Abstract
BACKGROUND
An estimated 1% to 1.9% of North Americans are infected with the hepatitis C virus (HCV). Although Indigenous peoples are considered to bear the highest burden, there are only limited data regarding the demographic features and epidemiology of hepatitis C in this population.
OBJECTIVES:
To document the demographic characteristics, rates of newly diagnosed hepatitis C cases and prevalence of HCV infection in a Canadian First Nations population, and to compare the findings with an infected non-First Nations population.
METHODS:
A research database spanning 1991 to 2002 was developed, linking records from multiple clinical and administrative sources. Over a 12-year period, 671 First Nations and 4347 non-First Nations HCV-positive Canadians were identified in the province of Manitoba. Demographics, residence and time trends were compared between infected First Nations and non-First Nations persons.
RESULTS:
HCV-infected First Nations individuals were younger (mean [± SD] age 33.0±0.4 years versus 39.7±0.2 years; P<0.0001), more often female (60% versus 40%; P<0.0001) and more often resided in urban centres (73% versus 27%; P<0.001). The rate of newly diagnosed HCV cases was 2.5-fold (91.1 per 100,000 versus 36.6 per 100,000; P<0.000) and prevalence 2.4-fold (801.7 per 100,000 versus 334.8 per 100,000; P<0.000) higher among the First Nations relative to non-First Nations populations.
CONCLUSIONS:
The results of the present large population-based study indicate that the First Nations population with hepatitis C is characteristically different from infected non-First Nations persons. The results also describe higher rates of newly diagnosed cases and prevalence of HCV infection in the First Nations population. These findings should serve as an important baseline for future primary prevention and therapeutic intervention strategies in this high-risk population.
Keywords: First Nations populations, Hepatitis C, HCV infection, Incidence, Longitudinal, Population-based, Prevalence
Abstract
HISTORIQUE :
On estime que de 1 % à 1,9 % des Nord-Américains sont infectés par le virus de l’hépatite C (VHC). Même si on considère que les peuples autochtones en portent le fardeau le plus élevé, on possède seulement des données limitées au sujet des caractéristiques démographiques et épidémiologiques de l’hépatite C au sein de cette population.
OBJECTIFS :
Étayer les caractéristiques démographiques, le taux de nouveaux diagnostics d’hépatite C et la prévalence d’infections par le VHC au sein de la population des Premières nations du Canada et comparer les résultats à ceux d’une population infectée ne faisant pas partie des Premières nations.
MÉTHODOLOGIE :
Les chercheurs ont mis au point une base de données de recherche couvrant les années 1991 à 2002, reliant les dossiers de multiples sources cliniques et administratives. Sur une période de 12 ans, ils ont recensé 671 Canadiens des Premières nations et 4 347 Canadiens ne faisant pas partie des Premières nations, tous positifs au VHC, dans la province du Manitoba. Ils ont comparé les facteurs démographiques, le lieu de résidence et les tendances dans le temps entre les personnes infectées des Premières Nations et ne faisant pas partie des Premières nations.
RÉSULTATS :
Les personnes infectées par le VHC faisant partie des Premières nations étaient plus jeunes (âge moyen [±ÉT] de 33,0±0,4 ans par rapport à 39,7±0,2 ans; P<0,0001), étaient plus souvent de sexe féminin (60 % par rapport à 40 %; P<0,0001) et habitaient plus souvent dans un centre urbain (73 % par rapport à 27 %; P<0,001). Le taux de nouveaux diagnostics de VHC était 2,5 fois plus élevé (91,1 cas sur 100 000 habitants par rapport à 36,6 cas sur 100 000 habitants; P<0,000) et la prévalence 2,4 fois élevée (801,7 cas sur 100 000 habitants, par rapport à 334,8 cas sur 100 000 habitants; P<0,000) chez les populations des Premières nations que chez les populations n’en faisant pas partie.
