Abstract
Sentinel lymph node biopsy has become the standard of clinical care in staging axillary lymph nodes for breast carcinoma. While deemed safe and effective, methylene blue dye has been associated with infection, fibrosis, and skin and fat necrosis. The variable appearance of surgical dye-related fibrosis and fat necrosis on imaging studies poses a challenge to both radiologists and clinicians. We present a patient in whom a new enhancing lesion was visualized on follow-up magnetic resonance imaging for known breast carcinoma in the setting of neoadjuvant chemotherapy.
Fat necrosis is a relatively common clinical and radiologic entity, often diagnosed on mammography. We present an atypical case of fat necrosis that manifested as an area of suspicious enhancement on magnetic resonance imaging (MRI). The area of enhancement corresponded to a site of previous sentinel lymph node biopsy.
CASE REPORT
A 52-year-old woman previously diagnosed with grade II infiltrating ductal carcinoma presented to Baylor University Medical Center for a follow-up breast MRI examination. The patient had completed a sentinel lymph node biopsy with methylene blue dye injection approximately 5 months before the follow-up MRI. Methylene blue dye was injected into the lateral left breast at the time. An axial image from the initial breast MRI demonstrated a 2.4 cm spiculated mass at the 8:00 position of the medial left breast, approximately 6 cm from the nipple (Figure 1). Follow-up breast MRI performed 6 months later demonstrated an interval decrease in the size of this mass, with residual dimensions measuring 1.7 × 0.5 × 0.4 cm (Figure 2a). A new area of nonmasslike enhancement was also identified at the 3:00 position of the lateral left breast, approximately 4 cm deep to the nipple (Figure 2b). This area of suspicious enhancement measured 3.6 × 2.0 × 1.3 cm and was not definitively visualized on the initial MRI examination. It corresponded to the site of previous methylene blue dye injection. Given its suspicious enhancement characteristics, percutaneous MR-guided biopsy of the lesion was performed. Histology results were consistent with areas of fibrosis and fat necrosis from prior methylene blue sentinel node injection.
Figure 1.
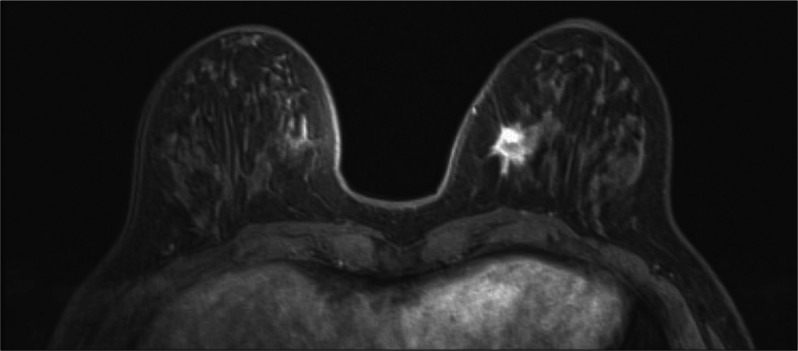
Gadolinium-enhanced axial image of the bilateral breasts from an initial MRI demonstrates a 2.4 cm spiculated mass at the 8:00 position of the medial left breast, approximately 6 cm from the nipple.
Figure 2.
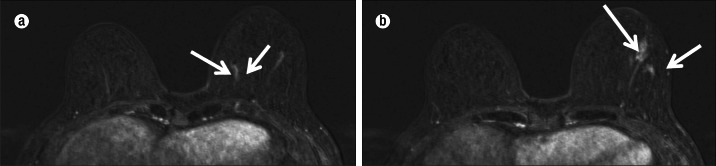
Gadolinium-enhanced axial images of the bilateral breasts from a follow-up MRI demonstrate (a) an interval decrease in the size of a spiculated mass at the 8:00 position of the left breast (arrows) and (b) a suspicious area of nonmasslike enhancement within the lateral left breast, approximately 4 cm from the nipple (arrows). This was new when compared to the original exam performed at diagnosis (see Figure 1).
DISCUSSION
Fat necrosis of the breast is a relatively benign and common radiologic entity and may result from trauma, previous surgery (i.e., needle or surgical biopsy, lumpectomy, or reduction mammoplasty), and/or radiation therapy. It results from a vascular insult to adipose tissue. When symptomatic, fat necrosis typically manifests as a small, painless mass, with up to 97% of cases presenting as a palpable abnormality. Concomitant or coexistent infection may further aggravate the development of fat necrosis (1, 2).
Fat necrosis exhibits a variety of diverse imaging appearances on mammography, a finding that is largely dependent upon the degree of ensuing fibrosis. It may present as a lipid cyst, focal asymmetry, spiculated mass, or calcific deposits (3). In the setting of minimal fibrosis, fat necrosis appears as a lucent mass or oil cyst, developing progressive areas of calcium. Fat necrosis may manifest as calcium alone. While these deposits are typically smooth, round, or curvilinear, some may take on a more ominous appearance with branching, rodlike, or angular morphologies. As fibrosis progresses, the appearance of fat necrosis changes into that of an irregular, asymmetric, or spiculated mammographic density (2).
Although fat necrosis may exhibit a varied appearance on breast MRI, the most common presentation is that of a lipid cyst, which appears as a round or oval mass with a hypointense T1 signal on fat-saturated images. While a thin rim of enhancement is common, the rim may also appear thickened, irregular, or spiculated. Additional features that can be visualized include fat-fluid levels and thin enhancing internal septations. Fat necrosis is characteristically isointense to fat seen elsewhere in the breast. Variable T1 hypointensity may occasionally be seen and presumably relates to hemosiderin deposition and surrounding inflammatory change. Predominantly fibrotic lesions are especially difficult to distinguish from malignant processes, appearing spiculated and solid rather than cystic. Kinetic analysis is often confounding, as fat necrosis exhibits the full continuum of benign to malignant enhancement patterns, including rapid and slow initial phase enhancement and progressive, plateau, and washout delayed kinetics. Enhancement may be focal or diffuse, homogenous or heterogeneous, and may persist for several years after the initial insult. Enhancement longevity depends upon the degree of ongoing inflammation and the quantity of granulation tissue. In cases in which fat necrosis cannot be confidently identified on the basis of imaging, biopsy should be obtained to confirm or deny histologic suspicions (1, 2).
Our case highlights one of the confounding complications of sentinel lymph node biopsy with methylene blue dye. It reiterates the association between surgical dye for axillary lymph node staging and the nonspecific imaging findings that fat necrosis and fibrosis may portend.
References
- 1.Daly CP, Jaeger B, Sill DS. Variable appearances of fat necrosis on breast MRI. AJR Am J Roentgenol. 2008;191(5):1374–1380. doi: 10.2214/AJR.07.4051. [DOI] [PubMed] [Google Scholar]
- 2.Taboada JL, Stephens TW, Krishnamurthy S, Brandt KR, Whitman GJ. The many faces of fat necrosis in the breast. AJR Am J Roentgenol. 2009;192(3):815–825. doi: 10.2214/AJR.08.1250. [DOI] [PubMed] [Google Scholar]
- 3.Chan LP, Gee R, Keogh C, Munk PL. Imaging features of fat necrosis. AJR Am J Roentgenol. 2003;181(4):955–959. doi: 10.2214/ajr.181.4.1810955. [DOI] [PubMed] [Google Scholar]


