Abstract
BACKGROUND
Posthospitalization care is important for recovery after trauma. Disadvantaged populations, like racial or ethnic minorities and the uninsured, make up substantial percentages of trauma patients, but their use of posthospitalization facilities is unknown.
STUDY DESIGN
This study analyzed National Trauma Data Bank admissions from 2007 for 18- to 64-year-olds and estimated relative risk ratios (RRR) of discharge to posthospitalization facilities—home, home health, rehabilitation, or nursing facility—by race, ethnicity, and insurance. Multinomial logistic regression adjusted for patient characteristics including age, sex, Injury Severity Score, mechanism of injury, and length of stay, among others.
RESULTS
There were 136,239 patients who met inclusion criteria with data for analysis. Most patients were discharged home (78.9%); fewer went to home health (3.3%), rehabilitation (5.0%), and nursing facilities (5.4%). When compared with white patients in adjusted analysis, relative risk ratios of discharge to rehabilitation were 0.61 (95% CI 0.56, 0.66) and 0.44 (95% CI 0.40, 0.49) for blacks and Hispanics, respectively. Compared with privately insured white patients, Hispanics had lower rates of discharge to rehabilitation whether privately insured (RRR 0.45, 95% CI 0.40, 0.52), publicly insured (RRR 0.51, 95% CI 0.42, 0.61), or uninsured (RRR 0.20, 95% CI 0.17, 0.24). Black patients had similarly low rates: private (RRR 0.63, 95% CI 0.56, 0.71), public (RRR 0.72, 95% CI 0.63, 0.82), or uninsured (RRR 0.27, 95% CI 0.23, 0.32). Relative risk ratios of discharge to home health or nursing facilities showed similar trends among blacks and Hispanics regardless of insurance, except for black patients with insurance whose discharge to nursing facilities was similar to their white counterparts.
CONCLUSIONS
Disadvantaged populations have more limited use of posthospitalization care such as rehabilitation after trauma, suggesting a potential improvement in trauma care for the underprivileged.
Acute injuries place an enormous burden on the long-term health and productivity of the United States population. Among those below age 75, injuries cause more years of life lost than cancer, heart disease, or HIV.1 Trauma accounts for more than 2 million hospitalizations annually, making up about 8% of all hospital admissions.1 Research has demonstrated the significant impairment that trauma patients suffer, with only 20% of patients in one San Diego study achieving a normal level of function after 18 months.2 One major step forward in strengthening trauma care is ensuring that all patients have access to the evidence-based therapies that are improving outcomes, including modalities used both in the hospital and those needed after acute hospitalization to improve functional and other long-term outcomes, such as rehabilitation or skilled nursing.
Annual reports indicate that disadvantaged populations continue to receive inferior quality of care due to lack of access to health services, provider and institutional biases, and poor health literacy, among other factors.3 Racial disparities have been well documented in both health care delivery and outcomes.4 Worse outcomes have been reported in studies of trauma patients among whom access to care is thought to be universal. Hispanic patients with traumatic brain injury (TBI) are more likely to be severely disabled 6 months after injury;5 Hispanic patients with spinal cord injury are more likely to be unemployed 1 year after injury;6 and black children have worse functional outcomes after TBI, including increased rates of speech, locomotion, and feeding deficits.7 Similar research exists for socioeconomically disadvantaged populations, such as the uninsured. In the trauma population, resource use is decreased among uninsured patients, who undergo fewer operative procedures,8 receive fewer physical therapy sessions, 8 and have less costly hospital stays.9 Furthermore, several studies have shown that uninsured patients have higher mortality rates after trauma.8,10
Posthospitalization care, particularly rehabilitation therapy, is widely accepted as an essential modality for improving short- and long-term functional outcomes and quality of life. In the case of TBI, an NIH consensus conference declared, “Rehabilitation services, matched to the needs of persons with TBI…, are required to optimize outcomes over the course of recovery.”11 The efficacy of rehabilitation therapies has been supported by a number of studies in settings that range from ankle sprains12 and hip fractures,13 to stroke,14 TBI,15,16 and trauma-related amputations.17 In cases of TBI, studies indicate that patients in rehabilitation ameliorate their ability to live at home, to function independently, and to find and maintain employment.15 Additionally, home rehabilitation programs have shown equivalent outcomes to inpatient rehabilitation programs in diverse populations from patients with hip fractures18 to TBI.19
Given the importance of rehabilitation and other posthospitalization care on health outcomes after trauma and the large contribution of disadvantaged racial, ethnic, and socioeconomic minorities to the trauma population, there is a paucity of research examining existing disparities in posthospitalization care for these patients. In the setting of TBI, studies have demonstrated disparities in rehabilitation placement for racial and ethnic minorities20 and patients with Medicaid;21 however, no study has examined the interplay of race, ethnicity, and insurance status on differences in discharge location among the general trauma population, using a large national database. This study hypothesized that patient race, ethnicity, and insurance status have a significant association with discharge location, even after adjusting for factors important in trauma outcomes, such as age, sex, mechanism of injury, and injury severity.
METHODS
This retrospective analysis used patient information from the National Trauma Data Bank (NTDB) for the year 2007, in which NTDB received entries from more than 700 trauma centers and other hospitals caring for trauma patients. The year 2007 was chosen because this was the first year that the NTDB used the National Trauma Data Standard (NTDS), which has significantly improved the reliability and fidelity of data in the NTDB.22 The database is maintained by the American College of Surgeons, which regularly publishes complete information on the NTDB.22
Analysis included trauma patients, aged 18 to 64 years. This study excluded pediatric (age 17 years or less) and geriatric (age 65 years or older) patients because of the high percentage of public insurance and low percentage of uninsured among these populations and because of their differing responses to trauma.23 Burn patients, patients who died in the hospital, and those with missing data on discharge location were also excluded.
The main variables of interest in this study were race or ethnicity and insurance status. Patients were divided into 3 insurance categories: Private insurance (Blue Cross/Blue Shield, private/commercial insurance, workers compensation, other government, no fault automobile); public insurance (Medicare and Medicaid); and uninsured (self-pay). Patients were additionally categorized as white, black, or Hispanic. Patients described as black were placed in the black group despite other descriptors listing them as Hispanic due to behaviors accessing health services that aligned Hispanic blacks more closely with non-Hispanic blacks than Hispanic whites.24 All other patients listed as Hispanic were placed with the Hispanic group despite other racial descriptors. Other racial minorities, such as Asian and American Indian, were excluded due to relatively low numbers.
Discharge location was the main explanatory outcome and was categorized into the following groups: home, home health, rehabilitation facility, and nursing facility. Nursing facility included both discharge locations listed as “skilled nursing facility” and “intermediate care facility,” as has been done in previous research.21 For unadjusted analysis, non-Hispanic white patients were considered the reference group; multivariable analysis used either privately insured patients, non-Hispanic white patients, or privately insured, non-Hispanic white patients as the reference, where appropriate. Home was established as the reference outcome. This study compared possible differences in patient demographic and injury severity features using ANOVA for continuous variables and Pearson’s chi-squared test for categorical variables. In unadjusted analysis, Pearson’s chi-squared test was also used to evaluate the significance of differing rates of discharge to the various locations listed above.
