Abstract
As a first step in conducting studies of airborne influenza transmission, we compared the collection performance of an SKC Biosampler, a compact cascade impactor (CCI), Teflon filters, and gelatin filters by collecting aerosolized influenza virus in a one-pass aerosol chamber. Influenza virus infectivity was determined using a fluorescent focus assay and influenza virus nucleic acid (originating from viable and non-viable viruses) was measured using quantitative PCR. The results showed that the SKC Biosampler recovered and preserved influenza virus infectivity much better than the other samplers – the CCI, Teflon, and gelatin filters recovered only 7–22% of infectious viruses compared with the Biosampler. Total virus collection was not significantly different among the SKC Biosampler, the gelatin, and Teflon filters, but was significantly lower in the CCI. Results from this study show that a new sampler is needed for virus aerosol sampling, as commercially available samplers do not efficiently collect and conserve virus infectivity. Applications for a new sampler include studies of airborne disease transmission and bioterrorism monitoring. Design parameters for a new sampler include high collection efficiency for fine particles and liquid sampling media to preserve infectivity.
Keywords: Influenza, Air sampler, Biosampler, Compact Cascade Impactor, Teflon filter, Gelatin filter
Introduction
Human respiratory viruses are difficult to collect from the airborne environment because of their small size and low concentration. Most of the bioaerosol samplers available are not sui for the collection of viruses (Sattar and Ijaz, 2002). Samplers typically run for short periods of time (min), making it difficult to capture large volumes or integrate sample collection over time. Most samplers do not separate particles by size and are inefficient at collecting submicron particles. The ease with which collected particles can be removed from the collection media and their suitability for various assays are additional important factors.
Few researchers have detected airborne respiratory viruses in the field, and even fewer have demonstrated infectiousness of viruses sampled from air. Measuring infectious virus from air samples is logistically difficult, as it requires infecting a host cell after collection. Methods such as immunoassays and PCR are logistically less rigorous but measure virus components, which may or may not be associated with infectious virus. In the field, airborne infectious viruses detected include Coxsackievirus (Couch et al., 1970), adenovirus (Artenstein and Miller, 1966), parainfluenza virus (Artenstein and Cadigan, 1964), and smallpox (Thomas, 1974). In these studies virus infectivity was determined using traditional cell culture techniques. Airborne viruses that have been detected in office environments and hospital rooms using standard PCR assays include influenza (Blachere et al., 2009), rhinovirus (Myatt et al., 2004), respiratory syncytial virus (Aintablian et al., 1998), Varicella-zoster virus (Sawyer et al., 1994), cytomegalovirus, and SARS (Booth et al., 2005). Viruses detected via PCR from exhaled breath samples include influenza (Fabian et al., 2008), human rhinovirus and parainfluenza (Huynh et al., 2008).
The purpose of this study was to compare the performance of four commercial air samplers in collecting both infectious and total airborne influenza virus. The four samplers were: Teflon filters, gelatin filters, the SKC Biosampler, and the compact cascade impactor (CCI). The SKC Biosampler has been used previously in bioaerosol field studies (Fabian et al., 2005; Farnsworth et al., 2006) and has a collection efficiency of 79% for particles larger than 0.3 µm and 100% for particles larger than 2 µm (Willeke et al., 1998). The Teflon filter is over 99% efficient in capturing particles larger than 0.3 µm (Burton et al., 2007; Pall Corporation, 2007) and has been used to collect airborne rhinovirus in the field (Myatt et al., 2004). The gelatin filter was selected because it can be completely dissolved in water, minimizing media extraction losses. The gelatin filter captures over 99.9% of T3 phages and is easy to extract via dissolution in water (Sartorius, 2007). The CCI impactor was selected because of its novel sampling media, the polyurethane foam (PUF), whose properties include minimal particle bounce and high loading capacity (Kavouras and Koutrakis, 2001; Lee et al., 2005). The CCI captures 100% of particles larger than 1 µm and 20% of particles <0.1 µm (Demokritou et al., 2004).
Materials and methods
Virus
Influenza A/PR8/34 (H1N1) virus was obtained from Advanced Biotechnologies Incorporated (Columbia, MD, USA) with a titer of 1.9 × 1011 virus particles/ml measured by electron microscopy. Virus was diluted 10−1 in phosphate buffered saline with Calcium and Magnesium (PBS++) and 0.1% bovine serum albumin (HyClone, Logan, UT, USA) and stored at −80°C in 50 µl single-use aliquots.
Bioaerosol samplers
The four aerosol samplers tested were: SKC Biosampler impinger (Eighty Four, PA, USA), a 37 mm cassette (Pall Life Sciences, East Hills, NY, USA) with a Teflon filter (Pall Life Sciences), a 37 mm cassette with a gelatin filter (Sartorius, Goettingen, Germany), and a CCI (Demokritou et al., 2004).
The Biosampler was filled with 20 ml of PBS++. Two Biosamplers were run in parallel at a sampling airflow of 12.5 lpm each, providing an airflow of 25 lpm through the chamber. This minimized temperature and relative humidity fluctuations while sampling with the Biosamplers compared to sampling with the filters and CCI, which required an airflow of 30 lpm each.
Three-piece filter cassettes were constructed with either 37-mm 2-µm pore Teflon filters or 37-mm 3-µm pore gelatin filters as substrate. Backing pads (Pall Life Sciences) provided filter support and in the case of gelatin filters a ring made from the backing pad material was added as a spacer to prevent damage to the filter.
Polyurethane foam (Merryweather Foam, Barberton, OH, USA) was sized for the last stage of the CCI impactor (d50 = 0.16 µm), cut in rectangles 0.64 × 6.4 cm (Demokritou et al., 2004). Based on results from preliminary PUF spike experiments recovering infectious influenza virus (data not shown), PUF was prepared by: (i) washing [sonicating four times for 15 min in cell-grade water (Hyclone)], and (ii) coating with BSA. Coating was applied by soaking each PUF piece in 1.5 ml of 0.1% BSA, draining the excess liquid and drying overnight. PUF pieces were stored over desiccant until used.
