Abstract
Kummell disease, or avascular necrosis of a vertebral body, presents as vertebral osteonecrosis typically affecting a thoracic vertebra with compression deformity, intravertebral vacuum cleft, and exaggerated kyphosis weeks to months after a minor traumatic injury. This rare disease is increasing in prevalence secondary to an aging population and the associated rise in osteoporosis. Treatment with vertebroplasty or surgical decompression and fusion is often required. We present a classic case of Kummell disease to illustrate the salient features of the condition, with associated imaging findings on computed tomography and magnetic resonance imaging.
Back pain is a common presenting complaint of patients in the emergency department and outpatient clinics and is a source of frustration for physicians and patients. Judicious imaging can elucidate the etiology and guide appropriate therapy. We present a case of Kummell disease, a rare but increasingly prevalent cause of back pain with classic imaging features.
CASE DESCRIPTION
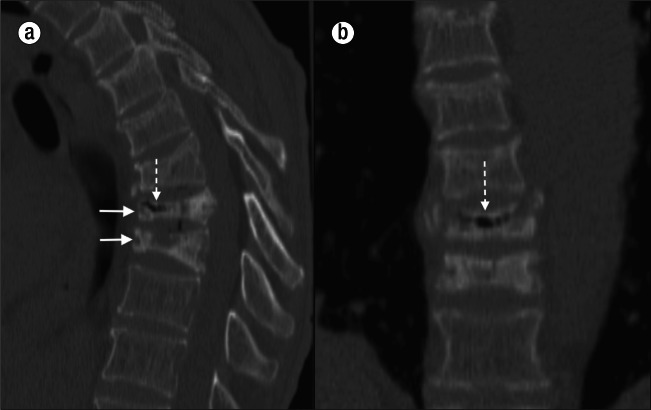
A 54-year-old man presented to the emergency department with abdominal pain and back pain. The patient described multiple prior minor traumatic events, namely falls from a standing position. He had end-stage renal disease and was on hemodialysis. He also had epilepsy and HIV infection. Computed tomography (CT) imaging of the abdomen showed multiple thoracic compression deformities and compression deformities of the T8 and T9 vertebral bodies with associated intravertebral vacuum clefts (Figure 1). Magnetic resonance imaging (MRI) of the thoracic spine revealed low signal intensity within the T8 and T9 vertebral bodies on all imaging sequences (Figure 2).
Figure 1.
CT images of Kummel's disease. (a) Sagittal and (b) coronal images of the thoracic spine show marked anterior compression deformities of the T8 and T9 vertebral bodies (solid arrows) with intravertebral vacuum clefts (dashed arrows) compatible with osteonecrosis.
Figure 2.
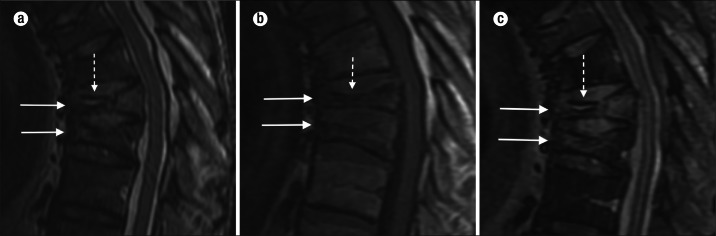
Sagittal MR images of a patient with Kummel's disease: (a) T2-weighted, (b) T1-weighted, and (c) STIR (short TI inversion recovery). Images show anterior compression deformities (solid arrows). The T2-weighted and STIR images show a classic “double line” sign of low-intensity vacuum cleft surrounded by elevated signal from edema (dashed arrow). The T1-weighted image shows the absence of signal within the vertebral body vacuum clefts (dashed arrow).
