Introduction
Society is facing one of the largest public health challenges in its history—the growth of the population of older adults. Improvements in public health, the discovery of antibiotics, and advances in modern medicine have resulted in unprecedented gains in human longevity. For most Americans the years after age 65 are a time of good health, independence, and integration of a life's work and experience. Eventually, however, most adults will develop one or more chronic illnesses with which they may live for many years before they die. Over three-quarters of deaths in the United States are due to chronic diseases of the heart, lungs, brain, and other vital organs.1 Even cancer, which accounts for nearly a quarter of U.S. deaths, has become a chronic, multiyear illness for many. For a minority of patients with serious illness (e.g., metastatic colon cancer), the time following diagnosis is characterized by a stable period of relatively good functional and cognitive performance followed by a predictable and short period of functional and clinical decline.2 However, for most patients with serious illness (e.g., heart or lung disease, Parkinson's disease, dementia, stroke, neuromuscular degenerative diseases, and many cancers), the time following diagnosis is characterized by months to years of physical and psychological symptom distress; progressive functional dependence and frailty; considerable family support needs; and high health care resource use.2–5 Currently and over the next decades most physicians will be caring for seriously ill elders with multiple comorbidities, lengthy duration of illness, and intermittent acute exacerbations interspersed with periods of relative stability.1 Abundant evidence suggests that most advanced stages of disease are characterized by inadequately treated physical distress; fragmented care systems; poor communication between doctors, patients, and families; and enormous strains on family caregiver and support systems.6
Palliative Care for Older Adults
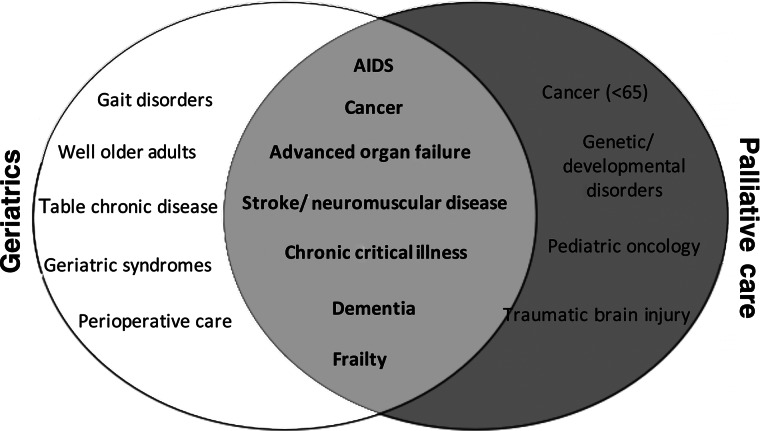
Palliative care for elders differs from what is usually appropriate in younger adults because of the nature and duration of chronic illness during old age. The prototypical example of a palliative care patient is that of a 55-year-old mother of two with advanced ovarian cancer. Care for this patient would include chemotherapy until it no longer meets the patient's goals of care; treating her symptoms (e.g., nausea, pain, fatigue); addressing her psychological and spiritual concerns; supporting her partner; and helping to arrange for care of her children after her death. The majority of this patient's care occurs at home (with or without hospice) or in the hospital, and the period of functional debility is brief (months). In reality, a frail 88-year-old widowed woman with advanced heart failure, diabetes mellitus, osteoarthritis, mild cognitive impairment, and frailty typifies the most common example of a patient requiring palliative care. Palliative care for this patient involves treating the primary disease process (advanced heart failure); managing her multiple chronic medical conditions and comorbidities (diabetes mellitus, arthritis) and geriatric syndromes (cognitive impairment, frailty); assessing and treating the physical and psychological symptom distress associated with all of these medical issues; and establishing goals of care and treatment plans in the setting of an unpredictable prognosis. Additionally, the needs of her caregiver(s) are also different from those of the caregiver of the younger patient. Individuals caring for geriatric patients are often adult children with their own families, work responsibilities, and medical conditions. These roles must be balanced with the months to years of personal care that they will provide to their aging parent. Finally, because older adults often make multiple transitions across care settings (home, hospital, rehabilitation, long-term care), especially in the last months of life, palliative care programs for older adults must assure that care plans and patient goals are maintained from one setting to another. Thus, palliative care for the elderly is centered on the identification and amelioration of functional and cognitive impairment; the development of frailty leading to dependence on caregivers; symptom, emotional, and spiritual distress; and bereavement needs of adult children and elderly partners. The overlap between the traditional fields of geriatrics and palliative care is shown in Figure 1.