CONCLUSIONS :
D’après les résultats de la présente étude en population d’envergure, la population des Premières nations atteinte d’hépatite C diffère de manière caractéristique des populations infectées n’en faisant pas partie. Les résultats font également foi de taux plus élevés de nouveaux diagnostics et d’une plus forte prévalence d’infection par le VHC au sein de la population des Premières nations. Ces observations devraient constituer une base importante pour les prochaines stratégies de prévention et d’intervention thérapeutique auprès de cette population à haut risque.
It is estimated that approximately 170 million people worldwide are chronically infected with the hepatitis C virus (HCV) (1). In North America, estimates range between 3.9 million and 4.1 million infected persons in the United States, and between 250,000 and 275,000 in Canada (2–4). While a plethora of data regarding various epidemiological and clinical aspects of hepatitis C in North America has been accumulated, the extent of infection and its burden among Indigenous populations, including Canada’s First Nations peoples, remains largely unstudied, this despite recent data suggesting that exposure rates to HCV are higher in Indigenous compared with non-Indigenous populations (5–12).
In Canada, national surveillance data are insufficient for determining the number of cases of hepatitis C among Aboriginal populations, largely because most provinces do not collect information according to ethnicity. As a result, information regarding ethnicity has been confined to population groups already at high risk for acquisition of bloodborne pathogens (such as prison inmates and the injection drug use [IDU] population). For example, the prevalence of antibodies to HCV (anti-HCV) among attendees of a First Nations alcohol and drug rehabilitation program in British Columbia was 18% (5), while the Enhanced Hepatitis Surveillance of Canadian Street Youth study (6) revealed 6% of self-identified Aboriginals to be anti-HCV positive. A study examining street-involved youth in Winnipeg (Manitoba) (7) found the anti-HCV prevalence among self-identified Aboriginal youth to be 20.1% compared with 14.4% among non-Aboriginal ethnicities. Finally, a high prevalence of hepatitis C (25% to 40%) and over-representation of HCV-infected individuals of Aboriginal heritage has also been documented among populations of prison inmates in Canada (8–12).
Thus, the objective of the present study was to provide detailed population-based data on the demographic features, rates of newly diagnosed cases and prevalence of HCV infection in a large Canadian Indigenous First Nations population.
METHODOLOGY
Data sources
The data used for the present study were derived from Manitoba Public Health and administrative databases. Universal health insurance is available to all residents of Manitoba; consequently, almost all (>98%) resident’s physician visits, hospitalizations, prescription drug use and vital statistics are accurately recorded (13,14). The developed study database contains a longitudinal record for Manitoba residents who tested positive for hepatitis C by the Cadham Provincial Laboratory and were, therefore, reported to the Public Health Unit of Manitoba Health. The Cadham Provincial Laboratory is the only laboratory performing HCV testing for the province of Manitoba. There were two distinct periods for HCV testing. From 1991 to 1995, no RNA assays were available and only first- and second-generation immunoassays were used to detect HCV infection. Consequently, cases diagnosed between 1991 and 1995 would include those infected with HCV at the time of testing as well as those previously infected who spontaneously cleared the virus. Subsequent to 1995, when RNA assays were introduced, specimens were considered to be positive only if both anti-HCV screening and HCV-RNA tests were positive (15). The study database includes records for the period between January 1, 1991 and December 31, 2002.
The Manitoba Health population registry was used to identify individuals belonging to a First Nations population. As part of the process for registration within the Manitoba Health insurance system, First Nations affiliation is recorded in the population registry. However, for a variety of historical and political reasons, some individuals of Aboriginal ancestry are not eligible for registration under the Indian Act of Canada. These individuals (an estimated 30%) were, therefore, not identified as First Nations in the present study (16,17). The anonymous linkage of Manitoba Health databases was possible via scrambled health numbers, thereby allowing for the creation of a de-identified longitudinal record of health services. The detailed description of the study database is provided elsewhere (18).
Definitions
For the purpose of the present study, the term ‘incidence’ was used to emphasize that the study was concerned with all new cases of HCV diagnosed in Manitoba (18). Therefore, all newly reported cases were regarded as incident cases, although they may not necessarily represent a newly acquired infection. The date of such ‘incident’ cases was based on the date of the first positive blood test recorded in the provincial Viral Hepatitis Surveillance Database, and cases were only counted once.
