Abstract
Context
Studies involving physicians suggest that unconscious bias may be related to clinical decision making and may predict poor patient-physician interaction. The presence of unconscious race and social class bias and its association with clinical assessments or decision making among medical students is unknown.
Objective
To estimate unconscious race and social class bias among first-year medical students and investigate its relationship with assessments made during clinical vignettes.
Design, Setting, and Participants
A secure Web-based survey was administered to 211 medical students entering classes at Johns Hopkins School of Medicine, Baltimore, Maryland, in August 2009 and August 2010. The survey included the Implicit Association Test (IAT) to assess unconscious preferences, direct questions regarding students’ explicit race and social class preferences, and 8 clinical assessment vignettes focused on pain assessment, informed consent, patient reliability, and patient trust. Adjusting for student demographics, multiple logistic regression was used to determine whether responses to the vignettes were associated with unconscious race or social class preferences.
Main Outcome Measures
Association of scores on an established IAT for race and a novel IAT for social class with vignette responses.
Results
Among the 202 students who completed the survey, IAT responses were consistent with an implicit preference toward white persons among 140 students (69%, 95% CI, 61%–75%). Responses were consistent with a preference toward those in the upper class among 174 students (86%, 95% CI, 80%–90%). Assessments generally did not vary by patient race or occupation, and multivariable analyses for all vignettes found no significant relationship between implicit biases and clinical assessments. Regression coefficient for the association between pain assessment and race IAT scores was −0.49 (95% CI, −1.00 to 0.03) and for social class, the coefficient was −0.04 (95% CI, −0.50 to 0.41). Adjusted odds ratios for other vignettes ranged from 0.69 to 3.03 per unit change in IAT score, but none were statistically significant. Analysis stratified by vignette patient race or class status yielded similarly negative results. Tests for interactions between patient race or class status and student IAT D scores in predicting clinical assessments were not statistically significant.
Conclusions
The majority of first-year medical students at a single school had IAT scores consistent with implicit preference for white persons and possibly for those in the upper class. However, overall vignette-based clinical assessments were not associated with patient race or occupation, and no association existed between implicit preferences and the assessments.
Race and socioeconomic status are predictors of worse health outcomes in the United States.1 Even among trauma patients, insurance status and race are independently associated with higher mortality.2–4 Although race-based disparities have been extensively documented, the underlying mechanisms that lead to these inequalities are still not fully understood, creating a barrier to the design of effective solutions.
Disparities may be related to where patients seek care, available resources, and the types of training physicians receive. Unconscious or implicit bias among physicians has recently been suggested as another important factor contributing to racial disparities in health care.5 Implicit bias is defined as a preference for a social group that is both unconscious and automatic. It is ubiquitous in society and informed by an individual’s experiences and perceptions of others.6 Given the majority white population in the United States, an implicit preference for white persons among 68% of persons in a nonrandom US sample participating in an online study7 is not surprising. Recent work has shown that implicit biases also exist among physicians8 and are associated with perceptions and beliefs about patients,8,9 patient-physician communication,10 and possibly clinical decision making.11 Taken together, these findings suggest that the relationship between physician-level implicit bias and clinical treatment may be an important factor contributing to racial disparities in health care.
It is unknown whether medical students hold similar implicit preferences and whether they are associated with their clinical assessments. It is also unclear when in the medical career implicit bias might become related to decision making and if medical education and training mediate such an association. Further investigation of the association of implicit bias with clinical interactions and the ways in which such biases may be generated or reinforced during medical education and training may enable the design of interventions to address disparities in health care. Thus, the objectives of this study were to estimate the presence or absence of unconscious race and social class bias among first-year medical students and to investigate the association of these biases with their clinical assessments.
METHODS
This was a cross-sectional study performed on 2 cohorts of first-year medical students entering the Johns Hopkins School of Medicine, Baltimore, Maryland. The medical school’s institutional review board (IRB) and dean’s office approved the study. During medical school orientation, students were invited to participate in a confidential, Web-based survey that remained online for 48 hours beginning August 17, 2009, for the class of 2013 and August 16, 2010, for the class of 2014. The survey was nonmandatory, and participants had to accept an IRB-approved consent. Participants were not informed of the survey content beforehand, and they were asked not to disclose its contents with their peers. Two days after the survey closed, students were presented with aggregate results during a health disparities intersession and offered an optional debriefing session with the study investigators. During the results presentation, students were asked if they knew the study’s intent before or during the online survey. The same procedure was repeated in the second year of the study with the class of 2014.
Investigators and school officials were blinded to participant identities because students created a confidential, acrostic study code based on personal information. Each survey included, in order of appearance: consent page; 8 clinical vignettes designed to assess clinical assessments and decisions; the race Implicit Association Test (IAT) that assesses unconscious preference for white persons vs black persons and a novel social class IAT that examines implicit preference for members of the upper class vs the lower class; direct questions regarding explicit race and social class preferences; and student demographics, including student sex, age group, and race/ethnicity (self-classified as Asian/Pacific Islander, African American [not of Hispanic origin], Hispanic, native American/Alaskan native, or white [not of Hispanic origin]). Participant race data were collected to control for an important factor that could affect results.
The IAT measures implicit attitudes toward different social categories and has been validated in numerous contexts.12 Since its introduction in 1998,13 this computer-based reaction time test has become a widely used measure of implicit preferences.14 Implicit association tests assess unconscious attitudes by measuring the ease with which an individual sorts concepts, assuming that associated concepts will be sorted more quickly than less associated concepts. Participants classify items by rapidly pressing 1 of 2 keys. When associated concepts share the same response key, performance is faster, whereas when associated concepts have different response keys, performance is slower. The implicit preference for 1 group over another is derived from these reaction times across distinct blocks of trials.13 The race IAT presents pictures of black or white people along with good (eg, pleasure, beautiful) and bad (eg, terrible, horrible) words; the ordering of the pairings between the race categories and the good or bad categories is randomized. The speed with which an individual pairs good and bad words with either race represents his or her unconscious preferences. In addition to the race IAT, a novel social class IAT (available at http://www.traumaoutcomesresearch.com) was constructed by combining approach or avoid with upper or lower class. Approach words included near, approach, closer, toward, and avoid words included escape, avoid, away, far. Upper-class items included wealthy, well-to-do, privileged, educated and lower-class items were poor, hard-up, disadvantaged, uneducated. This social class IAT was targeted at measuring the differential association for approach and avoid words with upper- and lower-class people and is similar to the rich and poor, good and bad IAT.15 Approach and avoid words were chosen because they were successfully used in studies investigating implicit biases in the context of alcohol and substance abuse.16,17 Internal consistency of the social class IAT was checked by partitioning the trials into 2 mutually exclusive sets and determining split half correlations, which were similar or better than (r=0.82) other IATs in common use.18 However, the social class IAT has not been fully validated.