Using multinomial logistic regression to determine relative risk ratios (RRR) for discharge to the various locations, this study was able to adjust for variables known to affect outcomes in trauma. Our analysis evaluated the effect of race or ethnicity and insurance, individually. In further analysis, we modeled the data on a variable that combined race or ethnicity and insurance status to examine the interplay of these characteristics. In these multivariable models, the following covariates were adjusted for because of their influence as described in previous trauma literature: age, sex, Injury Severity Score (4 ISS categories: mild [1 to 8], moderate [9 to 15], severe [16 to 24], and extremely severe [≥25]), presence of shock (systolic blood pressure < 90 mmHg) on emergency department arrival, Glasgow Coma Scale Motor Score (GCS-M), mechanism of injury (motor vehicle collision, fall, gunshot wound, etc), type of injury (blunt vs penetrating), intention of injury, presence of severe head and/or extremity injury (Abbreviated Injury Score [AIS] ≥3), trauma level designation (I to IV), and length of hospital stay (LOS).25,26 Because this study focused on postdischarge rehabilitation access, patients who died in the hospital were not included in the multinomial analysis.
Two types of sensitivity analyses were incorporated into this study to ensure that our results were consistent and generalizable to the relevant populations. First, multiple imputation was used to ensure that the significant amount of missing data that is often seen in large database analyses did not bias the results. These methods are becoming increasingly accepted and have been validated in a number of studies.27 After completing the reported analyses using a strategy in which cases with missing data were dropped, the same analyses were repeated with a dataset in which patient race, insurance, age, sex, ISS, shock on emergency department arrival, GCS-M, mechanism of injury, type of injury, intention of injury, trauma level designation, and LOS were imputed. However, patients with missing outcomes information were dropped in both the imputed and nonimputed analyses because we chose not to attempt to impute the outcome being studied. It was decided a priori that results would be regarded valid only if analyses of both of the imputed and nonimputed datasets were similar. Second, a sensitivity analysis restricting the dataset to blunt trauma victims with no TBI was also performed to establish that these results were significant for the majority of trauma patients—blunt trauma victims with no significant head injury. All statistical calculations were performed using Stata Version 11 (Stat Corp), and p < 0.05 was considered statistically significant.
RESULTS
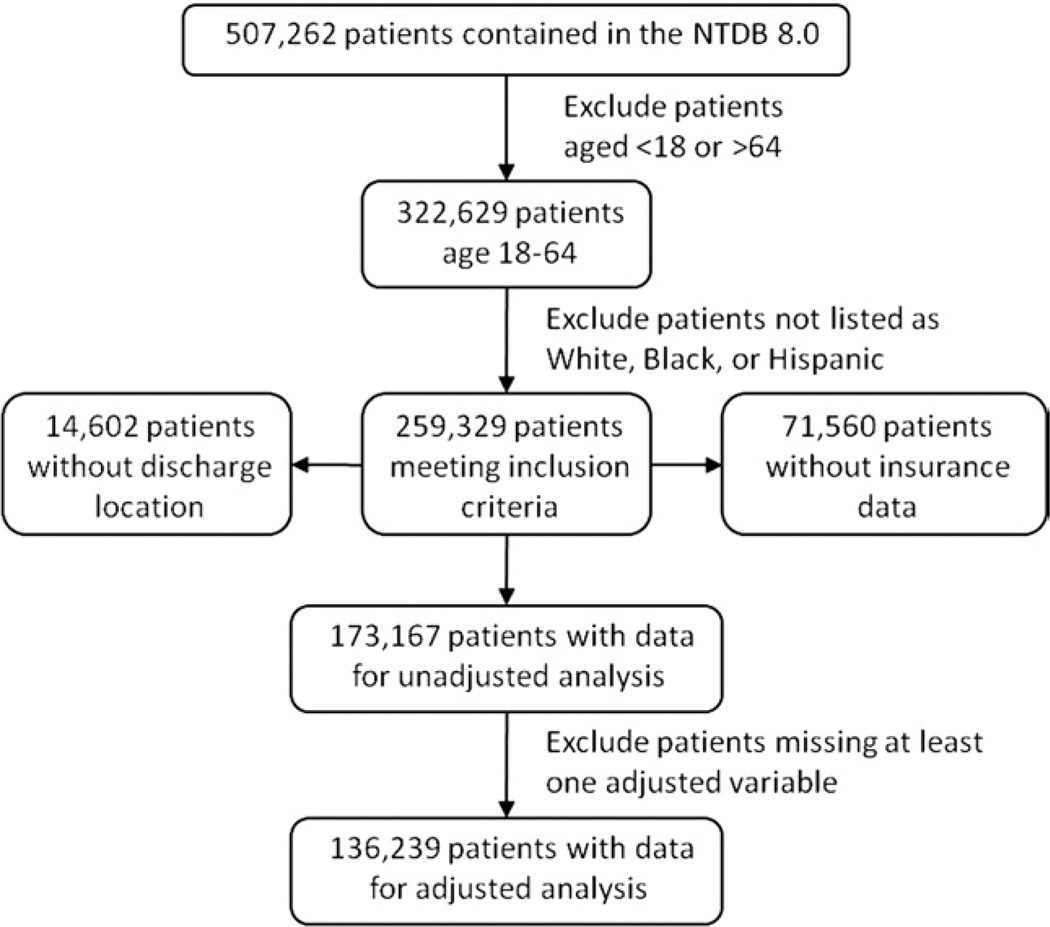
more than a half million patients were present in the NTDB 8.0, of which 173,167 met all inclusion criteria and had data for analysis. There were 5,034 patients who died in the hospital and were not included in multivariable analysis. An additional 31,894 patients (19.0%) were missing at least 1 piece of data required for multivariable analysis and could be evaluated only after multiple imputation; therefore, the final nonimputed dataset for adjusted analysis contained 136,239 patients (Fig. 1). Discharge location was missing in 5.6% of patients, who could not be evaluated. The study population was relatively young (mean age 37.7 ± 13.5 years), mostly male (72.9%), and white (65.8%). Table 1 contains a complete description of patient characteristics.
Figure 1.
Study inclusion criteria. NTDB, National Trauma Data Bank.
Table 1.