DISCUSSION
German surgeon Hermann Kummell described six patients with vertebral body compression deformities after minor trauma in 1895 (1, 2). Kummell hypothesized that “the nutrition of the affected vertebral bodies is injured,” leading to delayed collapse of the vertebral bodies (3). While initially Kummell disease (KD) was thought to be exceedingly rare, its prevalence is increasing with our aging and often osteoporotic population. The exact incidence of KD is unknown, and there is disagreement as to the appropriate eponym for the disease, with the terms Kummel, Kummell, and Kummell-Verneuil disease all being applied (1).
KD, avascular necrosis of a vertebral body, represents a failure of the fracture healing process after a minor traumatic injury (4). KD occurs most commonly in middle-aged to elderly men who complain of acute back pain after a fall. A number of risk factors have been identified, including chronic steroid use, osteoporosis, alcoholism, and radiation therapy (5).
Imaging studies immediately after the inciting event show no evidence of a compression deformity or acute fracture, although initial imaging is often not obtained due to the perceived mild nature of the traumatic event. Delayed compression deformity of the affected vertebral body and exaggerated thoracic kyphosis can be demonstrated on plain radiographs, CT, or MRI. Vertebral osteonecrosis with an intravertebral vacuum cleft is best shown on CT. CT shows compression deformities with sclerosis of the endplates and virtually pathognomonic foci of air within the vertebral body. MRI demonstrates a “double line sign,” where a linear region of low intensity represents the vacuum cleft surrounded by elevated T2/FLAIR (fluid-attenuated inversion recovery) signal of the fracture deformity or intravertebral fluid (6, 7).
Neurologic compromise is more common with KD than with osteoporotic compression fractures. Treatment of KD is designed to eliminate motion at the fracture site and to relieve neurologic symptoms. The preferred treatment method rests on three factors: the patient's subjective pain level, the degree of kyphotic deformity, and specific neurologic deficits (1). Vertebroplasty has shown favorable results and is successful at alleviating back pain, but surgical intervention is often indicated, especially in the presence of neurologic compromise (4, 5). Surgical decompression and fusion can be obtained from anterior, posterior, or combined approaches, with the goal of restoring near-anatomic sagittal alignment and eliminating pathologic motion.
References
- 1.Young WF, Brown D, Kendler A, Clements D. Delayed post-traumatic osteonecrosis of a vertebral body (Kummell's disease) Acta Orthop Belg. 2002;68(1):13–19. [PubMed] [Google Scholar]
- 2.Brower AC, Downey EF., Jr Kümmell disease: report of a case with serial radiographs. Radiology. 1981;141(2):363–364. doi: 10.1148/radiology.141.2.7291557. [DOI] [PubMed] [Google Scholar]
- 3.Benedek TG, Nicholas JJ. Delayed traumatic vertebral body compression fracture; part II: pathologic features. Semin Arthritis Rheum. 1981;10(4):271–277. doi: 10.1016/0049-0172(81)90004-4. [DOI] [PubMed] [Google Scholar]
- 4.Freedman BA, Heller JG. Kummel disease: a not-so-rare complication of osteoporotic vertebral compression fractures. J Am Board Fam Med. 2009;22(1):75–78. doi: 10.3122/jabfm.2009.01.080100. [DOI] [PubMed] [Google Scholar]
- 5.Osterhouse MD, Kettner NW. Delayed posttraumatic vertebral collapse with intravertebral vacuum cleft. J Manipulative Physiol Ther. 2002;25(4):270–275. doi: 10.1067/mmt.2002.123164. [DOI] [PubMed] [Google Scholar]
- 6.Yu CW, Hsu CY, Shih TT, Chen BB, Fu CJ. Vertebral osteonecrosis: MR imaging findings and related changes on adjacent levels. AJNR Am J Neuroradiol. 2007;28(1):42–47. [PMC free article] [PubMed] [Google Scholar]
- 7.Mirovsky Y, Anekstein Y, Shalmon E, Peer A. Vacuum clefts of the vertebral bodies. AJNR Am J Neuroradiol. 2005;26(7):1634–1640. [PMC free article] [PubMed] [Google Scholar]