Students were administered existing measures of explicit bias for race that were also adapted for social class (eFigure, available at http://www.jama.com).7 In addition to 10-point thermometer scales assessing the coldness or warmth of their feelings toward black and white individuals, students directly expressed their preferences on a 7-point relative preference scale for one race vs the other with the midpoint representing no preference. Explicit social class preferences were assessed using parallel measures.7
To assess the relationship between unconscious bias and clinical assessments and decision making, study participants were administered 8 clinical vignettes in 4 domains: pain assessment, obtaining consent for a procedure, patient reliability, and patient trust (eAppendix available at http://www.jama.com). Students received 4 vignettes in which black or white patients were randomly alternated, with each student receiving 2 patients of each race. Similarly, 4 social class vignettes were randomly assigned, with 2 upper-class and 2 lower-class patients to each student. The race vignettes showed a picture of either a black or white patient, with a clinical scenario followed by a multiple-choice question. Photographs were balanced for age appearance and attractiveness, had neutral expressions, and had been used as IAT stimuli in previous studies.
To compare social class status, 4 clinical vignettes incorporated information on patient occupation, randomly alternating between high- and low-socioeconomic class occupations, because patient vocation is commonly used as a proxy for social class in clinical medicine. Patient occupations were chosen using the Nam-Powers occupational prestige scale, which ranks occupations on a scale from 1 to 100.19
Clinical scenarios were created by consensus of a panel comprising attending physicians, nurses, surgical residents, first-year medical students, and senior undergraduate students and were pilot tested on 13 medical student volunteers recruited from senior classes. The judgments had adequate variability without ceiling or floor effects.
To investigate the relationship between unconscious preferences and clinical assessments, the association between IAT scores and responses on clinical vignettes was determined. The IAT D scores were used because they are standardized and control for the test taker’s average response speed.20 D scores calculate the difference in reaction time between 2 critical blocks of the IAT and theoretically range from −2 to 2; however, most are less than 1 in absolute value. Scores between −0.15 and 0.15 are considered to represent no preference. Scores of 0.16 to 0.35 and 0.36 to 0.65 map to slight and moderate preference, and values greater than 0.65 in absolute value are considered to be evidence for a strong preference.18 The IAT D scores also allow the creation of a 7-point relative preference measure similar to the explicit preference scale of strong preference, moderate preference, and slight preference for either race, with no racial preference set in the middle. Correlation between this 7-point relative preference measure and IAT D scores was excellent for both social class (r=0.93, P<.001) and race (r=0.97, P<.001).21
The outcome of the pain assessment vignettes was a continuous, 1 to 10 pain score. All other vignette responses were categorized into binary outcomes to isolate response choices that could affect patient care (eg, student deciding the patient is lying about previous narcotic use). For patient trust, responses were grouped as “believes the patient or is neutral” vs “did not believe the patient.” Informed consent responses were “appropriate” vs “inappropriate.” Patient reliability responses were grouped as “reliable or neutral” vs “unreliable.”
Correlation coefficients (r) were calculated to determine the relationship between implicit and explicit biases in 2 ways. First, correlation between the 7 preference groups on the IAT with the same preference groups on explicit questions was assessed and Spearman rank-correlation coefficient was calculated, for both race and social class. Second, a composite measure of explicit bias was created by merging together results from the thermometer scales for black and white individuals (or upper- and lower-social class) and the 7-point explicit scale. For the composite explicit measures, the differences in preference temperature between groups and the 7-point relative preference measures were each transformed into a scale with a range of −1 to 1 and averaged; the composite measure ranged from −1 (highest for black preference or for lower-class preference) to 1 (highest for white preference or for upper-class preference), with 0 signifying no preference.
Bivariable analysis used 2-sided t tests for continuous variables and the χ2 test for categorical variables to determine any unadjusted relationships of patient race or social class with vignette responses or with student factors. Multivariable regression was used to determine whether student IAT D scores or patient race (or social class) were associated with patient assessments on clinical vignettes, controlling for participant age, race, class year, and sex.
To examine whether IAT D scores had a differential association with student assessments of black vs white (and upper- vs lower-class) patients, we repeated our multivariable analyses, stratifying by vignette patient race or class and tested for interactions between patient race (or class) and student IAT D scores in predicting responses to each vignette. Comparable analyses to determine the association of explicit race and social class preferences with differential responses to the clinical vignettes were also performed.
Sensitivity analyses were performed, substituting IAT D scores with the 7 relative preference groups derived from the IAT D score ranges described above. Additionally, analyses were performed in which these preference groups were further condensed into 3 categories: any preference toward whites, no racial preferences, and any preference for blacks. Similar sensitivity analyses using the social class IAT were performed. To address possible ambiguity, sensitivity analyses were performed in which in the social class patient consent vignette option c was recoded as inappropriate, and in the social class trust vignette option a was recoded as unbelievable, and option b scored as believable.
Power estimates were performed using calculation software R2.22 Due to the large variation in values and likelihood of some shared variance, an estimate ρ2 at the lower end of the range was used to calculate the required sample size (ρ2=0.10). Using 6 variables in the model (k=6), with power estimates (1–β) at 0.80 and 0.95, standard significance (β=.05), and conservative ρ2 (ρ2=0.08), the required sample size was calculated to be between 164 and 186 participants.