The term ‘prevalence’ was used to describe the accumulation of previously diagnosed and newly diagnosed cases of hepatitis C each year in the province among residents whose health coverage had not been terminated by death or migration out of province (18). A prevalent case was counted annually from the incident year, provided the resident maintained provincial health care coverage.
Statistical analysis
Statistical analyses were performed using SAS version 9.1 (SAS Institute, USA) for Windows (Microsoft Corporation, USA). Both crude and age/sex-adjusted rates of newly diagnosed cases per 100,000 population were calculated to correct for the demographic differences between the First Nations and non-First Nations populations in Manitoba. Direct standardization was used for calculating adjusted rates, with the 2001 Canadian population (census data) as the standard (19). First Nations to non-First Nations, and female to male ratios of adjusted rate of newly diagnosed cases with 95% CIs were calculated. Annual rates of newly diagnosed cases of HCV infection were calculated using the population of Manitoba for the corresponding year. The cumulative rates of newly diagnosed cases for 1992 to 2002 were computed by summing all new cases and the mid-year population at risk for those years. The point prevalence at December of each year was estimated by determining the number of cases that had previously been diagnosed with hepatitis C and whose health coverage had not ended due to death or outmigration from the province according to the Manitoba Health population registry at that time.
RESULTS
Demographics
During the 12-year study period, a total of 5018 cases of HCV infection were reported, of which 671 (13.4%) were First Nations. This represents more than twice the proportion of First Nations persons registered with the Manitoba Health Plan Registry (20). The demographic features of the hepatitis C-diagnosed individuals are summarized in Table 1.
TABLE 1.
Demographic characteristics of hepatitis C cases in Manitoba, 1991 to 2002
| Characteristic | First Nations | Non-First Nations |
|---|---|---|
| Total | 671 (13.4) | 4347 (86.6) |
| Female sex | 392 (58.4)* | 1575 (36.2)* |
| Female:male ratio | 1.41 | 0.57 |
| Age group, years | ||
| <18 | 25 (3.7)* | 65 (1.5)* |
| 18–39 | 506 (75.4)* | 2278 (52.4)* |
| 40–59 | 129 (19.2)* | 1682 (38.7)* |
| >60 | 11 (1.6)* | 322 (7.4)* |
| Age, years, mean ± SD (median) | 33±0.4*(33) | 39.7±0.2*(39) |
| Female | 32±0.5*(32) | 39±0.4*(39) |
| Male | 34±0.5*(34) | 40±0.2*(39) |
| Residence | ||
| Urban (Winnipeg, Manitoba) | 530 (79.0)† | 3651 (84.0)† |
| Rural south | 87 (13.0) | 609 (14.0) |
| Rural north | 54 (8.0)* | 87 (2.0)* |
Data presented as n (%) unless otherwise indicated. First Nations versus non-First Nations:
P<0.0001;
P<0.001
First Nations subjects were younger than their non-First Nations counterparts, with 79% of First Nations persons testing positive for HCV before 40 years of age, compared with 54% of non-First Nations individuals (P<0.00001). Almost 60% of HCV-infected First Nations persons were female (female to male ratio 1.4:1). Conversely, there was a male predominance in the non-First Nations group (64%) (female to male ratio = 0.6:1).
Overall, 26% of all First Nations and 59% of non-First Nations Manitobans reside in Winnipeg. However, 79% of cases occurred among 26% of urban First Nations (ratio 3.7), whereas 84% of cases occurred in the 59% of urban non-First Nations (ratio 1.4). Rural residents, both First Nations and non-First Nations, were less often infected with HCV, with 21% of cases occurring among 78% of rural First Nations (ratio 0.3), and 16% of cases occurring in the 41% of rural non-First Nations (ratio 0.4).
Rate of newly diagnosed HCV infection
Since 1991/1992 (31 reported HCV cases), the annual number of cases increased to more than 500 new cases per year by 1995 (Table 2). The highest rates of HCV infection were observed among First Nations females, followed by First Nations males, non-First Nations males and non-First Nations females (Figure 1). The cumulative rate of newly diagnosed HCV among First Nations females was 4.1 times higher than the rate of newly diagnosed cases among non-First Nations females. The cumulative rate of newly diagnosed HCV infection among First Nations males was 1.6 times that of non-First Nations males.
