Abstract
The incidence of obesity has steadily climbed to epidemic proportions in the United States. To provide optimal surgical care for the growing number of obese surgical patients, surgeons and other healthcare personnel must often modify routine procedures and standard treatment protocols. Psychological support of obese patients is an additional factor that frequently must be addressed during the perioperative period.
Keywords: Bariatric medicine, bariatric surgery, obesity
INTRODUCTION
The incidence of obesity has steadily climbed to epidemic proportions in the United States (US). According to a 2010 report from the Centers for Disease Control, 26.7% of Americans currently meet the criteria for obesity (body mass index ≥30 kg/m2).1 To provide optimal surgical care for the growing number of obese surgical patients, surgeons and other healthcare personnel must overcome a variety of unique challenges. Routine procedures, daily patient care activities, and standard treatment protocols often must be modified to safely manage heavier patients. Psychological issues related to obesity are an additional factor that frequently must be addressed during the perioperative period.
RADIOGRAPHIC LIMITATIONS
Increased patient body habitus may compromise radiographic image quality. Obtaining adequate studies of obese patients may require modification of standard imaging techniques. In a 2006 review of radiology reports from a 15-year period, Uppot et al2 determined that abdominal ultrasound was the imaging modality most limited by patient obesity. To overcome the attenuation of the ultrasound signal by excess subcutaneous adipose tissue, the lowest frequency probe should be used. Pressing the probe deeper into the abdominal wall can decrease the distance from the peritoneum.3,4
Obesity may impair the quality and exposure level of plain radiographs. Because x-ray beams must travel a greater distance to penetrate the subject, longer exposure times and the introduction of motion artifact are common. Obtaining diagnostic-quality x-ray images may require technical adjustments, such as increasing film speed and imaging settings.2-4
In addition to suboptimal image quality, the weight and aperture diameter constraints of computed tomography (CT) and magnetic resonance imaging (MRI) limit the technology's usefulness in evaluating obese patients. The industry standard table weight limits and maximum diameter for CT, cylindrical-bore MRI, and vertical-field open MRI are 450 lbs/70 cm, 350 lbs/60 cm, and 550 lbs/55 cm, respectively. Table thickness (15-18 cm) must be taken into account when deciding whether the device will accommodate the physical dimensions of an obese patient.4
In response to the growing demand for bariatric-sized hospital equipment, imaging devices with larger diameters and weight limits are now commercially available. The significant additional capital expense for this equipment is often not feasible for small centers and rural hospitals, and emergency access to large-capacity scanners in these settings may not be available. A 2008 survey of US hospitals with emergency departments found that only 10% had a large-capacity (≥450 lb) CT scanner, and only 8% had a large-capacity MRI machine. Academic hospitals were most likely to have large-weight capacity scanners (28%). An inquiry of US zoos and veterinary schools determined that most of the facilities with large animal CT scanners have formal policies preventing their use for imaging human subjects.5
Obesity may complicate or altogether prevent the administration of radiation therapy indicated for certain cancer types. The maximum weight capacity of a standard radiation treatment couch is 440 lbs. To deliver radiotherapy to heavier patients, a treatment couch may be modified with the addition of a commercial lift device with a higher weight capacity.6 Positioning the obese patient for treatment is also a challenge. Excess abdominal tissue folds may cause skin markings to shift and impair the reproducibility of the treatment target. In the prone position, the patient may be able to assist by lifting the pannus and holding it outside of the treatment field.7,8 However, prone positioning may not always be practical for morbidly obese patients because of respiratory compromise and limited mobility. Although both costly and time-consuming, daily pretreatment radiographic simulation may be necessary to ensure the accurate delivery of external-beam radiation.9
EQUIPMENT, TRANSPORTATION, AND SAFETY CONCERNS
As the population of obese patients increases, hospitals will need to adapt to accommodate larger patients. Simply providing larger beds and transport devices for use with obese patients is not feasible. Bariatric specialty equipment with high weight capacity and mobility aids should be installed and used for the safety of both patients and healthcare workers. Patient care algorithms developed for bariatric surgery programs provide useful guidelines for the proper care of all obese patients in the acute care setting.