After completing the initial round of analyses, it was decided to repeat the multivariable regression models after stratifying by individual class years, sex, and student race. Given the smaller number of African American and Hispanic students, they were merged together as underrepresented minorities for this analysis.
Concordance or discordance between implicit and explicit preferences was also used to identify subgroups for further investigation. Participants were divided into 3 relative preference categories for implicit bias and 3 comparable categories for explicit bias (any white, none, or any black preference); those with any difference between explicit and implicit categorization were considered discordant. The same was repeated for social class groups and analyses described above performed on these individual groups as well, including the tests for interaction between vignette patient class (or race) and student IAT D scores. Finally, the group of students who reported at least some explicit racial preferences was identified, as were those with any social class preferences, and analyzed as specific subgroups as well.
All analyses were performed using STATA version 11,23 and a2-sided P<.05 was considered statistically significant.
RESULTS
Out of 241 entering medical students, 211 volunteered, yielding 202 complete surveys. Table 1 presents student demographics along with the mean IAT D scores with 95% confidence intervals for both the race and social class IAT by demographic group.
Table 1.
Participant Characteristics and Implicit Association Test D Scores for Race and Social Class
| No. (%) of Students | Mean (95% CI)
|
||
|---|---|---|---|
| Race IAT Scorea | Social Class IAT Scoreb | ||
| All students | 202 (100) | 0.32 (0.28 to 0.37) | 0.62 (0.55 to 0.67) |
|
| |||
| Age, y | |||
| ≤21 | 32 (16) | 0.39 (0.24 to 0.55) | 0.61 (0.51 to 0.71) |
|
| |||
| 22–25 | 155 (76) | 0.33 (0.26 to 0.40) | 0.64 (0.58 to 0.71) |
|
| |||
| ≥26 | 15 (8) | 0.18 (0.09 to 0.38) | 0.45 (0.28 to 0.81) |
|
| |||
| Sexc | |||
| Men | 97 (48) | 0.36 (0.28 to 0.45) | 0.62 (0.54 to 0.72) |
|
| |||
| Women | 103 (52) | 0.30 (0.22 to 0.39) | 0.62 (0.55 to 0.70) |
|
| |||
| Race/ethnicity | |||
| White | 108 (53.7) | 0.34 (0.25 to 0.42) | 0.61 (0.53 to 0.69) |
|
| |||
| Asian | 62 (30.9) | 0.43 (0.34 to 0.54) | 0.62 (0.54 to 0.72) |
|
| |||
| Black | 13 (6.4) | 0.13 (−0.14 to 0.39) | 0.84 (0.63 to 1.05) |
|
| |||
| Hispanic | 12 (5.9) | 0.22 (−0.11 to 0.54) | 0.68 (0.40 to 0.97) |
|
| |||
| Other or missing | 7 (3.2) | NAd | NAd |
|
| |||
| Class year | |||
| 2013 | 102 (51) | 0.34 (0.26 to 0.43) | 0.62 (0.55 to 0.71) |
|
| |||
| 2014 | 100 (49) | 0.31 (0.23 to 0.40) | 0.62 (0.54 to 0.70) |
Abbreviations: IAT, Implicit Association Test; NA, not available.
An IAT D score of 0.15 or lower means no preference; 0.16–0.35, slight white implicit preference; 0.36–0.65, moderate white implicit preference; and higher than 0.65, strong white implicit preference. Negative scores indicate black implicit preference with comparable interpretation of categories.
An IAT D score of 0.15 or lower means no preference; 0.16–0.35, slight upper class implicit preference; 0.36–0.65, moderate upper class implicit preference; and higher than 0.65, strong upper class implicit preference. Negative scores indicate lower class implicit preference with comparable interpretation of categories.
Two students did not report their sex.
Results for any group with fewer than 10 participants were withheld to protect student identities.
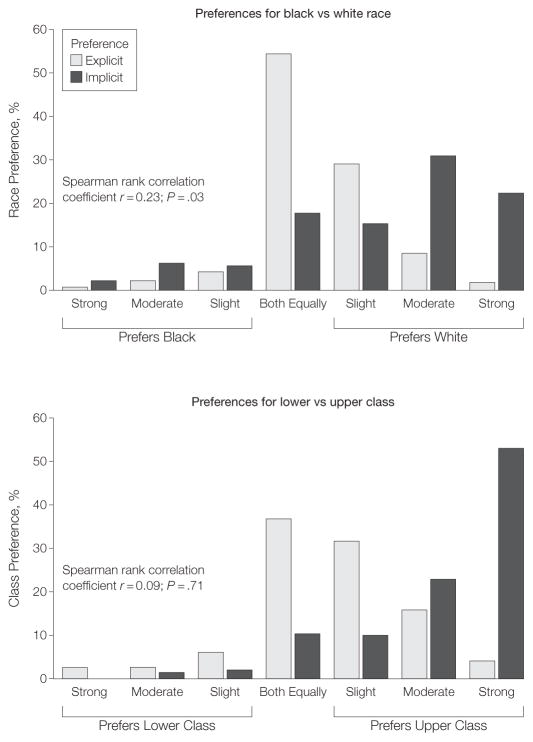
Of the 202 students, 110 (54%, 95% CI, 47%–61%) reported no explicit racial preference, whereas 78 (39%; 95% CI, 31%–45%) explicitly preferred white people and 14 (7%, 95% CI, 3%–10%) explicitly preferred black people. However, explicit race preferences were only weakly correlated with implicit preferences measured by the IAT (r =0.23, P =.03; Figure 1). Among the students, race IAT responses were consistent with no implicit preference in 34 (17%; 95% CI, 12%–22%), a white preference in 140 (69%; 95% CI, 61%–75%), and a black preference in 28 (14%, 95% CI, 9%–19%). When IAT D scores were compared with the composite measure of explicit bias, the correlation coefficient was similar (r=0.29, P=.03).
Figure 1.