Patient Demographic and Injury Severity Characteristics NTDB 2007
| Demographic/injury severity | All patients | White | Black | Hispanic | p Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Total | 173,167 | 113,954 | 65.8 | 33,906 | 19.6 | 25,307 | 14.6 | ||
| Male | 125,677 | 72.9 | 79,478 | 70.1 | 25,746 | 76.0 | 20,453 | 80.8 | <0.001 |
| Age, y | <0.001 | ||||||||
| 18–24 | 39,986 | 23.1 | 23,326 | 20.5 | 8,935 | 26.4 | 7,725 | 30.5 | |
| 25–34 | 38,172 | 22.0 | 22,006 | 19.3 | 8,497 | 25.1 | 7,669 | 30.3 | |
| 35–44 | 34,996 | 20.2 | 22,931 | 20.1 | 7,038 | 20.8 | 5,027 | 19.9 | |
| 45–54 | 35,618 | 20.6 | 25,986 | 22.8 | 6,375 | 18.8 | 3,257 | 12.9 | |
| 55–64 | 24,395 | 14.1 | 19,705 | 17.3 | 3,061 | 9.0 | 1,629 | 6.4 | |
| Insurance status | <0.001 | ||||||||
| Private insurance | 89,422 | 51.6 | 68,237 | 59.9 | 11,131 | 32.8 | 10,054 | 39.7 | |
| Public insurance | 27,349 | 15.8 | 16,817 | 14.8 | 7,462 | 22.0 | 3,070 | 12.1 | |
| Uninsured | 56,396 | 32.6 | 28,900 | 25.4 | 15,313 | 45.2 | 12,183 | 48.1 | |
| Type of injury | <0.001 | ||||||||
| Blunt | 139,533 | 85.5 | 99,433 | 92.5 | 21,327 | 66.7 | 18,773 | 78.8 | |
| Penetrating | 23,767 | 14.6 | 8,075 | 7.5 | 10,639 | 33.3 | 5,053 | 21.2 | |
| Mechanism of injury | <0.001 | ||||||||
| Motor vehicle collision | 75,112 | 44.3 | 54,743 | 48.9 | 10,760 | 32.7 | 9,609 | 39.0 | |
| Fall | 36,583 | 21.6 | 27,963 | 25.0 | 4,181 | 12.7 | 4,439 | 18.0 | |
| Gunshot wound | 12,366 | 7.3 | 3,066 | 2.7 | 6,948 | 21.1 | 2,352 | 9.6 | |
| Stab wound | 11,401 | 6.7 | 5,009 | 4.5 | 3,691 | 11.2 | 2,701 | 11.0 | |
| Struck | 21,413 | 12.6 | 11,989 | 10.7 | 5,666 | 17.2 | 3,758 | 15.3 | |
| Intentional injury | 33,366 | 19.6 | 12,696 | 11.3 | 13,955 | 42.3 | 6,715 | 27.0 | <0.001 |
| Region of body injury | <0.001 | ||||||||
| Head | 25,262 | 14.6 | 17,248 | 15.1 | 3,897 | 11.5 | 4,117 | 16.3 | |
| Thorax | 20,611 | 11.9 | 14,080 | 12.4 | 3,692 | 10.9 | 2,839 | 11.2 | |
| Abdomen | 5,536 | 3.2 | 3,079 | 2.7 | 1,459 | 4.3 | 998 | 3.9 | |
| Extremity | 22,324 | 12.9 | 15,115 | 13.3 | 4,428 | 13.1 | 2,781 | 11.0 | |
| Shock (SBP < 90 mmHg) | 5,697 | 3.4 | 3,366 | 3.1 | 1,444 | 4.4 | 887 | 3.6 | <0.001 |
| Injury severity | |||||||||
| Mild (ISS ≤ 8) | 76,678 | 45.7 | 47,815 | 43.1 | 16,694 | 51.0 | 12,169 | 50.4 | |
| Moderate (ISS: 9–14) | 51,056 | 30.4 | 35,067 | 31.6 | 9,352 | 28.6 | 6,637 | 27.5 | |
| Severe (ISS: 15–24) | 23,277 | 13.9 | 16,457 | 14.9 | 3,770 | 11.5 | 3,050 | 12.6 | |
| Extremely severe (ISS ≥ 25) | 16,707 | 10.0 | 11,492 | 10.4 | 2,901 | 8.9 | 2,314 | 9.6 | |
| Mean LOS, d ± SD | 6.0 ± 9.8 | 5.9 ± 9.3 | 6.1 ± 10.9 | 6.1 ± 10.9 | <0.001 | ||||
| Discharge disposition | <0.001 | ||||||||
| Home | 136,600 | 78.9 | 87,488 | 76.8 | 27,286 | 80.5 | 21,826 | 86.2 | |
| Home health | 5,770 | 3.3 | 4,253 | 3.7 | 1,140 | 3.4 | 377 | 1.5 | |
| Rehabilitation facility | 8,641 | 5.0 | 6,794 | 6.0 | 1,068 | 3.2 | 779 | 3.1 | |
| Nursing facility | 9,399 | 5.4 | 7,187 | 6.3 | 1,657 | 4.9 | 555 | 2.2 | |
| Hospital transfer | 5,395 | 3.1 | 3,847 | 3.4 | 927 | 2.7 | 621 | 2.5 | |
| Other | 2,328 | 1.3 | 1,389 | 1.2 | 617 | 1.8 | 322 | 1.3 | |
| In-hospital mortality | 5,034 | 2.9 | 2,996 | 2.6 | 1,211 | 3.6 | 827 | 3.3 | <0.001 |
Table represents demographic and injury severity characteristics for patients from the NTDB 8.0, collected during the year 2007, who met the following inclusion criteria: age 18 to 64; listed as white, black, or Hispanic; having no burn injury; having data on discharge location and insurance status. White represents non-Hispanic white, and Hispanic represents non-black Hispanic. The p values represent significance of Pearson’s chi-squared test or ANOVA test when comparing variable of interest by race/ethnicity.
ISS, Injury Severity Score; LOS, length of stay; NTDB, National Trauma Data Bank; SBP, systolic blood pressure.
The majority of patients were discharged to home (78.9%). Notably more blacks (80.5%) and Hispanics (86.2%) were discharged to home than their white counterparts (76.8%), each p < 0.05 vs the white reference group in unadjusted analysis. Fewer black patients (3.2%) and Hispanic patients (3.1%) were discharged to rehabilitation facilities than whites (6.0%), each p < 0.05 vs white reference group in unadjusted analysis. A complete list of rates of discharge locations is included in Table 1.
In adjusted analysis, racial and ethnic minorities were less likely than whites to be discharged to rehabilitation facilities. Compared with white patients, the RRRs for similarly injured black or Hispanic patients to be discharged to rehabilitation facilities were 0.61 (95% CI 0.56, 0.66) and 0.44 (95% CI 0.40, 0.49), respectively. RRRs for home health care were similar in blacks (RRR 0.92, 95% CI 0.84, 1.00) compared with whites; Hispanics had significantly lower rates (RRR 0.37, 95% CI 0.33, 0.42) with regard to whites. Blacks (RRR 0.99, 95% CI 0.92, 1.06) were no less likely to be discharged to nursing facilities than whites; Hispanics (RRR 0.33, 95% CI 0.30, 0.37) were less likely (Table 2).
Table 2.
