. doi: 10.1128/IAI.00898-10. [DOI] [PMC free article] [PubMed] [Google Scholar]