Explicit and Implicit Preference for Race and Social Class
For implicit preferences, a 7-point relative preference measure derived from Implicit Association Test (IAT) D scores from 202 students was used, with no preference set in the center. Explicit preferences reflect participants’ direct response to a similar 7-point relative preference scale.
There was no significant correlation between explicit and implicit preferences according to socioeconomic class (r=0.09, P=.71; Figure 1). Of the participants, 75 (37%, 95% CI, 30%–44%) reported no social class preference, 103 (51%, 95% CI, 43%–58%) an explicit upper-class preference, and 24 (12%, 95% CI, 7%–16%) an explicit lower-class preference. However, social class IAT responses were consistent with an implicit upper-class preference in 174 (86%, 95% CI, 80%–90%), no preference in 22 (11%, 95% CI, 6%–14%), and a lower-class preference in 6 (3%, 95% CI, 1%–6%). When IAT D scores were compared with the composite measure of explicit social class bias, the correlation coefficient was low (r=0.19; P=.62).
Across all vignettes, participant responses demonstrated the expected variance in answers. However, for almost all vignettes, participant responses were not associated with the race of the patient they were randomly assigned (Figure 2). For example, in assessing patient pain on a scale of 1 to 10, participant answers ranged from 1 to 10, with a mean of 8.0 (95% CI, 7.7–8.3) for clinical vignettes with a white patient and 8.2 (95% CI, 7.9–8.3) for the same vignette with a black patient. In only 1 vignette (informed consent) was race associated with student responses. In multivariable regression analyses, patient race and student race IAT D were not significantly associated with pain ratings or other vignette responses after controlling for student race, age, sex, and graduation year (Table 2).
Figure 2.
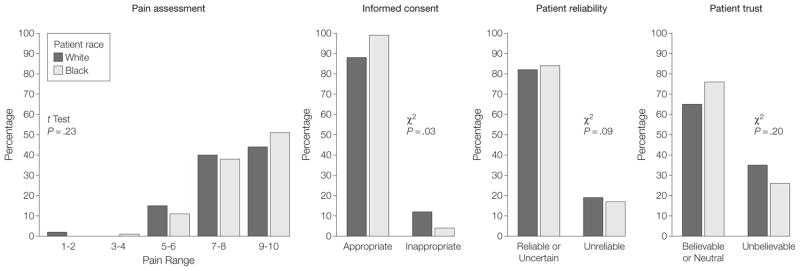
Responses to Clinical Vignettes by Patient Race
Mean pain score for white patients was 8.0 (95% CI, 7.7–8.3) and black patients 8.2 (95% CI, 7.9–8.3; P=.23). The P values, derived by the t test, compare black with white patients.
Table 2.
Multivariable Regression Models of the Associations With Medical Student Vignette Assessments (n = 196 Students in Full Models)a
| Race Vignettesb
|
||||
|---|---|---|---|---|
| Pain, Regression Coefficient (95% CI) | Consent, OR (95% CI) | Reliability, OR (95% CI) | Trust, OR (95% CI) | |
| Patient racec | 0.10 (−0.32 to 0.52) | 0.28 (0.07 to 1.07) | 0.61 (0.31 to 1.20) | 0.65 (0.33 to 1.26) |
|
| ||||
| Student characteristics | ||||
| IAT D scored | −0.49 (−1.00 to 0.03) | 1.05 (0.26 to 4.34) | 1.90 (0.84 to 4.29) | 1.21 (0.54 to 2.73) |
|
| ||||
| Sexe | −0.12 (−0.55 to 0.30) | 0.67 (0.21 to 2.16) | 0.58 (0.30 to 1.14) | 1.65 (0.84 to 3.24) |
|
| ||||
| Race/ethnicityf | ||||
| Black (n = 13) | −0.94 (−1.85 to −0.02)g | NAh | 2.35 (0.51 to 10.8) | 0.34 (0.08 to 1.44) |
|
| ||||
| Asian (n = 62) | −0.85 (−1.35 to −0.34)i | 0.69 (0.16 to 23.02) | 1.14 (0.67 to 2.08) | 0.93 (0.42 to 2.03) |
|
| ||||
| Hispanic (n = 12) | 0.62 (−0.28 to 1.51) | 1.13 (0.11 to 11.3) | 2.18 (0.51 to 9.33) | 0.16 (0.04 to .68) |
|
| ||||
| Other (n = 7)j | NA | NA | NA | NA |
|
| ||||
| Age, yk | 0.01 (−0.40 to 0.41) | 1.51 (0.57 to 4.06) | 1.46 (0.76 to 2.82) | 1.49 (0.75 to 3.00) |
|
| ||||
| Graduation yearl | −0.34 (−0.76 to 0.08) | 3.24 (0.82 to 12.7) | 1.55 (0.79 to 3.05) | 1.21 (0.54 to 2.73) |
|
| ||||
| Social Class (Occupation Vignettes)b | ||||
| Patient social classc | 0.34 (−0.13 to 0.71) | 0.49 (0.03 to 3.24) | 0.63 (0.28 to 1.41) | 0.69 (0.27 to 1.76) |
|
| ||||
| Student characteristics | ||||
| IAT D scored | −0.04 (−0.50 to 0.41) | 3.03 (0.11 to 19.4) | 1.23 (0.45 to 3.38) | 0.69 (0.22 to 2.16) |
|
| ||||
| Sexe | −0.04 (−0.41 to 0.33) | 1.05 (0.06 to 15.2) | 1.00 (0.44 to 2.28) | 0.69 (0.26 to 1.81) |
|
| ||||
| Race/ethnicityf | ||||
| Black (n = 13) | −0.24 (−1.04 to 0.56) | NAh | 0.84 (0.16 to 4.42) | 2.20 (0.39 to 12.4) |
|
| ||||
| Asian (n = 62) | −0.29 (−0.74 to 0.15) | 1.13 (0.71 to 2.1) | 1.12 (0.42 to 3.01) | 1.38 (0.45 to 4.29) |
|
| ||||
| Hispanic (n = 12) | 0.65 (0.15 to 1.45) | NAh | 0.30 (0.07 to 1.24) | 2.26 (0.39 to 13.2) |
|
| ||||
| Other (n = 7)j | NA | NA | NA | NA |
|
| ||||
| Age, yk | 0.31 (−0.06 to 0.68) | 2.97 (0.07 to 11.9) | 1.08 (0.49 to 2.39) | 1.17 (0.50 to 2.78) |
|
| ||||
| Graduation yearl | −0.34 (−0.71 to 0.04) | 0.90 (0.64 to 1.27) | 1.26 (0.56 to 2.84) | 0.92 (0.36 to 2.32) |
Abbreviations: IAT, Implicit Association Test; NA, not available; OR, odds ratio
Models for variable were adjusted for all other variables in the table.