Adjusted Relative Risk Ratio of Discharge Location Compared with White Patients by Race/Ethnicity
| Race | Discharge location, RRR (95% CI) | |||
|---|---|---|---|---|
| Home health | Rehabilitation facility |
Nursing facility | ||
| Black | 0.92 (0.84–1.00) | 0.61 (0.56–0.66) | 0.99 (0.92–1.06) | |
| Hispanic | 0.37 (0.33–0.42) | 0.44 (0.40–0.49) | 0.33 (0.30–0.37) | |
Multinomial logistic regression with home as reference outcome and non-Hispanic, white patients as reference group. Hispanic refers to Non-black Hispanic. n = 136,239 patients who had complete data for all variables in adjusted analysis. Variables adjusted for include: age, sex, insurance status, type of injury, extremity injury, head injury, intentional injury, Injury Severity Score, shock, Glasgow Coma Scale Motor Score, mechanism of injury, trauma level designation, and length of stay.
RRR, relative risk ratio.
When looking at relative rates of discharge location by insurance status, uninsured patients were less likely to be discharged to home health care (RRR 0.61, 95% CI 0.57, 0.66), rehabilitation (RRR 0.46, 95% CI 0.43, 0.50), and nursing facilities (RR 0.44, 95% CI 0.41, 0.47) compared with the privately insured. Publicly insured patients were more likely to be discharged to rehabilitation (RRR 1.20, 95% CI 1.12, 1.29) or nursing facilities (RRR 1.70, 95% CI 1.60, 1.82), with differences in discharge to home health care (RRR 0.91, 95% CI 0.83, 0.99) that did not reach statistical significance in all sensitivity analyses (Table 3).
Table 3.
Adjusted Relative Risk Ratio (95% CI) of Discharge Location Compared with Privately Insured Patients (Reference Group) by Insurance Status
| Insurance status | Discharge location, RRR (95% CI) | ||
|---|---|---|---|
| Home health | Rehabilitation facility | Nursing facility | |
| Public | 0.91 (0.83–0.99)* | 1.20 (1.12–1.29) | 1.70 (1.60–1.82) |
| Uninsured | 0.61 (0.57–0.66) | 0.46 (0.43–0.50) | 0.44 (0.41–0.47) |
Multinomial logistic regression with home as reference outcome and privately insured patients as reference group.
The result was not significant in all sensitivity analyses; n = 136,239 patients who had complete data for all variables in adjusted analysis. Variables adjusted for include: age, sex, insurance status, type of injury, extremity injury, head injury, intentional injury, Injury Severity Score, shock, Glasgow Coma Scale Motor Score, mechanism of injury, trauma level designation, and length of stay.
RRR, relative risk ratio.
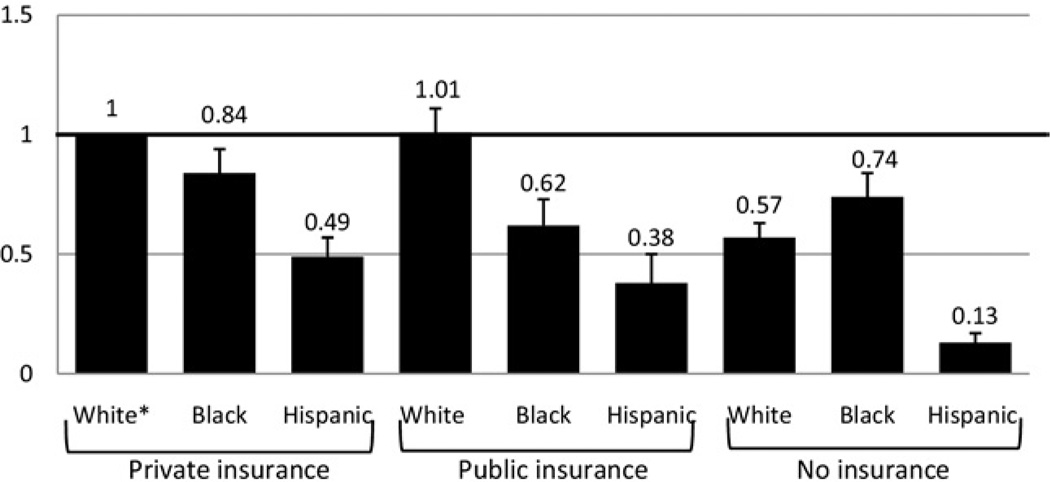
When examining the combined effect of race and insurance, adjusted analysis demonstrated that Hispanic patients, regardless of insurance status, were discharged at lower rates to all posthospitalization care facilities when examined against privately insured, non-Hispanic white patients. Compared with privately insured white patients, privately insured Hispanics were only 49% (RRR 0.49, 95% CI 0.41, 0.57) as likely to be discharged to home health care, and uninsured Hispanics were only 13% (RRR 0.13, 95% CI 0.10, 0.17) as likely. Privately insured black patients were less likely to be discharged to home health care as their privately insured white counterparts (RRR 0.84, 95% CI 0.74, 0.94). This difference was also seen in publicly insured black patients (RRR 0.62, 95% CI 0.53, 0.73) and uninsured black patients (RRR 0.74, 95% CI 0.66, 0.84) (Fig. 2 and Table 4).
Figure 2.
Adjusted relative risk ratio (RRR) of discharge to home health by race and insurance status. Multinomial logistic regression with “home” as reference outcome. * indicates reference group: non-Hispanic, white, privately insured patients. Error bars represent 95% CIs. White refers to non-Hispanic white; Hispanic refers to non-black Hispanic; n = 136,239 patients who had complete data for all variables in adjusted analysis. Variables adjusted for include age, sex, type of injury, extremity injury, head injury, intentional injury, Injury Severity Score, shock, Glasgow Coma Scale Motor Score, mechanism of injury, trauma level designation, and length of stay.
Table 4.
Adjusted Relative Risk Ratio of Discharge Location Compared with White, Privately Insured Patients (Reference Group) by Race and Insurance
| Insurance status | Race | Discharge location, RRR (95% CI) | ||
|---|---|---|---|---|
| Home health | Rehabilitation facility | Nursing facility | ||
| Private | Black | 0.84 (0.74–0.94) | 0.63 (0.56–0.71) | 1.08 (0.97–1.20) |
| Hispanic | 0.49 (0.41–0.57) | 0.45 (0.40–0.52) | 0.38 (0.32–0.44) | |
| Public | White | 1.01 (0.92–1.11) | 1.23 (1.14–1.33) | 1.86 (1.73–2.00) |
| Black | 0.62 (0.53–0.73) | 0.72 (0.63–0.82)* | 1.53 (1.36–1.71) | |
| Hispanic | 0.38 (0.29–0.50) | 0.51 (0.42–0.61) | 0.42 (0.34–0.52) | |
| Uninsured | White | 0.57 (0.52–0.63) | 0.47 (0.43–0.51) | 0.44 (0.40–0.48) |
| Black | 0.74 (0.66–0.84) | 0.27 (0.23–0.32) | 0.46 (0.40–0.53) | |
| Hispanic | 0.13 (0.10–0.17) | 0.20 (0.17–0.24) | 0.16 (0.13–0.20) | |
Multinomial logistic regression with home as reference outcome and non-Hispanic, white, privately insured patients as reference group.
indicates that result was not significant in all sensitivity analyses. White refers to Non-Hispanic white. Hispanic refers to Non-black Hispanic; n = 136,239 patients who had complete data for all variables in adjusted analysis. Variables adjusted for include: age, sex, insurance status, type of injury, extremity injury, head injury, intentional injury, Injury Severity Score, shock, Glasgow Coma Scale Motor Score, mechanism of injury, trauma level designation, and length of stay.