FIG. 1.
The intersection between geriatrics and palliative care.
The Knowledge Base of Palliative Care for Older Adults
Although death occurs far more commonly in the elderly than in any other age group, the evidence base for palliative care in older adults is sparse.7 For example, the majority of symptom prevalence studies have focused on patients with cancer and AIDS, have not included the oldest old, have excluded patients with associated comorbidities, or have focused almost exclusively on pain. The incidence and prevalence of pain in older populations is unknown. Studies have suggested that the prevalence of significant pain in community-dwelling older adults may be as high as 56%8 and that almost one-fifth of older adults take analgesic medications on a regular basis.9 Similarly, it has been suggested that 45%–80% of nursing home residents have substantial pain and that many of these patients have multiple pain complaints and multiple potential sources of pain.10 Available data also point to a high prevalence of nonpain symptoms in older adults with serious and chronic illness. In retrospective interviews with family members of patients who died of noncancer illnesses in the United Kingdom, 67% of patients experienced moderate to severe pain, 49% had trouble breathing, 27% reported nausea, 36% reported depression, and 36% reported sleep disturbances.11 In an analysis of patients with heart failure, end-stage liver disease, lung cancer, and COPD from the SUPPORT trial, over 20% of patients consistently experienced severe dyspnea during the six months prior to death.12–14 A companion study to SUPPORT reported almost identical pain findings for a cohort of hospitalized patients 80 years and older15 and also noted a high prevalence of anxiety and depression in the last six months of life.16
Preliminary studies suggest pain and other symptoms are underassessed, undertreated, and are associated with a number of negative outcomes in older adults.17 Pain is perhaps the best studied symptom, and data from several studies suggest that untreated pain is associated with depression, decreased socialization, sleep disturbance, impaired ambulation, and increased health care utilization in older adults.18 These studies are limited by small sample sizes, have included relatively healthy subjects with defined conditions (e.g., osteoarthritis), have focused on postoperative surgical patients, or have been confined to one disease state (e.g., cancer). Additionally, they have not included frail older adults nor adults with multiple comorbidities and have not examined the association of pain with outcomes such as gait disturbances, rehabilitation and functional recovery, frailty, and functional dependence.18 Studies in older adults that have included these outcomes (functional recovery, frailty, falls, and function) have typically not included pain and other symptoms as independent variables.19–21 Studies on the prevalence, assessment, and association of other symptoms (e.g., dyspnea, anxiety, nausea, fatigue) on quality of life, function, and other outcomes are largely lacking.
The evidence base for the effective management of pain and other symptoms in older adults is also sparse. Although the American Geriatrics Society published guidelines for the treatment of acute and persistent pain, these guidelines were largely based upon small cohort studies and expert opinion.22 Recommendations for age-adjusted dosing are not available for most analgesics,18 and almost all analgesics have side effect profiles that are particularly problematic in older adults.22 Interventions directed at other symptoms (e.g., dyspnea, nausea, anxiety) have rarely included older adults or have focused on relatively narrow conditions (e.g., chemotherapy induced nausea), and the results are difficult to generalize to older adults with advanced illness and multiple comorbidities.7 Even studies in younger adults have rarely linked the treatment of pain to outcomes other than symptom relief. Although many have argued that patient comfort should be sufficient stimulus to alter pain management practices,1,23,24 the documented difficulties in shifting clinician priorities and behaviors25 suggest that empirical data regarding the adverse effects of pain and other symptoms on clinical outcomes are required to change practice patterns and improve patient care.
Moreover, the burdens of serious illness extend to patients' families and friends.4,5,26 More than 50 million individuals are relied on as informal caregivers27 due to recent efforts to reduce hospitalization rates and lengths of stay. The majority of these people are older adults who endure stress and burden related to both caring for the individual in the setting of serious illness and in coping with their death. An increasing body of research demonstrates adverse financial, physical, and psychological effects on them. For example, a study recently reported that over one-third of 893 caregivers had substantial stress; and 86% stated that they needed more help with transportation (62%), homemaking (55%), nursing (28%), or personal care (26%) than they were currently receiving or could afford.5 Caregivers with care needs were significantly more likely to consider suicide, have depressive symptoms, and to report that caring for patients interfered with their lives and reduced their independence.4 Caregiving has also been shown to be an independent risk factor for death, major depression, and associated comorbidities.28
What Is Needed?