TABLE 2.
Annual age- and sex-adjusted rates of newly diagnosed cases and prevalence of hepatitis C virus infection (per 100,000 population) among First Nations and non-First Nations persons, Manitoba, 1991 to 2002
| Newly diagnosed cases | Prevalent cases | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| First Nations | Non-First Nations | First Nations | Non-First Nations | Prevalence ratio | ||||||
|
|
|
|||||||||
| Year | Cases, n | Rate | Cases, n | Rate | Rate ratio | Cases, n | Prevalence | Cases, n | Prevalence | |
| 1991/1992 | * | 30 | 2.71 | * | 30 | 2.80 | ||||
| 1993 | 7 | 19.61 | 80 | 7.34 | 2.7 | 7 | 11.41 | 110 | 10.23 | 1.1 |
| 1994 | 22 | 37.01 | 217 | 19.85 | 1.9 | 29 | 46.08 | 325 | 30.01 | 1.5 |
| 1995 | 87 | 141.56 | 478 | 43.8 | 3.2 | 116 | 180.95 | 792 | 73.14 | 2.5 |
| 1996 | 71 | 107.93 | 479 | 43.95 | 2.5 | 184 | 281.23 | 1219 | 112.95 | 2.5 |
| 1997 | 87 | 140.66 | 503 | 46.21 | 3.0 | 263 | 394.95 | 1671 | 154.76 | 2.6 |
| 1998 | 94 | 160.51 | 582 | 53.59 | 3.0 | 352 | 521.42 | 2161 | 201.03 | 2.6 |
| 1999 | 87 | 144.96 | 485 | 44.53 | 3.3 | 433 | 629.49 | 2551 | 237.16 | 2.7 |
| 2000 | 57 | 88.29 | 477 | 43.69 | 2.0 | 471 | 656.34 | 2915 | 270.37 | 2.4 |
| 2001 | 89 | 146.85 | 596 | 54.36 | 2.7 | 539 | 733.84 | 3364 | 311.62 | 2.4 |
| 2002 | 69 | 101.53 | 420 | 38.32 | 2.6 | 598 | 801.71 | 3621 | 334.77 | 2.4 |
| Cumulative | 671 | 91.10 | 4347 | 36.63 | 2.5 | |||||
Suppressed due to small number
Figure 1).
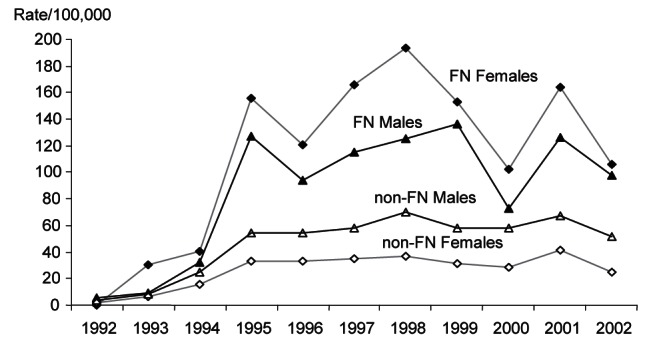
Annual age-adjusted rate of newly diagnosed hepatitis C virus infection according to sex among First Nations (FN) versus non-FN persons, Manitoba, 1992 to 2002 (per 100,000 population)
The age-specific rates of newly diagnosed HCV infections were higher among First Nations than non-First Nations individuals in most age groups (Table 3). In First Nations, the rates of newly diagnosed hepatitis C among females were higher compared with males in all age groups except 40 to 44 years. In contrast, the rates of newly diagnosed HCV infection among non-First Nations males were higher than in females in all age groups beginning at 25 years of age.
TABLE 3.