RRR, relative risk ratio.
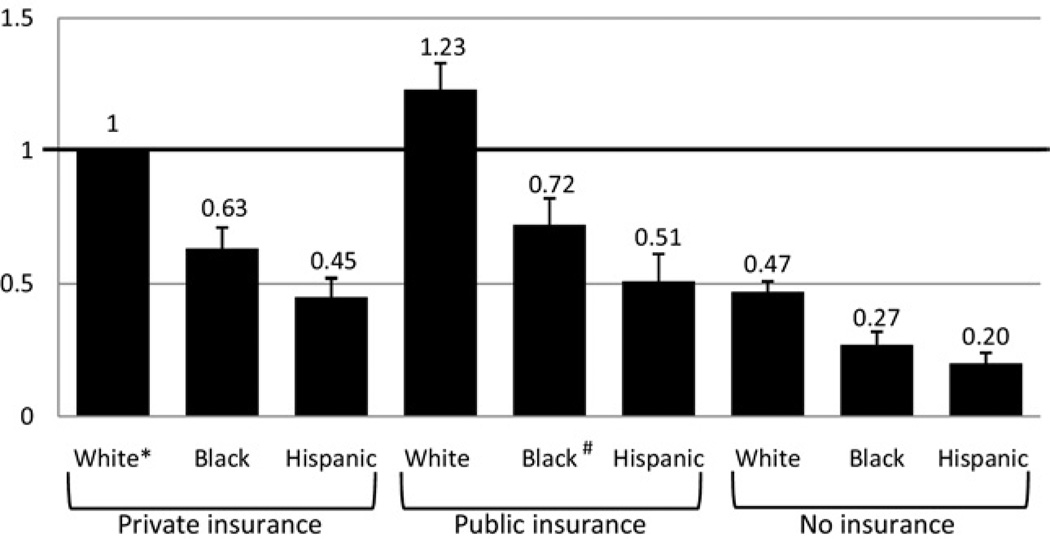
Black patients were less likely to be discharged to rehabilitation facilities than privately insured white patients, whether the black patients had private insurance (RRR 0.63, 95% CI 0.56, 0.71), public insurance (RRR 0.72, 95% CI 0.63, 0.82), or were uninsured (RRR 0.27, 95% CI 0.23, 0.32). Of note, publicly insured black patients showed similar RRRs of discharge to rehabilitation facilities compared with privately insured white patients in sensitivity analysis examining only blunt trauma with no TBI. Similarly, Hispanic patients had lower rates of rehabilitation discharges for private insurance (RRR 0.45, 95% CI 0.40, 0.52), public insurance (RRR 0.51, 95% CI 0.42, 0.61), or uninsured (RRR 0.20, 95% CI 0.17, 0.24) (Fig. 3 and Table 4).
Figure 3.
Adjusted relative risk ratio (RRR) of discharge to rehabilitation facility by race and insurance status. Multinomial logistic regression with home as reference outcome. * Reference group, non-Hispanic, white, privately insured patients. # Values that were not significant in all sensitivity analyses. Error bars represent 95% CIs. White refers to non-Hispanic white; Hispanic refers to non-black Hispanic; n = 136,239 patients who had complete data for all variables in adjusted analysis. Variables adjusted for include age, sex, type of injury, extremity injury, head injury, intentional injury, Injury Severity Score, shock, Glasgow Coma Scale Motor Score, mechanism of injury, trauma level designation, and length of stay.
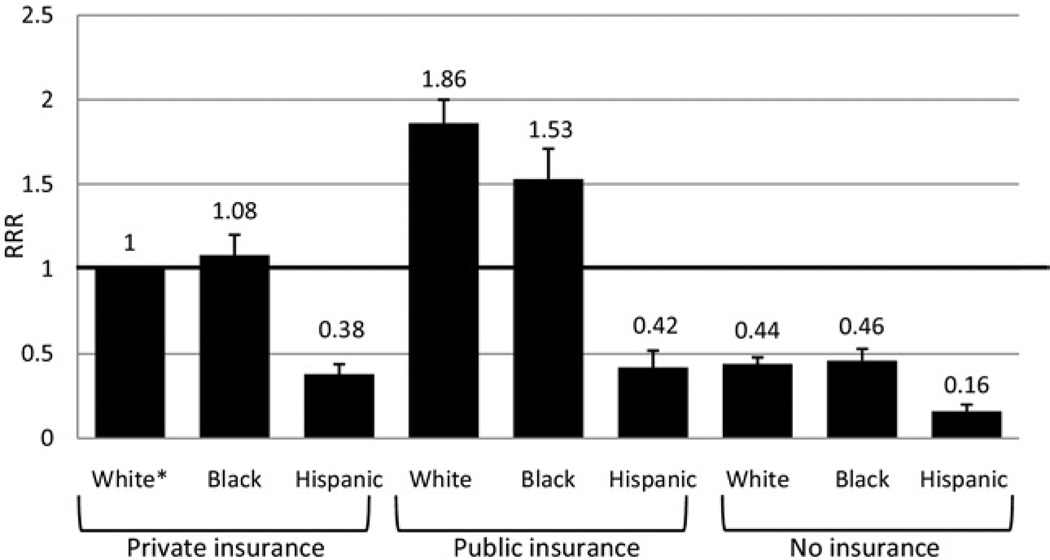
Finally, black patients showed no difference in discharge to nursing facilities compared with their white counterparts when they had private insurance (RRR 1.08, 95% CI 0.97, 1.20). Publicly insured patients were discharged to nursing homes more often than privately insured white patients, whether publicly insured black (RRR 1.53, 95% CI 1.36, 1.71) or white (RRR 1.86, 95% CI 1.73, 2.00) patients. On the other hand, Hispanics were discharged to nursing facilities less often with private (RRR 0.38, 95% CI 0.32, 0.44), public (RRR 0.42, 95% CI 0.34, 0.52), or no insurance (RRR 0.16, 95% CI 0.13, 0.20), when compared with the privately insured white reference group (Fig. 4 and Table 4).
Figure 4.
Adjusted relative risk ratio (RRR) of discharge to nursing facility by race and insurance status. Multinomial logistic regression with home as reference outcome. * Reference group, non-Hispanic, white, privately insured patients. Error bars represent 95% CIs. White refers to non-Hispanic white; Hispanic refers to non-black Hispanic; n = 136,239 patients who had complete data for all variables in adjusted analysis. Variables adjusted for include age, sex, type of injury, extremity injury, head injury, intentional injury, Injury Severity Score, shock, Glasgow Coma Scale Motor Score, mechanism of injury, trauma level designation, and length of stay.