Vignette themes and outcomes: pain measures, clinical assessment of pain (scale of 1–10); consent, whether obtaining informed consent (appropriate vs inappropriate); reliability, reliability of family or patient (reliable or uncertain vs unreliable); trust, trust of accuracy of patient history or symptoms (believable or neutral vs unbelievable). For examples of interpretation, patient race being black was associated with a nonstatistically significant increase of 0.10 in the pain score, and a 1-unit increase in race IAT D score was associated with a nonstatistically significant decrease of 0.49 in the pain score. Patient occupation classified as lower class was associated with a nonstatistically significant increase of 0.34 in the pain score, and a 1-unit increase in social class IAT D score was associated with a nonstatistically significant decrease of 0.04 in the pain score. The OR for obtaining inappropriate consent from a black patient vs a white patient was 0.28 (95% CI, 0.07–1.07), and the OR for obtaining inappropriate consent per 1-point change in the race IAT D score was 1.05 (95% CI, 0.26–4.34).
The white race and upper-class status groups are the reference for their respective categories.
The IAT D score ranges from −2 to 2.
The reference group is male.
The reference group is white.
P=.04.
The model could not run because there were too few students with varying outcomes in subgroup.
P=.002.
Results for any group with fewer than 10 participants were withheld to protect student identities.
Age converted into ordinal groups of 21 or younger, 22 to 25, older than 25 years; The 21-or-younger group was the reference group.
Reference group=2013.
In assessing patient pain, participant responses did not vary significantly according to occupation of the patient to whom they were randomly assigned (Figure 3). For an occupation associated with the upper class, the mean pain score assessed was 8.5 (95% CI, 8.2–8.7), whereas for an occupation associated with the lower class, the mean was 8.8 (95% CI, 8.5–9.1). Participants ranged in their responses to the informed consent, patient reliability, and patient trust vignettes, but there were no significant differences in response according to patient occupation. These results persisted in multivariable analyses in which, after adjustment, neither patient occupation nor student social class IAT D scores were significantly associated with any differences in assessments (Table 2).
Figure 3.
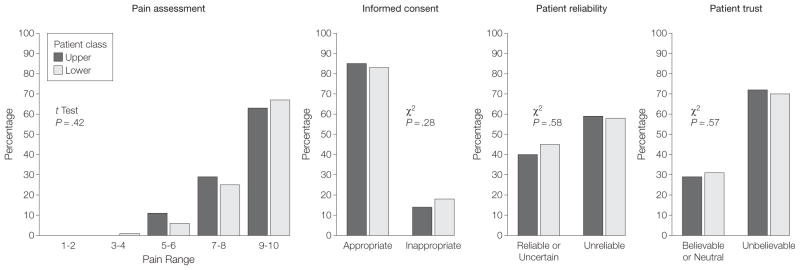
Responses to Clinical Vignettes by Patient Social Class
The mean pain score, a scale of 1 to 10, was 8.5 (95% CI, 8.2–8.7) for upper-class patients and 8.8 (95% CI, 8.5–9.1; P=.42) for lower-class patients. The P values, derived by the t test, compare upper-class with lower-class patients.
Although race and social class IAT responses consistent with implicit preference for whites and upper class occupation were prevalent among the first-year medical students, analysis stratified by patient race or class did not demonstrate any statistically significant association between student IAT D scores and how students assessed patients for any of the vignettes (Table 3). No interaction between IAT D scores and vignette patient race (or class) was found for any of the vignettes.
Table 3.
Association of Implicit Association Test Scores With Student Assessments by Vignette Patient Race or Social Class (n = 196 Students in Full Models)
| Patient Race, Odds Ratio (95% CI)a | P Valueb | ||
|---|---|---|---|
| White | Black | ||
| Pain, regression coefficientc | −0.69 (−1.52 to 0.13) | −0.35 (−1.0 to 0.36) | .43 |
| Consentc | 0.93 (0.20 to 4.20) | 0.60 (0.22 to 6.2) | .89 |
| Reliabilityc | 1.50 (0.38 to 5.80) | 2.45 (0.82 to 5.36) | .72 |
| Trustc | 1.34 (0.43 to 4.21) | 1.22 (0.35 to 4.30) | .99 |
| Patient Social Class, Odds Ratio (95% CI)a | |||
| Upper | Lower | ||
| Pain, regression coefficientc | 0.11 (−0.73 to 0.75) | −0.16 (−0.76 to 0.44) | .66 |
| Consentc | 1.65 (0.34 to 4.00) | 0.88 (0.21 to 3.77) | .49 |
| Reliabilityc | 0.93 (0.16 to 5.35) | 0.39 (0.06 to 2.67) | .92 |
| Trustc | 0.70 (0.12 to 3.90) | 0.33 (0.04 to 2.27) | .61 |
Multivariable regression model were used to determine the association between Implicit Association Test (IAT) D scores and differences in medical students assessments, stratified by patient race or social class presented in the clinical vignettes. Covariates controlled for in the model include student race, age group, sex, and class year. Effect sizes are per 1-unit increase in IAT D score. For example of interpretation, a 1-unit increase in the race IAT D score was associated with a nonstatistically significant pain score decrease of 0.69 among white patients and 0.35 among black patients. Similarly a 1-unit increase in the class IAT D score was associated with a nonstatistically significant pain score increase of 0.11 among upper-class patients and a nonsignificant decrease of 0.16 among lower-class patients.