Infectious virus quantification
Influenza virus infectivity assays were performed on Madin-Darby Canine Kidney Cells (MDCK) (CCL-34; ATCC, Manassas, VA, USA) grown in Dulbecco’s Modification of Eagle’s Medium with glucose and l-glutamine (DMEM) (Mediatech, Herndon, VA, USA) with 10% heat-inactivated fetal bovine serum (Hyclone). Cell monolayers were grown to confluency in 96-well plates by inoculating wells with 100 µl of 5 × 105 cells/ml and incubating overnight at 37°C, 95% air and 5% CO2. We used the fluorescent focus reduction assay described by Hartshorn et al. (2007), optimized for our application. Briefly, triplicate wells of MDCK monolayers were infected with 50 µl of influenza virus dilutions for 45 min at 37°C and 5% CO2. Cells were then washed with DMEM containing 0.1% bovine serum albumin (SeraCare Life Sciences, West Bridgewater, MA, USA) and incubated for 6–7 h. After the incubation medium was removed, cells were washed three times with 100 µl PBS++ and fixed with 50 µl of 80% acetone for 10 min at 4°C. Next, wells were washed with 100 µl of PBS++ and conditioned for 10 min in 100 µl of Reagent A (phosphate buffered saline with 0.1% bovine serum albumin, 0.02% sodium azide and 1% human serum, buffered to a pH 7.4). Cells were then stained with 50 µl of 1% of mouse monoclonal antibody A-1 – diluted in Reagent A – directed against influenza virus nucleoprotein (Influenza Division, CDC, Atlanta, GA, USA) and incubated at 4°C for 30 min. After incubation cells were washed three times with 100 µl of Reagent A, stained with 50 µl of 1% FITC-labeled goat anti-mouse IgG (Jackson ImmunoResearch Laboratories, Inc., West Grove, PA, USA) and incubated for 30 min at 4°C. The resulting fluorescent foci were counted at 200× magnification under a CKX41 Olympus inverted epifluorescent microscope (Center Valley, PA, USA). Ten standard fields were counted per well, corresponding to 30% of the well area.
Total virus quantification
Influenza virus RNA was extracted, reverse transcribed, and quantified as described previously (Fabian et al., 2009). Briefly, RNA was extracted from 400 µl of each sampler media using a Trizol–chloroform based method modified from a protocol developed for extraction of nasal swab and lavage samples (Lee et al., 2007). RNA was suspended in 20 µl of nuclease-free water (Promega, Fitchburg, WI, USA) and immediately converted to cDNA. Unused RNA was stored at −80°C. A 10 µl aliquot of 10−3 dilution of influenza virus stock (1.9 × 109 virus particles/ml) was included in each extracted batch as positive control. cDNA was synthesized using a High Capacity cDNA Reverse Transcription Kit (Applied Biosystems), yielding 20 µl of CDNA. Quantitative PCR was performed using an Applied Biosystems Prism 7500 detection system (Foster City, CA, USA) with the following primers and probe (van Elden et al., 2001): two forward primers 5’-GGA CTG CAG CGT AGA CGC TT-3’ and 5’-CAT CCT GTT GTA TAT GAG GCC CAT-3’ reverse primer 5’-CAT CT GTT GTA TAT GAG GCC CAT-3’ and probe 5’-FAM-CTC AGT TAT TCT GCT GGT GCA CTT GCC A-3’ TAMRA. The limit of quantification for the qPCR was six influenza A viral RNA particles per PCR well, with all three replicates crossing the qPCR fluorescence threshold within 40 cycles. Aliquots of RNA and cDNA of known concentrations were used in every reverse transcription and qPCR run as positive controls. The standard curve used for qPCR had at least six 1:10 dilutions and provided information on intra assay variation.
Bench top virus spike recovery experiments
We initially tested recovery with bench top virus spike recovery experiments conducted for each type of sampler media. Duplicate pieces of each media (PUF, Teflon, and gelatin filters) and 20-ml PBS++ were spiked with 20 × 5 µl droplets of a 10−2 dilution of influenza virus stock (1.9 × 109 virus particles/ml) and dried for 60–90 min. The ‘no media’ positive controls were two 100 µl aliquots of virus spiked into 1.4 ml of PBS++, the volume used to extract virus from the PUF, Teflon, and gelatin filters. The Teflon filters were initially treated with 10 µl of methanol prior to spiking with virus to reduce the hydrophobic properties of the Teflon filter and allow the virus to dry on the surface.
Subsequently, a second experiment was conducted to compare influenza virus recovery from methanol-treated and untreated Teflon filters. Duplicate Teflon filters were spiked with 20 × 5 µl droplets of a 10−2 dilution of influenza virus stock (1.9 × 109 virus particles/ml) and dried for 60–90 min. The ‘no media’ positive controls were two 100 µl aliquots of virus spiked into 1.4 ml of PBS++
To extract viruses, PUF pieces were placed in a 2.0 ml LoBind Eppendorf tube containing 1.5 ml of PBS++. Samples were vortexed for 15 s and the supernatant decanted into a new 1.7 ml tube. Gelatin filters were placed in 50 ml polypropylene centrifuge tubes containing 1.5 ml of PBS++ . Samples were briefly vortexed, incubated at 37°C for 5 min and the dissolved gelatin transferred to a clean 1.7 ml Eppendorf tube. The ring around the Teflon filters was cut and the filters placed in a 50 ml polypropylene tube containing 1.5 ml of PBS++ . Samples were vortexed for 15 s and the liquid transferred to a clean 1.7 ml Eppendorf tube. The PBS++ in the SKC Biosampler was vortexed for 15 s and 1.5 ml transferred to a 1.7 ml Eppendorf tube. Samples were assayed via the infectivity focus assay and quantitative PCR as described above. Blanks were included in each assay. For comparison, results were reported as virus focus forming units (FFU) or virus RNA particles (VP) per milliliter of original virus stock.