Age-specific cumulative rate of newly diagnosed cases and prevalence of hepatitis C virus infection infection according to sex
| Age group, years | Age-specific rate of newly diagnosed cases, 1991 to 2002 | Age-specific prevalence, 2002 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| First Nations | Non-First Nations | Rate ratio* (95% CI) | First Nations | Non-First Nations | Rate ratio* (95% CI) | |||||
|
|
|
|||||||||
| Cases, n | Rate per 100,000 | Cases, n | Rate per 100,000 | Cases | Rate per 100,000 | Cases | Rate per 100,000 | |||
| Female | ||||||||||
| 0–17 | 19 | 10.6 | 36 | 2.3 | 4.6 (2.5–7.8) | 17 | 103.1 | 31 | 25.0 | 4.1 (2.1–7.2) |
| 18–24 | 61 | 119.1 | 166 | 27.2 | 4.4 (3.2–5.8) | 59 | 1313.2 | 148 | 298.7 | 4.4 (3.2–5.8) |
| 25–29 | 68 | 192.8 | 199 | 43.7 | 4.4 (3.3–5.7) | 63 | 2159.8 | 175 | 511.8 | 4.2 (3.1–5.5) |
| 30–34 | 95 | 296.6 | 278 | 55.5 | 5.3 (4.2–6.7) | 87 | 2904.8 | 239 | 672.0 | 4.3 (3.3–5.5) |
| 35–39 | 76 | 290.3 | 270 | 51.3 | 5.7 (4.3–7.2) | 66 | 2381.0 | 231 | 561.6 | 4.2 (3.1–5.5) |
| 40–44 | 39 | 199.0 | 216 | 43.3 | 4.6 (3.1–6.2) | 36 | 1604.3 | 190 | 431.0 | 3.7 (2.5 –5.1) |
| 45–49 | 18 | 125.1 | 142 | 32.4 | 3.9 (2.1–5.9) | 17 | 1036.0 | 133 | 319.8 | 3.2 (1.7–5.0) |
| ≥50 | 16 | 41.3 | 268 | 13.5 | 3.1 (1.6–4.6) | 12 | 305.6 | 210 | 117.4 | 2.6 (1.1–4.2) |
| Total | 392 | 98.8 | 1575 | 24.0 | 4.1 (3.7–4.6) | 357 | 953.0 | 1357 | 247.1 | 3.9 (3.4–4.3) |
| Male | ||||||||||
| 0–17 | 6 | 3.2 | 31 | 1.9 | 1.7 (0.4–3.4) | 6 | 35.3 | 28 | 21.4 | 1.6 (0.4–3.4) |
| 18–24 | 32 | 63.6 | 129 | 20.5 | 3.1 (2.0–4.4) | 27 | 593.7 | 104 | 203.8 | 2.9 (1.8–4.3) |
| 25–29 | 44 | 133.9 | 300 | 65.3 | 2.1 (1.4–2.7) | 42 | 1564.8 | 240 | 694.0 | 2.3 (1.5–3.0) |
| 30–34 | 69 | 229.6 | 425 | 83.7 | 2.7 (2.1–3.5) | 57 | 2106.4 | 351 | 985.0 | 2.1 (1.6–2.8) |
| 35–39 | 61 | 246.5 | 510 | 95.9 | 2.6 (1.9–3.3) | 55 | 2164.5 | 433 | 1062.4 | 2.0 (1.5–2.6) |
| 40–44 | 41 | 215.2 | 510 | 101.7 | 2.1 (1.5–2.8) | 36 | 1662.8 | 419 | 933.1 | 1.8 (1.2–2.4) |
| 45–49 | 12 | 81.6 | 424 | 96.5 | 0.8 (0.4–1.3) | 12 | 791.6 | 356 | 855.5 | 0.9 (0.4–1.5) |
| ≥50 | 14 | 34.8 | 443 | 26.4 | 1.3 (0.6–2.0) | 6 | 150.2 | 333 | 217.2 | 0.7 (0.1–1.3) |
| Total | 279 | 70.0 | 2772 | 43.5 | 1.6 (1.4–1.8) | 241 | 649.1 | 2264 | 425.1 | 1.5 (1.3–1.7) |
First Nations/non-First Nations
The difference in age-specific rate of newly diagnosed HCV infection was particularly large in women, with the cumulative rate of newly diagnosed cases in First Nations females four times that of non-First Nations females, while the cumulative rate of newly diagnosed cases of hepatitis C in First Nations males was 1.6 times higher than in non-First Nations males.