P values are from tests of significance of interaction between patient race or social class and student IAT D scores in predicting each outcome (covariates in multivariable models included patient race or class, student race, age, sex, and class year).
Vignette themes and outcomes: pain is the clinical assessment of pain (scale of 1–10); consent, appropriately or inappropriately obtaining informed consent; reliability, whether family or patient is deemed reliable or uncertain vs unreliable; trust, accuracy of patient history or symptoms is deemed believable or neutral vs unbelievable.
Multiple sensitivity analyses and stratified analyses were performed. All of the preceding analyses, including the tests for interaction, were repeated with IAT D scores categorized as the 7 relative preference categories and again with the 3 different preference categories (preference for whites, no preference, preference for blacks; and preference for upper class, no preference, preference for lower class). However, no associations were noted between patient race or class status and vignette responses, and there were no interactions between patient race or class status and IAT scores (eTable 1, available at http://www.jama.com).
In analyses stratified by student race and sex, no differences in results were noted (eTable 2). Of the participants, 109 (54%) had a discordance between their explicit and implicit preferences as measured by the IAT, with a mean score on the race IAT of 0.29 (95% CI, 0.20–0.36), which was not significantly different from the mean of 0.38 (95% CI, 0.30–0.46) for those who had concordant implicit and explicit preferences (n=93). Multivariable regression models in the subgroup of participants who had this discordance and the subgroup with concordant preferences showed no significant associations between patient race (or class), IAT D scores, and vignette-based clinical assessments (eTable 3). In all of these subgroups, no interaction between IAT D scores and vignette patient race (or class) was found for any of the vignettes (eTables 2 and 3, available at http://www.jama.com).
Mean social class IAT scores were also not significantly different between the 115 (57%) students with discordant implicit and explicit social class preferences (IAT mean score, 0.58; 95% CI, 0.49–0.66) and those who had concordant social preferences (mean IAT score, 0.68; 95% CI, 0.61–0.75). Multivariable regression models in the subgroup of participants with such discordance and the subgroup of participants with concordance showed no significant associations. Given the degree of discordance between implicit and explicit preferences, exploratory analyses were performed restricted to only those participants who indicated they had at least some level of explicit bias. This was done for both race (n=93) and social class (n=125), and no significant associations were found (eTable 3).
Recoding responses to 2 of the social class vignettes did not result in any significant associations. The adjusted odds ratio (OR) per point change in the social class IAT score for the consent vignette with response c scored inappropriate was 0.90 (95% CI, 0.34–2.35; eAppendix). The adjusted OR for the trust vignette with response a scored as unbelievable and b scored as believable was 0.62 (95% CI, 0.32–1.22).
There were no significant associations between explicit preferences and responses on the clinical vignettes on multivariable analysis. The regression coefficient for the composite explicit race preference measure and the pain scores was −0.12 (95% CI, −1.24 to 1.00). For the associations of explicit race preferences with vignettes for race, the adjusted ORs per unit change in the composite explicit race measure were 0.21 for consent (95 CI%, 0.05–7.7), 0.62 for reliability (95% CI, 0.31–1.15), and 0.62 for trust (95% CI, 0.11–3.5). The regression coefficient for explicit social class preferences and the pain scores was −0.27 (95% CI, −1.28 to 0.73). For the associations of explicit social class preferences with the other vignettes for occupation, the adjusted ORs per unit change in the social class explicit measure were 0.99 for consent (95% CI, 0.21–4.6), 0.93 for reliability (95% CI, 0.05–5.14), and 0.90 for trust (95% CI, 0.15–5.32). Tests for interaction between the composite explicit preference measures and patient race were not statistically significant (P =.62 for pain, P =.55 for consent, P =.16 for reliability, and P =.86 for trust). Similarly, tests of interactions between explicit social class preferences and patient occupation were negative for each vignette (P = .69 for pain, P =.99 for consent, P =.41 for reliability, and P =.61 for trust).
During feedback sessions in both years, more than 90% of participants indicated that they did not know the intent of this study before accessing its Web site. Approximately 40% to 50% realized that the study may relate to race when they completed the IAT or while answering the explicit questions.
COMMENT
This study found that the majority of first-year medical students at one institution exhibited IAT scores consistent with implicit preferences toward white people and members of the upper class, as seen in 69% and 86% of participants, respectively. The implicit biases suggested by the IAT were significantly different from the participants’ stated preferences. Despite the prevalence of implicit biases among the students, these unconscious preferences were not associated with their clinical assessments as measured by 8 patient vignettes.
These findings among medical students are in contrast to emerging but inconsistent evidence suggesting that implicit biases held by physicians may lead to differences in clinical treatment. Green et al11 used clinical vignettes and the race IAT to determine whether implicit bias was associated with clinical decision making in a sample of 287 resident physicians. Vignettes depicting either black or white patients with symptoms of an acute coronary syndrome were shown to resident physicians and their decision to provide thrombolysis treatment assessed. Although physicians explicitly reported no bias, a higher IAT score was associated with a decreased likelihood of treating black patients with thrombolysis and an increased likelihood of treating white patients.
Another study by Sabin et al8 also used the IAT and found that a sample of 95 pediatricians had scores consistent with an implicit preference for adult European Americans relative to adult African Americans that was associated with perceived pediatric patient compliance. However, this study found a correlation between adult implicit bias and differences in pediatric treatment in only 1 of 4 vignette-based clinical scenarios, treatment of urinary tract infections.
Unconscious biases are normal and rooted in stereotyping, a cognitive process in which individuals use a social category to acquire, process, and recall information about people.24 This processing pattern functions unconsciously to help individuals organize complex information. The conscious reduction of automatic stereotyping requires considerable cognitive resources, and under heavy cognitive load individuals rely more heavily on stereotyping to process information.25–28 Fatigue and time pressure are cognitive load factors that burden many physicians.29 Even in situations eliciting automatic and highly trained responses (eg, physicians in trauma resuscitations), implicit attitudes may affect judgments because these attitudes are thought to form the basis for perceptions about the patient or situation at hand.30
Implicit race and social class biases held by physicians are increasingly recognized as potential factors contributing to disparities in health care.8,11 Several studies have found that physicians prescribe fewer analgesics for blacks and Hispanics in the emergency department despite similar estimates of pain.31–33 A study by Tamayo-Sarver et al34 examined emergency department physicians’ treatment of pain using clinical vignettes and found that socially desirable information increased the prescribing rates by a small but statistically significant percentage. In our study, neither race nor social class preferences had an association with medical student clinical assessments, suggesting that physician-level implicit bias could be an important intervention point to reduce disparities.