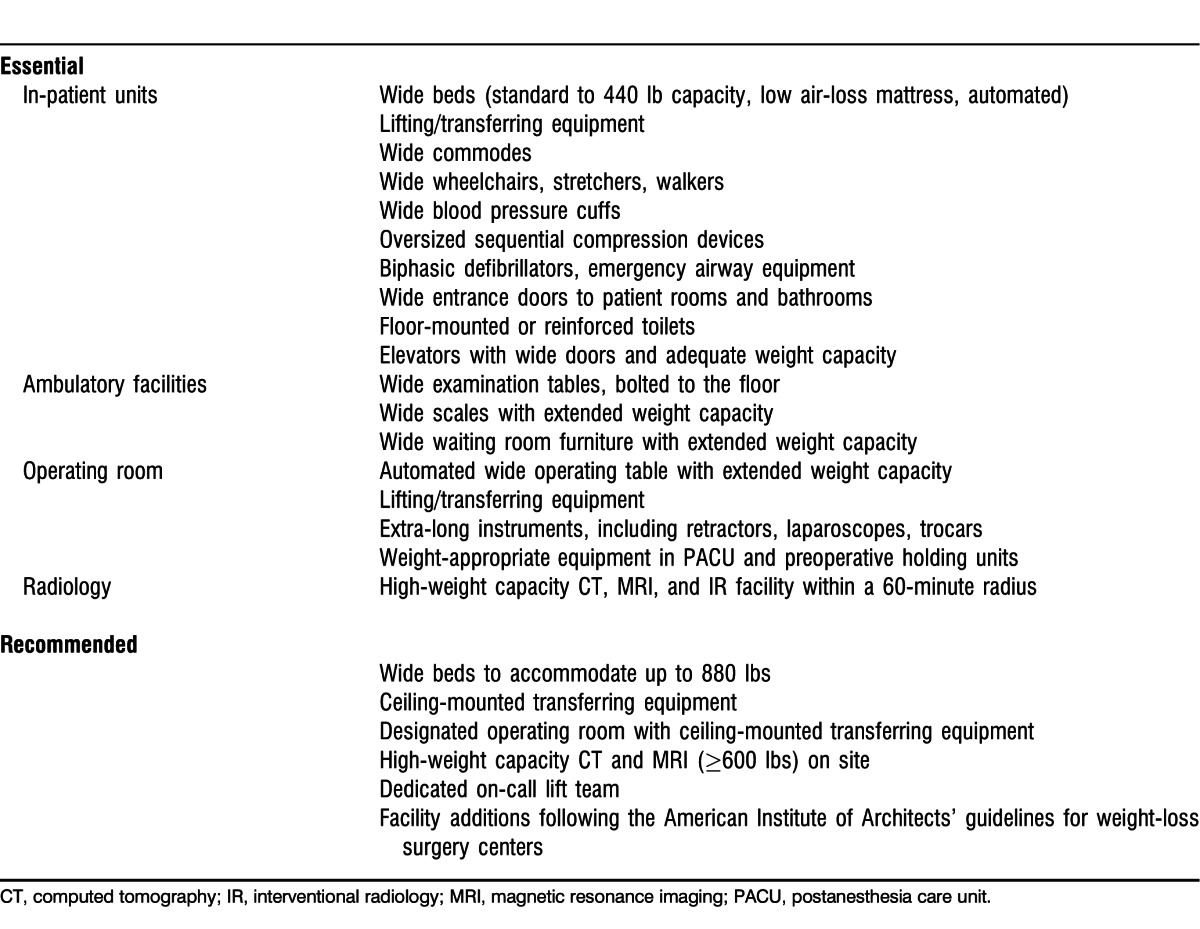
The education of healthcare providers on the unique needs of obese patients is essential for injury reduction. On the admission of each patient, providers should assess and document their weight and activity level and should then use a team-assist approach when transferring patients with a limited ability to support their own weight. Hospital equipment—including beds, toilets, shower chairs, wheelchairs, and stretchers—should be labeled according to weight capacity, with a list of available equipment and location displayed for reference on the hospital ward (Figure).10-12 The table lists essential and recommended bariatric patient care equipment.