One-pass aerosol chamber
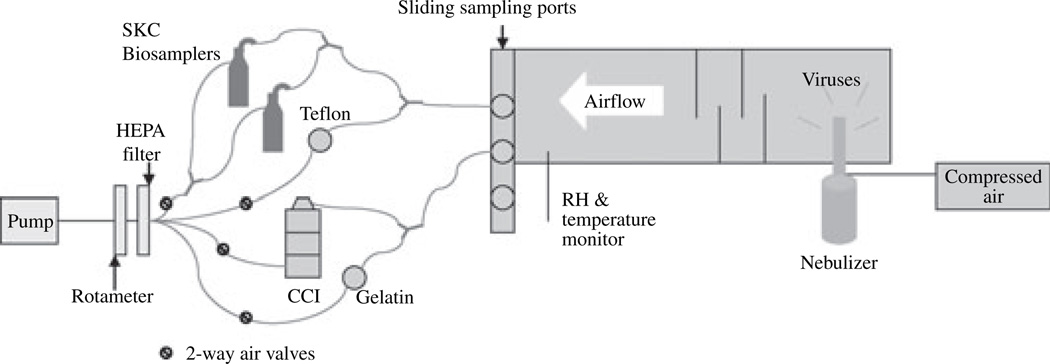
Figure 1 presents a schematic of the one-pass experimental chamber used to aerosolize and collect influenza viruses. The system was designed to study microorganism susceptibility to ultraviolet light and has been previously used in studies of Serratia marcescens, bacilli Calmette-Guerin (Ko et al., 2000; Lai et al., 2004) and vaccinia virus (Mcdevitt et al., 2007). The chamber was housed inside a type IIA biosafety cabinet and consisted of two areas: (i) aerosol generation and drying and (ii) sampling. The first area contained a 6-jet Collison nebulizer (model CN-25, BGI; Waltham, MA, USA) running at 20 psig (Gussman, 2007; May, 1973). The liquid in the nebulizer contained 24.75 ml PBS, 24.75 ml water, 1 ml of 10−2 diluted influenza virus stock, 5 µl of antifoam A, and 0.1% BSA. Aerosols were released from the nebulizer into a diffuser and passed through baffles, which allowed for mixing and drying of the aerosol before being introduced to the sampling area. A relative humidity and temperature probe was located at the end of the drying chamber and continuously monitored environmental conditions. The second area included the four bioaerosol samplers, a magnahelix to monitor the pressure drop through the system, an air bypass, a rotameter for monitoring flowrate, and a HEPA filter equipped pump. The rotameter was calibrated against a 30 lpm Gilian Gilibrator (Sensidyne, Clearwater, FL, USA). A Medo vacuum pump (model VP0935A; Medo USA, Hanover Park, IL, USA) maintained an airflow rate of 25 or 30 lpm through the chamber depending on the sampler demand. The samplers were connected to four ports via a series of Y connectors and tubing to collect serial samples without interrupting the airflow through the chamber. All air was exhausted through the HEPA filter into the biohood.
Fig. 1.
Diagram of the one-pass experimental system used to aerosolize and collect influenza viruses
Experimental protocol
Duplicate aerosol detection experiments were carried out. Airflow through the system was maintained at 30 lpm for 15 min prior to sampling. The nebulizer was pressurized with air at 20 psig and pressure monitored every 5 min. The nebulizer was started 10 min prior to sampling to equilibrate the virus concentrations in the chamber. Airborne VPs were collected for 5 min for each sampler in a continuous manner. Samples were collected first with the SKC, then the Teflon filter, the CCI, and the gelatin filter and so on in the same order until triplicate samples for each biosampler had been collected. Initial and final airflows, initial and final pressure drop across the system, relative humidity and temperature were recorded for each sample. As a result of slight decreases (<10%) in airflow because of filter loading of gelatin and Teflon filters, initial and final airflows were used to calculate the average collected air volume for each sample. Collected samples were stored at 4°C until the end of the experiment, then immediately assayed via focus assay and stored at −80°C until assayed by qPCR. Samples collected with each aerosol sampler, nebulizer liquid pre- and post-experiment, virus stock, and field blanks were analyzed with the fluorescent focus reduction assay and by qPCR as described above.
Statistical analysis
The Proc MIXED procedure in the SAS System for Windows 9.13 (Cary, NC, USA) was used to build regression models where the dependent variable was the log of the influenza virus concentration (infectious or total virus RNA particles per liter of air) and the covariates were the experiment number, type of sampler, and time. Experiment number controlled for differences in initial nebulizer concentration between the two experiments. The linear effect of time accounted for increases in nebulizer output over the 70 min experiment. A random effect of sample was included to control for correlation among the triplicate focus assay and qPCR wells. Proc GLM was used to build ANOVA models to model bench top spike recovery experiment results.
Results
Bench top virus spike recovery experiments
Compared with the ‘no media’ control, infectious virus recovery as determined by the focus assay was 23% from the gelatin filter (P = 0.0005), 24% from the PUF (P = 0.0004), 130% from the SKC Biosampler (20-ml PBS++ ) (P-value = 0.16), and 0.5% from the Teflon (P = 0.0001). Infectious recovery from the PUF, Teflon, and gelatin filters was significantly lower compared with the positive controls, recovery from the SKC Biosampler was not significantly different from the positive controls.
Total virus collection as determined by qPCR was 131% from the gelatin filter (P = 0.2), 21% from the methanol-treated Teflon filter (P = 0.0006), 69% from the PUF (P = 0.2), and 67% from the PBS++ (P = 0.1). Only total virus concentrations extracted from the Teflon filter were significantly lower than the positive control.
Subsequently, another spike experiment was conducted to compare virus recovery from Teflon filters treated with methanol to untreated Teflon filters. The results showed that infectious virus recovery from the untreated Teflon filters was 69% compared with 0.5% from treated filters and total VP recovery from the untreated Teflon filters was 68% compared with 33% from the treated filters.
Measured virus concentrations were used to calculate a ratio of total virus RNA particles to infectious VPs (T/I). The T/I ratio in the SKC Biosampler was the same as the positive control. The gelatin filter and PUF T/I ratios were approximately one order of magnitude higher and the Teflon filter T/I ratio was two orders of magnitude higher than the positive control ratio.
Influenza virus aerosol detection experiments
A total of six replicate samples were collected for each type of sampler over the course of two aerosol detection experiments. The average relative humidity was 55 ± 6% in the initial experiment and 50 ± 6% in the subsequent experiment. Temperature remained constant at 25°C ± 0.5°C during both experiments.