Sensitivity analyses excluding patients with penetrating trauma and TBI demonstrated that these trends remained and no significant associations changed, except as mentioned above. Imputation of incomplete data did not demonstrate any significant quantitative or qualitative differences in the results.
DISCUSSION
Posthospitalization care is an integral part of the health care system after acute injury because it enables the critically injured to achieve their full recovery potential. This study demonstrates that race, ethnicity, and insurance status have important associations with the use of posthospitalization facilities and services. Hispanic patients are less likely to receive skilled nursing care, inpatient rehabilitation, and home health services after hospital discharge. Although black patients do not appear to universally receive fewer discharges that include posthospitalization care facilities or services, they do receive fewer discharges to inpatient rehabilitation centers. These racial disparities persist regardless of insurance status, and decreased use of these modalities is exacerbated by lack of insurance. Respectively, uninsured Hispanic and black patients are discharged to inpatient rehabilitation centers only about one-fifth to one-fourth as often as privately insured white patients. These findings are especially concerning given the considerable evidence that rehabilitation improves long-term outcomes.
Recovery after trauma affects a patient’s ability to function independently, achieve employment and productivity, and maintain an acceptable quality of life. The importance of rehabilitation services has been demonstrated across the injury spectrum, from studies of hip fractures,13 strokes,14 TBIs,15,16 and post-traumatic injury amputations.17 Evidence that rehabilitation improves long-term functional outcomes has made posthospital discharge to rehabilitation and other care facilities and services a fundamental part of the US trauma system, in order to maximize the recovery potential of the trauma population.
Hispanic patients have strikingly low rates of discharge to posthospitalization facilities and services. Even among the privately insured Hispanic population, patients access these resources only about half as often as their non-Hispanic white counterparts. Whether due to family support factors, language barriers, provider or institutional bias, fear of the medical system, or potential fear of legal repercussions due to immigration status, these lower rates of discharge to posthospitalization care may put these patients at increased risk to remain more severely handicapped than parts of the population able to access these services. Among the groups that we studied, these disparities are most worrisome among the uninsured Hispanic population. The rates of being without insurance in the Hispanic population are extremely high, with US Census Bureau estimates of 32%, or more than 14.5 million Hispanics in 2007.28 With rates of access to posthospitalization care that are only 15% to 25% of those for privately insured white patients, the health care system may be failing a huge proportion of the Hispanic population. Often at the lowest socioeconomic levels of our society and engaged in physically demanding labor, these patients may be least able to afford losing the functionality that is central to their source of income.
In order to achieve the higher rates of discharge to appropriate posthospitalization care in the Hispanic population, barriers to these services need to be explored. One major obstacle suggested by these data and is commonly noticed in clinical practice is the financial barrier, seen in the extremely low rates of discharge to these facilities in the uninsured population. Conversely, even privately insured Hispanics are suffering lower rates of access to these services, indicating that other barriers exist.
Another potential barrier is language, and optimal use of interpretive services for patient communication is a complex question. Although interpreters can play an invaluable role in bridging lingual and even cultural gaps between patients and providers, they can also hinder the patient-provider relationship when used in inappropriate circumstances. The task of assessing a patient’s comfort in communicating in a given language is not always easy; however, providers must be cognizant of this issue and ensure that dialogue occurs in the most appropriate setting. In some cases, Hispanic patients may need to be engaged in their native language at all levels of care, from physicians and nurses, to physical and occupational therapists, and even social workers and discharge planners. A clear association has been seen between language and long-term disability after injury,5 suggesting that current practices may not adequately address lingual barriers. The US trauma system may be able to achieve significant improvements by engaging patients in their native language or the language most comfortable for the patient and his support network. This practice may make the use of posthospitalization facilities less intimidating, allow improved assessment of health care needs, and provide better patient education about the importance of rehabilitation or other postdischarge care.
Although this study provides evidence that the black population does not underuse posthospitalization care to the extent of the Hispanic population after adjusting for covariates, several trends in these rates of discharge are concerning. Decreased rates of discharge to inpatient rehabilitation centers may be increasing the burden of permanent disability in this population. The relative increases in the rates of discharge to nursing facilities compared with rehabilitation facilities raise the possibility that black patients are being discharged to these facilities for care of their disabilities rather than rehabilitation to improve and overcome them. Previous discussions of racial disparities have suggested a number of potential barriers to appropriate care, including poor patient-provider relationships due to differences in race, education, and socioeconomic status.29 Perceived differences in the ability of these patients to respond to rehabilitation may also stem from patient mistrust of the medical system, leading to poor performance and improvement on inpatient exams.30 Further research needs to address the root causes of these differences so that the medical community can more appropriately engage this vulnerable population in their care after injury.
Previous studies have demonstrated that disparities exist in the discharge location of TBI patients based both on race20 and insurance status.21 To our knowledge, this analysis is the first to use a large national database to expose the combined problem of race/ethnicity and insurance status in the larger context of the general trauma population. Subset analysis demonstrates that non-TBI, blunt trauma victims—a potentially important population for rehabilitation and posthospital services—also suffer from disparities in access to postdischarge care (data not shown). Although TBI is certainly an area of established importance for rehabilitation, studies also indicate the major impact of all types of trauma on functional disability2 and the potential for improvement with rehabilitation.13,17
This study also differs from previously mentioned studies because it uses multinomial logistic regression. This technique, which has previously been applied by researchers such as Dillingham and colleagues,31 enabled examination of multiple discharge locations rather than restricting the outcomes to 2 possible dispositions. The ability to examine several discharge locations broadens the discussion of how race and insurance influence patient disposition and which types of posthospitalization care are replacing rehabilitation in disadvantaged populations. In the case of the Hispanic population, this study shows that patients are simply being discharged to home, with decreased rates of discharge to all posthospitalization facilities. In contrast, the black population shows significantly lower rates of discharge to rehabilitation; nursing home and home health discharges are relatively higher, often comparable to those in the white population. This more nuanced view of discharge locations offers insight into potential differences in posthospitalization care that may lead to disparities in long-term outcomes.
Research on the difference between inpatient and outpatient or home rehabilitation has generally found that no detectable difference exists between inpatient and home rehabilitation in settings ranging from combat related TBI,19 to cardiac rehabilitation,32 to rehabilitation after hip fracture.18 Again, black patients going to home health did not show as great a disparity as for inpatient rehabilitation; Hispanic patients continue to have extremely low rates of discharge to all forms of posthospitalization care. Comparable rates of discharge to an equivalent therapeutic modality would be reassuring, but this study cannot confirm that home health always included home rehabilitation. The decreased rates of inpatient rehabilitation discharge remain concerning as an indicator of overall discharge including rehabilitation services. On the other hand, these rates may be an indication that home health and home rehabilitation may be an important option to provide equivalent outcomes to populations that are not agreeable or appropriate for inpatient rehabilitation.