Figure.
Sample nursing ward reference placard.
Table.
Essential and Recommended Equipment for Bariatric Care
Structural changes to patient care facilities that may be necessary to accommodate increasingly larger patients include the expansion of doorways in patient rooms and bathroom facilities, the installation of floor-mounted or reinforced toilets, and the expansion of overall room dimensions. Common areas, such as clinic waiting rooms, also should provide oversized seating options to prevent injury and potential embarrassment for obese patients.
The economic implications of hospitals treating an increasing number of obese patients are extensive. Expanded weight capacity equipment typically costs 25%-100% more than standard items. Building renovations may cost hundreds of thousands of dollars.13 Injuries to healthcare workers while treating obese patients are another source of financial impact. A back injury claim can cost up to $500,000 in wage replacement and treatment costs.14 In response to increasing reports of injury by hospital employees, some hospitals have hired and trained lift teams that are readily available to transfer and transport obese patients.13,14
SENSITIVITY TRAINING AND PSYCHOLOGICAL SUPPORT
Discrimination based on weight is common in US society and can have a negative impact on the overall health of obese people. In one study, 69% of the overweight and obese women surveyed reported weight-based discrimination from healthcare professionals.15
Weight bias occurs in various forms in the healthcare environment. Physicians, medical students, and healthcare providers may equate obesity with laziness, noncompliance, and a general lack of personal responsibility. They may also perceive an increase in the work effort required to care for an obese patient. Explicit displays of weight bias include disparaging comments made directly to or overheard by the patient. Implicit bias, delivered through body language and avoidance, is likely more common.16 As a result, patients may perceive that their caregivers feel they are to blame for their weight and medical problems. Depression, low self-esteem, and further avoidance of healthy activities are common consequences. Obese patients who feel like second-class patients may further delay or avoid necessary medical care.15,16
An optimal postoperative recovery environment for obese patients should be free of obesity-related prejudice. Formal sensitivity training for hospital employees is a required component for bariatric surgical centers of excellence. As the number of obese patients increases, weight-bias education and policies should become mainstream.
CONCLUSION
Based on data collected from 1970-2004, a study supported by the National Institutes of Health and the US Department of Agriculture projected further increases in the prevalence and cost of obesity in the United States.17 If current growth rates were sustained over time, nearly 100% of Americans would meet criteria for obesity by 2048. Annual obesity-related healthcare expenses are projected to double each decade, reaching nearly $1 trillion by 2030. As the number of obese patients continues to escalate, hospitals must adapt to accommodate the various needs of this patient population to provide them with safe, timely, and high-quality medical care.