The nebulizer was operated for a total of 70 min and nebulizer liquid decreased from 50 ml to 30 ml and 24 ml in the first and second experiments respectively. Preliminary aerosol detection experiments showed that nebulizer output increased linearly over time, although the change was not significantly different in the first 70 min (data not shown). We assayed the contents of the nebulizer before and after sampling to ascertain the effect to the nebulization on virus concentration and viability. The ratio of total to infectious (T/I) VPs was calculated by dividing the qPCR results by the focus assay results. The nebulizer T/I ratio of VPs to infectious foci for experiment A was 200 RNA particles/FFU at the beginning of the experiment and 240 RNA particles/FFU at the end of the experiment. In experiment B the nebulizer T/I ratio increased from 340 to 380 RNA particles/FFU. Although results indicated a slight increase in infectious and total virus nebulizer concentrations over the course of the aerosol experiment, only in the second aerosol experiment were total virus concentrations significantly higher (P < 0.05).
Table 1 presents the results of the focus assay and RT-qPCR for each aerosol experiment comparing the number of infectious and total influenza virus concentrations collected by all four samplers. The average T/I ratio calculated for the viruses collected with the SKC Biosampler was similar to the T/I ratio of the nebulizer liquid, indicating that there is little or no loss of virus infectivity from the time the virus was aerosolized to when it was collected by the sampler. The average T/I ratios of the viruses measured from the CCI-PUF, gelatin filter, and Teflon filter were significantly higher than the T/I ratio of the nebulizer liquid. The last column compared the infectiousness of the virus recovered from the sampler to that observed in the nebulizer where infectiousness is the reciprocal of particles per FFU. This column shows that the SKC Biosampler and nebulizer fluid were similarly infectious, while the CCI, gelatin filter, and Teflon filter samples were less infectious than the nebulizer liquid.
Table 1.
Infectious and total influenza virus concentrations collected from aerosol samplers, determined by culture and quantitative PCR
| Sampler | Infectious concentration – (FFU/la) (s.d.c) |
Total virus concentration – (VP/lb) (s.d.c) |
Total to infectious (T/I) ratio (VP/FFU) |
% of nebulizer infectiousnessd |
|---|---|---|---|---|
| Experiment 1 | ||||
| Gelatin filter | 45 (18) | 8.9 × 104 (1.7 × 104) | 2.0 × 103 | 11 |
| Compact cascade impactor (PUF) | 34 (17) | 4.6 × 104 (1.1 × 104) | 1.4 × 103 | 16 |
| SKC Biosampler | 5.5 × 102 (3.8 × 102) | 1.6 × 104 (1.8 × 104) | 2.9 × 102 | 75 |
| Teflon filter | 62 (24) | 8.8 × 104 (1.2 × 104) | 1.4 × 103 | 15 |
| Experiment 2 | ||||
| Gelatin filter | 53 (24) | 9.7 × 104 (1.8 × 104) | 1.8 × 103 | 19 |
| Compact cascade impactor (PUF) | 38 (19) | 4.7 × 104 (5.5 × 103) | 1.2 × 103 | 29 |
| SKC Biosampler | 4.1 × 102 (3.4 × 102) | 1.3 × 105 (2.5 × 104) | 3.2 × 102 | 110 |
| Teflon filter | 1.8 × 102 (58) | 1.5 × 105 (3.7 × 104) | 8.3 × 102 | 43 |
Results are reported as infectious influenza virus particles per liter of collected air.
Results are reported as influenza virus RNA particles per liter of collected air.
s.d. = standard deviation (n = 9 [3 samples × 3 wells/sample]).
% of nebulizer infectiousness was estimated to determine viral viability loss through the aerosol system and in the samplers. It was calculated by dividing the average nebulizer total to infectious virus particle ratio (T/I) by the T/I ratio of each sampler.
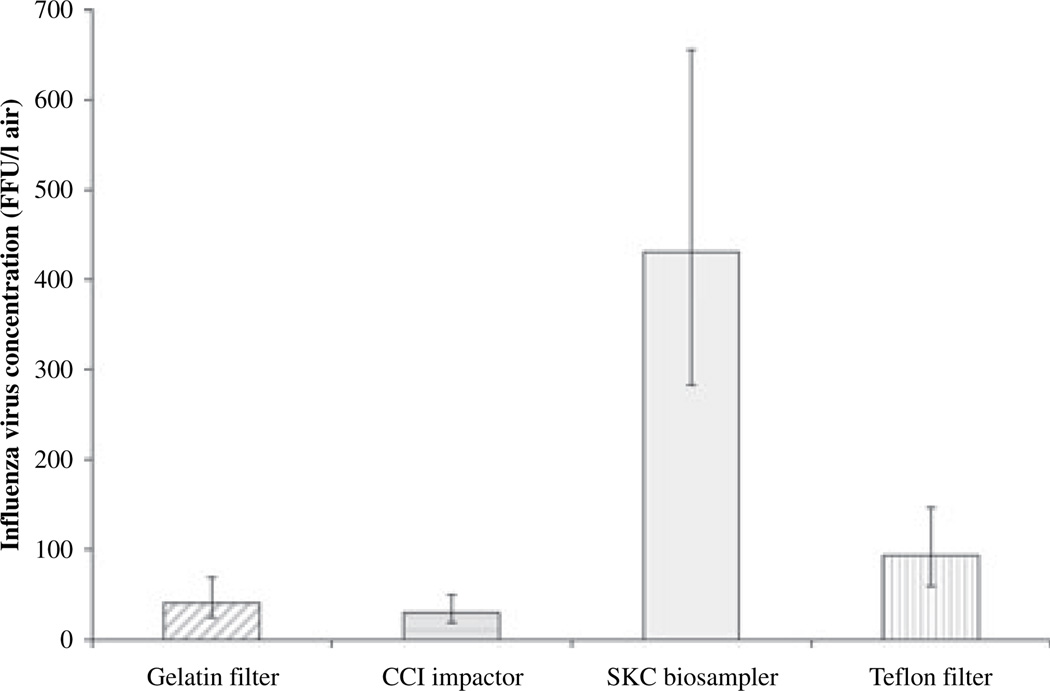
Figure 2 shows the infectious VP concentrations collected by all four samplers, estimated from the regression models integrating results from both aerosol experiments and relevant covariates. Infectious particle counts ranged between 34 and 550 FFU per liter of air. The SKC Biosampler had the highest recovery of infectious VPs, collecting on average 430 FFU/l air. Infectious VPs assayed from the gelatin filter, CCI impactor, and Teflon filter were 10, 7, and 22%, respectively of the number assayed from the SKC Biosampler. The differences were statistically significant at the 0.05 level.