The NTDB has many weaknesses due to missing data points and the variability in data provided by some centers. Without good data on education and income, we are unable to evaluate these factors independently; however, we expect that insurance status is a surrogate for these measures, thereby lessening their influence on results stratified by insurance status. NTDB 8.0 also lacks complete data on comorbidities, which are known to affect outcomes in trauma patients. Minorities are generally considered to have poorer general health status, supported by data that show black patients have higher age-adjusted rates for 8 of the top 12 disease-related causes of mortality,33 including heart disease, malignancy, and cerebrovascular disease; therefore, these data would likely only strengthen the need for rehabilitation and other posthospitalization care for these patients.
The NTDB does not provide information on whether insurance status is recorded at the time of discharge or admission. Typically recorded from the billing sheet or admission form,34 the information is likely from hospital admission, but it is impossible to determine if some patients who remained in the hospital for an extended period received insurance during their hospitalization. There are also no data to qualify various discharge facilities; therefore, all rehabilitation facilities were treated as equal, although this simplification may be masking an important discharge distinction. Additionally, as a convenience sample, the NTDB is not necessarily representative of the entire trauma population. As expected, the study population was significantly different from the general NTDB population, with fewer publicly insured, and more patients who were male, black or Hispanic, and uninsured (data not shown). In particular, the exclusion criteria in this study make the results applicable only to patients aged 18 to 64, without burns.
The NTDB lacks data on many specifics of insurance status, and in order to simplify our analysis, this study defined broad categories of insurance. This simplification may have caused our analysis to miss nuanced associations, such as a different pattern of discharge disposition among patients with worker’s compensation as opposed to others with private insurance. Specific associations between insurance and discharge disposition may also vary by state, hospital, or provider, and this analysis is unable to examine these variations in detail. The NTDB dataset used in this analysis also lacked regional data, making this important variable unavailable for analysis.
Patient or family preference undoubtedly influenced decisions about discharge disposition. These data are unavailable in the NTDB and any data on this subject would be difficult to disentangle from previously mentioned factors such as financial, cultural, health education, and lingual barriers. Furthermore, any differences based on these factors are not necessarily an adequate explanation for these disparities, but an opportunity for improved education and communication with these groups. Research able to incorporate patient preference in this type of analysis would be invaluable in delineating the causes of these disparities and helping to demonstrate the role of provider and institutional bias on these results.
Many pitfalls exist when using large retrospective databases, particularly to compare populations with varying demographic and injury severity characteristics. Although the NTDB 8.0 has an impressive quantity of data points, the large amount of missing data is concerning. Multiple imputation has become a proven method to allow for analysis of these data while providing confidence that the missing data will not skew the conclusions.27,35 In addition, we implemented methods to control for differences in patient characteristics shown to affect outcomes in trauma as well as minimize loss of power due to missing data.25,26 Using these techniques, this article provides a sophisticated analysis of the NTDB to generate conclusions with a high level of validity.
Finally, although medical consensus and substantial evidence exist promoting the importance of posthospitalization care, particularly rehabilitation care, NTDB 8.0 has no follow-up on short- or long-term functional deficits of the patient population. This study establishes a clear association between race, ethnicity, insurance status, and use of posthospitalization care; however, it can only hypothesize about the increased functional deficits caused by this lack of access. Future studies should attempt to create a direct link between decreased access to rehabilitation facilities and deficits in functional status, employment status, and quality of life.
Disparities in access to rehabilitation facilities and other posthospitalization services exacerbate the socioeconomic inequalities that help create them. Without rehabilitation or home health care, patients may suffer poorer long-term functional outcomes, leading to worse employment and educational opportunities. The vicious cycle of disadvantaged racial and ethnic minorities and socioeconomic groups suffering from decreased access to health care services, which, in turn, led to decreased long-term potential, continues to burden a large part of the American population. This study reinforces previous work on the inequalities that exist for racial and ethnic minorities and those lacking adequate health insurance, and it expands the discussion beyond the setting of TBI to the entire population of trauma patients. The enormous burden of traumatic injury on the future functional outcomes, employment potential, and quality of life for these patients makes adequate access to posthospitalization care a vital component of any effort to improve the US trauma system and health care disparities among racial and ethnic minorities, as well as the uninsured.
Acknowledgments
Financial support for this work was provided by: National Institutes of Health/NIGMS K23GM093112-01; American College of Surgeons C James Carrico Fellowship for the Study of Trauma and Critical Care and Hopkins Center for Health Disparities Solutions (Dr Haider)
Abbreviations and Acronyms
- AIS
Abbreviated Injury Scale
- GSC-M
Glasgow Coma Scale Motor Score
- ISS
Injury Severity Score
- LOS
length of hospital stay
- NTDB
National Trauma Data Bank
- RRR
relative risk ratio
- TBI
traumatic brain injury
Footnotes
Author Contributions
Study conception and design: Englum, Cornwell, Efron, Haider
Acquisition of data: Englum, Haut, Cornwell, Efron, Haider, Villegas
Analysis and interpretation of data: Englum, Haider, Villegas
Drafting of manuscript: Englum, Haider, Villegas
Critical revision: Haut, Cornwell, Efron, Haider
Disclosure Information: Nothing to disclose.
Presented at The American College of Surgeons 96th Annual Clinical Congress, Washington, DC, October 2010.