Footnotes
The author has no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care and Medical Knowledge.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC) Vital signs: state-specific obesity prevalence among adults—United States, 2009. MMWR Morb Mortal Wkly Rep. 2010 Aug 6;59(30):951–955. [PubMed] [Google Scholar]
- 2.Uppot RN, Sahani DV, Hahn PF, Kalra MK, Saini SS, Mueller PR. Effect of obesity on image quality: fifteen-year longitudinal study for evaluation of dictated radiology reports. Radiology. 2006 Aug;240(2):435–439. doi: 10.1148/radiol.2402051110. Epub 2006 Jun 26. [DOI] [PubMed] [Google Scholar]
- 3.Obesity Reynolds A. Radiol Technol. 2011 Jan-Feb;82(3):219–239. medical imaging challenges. Erratum in: Radiol Technol. 2011 Mar-Apr;82(4):320. [Google Scholar]
- 4.Uppot RN, Sahani DV, Hahn PF, Gervais D, Mueller PR. Impact of obesity on medical imaging and image-guided intervention. AJR Am J Roentgenol. 2007 Feb;188(2):433–440. doi: 10.2214/AJR.06.0409. [DOI] [PubMed] [Google Scholar]
- 5.Ginde AA, Foianini A, Renner DM, Valley M, Camargo CA., Jr The challenge of CT and MRI imaging of obese individuals who present to the emergency department: a national survey. Obesity (Silver Spring) 2008 Nov;16(11):2549–2551. doi: 10.1038/oby.2008.410. Epub 2008 Sep 11. [DOI] [PubMed] [Google Scholar]
- 6.Towns P, Free B, Cernica G, Podgorsak MB. Practical issues in treating heavy patients on a LINAC treatment couch. J Appl Clin Med Phys. 2005 Winter;6(1):135–142. doi: 10.1120/jacmp.v6i1.2077. Epub 2005 Jan 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bentel GC. Radiation Therapy Planning. 2nd ed. New York, NY: McGraw-Hill;; 1996. [Google Scholar]
- 8.Purdy JA, Vijayakumar S, Perez CA, Levitt SH. Physics of treatment planning in radiation oncology. In: Levitt SH, Purdy JA, Perez CA, Vijayakumar S, editors. Technical Basis of Radiation Therapy: Practical Clinical Applications. 4th ed. Heidelberg, Germany: Springer-Verlag;; 2008. pp. 69–106. In. eds. [Google Scholar]
- 9.Sweigart KD. A simple method of alignment for pelvic irradiation in obese patients. Med Dosim. 2002 Winter;27(4):269–270. doi: 10.1016/s0958-3947(02)00151-6. [DOI] [PubMed] [Google Scholar]
- 10.Baptiste A. Safe bariatric patient handling toolkit. Bariatr Nurs Surg Patient Care. 2007 Spring;2(1):17–46. [Google Scholar]
- 11.Wright K, Bauer C. Meeting bariatric patient care needs: procedures and protocol development. J Wound Ostomy Continence Nurs. 2005 Nov-Dec;32(6):402–406. doi: 10.1097/00152192-200511000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Lautz DB, Jiser ME, Kelly JJ, et al. An update on best practice guidelines for specialized facilities and resources necessary for weight loss surgical programs. Obesity (Silver Spring) 2009 May;17(5):911–917. doi: 10.1038/oby.2008.581. Epub 2009 Feb 19. [DOI] [PubMed] [Google Scholar]
- 13.Diconsiglio J. Hospitals equip to meet the bariatric challenge. Rising number of obese patients necessitates specific supplies. Mater Manag Health Care. 2006 Apr;15(4):36–39. [PubMed] [Google Scholar]
- 14.Larkin H. Capital & candor. To meet the needs of obese patients, hospitals change processes, equipment and attitudes. Hosp Health Netw. 2004 Feb;78(2):58–62. [PubMed] [Google Scholar]
- 15.Puhl RM, Brownell KD. Confronting and coping with weight stigma: an investigation of overweight and obese adults. Obesity (Silver Spring) 2006 Oct;14(10):1802–1815. doi: 10.1038/oby.2006.208. [DOI] [PubMed] [Google Scholar]
- 16.O'Brien KS, Puhl RM, Latner JD, Mir AS, Hunter JA. Reducing anti-fat prejudice in preservice health students: a randomized trial. Obesity (Silver Spring) 2010 Nov;18(11):2138–2144. doi: 10.1038/oby.2010.79. Epub 2010 Apr 15. [DOI] [PubMed] [Google Scholar]
- 17.Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? estimating the progression and cost of the US obesity epidemic. Obesity (Silver Spring) 2008 Oct;16(10):2323–2330. doi: 10.1038/oby.2008.351. Epub 2008 Jul 24. [DOI] [PubMed] [Google Scholar]