Fig. 2.
Infectious influenza virus recovered from aerosol samplers, quantified by culture (n = 18 [3 samples × 2 experiments × 3 wells]). Mean concentrations estimated from mixed regression model and controlled for experiment number, time and correlation among focus assay wells. Error bars indicate 95% confidence intervals.
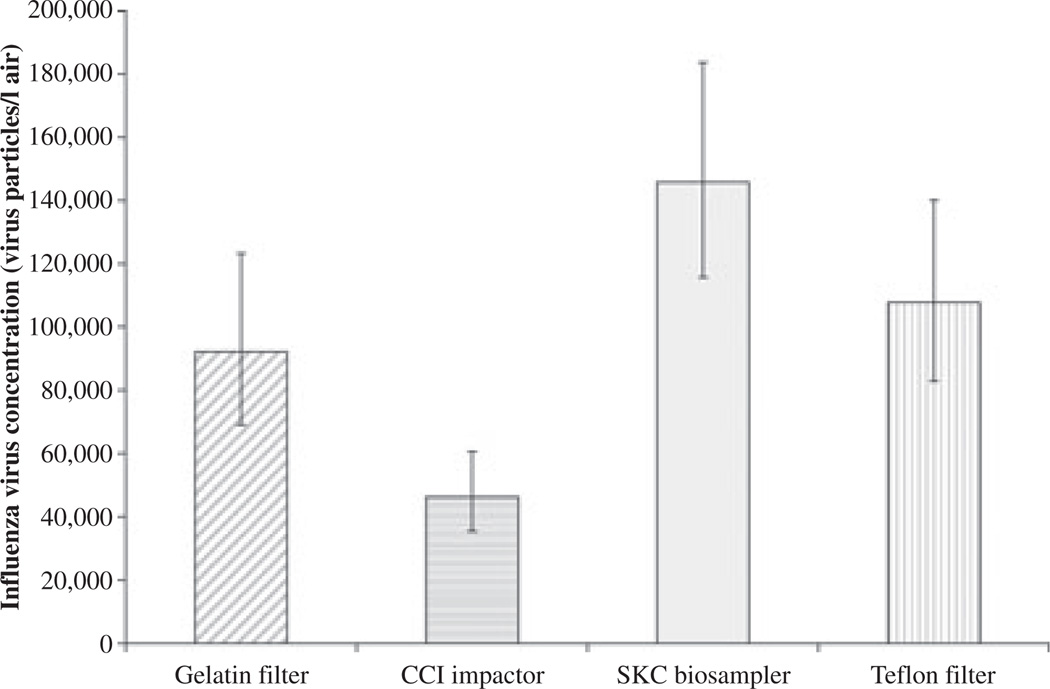
Figure 3 presents total virus concentrations collected by the four aerosol samplers estimated from the regression models integrating results from both aerosol experiments and relevant covariates. Total virus concentrations ranged between 4.4 × 104 and 1.6 × 105 RNA VPs per liter of air. Sampler efficiency followed the same order as the infectious particle collection: the SKC Biosampler had the highest total VP recovery, with an average of 1.5 × 105 RNA VPs per liter of air. Recovery from the gelatin filter, CCI, and Teflon filter was 63, 32, and 74%, respectively of the SKC Biosampler total, although only the CCI recovery was significantly lower than the Biosampler at the 0.05 level.
Fig. 3.
Total influenza virus RNA measured from aerosol samplers, quantified by qPCR (n = 18 [3 samples × 2 experiments × 3 wells]). Mean concentrations estimated from a mixed regression model and controlled for experiment number, time and correlation among focus assay wells. Error bars indicate 95% confidence intervals.
Discussion
The SKC Biosampler recovered infectious virus much more effectively from aerosols than did the CCI, Teflon, and gelatin filters showing that infectiousness is only preserved in liquid collection media (PBS). Recovery of infectious virus from the dry media was much better in the bench top spiking experiments than in the aerosol experiments. This implies that drying of the aerosol on the dry surfaces with continued airflow, rather than an intrinsic property of the dry media, was responsible for the loss of infectiousness. These results show that, for studies where it is important to determine the infectiousness of viruses, only liquid collection media can be used. Other than in the smallpox study, which used a plate coated with sucrose, glycerol, and bovine serum albumin (Thomas, 1974), the few field studies that have cultured infectious viruses from air samples also used water or buffer as their collection medium (Artenstein and Cadigan, 1964; Artenstein and Miller, 1966; Couch et al., 1970). In laboratory studies airborne infectious influenza virus has been collected with personal biosamplers with virus maintenance fluid (Agranovski et al., 2004) and all-glass impingers filled with buffer (Harper, 1961; Schaffer et al., 1976). Two recent field studies isolated influenza virus RNA from the air– from hospital rooms (Blachere et al., 2009) and from exhaled breath (Fabian et al., 2008); both studies used ‘dry’ media, filters and cyclones that do not conserve virus infectivity.