Our study raises the question of why the decision-making processes of first-year medical students do not correlate with their implicit biases in the same way that may occur among more experienced physicians. Younger students may have been more exposed to educational curricula focused on cultural competency, translating to improved awareness and management of implicit bias.35 Naive students who have not been exposed to the rigors of medical training might not be influenced by implicit preferences. It has been recommended that medical education curricula focus on integrating cross-cultural education to reduce disparities36; however, students have noted the existence of a “hidden curriculum” in which what is taught about bias in the classroom differs starkly from inhospital training experiences.37
Our study should be interpreted in light of a number of limitations. Use of computerized clinical vignettes might not fully reflect the outcomes of an in-person patient-physician encounter, although vignettes have been used in several studies investigating the role of the physician in clinical decision making.11,34 The absence of a correlation between either IAT scores or explicit preference measures and vignette-based clinical assessments in this study does not mean that there is an absence of unconscious bias in decision making.
The race IAT is well-established and has been used in a number of research studies, making it more likely that the race findings are robust. However, the social class IAT is novel; until this is further validated, the social class findings should be considered preliminary. Although the IAT design accounts for order effects by randomly presenting categories and pairings, each student underwent each IAT a single time, so that ordering may have affected the accuracy of the individual scores.
Some students may have known the study’s intent, and the similar response to black and white patients in the scenarios could reflect social desirability. Many safeguards were introduced in the study design to prevent this, including not informing students of the content of the study beforehand, presenting the clinical vignettes before the IAT, and administering the study as the first clinically oriented test at medical school.
Because of the relatively small number of students available for stratified and subset analyses (such as those with explicit biases), a type II error in these groups cannot be ruled out; in addition, student social class could not be assessed. This study was performed at a single institution, and it is possible that the demographic composition of this medical school may have led to aggregate responses not representative of all medical students. This study should be replicated at other institutions.
CONCLUSIONS
Much like the general population, a majority of medical students in this study exhibited findings consistent with an unconscious preference toward white people and upper social class. Implicit attitudes were not related to clinical assessments or decision making, in contrast to some other studies involving physicians. Further studies are needed to have a better understanding of whether implicit preferences are associated with clinical assessments and whether experiences during medical training influence social or racial bias in decision making. If this occurs, medical training could be an effective intervention point to decrease implicit biases and possibly mitigate physician-driven health care disparities.
Acknowledgments
Funding/Support: This study was supported by grant K23GM093112-01 from the National Institute of General Medical Sciences, National Institutes of Health and by the American College of Surgeons C. James Carrico Fellowship for the study of Trauma and Critical Care (Dr Haider), and grant K24HL083113 from the National Heart, Lung, and Blood Institute (Dr Cooper).
Role of the Sponsors: None of these organizations had any role in design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Online-Only Material: The eFigure, eTables 1 through 3, the eAppendix, and the Author Interview are available at http://www.jama.com.
Additional Contributions: We thank Valerie K. Scott ( Johns Hopkins Bloomberg School of Public Health, MSPH candidate) for her editorial assistance in the preparation of this article. Ms Scott received hourly compensation for her efforts.
Author Contributions: Dr Haider had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Haider, Sexton, Cooper, Efron, Swoboda, Haut, Bonds, Pronovost, Lipsett, Cornwell.
Acquisition of data: Haider, Sriram, Villegas, Bonds.
Analysis and interpretation of data: Haider, Sexton, Sriram, Cooper, Efron, Villegas, Haut, Bonds, Lipsett, Freischlag.
Drafting of the manuscript: Haider, Swoboda.
Critical revision of the manuscript for important intellectual content: Haider, Sexton, Sriram, Cooper, Efron, Villegas, Haut, Bonds, Pronovost, Lipsett, Freischlag, Cornwell.
Statistical analysis: Haider, Sexton, Sriram, Villegas, Bonds.
Obtained funding: Haider, Villegas.
Administrative, technical, or material support: Haider, Sexton, Swoboda, Lipsett.
Study supervision: Cooper, Efron, Pronovost, Lipsett, Freischlag, Cornwell.
References
- 1.Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE., III Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143(10):945–949. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 3.Haider AH, Efron DT, Haut ER, DiRusso SM, Sullivan T, Cornwell EE., III Black children experience worse clinical and functional outcomes after traumatic brain injury: an analysis of the National Pediatric Trauma Registry. J Trauma. 2007;62(5):1259–1262. doi: 10.1097/TA.0b013e31803c760e. [DOI] [PubMed] [Google Scholar]
- 4.Crompton JG, Pollack KM, Oyetunji T, et al. Racial disparities in motorcycle-related mortality: an analysis of the National Trauma Data Bank. Am J Surg. 2010;200(2):191–196. doi: 10.1016/j.amjsurg.2009.07.047. [DOI] [PubMed] [Google Scholar]
- 5.van Ryn M, Fu SS. Paved with good intentions: do public health and human service providers contribute to racial/ethnic disparities in health? Am J Public Health. 2003;93(2):248–255. doi: 10.2105/ajph.93.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dovidio JF, Gaertner SL. Aversive racism and selection decisions: 1989 and 1999. Psychol Sci. 2000;11(4):315–319. doi: 10.1111/1467-9280.00262. [DOI] [PubMed] [Google Scholar]
- 7.Nosek BA, Smyth FL, Hansen JJ, et al. Pervasiveness and correlates of implicit attitudes and stereotypes. Eur Rev Soc Psychol. 2007;18:36–88. [Google Scholar]
- 8.Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Med Care. 2008;46(7):678–685. doi: 10.1097/MLR.0b013e3181653d58. [DOI] [PubMed] [Google Scholar]
- 9.van Ryn M, Burke J. The effect of patient race and socioeconomic status on physicians’ perceptions of patients. Soc Sci Med. 2000;50(6):813–828. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- 10.Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health. 2004;94(12):2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22(9):1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the implicit association test, III: meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41. doi: 10.1037/a0015575. [DOI] [PubMed] [Google Scholar]
- 13.Greenwald AG, McGhee DE, Schwartz JL. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. 1998;74(6):1464–1480. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- 14.Nosek BA, Greenwald AG, Banaji MR. The implicit association test at age 7: a methodological and conceptual review. In: Bargh JA, editor. Automatic Processes in Social Thinking and Behavior. London, England: Psychology Press; 2007. pp. 265–292. [Google Scholar]
- 15. [Accessed May 30, 2011.];Project implicit [Web site] https://implicit.harvard.edu/implicit.