An adequate evidence base for palliative care for older adults will require new knowledge; creation of innovative models of care delivery; the development of new research instruments, designs, and analytic techniques; and the application of established instruments, designs, and techniques from other fields to palliative care and aging research. Traditionally, research in pain and other symptoms has relied upon patient self-report as the gold standard of assessment.29 For patients with cognitive impairment, such assessment may be impractical or simply impossible, and reliable means of assessing pain and other symptoms through behavioral observation or through the use of proxies are required. Unfortunately, existing observational scales30 require considerable skill, experience, and familiarity with the patient to administer; and validated scales employing proxy respondents are not available.18 Researchers also face complexities in studying patients with multiple symptoms that may interact with each other—particularly since it may be difficult to distinguish symptoms caused by the patient's illness from those resulting from treatments. Such patients require instruments that assess a wide constellation of symptoms and multiple dimensions within each individual symptom. A few such instruments exist, however, they are relatively complex, lengthy, burdensome, and have not been validated in older adults.31–34 Indeed, in a population-based study of adults with recently diagnosed rectal cancer, subjects who were older, had poor performance status, or were receiving active palliative care were significantly more likely to have missing data on physical functioning and on global quality of life than younger and more highly functional patients over the two-year study.35 Although some research questions in geriatric palliative care may be addressed using the gold standard of clinical research—the randomized controlled trial—many others may only be feasibly addressed through observational data and quasi-experimental designs. Thus, improvements in care require careful and innovative use of nonrandomized and sometimes uncontrolled settings.1
Finally, specific analytic issues unique to palliative care in older adults also require attention. For example, the problem of missing or distorted data is considerable in palliative care research.1 Data is often missing because patients with advanced disease die during studies or are unable to report directly about their symptoms, concerns, or attitudes due to their illness, treatment, or both have left them confused, weak, or unconscious. Sophisticated research methods to deal with nonrandom missing data are required in palliative care research but are not yet widely used. Many studies in palliative care are observational or employ quasi-experimental designs and thus require analytic techniques that strengthen the inferences made from the studies.
Addressing the Knowledge Gap
In summary, there is a pressing need to improve the evidence base for palliative care in older adults. The areas of research that need to be addressed include establishing the prevalence of symptoms in patients with chronic disease; evaluating the association between symptom treatment and outcomes; increasing the evidence base for symptom treatment; understanding patients' psychological/spiritual well-being and quality of life goals; and elucidating sources of caregiver burden, reevaluating service delivery, and adapting research methodologies specifically for palliative care. Although great strides were made in outlining the need for improving palliative care at the 2004 NIH State of the Science Conference on Improving End-of-Life Care,36 even at this landmark event there was a focus on terminal disease and not on expanding the idea of palliative care to include improving the quality of care of older patients with multiple chronic illnesses. In an effort to address this gap in research and develop the knowledge that clinicians need to appropriately care for older adults with serious illness, 15 research experts in aging and palliative care research gathered in Bethesda, Maryland, on January 31, 2013 at a meeting co-sponsored by the National Palliative Care Research Center, the National Institute on Aging (NIA), and the Icahn School of Medicine at Mount Sinai Claude D. Pepper Older Adult Independence Center. The purpose of the meeting was to examine the state of the science in geriatric palliative care, identify research priorities that could, if addressed, lead to improved palliative care in older adults, and identify studies needed to fill gaps. Over the next six months, the Journal will be publishing a series comprising the proceedings of this conference entitled “Research Priorities in Geriatric Palliative Care.” The topics that will be addressed include the epidemiology of serious illness; research methods; multimorbidity; nonpain symptoms; informal caregiving; establishing goals, values, and preferences; long-term care; disparities; and policy initiatives. The topics of research priorities for pain in older adults 37 and care for persons with end-stage dementia38 are not included in this series, as comprehensive papers addressing these topics have been recently published. It is our hope that this series will help to develop a template that will guide research and funding priorities in palliative care for older adults.
Acknowledgments
This work was supported by the NIA, Claude D. Pepper Older Americans Independence Center at the Icahn School of Medicine at Mount Sinai [5P30AG028741], and the National Palliative Care Research Center. Dr. Morrison is the recipient of a Midcareer Investigator Award in Patient-Oriented Research (5K24AG022345-10).