Total virus (influenza RNA) collection was similar for the SKC Biosampler, Teflon, and gelatin filters but significantly lower with the CCI impactor. Based on the collection efficiency specifications of each sampler, we expected the Biosampler to recover the lowest virus concentrations. The SKC Biosampler has a 96% collection efficiency for particles 1 µm and larger compared with the >99.99% efficiency of the CCI, gelatin, and Teflon filters for the same size particles (Demokritou et al., 2004; Pall Corporation, 2007; Sartorius, 2007; Willeke et al., 1998). The Biosampler’s efficiency declines as particle size decreases, dropping to 79% for particles of 0.3 µm diameter. However, the Collison nebulizer generates droplets with a 2 µm mass median diameter, which then dry to smaller particle sizes depending on the composition of the nebulizer liquid (Gussman, 2007; May, 1973). VPs are so small that they do not affect particle size output of the nebulizer (Hogan et al., 2005) but the nebulizer media does. A previous study of aerosolized S. marcescens found that nebulizing the bacteria in synthetic respiratory fluid (phosphate buffered saline + 10% fetal calf serum) instead of water shifted particle sizes from 96% of collected particles in the 0.65–1.1 µm size range to 26% between 0.65 and 1.1 µm; 60% between 1.1 and 2.1 µm; and 13% between 2.1 and 3.3 µm (Lai et al., 2004). Although influenza viruses range between 80 nm and 120 nm (Moorman, 2003), particles generated by the nebulizer were likely larger because of the nebulizer liquid being made up of phosphate buffered saline with bovine serum albumin and Antifoam A. Based on the typical Collison nebulizer particle size output and the composition of the nebulizer liquid, it is likely that a significant fraction of the VPs generated were above 1 µm and that for this study, collection efficiencies of the samplers were comparable.
In the case of PUF, although our bench top spike experiment results showed we could measure close to 100% of the total virus spike, the aerosol experiment showed that only 38% of the total virus could be detected. The difference was likely because of the particle extraction efficiency. For bench top virus spike experiments virus was seeded in a liquid at the surface of the PUF and allowed to dry, then washed off and assayed. The viruses in the aerosol experiment were dried particles that were dispersed by impaction throughout the internal surfaces of the PUF. Aerosol sampling efficiency is high for the CCI, and the CCI has many attractive features for sampling in the field, including the minimal loss of particles because of particle bounce, particle size separation, and high loading capacity (Demokritou et al., 2004) but further experiments to optimize extraction methods for virus aerosols collected on PUF will be required before the CCI can be recommended for this application.
In the case of Teflon filters, benchtop experiment results showed a significantly lower recovery (68%) of total virus from Teflon filters not treated with methanol compared with 100% from the PBS. In the aerosol experiments, recovery from the Teflon filter was not significantly less than the SKC Biosampler. The discrepancy is likely because of differences in virus binding from liquid solution to aerosols. Teflon filters bind proteins to the membrane through non-covalent hydrophobic interaction forces (verbal communication, Millipore). Our preliminary virus spike experiments showed that an aqueous solution of virus dried faster on the Teflon filter if the filter was treated first with methanol but also reduced virus recovery from 68% in untreated filters to 33% from methanol-treated filters The results from the PUF and Teflon filters highlight the importance of conducting sampler experiments using test aerosols because they can behave very differently than spiked samples on the bench top.
The average T/I ratio measured in the nebulizer across experiments was 290 VP/FFU, meaning one infectious virus was detected per 290 influenza virus RNA particles measured. T/I ratios measured in the nebulizer and the Biosampler were comparable, indicating that the process of aerosolization, transit through the aerosol chamber and collection with the Biosampler did not affect influenza virus infectiousness. The T/I ratios measured with the CCI, Teflon, and gelatin filters were lower than the T/I ratio measured in the nebulizer, indicating that virus aerosols lost infectivity once collected in each of these other samplers.
Based on the results of this study, none of the commercial aerosol samplers tested was ideal for collecting and preserving infectious viruses from the environment. In the case of the CCI, influenza virus appears to bind to the PUF and is not washed off by mechanical mixing. The gelatin filter can only be used for short sampling times (<15 min) as it desiccates and cracks. Teflon filters capture VPs efficiently but do not preserve infectivity. Despite its better performance, the SKC Biosampler has limitations for field applications: it is fragile and liquids are difficult to handle in the field, the volume necessary for operation is large (20 ml), introducing a large dilution factor, and its collection efficiency for particles under 1 µm, although much superior to earlier impingers, is low compared with filters and impactors (Willeke et al., 1998).
The relative humidity and temperature during our experiments was around 50% and 25°C respectively, but did not appear to affect the influenza virus infectivity. Although other studies have shown an effect of relative humidity and temperature on the infectiousness of influenza viruses (Lowen et al., 2007, 2008), in our study the T/I infectious virus ratios in the nebulizer liquid and the SKC Biosampler were the same, indicating that the viruses did not lose infectivity over the short time it took for viruses to travel between the nebulizer and the samplers.
There is a gap in the information available on viral particle production during respiratory activities such as sneezing, coughing, talking, and breathing. Although older studies of exhaled breath particles only measured VPs larger than 1 µm (Couch et al., 1966; Duguid, 1945, 1946), more recent studies show that most of the particles humans exhale are under 1 µm (Edwards et al., 2004; Fairchild and Stampfer, 1987; Papineni and Rosenthal, 1997). Our previous studies of exhaled breath showed that influenza virus RNA is found in particles between 0.3 µm and 1 µm (Fabian et al., 2008). These particles remain airborne for long periods of time, may carry infectious viruses, and may be responsible for airborne transmission of communicable viral diseases. To further examine the risk posed by submicron exhaled particles, it will be important to investigate whether the viral RNA present in these particles indicates the presence of infectious virus. The experiments reported here indicate that it will be essential for such investigations to collect submicron particle into liquid media. Therefore, future studies of airborne infectious viruses will need to employ a new sampler that combines high submicron particle collection efficiency with liquid sampling media.
Conclusions
We evaluated the efficiency of four commercially available samplers to collect laboratory-generated influenza virus aerosols and found that only the SKC Biosampler was efficient in collecting airborne viruses and preserving virus infectivity. These results highlight the importance of liquid media to preserve infectivity. Although the SKC Biosampler performed well in our laboratory experiments, its declining collection efficiency for particles less than 1 µm, its high dilution factor, and relatively low collection flow rate limit its utility for investigation naturally occurring aerosols. Total influenza virus (determined by molecular methods) was recovered efficiently with Teflon and gelatin filters, as well as the Biosampler. Thus, any of these methods can be used when it is not necessary to determine aerosol infectiousness. Results from this study provide useful design parameters for a new sampler that can efficiently collect submicron aerosols and preserve airborne infectious viruses. Such a sampler is needed for studies of airborne virus transmission.