- 16.Wiers RW, Rinck M, Kordts R, Houben K, Strack F. Retraining automatic action-tendencies to approach alcohol in hazardous drinkers. Addiction. 2010;105(2):279–287. doi: 10.1111/j.1360-0443.2009.02775.x. [DOI] [PubMed] [Google Scholar]
- 17.Ostafin BD, Marlatt GA. Surfing the urge: experiential acceptance moderates the relation between automatic alcohol motivation and hazardous drinking. J Soc Clin Psychol. 2008;27(4):404–418. [Google Scholar]
- 18.Sriram N, Greenwald AG. The brief implicit association test. Exp Psychol. 2009;56(4):283–294. doi: 10.1027/1618-3169.56.4.283. [DOI] [PubMed] [Google Scholar]
- 19.Nam CB, Boyd M. Occupational status in 2000: over a century of census-based measurement. Popul Res Policy Rev. 2004;23:327–358. [Google Scholar]
- 20.Greenwald AG, Nosek BA, Banaji MR. Understanding and using the implicit association test, I: an improved scoring algorithm. J Pers Soc Psychol. 2003;85(2):197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- 21.Greenwald AG, Nosek BA, Sriram N. Consequential validity of the implicit association test: comment on Blanton and Jaccard (2006) Am Psychol. 2006;61(1):56–61. doi: 10.1037/0003-066X.61.1.56. [DOI] [PubMed] [Google Scholar]
- 22.Steiger JH, Fouladi RT. R2: A computer program for interval estimation, power calculation, and hypothesis testing for the squared multiple correlation. Behav Res Methods Instrum Comput. 1992;4:581–582. [Google Scholar]
- 23.StataCorp. Statistical Software: Release 11.0. College Station, TX: Stata Corp; 2009. [Google Scholar]
- 24.Blair IV. The malleability of automatic stereotypes and prejudice. Pers Soc Psychol Bull. 2002;6(3):242–261. [Google Scholar]
- 25.Devine PG. Stereotypes and prejudice: their automatic and controlled components. J Pers Soc Psychol. 1989;56(1):5–18. [Google Scholar]
- 26.Tversky A, Kahneman D. Judgment under uncertainty: heuristics and biases. Science. 1974;185 (4157):1124–1131. doi: 10.1126/science.185.4157.1124. [DOI] [PubMed] [Google Scholar]
- 27.Gilbert DT, Hixon JG. The trouble of thinking: activation and application of stereotypic beliefs. J Pers Soc Psychol. 1991;60(4):509–517. [Google Scholar]
- 28.MaCrae C, Milne AB, Bodenhausen GV. Stereotypes as energy-saving devices: a peek inside the cognitive toolbox. J Pers Soc Psychol. 1994;66(1):37–47. [Google Scholar]
- 29.Paas F, Van Merriënboer J. Instructional control of cognitive load in the training of complex cognitive tasks. Educ Psychol Rev. 1994;6(4):351–371. [Google Scholar]
- 30.Fiske ST. Unconscious and automatic processes in social psychology. In: Fiske ST, Gilbert DT, Lindzey G, editors. Handbook of Social Psychology. 5. Hoboken, NJ: John Wiley & Sons; 2010. pp. 237–238. [Google Scholar]
- 31.Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA. 1993;269(12):1537–1539. [PubMed] [Google Scholar]
- 32.Todd KH, Deaton C, D’Adamo AP, Goe L. Ethnicity and analgesic practice. Ann Emerg Med. 2000;35(1):11–16. doi: 10.1016/s0196-0644(00)70099-0. [DOI] [PubMed] [Google Scholar]
- 33.Tamayo-Sarver JH, Hinze SW, Cydulka RK, Baker DW. Racial and ethnic disparities in emergency department analgesic prescription. Am J Public Health. 2003;93(12):2067–2073. doi: 10.2105/ajph.93.12.2067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tamayo-Sarver JH, Dawson NV, Hinze SW, et al. The effect of race/ethnicity and desirable social characteristics on physicians’ decisions to prescribe opioid analgesics. Acad Emerg Med. 2003;10(11):1239–1248. doi: 10.1111/j.1553-2712.2003.tb00608.x. [DOI] [PubMed] [Google Scholar]
- 35.Teal CR, Shada RE, Gill AC, et al. When best intentions aren’t enough: helping medical students develop strategies for managing bias about patients. J Gen Intern Med. 2010;25(suppl 2):S115–S118. doi: 10.1007/s11606-009-1243-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Betancourt JR. Eliminating racial and ethnic disparities in health care: what is the role of academic medicine? Acad Med. 2006;81(9):788–792. doi: 10.1097/00001888-200609000-00004. [DOI] [PubMed] [Google Scholar]
- 37.Thompson BM, Haidet P, Casanova R, et al. Medical students’ perceptions of their teachers’ and their own cultural competency: implications for education. J Gen Intern Med. 2010;25(suppl 2):S91–S94. doi: 10.1007/s11606-009-1245-9. [DOI] [PMC free article] [PubMed] [Google Scholar]