References
- 1.Field MJ, editor; Cassel CK, editor. Approaching death: Improving care at the end of life. Washington, DC: National Academy Press; 1997. [PubMed] [Google Scholar]
- 2.Lunney JR. Lynn J. Foley DJ. Lipson S. Guralnik JM. Patterns of functional decline at the end of life. JAMA. 2003;289(18):2387–2392. doi: 10.1001/jama.289.18.2387. [DOI] [PubMed] [Google Scholar]
- 3.SUPPORT Principal Investigators: A controlled trial to improve care for seriously ill hospitalized patients: The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT) JAMA. 1995;274(20):1591–1598. [PubMed] [Google Scholar]
- 4.Emanuel EJ. Fairclough DL. Slutsman J. Emanuel LL. Understanding economic and other burdens of terminal illness: The experience of patients and their caregivers. Ann Intern Med. 2000;132(6):451–459. doi: 10.7326/0003-4819-132-6-200003210-00005. [DOI] [PubMed] [Google Scholar]
- 5.Emanuel EJ. Fairclough DL. Slutsman J. Alpert H. Baldwin D. Emanuel LL. Assistance from family members, friends, paid care givers, and volunteers in the care of terminally ill patients. N Engl J Med. 1999;341(13):956–963. doi: 10.1056/NEJM199909233411306. [DOI] [PubMed] [Google Scholar]
- 6.Signorielli N. Mass Media Images and Impact on Health: A Sourcebook. Westport, CT: Greenwood Press; 1993. Physical disabilities, impairment and safety, mental illness, and death; pp. 37–42. [Google Scholar]
- 7.Morrison RS, editor; Meier DE, editor. Geriatric Palliative Care. New York: Oxford University Press; 2003. [Google Scholar]
- 8.Helm RD. Gibson SJ. Pain in older people. In: Cronbie IK, editor; Croft R, editor; Linton SJ, editor; Lerexche L, editor; Von Dorff M, editor. Epidemiology of Pain. Seattle, WA: IASP Press; 2000. pp. 102–112. [Google Scholar]
- 9.Cooner E. Amorosi S. The Study of Pain in Older Americans. New York: Louis Harris and Associates; 1997. [Google Scholar]
- 10.Ferrell B. Pain evaluation and management in the nursing home. Ann Intern Med. 1995;123:681–687. doi: 10.7326/0003-4819-123-9-199511010-00007. [DOI] [PubMed] [Google Scholar]
- 11.Seale C. Cartwright A. The Year Before Death. Brookfield, VT: Ashgale Publishing Co.; 1994. [Google Scholar]
- 12.Claessens MT. Lynn J. Zhong Z, et al. Dying with lung cancer or chronic obstructive pulmonary disease: Insights from SUPPORT. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Geriatr Soc. 2000;48(S5):S146–S153. doi: 10.1111/j.1532-5415.2000.tb03124.x. [DOI] [PubMed] [Google Scholar]
- 13.Roth K. Lynn J. Zhong Z. Borum M. Dawson NV. Dying with end stage liver disease with cirrhosis: Insights from SUPPORT. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. J Am Geriatr Soc. 2000;48(S5):S122–S130. [PubMed] [Google Scholar]
- 14.Levenson JW. McCarthy EP. Lynn J. Davis RB. Phillips RS. The last six months of life for patients with congestive heart failure. J Am Geriatr Soc. 2000;48(S5):S101–S109. doi: 10.1111/j.1532-5415.2000.tb03119.x. [DOI] [PubMed] [Google Scholar]
- 15.Desbiens NA. Mueller-Rizner N. Connors AF., Jr. Hamel MB. Wenger NS. Pain in the oldest-old during hospitalization and up to one year later. HELP Investigators. Hospitalized Elderly Longitudinal Project. J Am Geriatr Soc. 1997;45(10):1167–1172. doi: 10.1111/j.1532-5415.1997.tb03765.x. [DOI] [PubMed] [Google Scholar]
- 16.Somogyi-Zalud E. Zhong Z. Lynn J. Hamel MB. Elderly persons' last six months of life: Findings from the Hospitalized Elderly Longitudinal Project. J Am Geriatr Soc. 2000;48(S5):S131–S139. doi: 10.1111/j.1532-5415.2000.tb03122.x. [DOI] [PubMed] [Google Scholar]
- 17.Reyes-Gibby CC. Aday L. Cleeland C. Impact of pain on self-rated health in the community-dwelling older adults. Pain. 2002;95(1–2):75–82. doi: 10.1016/s0304-3959(01)00375-x. [DOI] [PubMed] [Google Scholar]
- 18.Ferrell BA. E WJ. Meier DE. Pain. In: Morrison RS, editor; Geriatric Palliative Care. New York: Oxford University Press; 2003. pp. 205–229. [Google Scholar]