Practical Implications.
New air samplers are needed to study infectious airborne viruses and learn about airborne disease transmission. As a first step in designing a new air sampler to collect influenza virus we evaluated four commercial samplers and determined necessary design parameters for a new collector.
Acknowledgements
This work has received financial support from the US Centers for Disease Control and Prevention (CDC) (cooperative grant no. 1U01CI000446-01), the National Institute of Health (training grants no. HL07118 and no. AI061884), and the Federal Aviation Administration (FAA) Office of Aerospace Medicine through the Air Transportation Center of Excellence for Airliner Cabin Environment Research (ACER). Although the FAA and CDC have sponsored this project, they neither endorse nor reject the findings of this research.
References
- Agranovski IE, Safatov AS, Borodulin AI, Pyankov OV, Petrishchenko VA, Sergeev AN, Agafonov AP, Ignatiev GM, Sergeev AA, Agranovski V. Inactivation of viruses in bubbling processes utilized for personal bioaerosol monitoring. Appl. Environ. Microbiol. 2004;70:6963–6967. doi: 10.1128/AEM.70.12.6963-6967.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aintablian N, Walpita P, Sawyer MH. Detection of Bordetella pertussis and respiratory syncytial virus in air samples from hospital rooms. Infect. Control Hosp. Epidemiol. 1998;19:918–923. doi: 10.1086/647764. [DOI] [PubMed] [Google Scholar]
- Artenstein MS, Cadigan FC., Jr Air sampling in viral respiratory disease. Arch. Environ. Health. 1964;9:58–60. doi: 10.1080/00039896.1964.10663793. [DOI] [PubMed] [Google Scholar]
- Artenstein MS, Miller WS. Air sampling for respiratory disease agents in army recruits. Bacteriol. Rev. 1966;30:571–572. doi: 10.1128/br.30.3.571-572.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blachere FM, Lindsley WG, Pearce TA, Anderson SE, Fisher M, Khakoo R, Meade BJ, Lander O, Davis S, Thewlis RE, Celik I, Chen BT, Beezhold DH. Measurement of airborne influenza virus in a hospital emergency department. Clin. Infect. Dis. 2009;48:438–440. doi: 10.1086/596478. [DOI] [PubMed] [Google Scholar]
- Booth TF, Kournikakis B, Bastien N, Ho J, Kobasa D, Stadnyk L, Li Y, Spence M, Paton S, Henry B, Mederski B, White D, Low DE, Mcgeer A, Simor A, Vearncombe M, Downey J, Jamieson FB, Tang P, Plummer F. Detection of airborne severe acute respiratory syndrome (SARS) coronavirus and environmental contamination in SARS outbreak units. J. Infect. Dis. 2005;191:1472–1477. doi: 10.1086/429634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton NC, Grinshpun SA, Reponen T. Physical collection efficiency of filter materials for bacteria and viruses. Ann. Occup. Hyg. 2007;51:143–151. doi: 10.1093/annhyg/mel073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couch RB, Cate TR, Douglas RG, Jr, Gerone PJ, Knight V. Effect of route of inoculation on experimental respiratory viral disease in volunteers and evidence for airborne transmission. Bacteriol. Rev. 1966;30:517–529. doi: 10.1128/br.30.3.517-529.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couch RB, Douglas RG, Jr, Lindgren KM, Gerone PJ, Knight V. Airborne transmission of respiratory infection with coxsackievirus A type 21. Am. J. Epidemiol. 1970;91:78–86. doi: 10.1093/oxfordjournals.aje.a121115. [DOI] [PubMed] [Google Scholar]
- Demokritou P, Lee SJ, Ferguson ST, Koutrakis P. A compact multistage (cascade) impactor for the characterization of atmospheric aerosols. J. Aerosol Sci. 2004;35:281–299. [Google Scholar]
- Duguid J. The numbers and the sites of origin of the droplets expelled during expiratory activities. Edinb. Med. J. 1945;52:385–401. [PMC free article] [PubMed] [Google Scholar]
- Duguid J. The size and duration of air-carriage of respiratory droplets and droplet-nuclei. J. Hyg. 1946;44:471–479. doi: 10.1017/s0022172400019288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards DA, Man JC, Brand P, Katstra JP, Sommerer K, Stone HA, Nardell E, Scheuch G. Inhaling to mitigate exhaled bioaerosols. PNAS. 2004;101:17383–17388. doi: 10.1073/pnas.0408159101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Elden LJ, Nijhuis M, Schipper P, Schuurman R, Van Loon AM. Simultaneous detection of influenza viruses A and B using real-time quantitative PCR. J. Clin. Microbiol. 2001;39:196–200. doi: 10.1128/JCM.39.1.196-200.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabian MP, Miller SL, Reponen T, Hernandez MT. Ambient bioaerosol indices for indoor air quality assessments of flood reclamation. J. Aerosol Sci. 2005;36:763–783. [Google Scholar]
- Fabian P, Mcdevitt JJ, Dehaan WH, Fung RO, Cowling BJ, Chan KH, Leung GM, Milton DK. Influenza virus in human exhaled breath: an observational study. PLoS ONE. 2008;3:e2691. doi: 10.1371/journal.pone.0002691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabian P, Mcdevitt JJ, Houseman EA, Milton DK. An optimized method to detect influenza virus and human rhinovirus from exhaled breath and the airborne environment. J. Environ. Methods. 2009;11:314–317. doi: 10.1039/b813520g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairchild CI, Stampfer JF. Particle concentration in exhaled breath. Am. Ind. Hyg. Assoc. J. 1987;48:948–949. doi: 10.1080/15298668791385868. [DOI] [PubMed] [Google Scholar]
- Farnsworth JE, Goyal SM, Kim SW, Kuehn TH, Raynor PC, Ramakrishnan MA, Anantharaman S, Tang W. Development of a method for bacteria and virus recovery from heating, ventilation, and air conditioning (HVAC) filters. J. Environ. Monit. 2006;8:1006–1013. doi: 10.1039/b606132j. [DOI] [PubMed] [Google Scholar]
- Gussman RA. [last accessed 28 February 2007];Generalized Output Data for BGI Collison Nebulizers. 2007 Available at: http://bgiusa.com/agc/collison.htm.