REFERENCES
- 1.MacKenzie EJ. Epidemiology of injuries: Current trends and future challenges. Epidemiol Rev. 2000;22:112–119. doi: 10.1093/oxfordjournals.epirev.a018006. [DOI] [PubMed] [Google Scholar]
- 2.Holbrook TL, Anderson JP, Sieber WJ, et al. Outcome after major trauma: 12-month and 18-month follow-up results from the trauma recovery project. J Trauma. 1999;46:765–771. doi: 10.1097/00005373-199905000-00003. discussion 771–773. [DOI] [PubMed] [Google Scholar]
- 3.Agency for Healthcare Research and Quality. Rockville, MD: Agency for Healthcare Quality and Research; 2008. National healthcare disparities report. [Google Scholar]
- 4.Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in quality: Addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000;283:2579–2584. doi: 10.1001/jama.283.19.2579. [DOI] [PubMed] [Google Scholar]
- 5.Marquez de la Plata C, Hewlitt M, de Oliveira A, et al. Ethnic differences in rehabilitation placement and outcome after TBI. J Head Trauma Rehabil. 2007;22:113–121. doi: 10.1097/01.HTR.0000265099.29436.56. [DOI] [PubMed] [Google Scholar]
- 6.Arango-Lasprilla JC, Ketchum JM, Stevens LF, et al. Ethnicity/racial differences in employment outcomes following spinal cord injury. NeuroRehabilitation. 2009;24:37–46. doi: 10.3233/NRE-2009-0452. [DOI] [PubMed] [Google Scholar]
- 7.Haider AH, Efron DT, Haut ER, et al. Mortality in adolescent girls vs boys following traumatic shock: An analysis of the national pediatric trauma registry. Arch Surg. 2007;142:875–880. doi: 10.1001/archsurg.142.9.875. discussion 879–880. [DOI] [PubMed] [Google Scholar]
- 8.Haas JS, Goldman L. Acutely injured patients with trauma in Massachusetts: Differences in care and mortality, by insurance status. Am J Pub Health. 1994;84:1605–1608. doi: 10.2105/ajph.84.10.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Doyle JJ. Health insurance, treatment and outcomes: Using auto accidents as health shocks. Rev Econ Stat. 2005;87:256–270. [Google Scholar]
- 10.Haider AH, Chang DC, Efron DT, et al. Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143:945–949. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 11.Consensus conference. Rehabilitation of persons with traumatic brain injury. NIH Consensus Development Panel on Rehabilitation of Persons with Traumatic Brain Injury. JAMA. 1999;282:974–983. [PubMed] [Google Scholar]
- 12.Bleakley CM, O’Connor SR, Tully MA, et al. Effect of accelerated rehabilitation on function after ankle sprain: Randomised controlled trial. BMJ. 2010;340:c1964. doi: 10.1136/bmj.c1964. [DOI] [PubMed] [Google Scholar]
- 13.Binder EF, Brown M, Sinacore DR, et al. Effects of extended outpatient rehabilitation after hip fracture: A randomized controlled trial. JAMA. 2004;292:837–846. doi: 10.1001/jama.292.7.837. [DOI] [PubMed] [Google Scholar]
- 14.Kramer AM, Steiner JF, Schlenker RE, et al. Outcomes and costs after hip fracture and stroke. A comparison of rehabilitation settings. JAMA. 1997;277:396–404. [PubMed] [Google Scholar]
- 15.Hawkins ML, Lewis FD, Medeiros RS. Serious traumatic brain injury: An evaluation of functional outcomes. J Trauma. 1996;41:257–263. doi: 10.1097/00005373-199608000-00010. discussion 263–264. [DOI] [PubMed] [Google Scholar]
- 16.Whitlock JA, Jr, Hamilton BB. Functional outcome after rehabilitation for severe traumatic brain injury. Arch Phys Med Rehabil. 1995;76:1103–1112. doi: 10.1016/s0003-9993(95)80117-0. [DOI] [PubMed] [Google Scholar]
- 17.Pezzin LE, Dillingham TR, MacKenzie EJ. Rehabilitation and the long-term outcomes of persons with trauma-related amputations. Arch Phys Med Rehabil. 2000;81:292–300. doi: 10.1016/s0003-9993(00)90074-1. [DOI] [PubMed] [Google Scholar]
- 18.Crotty M, Whitehead CH, Gray S, Finucane PM. Early discharge and home rehabilitation after hip fracture achieves functional improvements: A randomized controlled trial. Clin Rehabil. 2002;16:406–413. doi: 10.1191/0269215502cr518oa. [DOI] [PubMed] [Google Scholar]
- 19.Salazar AM, Warden DL, Schwab K, et al. Cognitive rehabilitation for traumatic brain injury: A randomized trial. Defense and Veterans Head Injury Program (DVHIP) study group. JAMA. 2000;283:3075–3081. doi: 10.1001/jama.283.23.3075. [DOI] [PubMed] [Google Scholar]
- 20.Shafi S, de la Plata CM, Diaz-Arrastia R, et al. Ethnic disparities exist in trauma care. J Trauma. 2007;63:1138–1142. doi: 10.1097/TA.0b013e3181568cd4. [DOI] [PubMed] [Google Scholar]
- 21.Chan L, Doctor J, Temkin N, et al. Discharge disposition from acute care after traumatic brain injury: The effect of insurance type. Arch Phys Med Rehabil. 2001;82:1151–1154. doi: 10.1053/apmr.2001.24892. [DOI] [PubMed] [Google Scholar]
- 22.American College of Surgeons Committe on Trauma. National Trauma Data Bank (NTDB) version 8.0. 2008 [Google Scholar]
- 23.Susman M, DiRusso SM, Sullivan T, et al. Traumatic brain injury in the elderly: Increased mortality and worse functional outcome at discharge despite lower injury severity. J Trauma. 2002;53:219–223. doi: 10.1097/00005373-200208000-00004. discussion 223–224. [DOI] [PubMed] [Google Scholar]
- 24.Laveist-Ramos TA, Galarraga J, Thorpe RJ, Jr, et al. Are black Hispanics black or Hispanic? Exploring disparities at the intersection of race and ethnicity. J Epidemiol Community Health. 2011 Mar 3; doi: 10.1136/jech.2009.103879. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oyetunji T, Crompton JG, Efron DT, et al. Simplifying physiologic injury severity measurement for predicting trauma outcomes. J Surg Res. 2010;159:627–632. doi: 10.1016/j.jss.2009.08.026. [DOI] [PubMed] [Google Scholar]
- 26.Haider AH, Chang DC, Haut ER, et al. Mechanism of injury predicts patient mortality and impairment after blunt trauma. J Surg Res. 2009;153:138–142. doi: 10.1016/j.jss.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 27.Oyetunji TA, Crompton JG, Ehanire ID, et al. Multiple imputation in trauma disparity research. J Surg Res. 2011;165:e37–e41. doi: 10.1016/j.jss.2010.09.025. [DOI] [PubMed] [Google Scholar]
- 28.DeNavas-Walt C, Proctor BD, Smith JC. Income, poverty, and health insurance coverage in the United States: 2007. Washington, DC: U.S. Government Printing Office; 2008. U.S. Census Bureau, current population reports; pp. 60–235. [Google Scholar]
- 29.Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O., 2nd Defining cultural competence: A practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118:293–302. doi: 10.1016/S0033-3549(04)50253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brandon DT, Isaac LA, LaVeist TA. The legacy of Tuskegee and trust in medical care: Is Tuskegee responsible for race differences in mistrust of medical care? J Natl Med Assoc. 2005;97:951–956. [PMC free article] [PubMed] [Google Scholar]
- 31.Dillingham TR, Pezzin LE, Mackenzie EJ. Discharge destination after dysvascular lower-limb amputations. Arch Phys Med Rehabil. 2003;84:1662–1668. doi: 10.1053/s0003-9993(03)00291-0. [DOI] [PubMed] [Google Scholar]
- 32.Jolly K, Taylor R, Lip GY, et al. The Birmingham Rehabilitation Uptake Maximisation study (BRUM). Home-based compared with hospital-based cardiac rehabilitation in a multi-ethnic population: Cost-effectiveness and patient adherence. Health Technol Assess. 2007;11:1–118. doi: 10.3310/hta11350. [DOI] [PubMed] [Google Scholar]
- 33.Heron M, Hoyert DL, Murphy SL, et al. Deaths: Final data for 2006. Natl Vital Stat Rep. 2009;57:1–134. [PubMed] [Google Scholar]
- 34.American College of Surgeons Committee on Trauma. National Trauma Data Bank (NTDB) research data set admission year 2007 user manual. Chicago, IL: American College of Surgeons; 2008. [Google Scholar]
- 35.Schluter PJ, Nathens A, Neal ML, et al. Trauma and Injury Severity Score (TRISS) coefficients 2009 revision. J Trauma. 2010;68:761–770. doi: 10.1097/TA.0b013e3181d3223b. [DOI] [PubMed] [Google Scholar]