- 19.Magaziner J. Hawkes W. Hebel JR, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. 2000;55(9):M498–M507. doi: 10.1093/gerona/55.9.m498. [DOI] [PubMed] [Google Scholar]
- 20.Fried LP. Tangen CM. Walston J, et al. Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 21.Tinetti ME. Speechley M. Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 22.American Geriatrics Society: The management of persistent pain in older adults. www.americangeriatrics.org/healthcareprofessionals/clinical-practice/clinical_guidelines_recommendations/2009/ [May 21;2013 ]. www.americangeriatrics.org/healthcareprofessionals/clinical-practice/clinical_guidelines_recommendations/2009/
- 23.Meier DE. Morrison RS. Cassel CK. Improving palliative care. Ann Intern Med. 1997;127(3):225–230. doi: 10.7326/0003-4819-127-3-199708010-00008. [DOI] [PubMed] [Google Scholar]
- 24.Cassell EJ. The nature of suffering and the goals of medicine. N Engl J Med. 1982;306(11):639–645. doi: 10.1056/NEJM198203183061104. [DOI] [PubMed] [Google Scholar]
- 25.Foley KM. Pain relief into practice: Rhetoric without reform. J Clin Oncol. 1995;13(9):2149–2151. doi: 10.1200/JCO.1995.13.9.2149. [DOI] [PubMed] [Google Scholar]
- 26.Levine C. The loneliness of the long term caregiver. N Engl J Med. 1999;340:1587–1590. doi: 10.1056/NEJM199905203402013. [DOI] [PubMed] [Google Scholar]
- 27.Caregiving in the U.S. National Alliance for Caregiving and AARP; Washington, DC: 2004. [Google Scholar]
- 28.Schulz R. Beach S. Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. JAMA. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 29.Agency for Health Care Policy and Research. Management of cancer pain: Adults. Cancer Pain Guideline Panel. Am Fam Physician. 1994;49(8):1853–1868. [PubMed] [Google Scholar]
- 30.Hurley A. Volicer B. Hanrahan P, et al. Assessment of discomfort in advanced Alzheimer patients. Res Nurs Health. 1992;15:369–377. doi: 10.1002/nur.4770150506. [DOI] [PubMed] [Google Scholar]
- 31.Daut RL. Cleeland CS. Flanery RC. Development of the Wisconsin Brief Pain Questionnaire to assess pain in cancer and other diseases. Pain. 1983;17(2):197–210. doi: 10.1016/0304-3959(83)90143-4. [DOI] [PubMed] [Google Scholar]
- 32.Portenoy RK. Thaler HT. Kornblith AB, et al. The Memorial Symptom Assessment Scale: An instrument for the evaluation of symptom prevalence, characteristics and distress. Eur J Cancer. 1994;30A(9):1326–1336. doi: 10.1016/0959-8049(94)90182-1. [DOI] [PubMed] [Google Scholar]
- 33.Dudgeon D. Raubertas RF. Rosenthal SN. The short-form McGill Pain Questionnaire in chronic cancer pain. J Pain Symptom Manage. 1993;8(4):191–195. doi: 10.1016/0885-3924(93)90126-g. [DOI] [PubMed] [Google Scholar]
- 34.Dudgeon D. Multidemensional assessment of dyspnea. In: Portenoy RK, editor; Bruera E, editor. Palliative Care Research. New York: Oxford University Press; 2003. [Google Scholar]
- 35.Kopp I. Lorenz W. Rothmund M. Koller M. Relation between severe illness and non-completion of quality-of-life questionnaires by patients with rectal cancer. J R Soc Med. 2003;96(9):442–448. doi: 10.1258/jrsm.96.9.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.NIH: National Institutes of Health State-of-the-Science Conference Statement on Improving End-of-Life Care. U.S. Department of Health and Human Services: National Institutes of Health. Bethesda, MD: 2007. [Google Scholar]
- 37.Reid MC. Bennett DA. Chen WG, et al. Improving the pharmacologic management of pain in older adults: Identifying the research gaps and methods to address them. Pain medicine. 2011;12(9):1336–1357. doi: 10.1111/j.1526-4637.2011.01211.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mitchell SL. Black BS. Ersek M, et al. Advanced dementia: State of the art and priorities for the next decade. Ann Intern Med. 2012;156(1 Pt 1):45–51. doi: 10.1059/0003-4819-156-1-201201030-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]