- Harper GJ. Airborne micro-organisms: survival tests with four viruses. J. Hyg. 1961;59:479–486. doi: 10.1017/s0022172400039176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartshorn K, White M, Tecle T, Tornoe I, Sorensen G, Crouch E, Holmskov U. Reduced influenza viral neutralizing activity of natural human trimers of surfactant protein D. Respir. Res. 2007;8:9–19. doi: 10.1186/1465-9921-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan CJ, Kettleson EM, Lee MH, Ramaswami B, Angenent LT, Biswas P. Sampling methodologies and dosage assessment techniques for submicrometre and ultrafine virus aerosol particles. J. Appl. Microbiol. 2005;99:1422–1434. doi: 10.1111/j.1365-2672.2005.02720.x. [DOI] [PubMed] [Google Scholar]
- Huynh KN, Oliver BG, Stelzer S, Rawlinson WD, Tovey ER. A new method for sampling and detection of exhaled respiratory virus aerosols. Clin. Infect. Dis. 2008;46:93–95. doi: 10.1086/523000. [DOI] [PubMed] [Google Scholar]
- Kavouras I, Koutrakis P. Use of polyurethane foam as the impaction substrate/collection medium in conventional inertial impactors. Aerosol. Sci. Technol. 2001;34:46–56. [Google Scholar]
- Ko G, First MW, Burge HA. Influence of relative humidity on particle size and UV sensitivity of Serratia marcescens and Mycobacterium bovis BCG aerosols. Tuber. Lung Dis. 2000;80:217–228. doi: 10.1054/tuld.2000.0249. [DOI] [PubMed] [Google Scholar]
- Lai KM, Burge HA, First MW. Size and UV germicidal irradiation susceptibility of Serratia marcescens when aerosolized from different suspending media. Appl. Environ. Microbiol. 2004;70:2021–2027. doi: 10.1128/AEM.70.4.2021-2027.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SJ, Demokritou P, Koutrakis P. Performance evaluation of commonly used impaction substrates under various loading conditions. J. Aerosol Sci. 2005;36:881–895. [Google Scholar]
- Lee WM, Grindle K, Pappas T, Marshall DJ, Moser MJ, Beaty EL, Shult PA, Prudent JR, Gern JE. High-throughput, sensitive, and accurate multiplex PCR-microsphere flow cytometry system for large-scale comprehensive detection of respiratory viruses. J. Clin. Microbiol. 2007;45:2626–2634. doi: 10.1128/JCM.02501-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowen AC, Mubareka S, Steel J, Palese P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 2007;3:1470–1476. doi: 10.1371/journal.ppat.0030151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowen AC, Steel J, Mubareka S, Palese P. High temperature (30 degrees C) blocks aerosol but not contact transmission of influenza virus. J. Virol. 2008;82:5650–5652. doi: 10.1128/JVI.00325-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May KR. The collison nebulizer: description, performance and application. J. Aerosol Sci. 1973;4:235–238. [Google Scholar]
- Mcdevitt JJ, Lai KM, Rudnick SN, Houseman EA, First MW, Milton DK. Characterization of UVC light sensitivity of vaccinia virus. Appl. Environ. Microbiol. 2007;73:5760–5766. doi: 10.1128/AEM.00110-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moorman JP. Viral characteristics of influenza. South. Med. J. 2003;96:758–761. doi: 10.1097/01.SMJ.0000084986.13843.52. [DOI] [PubMed] [Google Scholar]
- Myatt TA, Johnston SL, Zuo Z, Wand M, Kebadze T, Rudnick S, Milton DK. Detection of airborne rhinovirus and its relation to outdoor air supply in office environments. AJRCCM. 2004;169:1187–1190. doi: 10.1164/rccm.200306-760OC. [DOI] [PubMed] [Google Scholar]
- Pall Corporation. PTFE membrane disc filters, Pall Corporation Catalogue 2007. New York, USA: East Hills; 2007. [last accessed 5 January 2007]. Available at: http://labfilters.pall.com/catalog/924_20061.asp. [Google Scholar]
- Papineni RS, Rosenthal FS. The size distribution of droplets in the exhaled breath of healthy human subjects. J. Aerosol Med. 1997;10:105–116. doi: 10.1089/jam.1997.10.105. [DOI] [PubMed] [Google Scholar]
- Sartorius. Gelatine membrane filters, Sartorius Product Catalogue 2007. France: Aubagne; 2007. [last accessed 5 January 2007]. Available at: http://www.sartorius.com/biotechnology/products-laboratory/microbiological-analysis/air-monitoring/gelatine-membrane-filters.html. [Google Scholar]
- Sattar SA, Ijaz MK. Airborne viruses. In: Hurst CJ, Knudsen GR, Mcinerney MJ, Stetzenbach LD, Walter MV, Knudsen GR, editors. Manual of Environmental Microbiology. Washington, USA: ASM Press; 2002. pp. 682–692. [Google Scholar]
- Sawyer MH, Chamberlin CJ, Wu YN, Aintablian N, Wallace MR. Detection of varicella-zoster virus DNA in air samples from hospital rooms. J. Infect. Dis. 1994;169:91–94. doi: 10.1093/infdis/169.1.91. [DOI] [PubMed] [Google Scholar]
- Schaffer FL, Soergel ME, Straube DC. Survival of airborne influenza virus: effects of propagating host, relative humidity, and composition of spray fluids. Arch. Virol. 1976;51:263–273. doi: 10.1007/BF01317930. [DOI] [PubMed] [Google Scholar]
- Thomas G. Air sampling of smallpox virus. J. Hyg. (Lond) 1974;73:1–7. doi: 10.1017/s0022172400023767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willeke K, Lin X, Grinshpun SA. Improved aerosol collection by combined impaction and centrifugal motion. Aerosol Sci. Technol. 1998;28:439–456. [Google Scholar]