Prevalence
The age-adjusted prevalence of hepatitis C among Manitoba residents increased steadily between 1991/1992 and 2002 for First Nations and non-First Nations. There was a 4.5-fold increase in age-adjusted prevalence from in 2002 compared with 1995 (Figure 2). At the end of the study period, 89% of all HCV-infected First Nations persons and 83% of infected non-First Nations remained in the province (Table 2), illustrating the significant burden of chronic HCV infection. Throughout the 12-year study period, First Nations males had an average prevalence of HCV infection 1.5 times that of non-First Nations males, whereas First Nations females had an average prevalence of HCV 3.9 times that of non-First Nations females.
Figure 2).
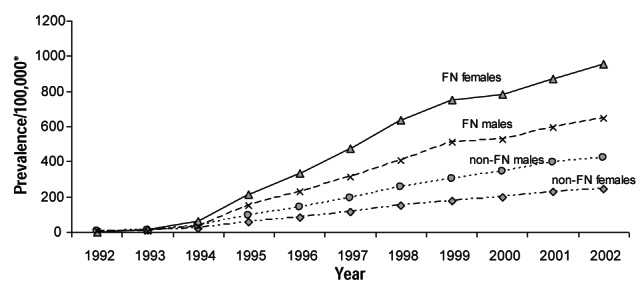
Annual age-adjusted prevalence of hepatitis C in Manitoba, 1992 to 2002. FN First Nations
In 2002, the age-specific prevalence of hepatitis C was higher among First Nations than non-First Nations individuals in almost all age groups (Table 3). The highest age-specific prevalence was in the 30 to 34 years of age group among females (both First Nations and non-First Nations), and in the 35 to 39 years of age group for males (also both First Nations and non-First Nations).
In First Nations persons, the age-specific prevalence of hepatitis C was higher among females than males in all groups except the 40 to 44 years of age group. Conversely, the prevalence of hepatitis C was higher among non-First Nations males than females in all age groups except those zero to 24 years of age.
DISCUSSION
Unlike the sex distribution of HCV infection described in the literature and noted in the non-First Nations populations of the present study, the majority of First Nations persons with HCV infection are female. HCV-infected First Nations persons are also significantly younger than non-First Nations individuals. Collectively, these findings are consistent with the Enhanced Hepatitis Strain Surveillance System report, which demonstrated that Aboriginal patients with newly acquired HCV infection were more often female (55% of Aboriginal versus 38% non-Aboriginal persons) and significantly younger than non-Aboriginal persons (21). The most likely explanation for these findings is the predominance of First Nations females of younger age in the IDU population, which has been described in several North American studies (3,20–25). For example, the Winnipeg Injection Drug Epidemiology (WIDE) study found a clear trend toward younger drug users being female, with 41% of Aboriginal females versus 25% of males <30 years of age and the overall proportion of Aboriginal females in the study’s IDU cohort being 52% (22). Callaghan et al (23) documented that among Canadian Aboriginal individuals admitted to an inpatient substance abuse detoxification program in Prince George, British Columbia, females were younger than males, received proportionately higher rates of cocaine and opiate detoxification diagnoses (highest among females 18 to 25 years of age), and more often reported having hepatitis C compared with male clients (29% versus 21%, respectively). Finally, in the Cedar Project from British Columbia (24), 65% of community-based young Aboriginal women between 14 and 30 years of age used injection drugs for periods of between 0.1 and 13 years; the proportion of HCV-infected individuals was 43.6% in women compared with 25.4% in men. Restricting analysis to young injection drug users resulted in the same trend in that the proportions who were HCV-positive were significantly higher among Aboriginal females (25). Our results are also consistent with data from American Indian populations in which 3% of women screened during routine prenatal care were anti-HCV positive compared with 1.6% in the general population (26). On the other hand, Armstrong et al (3) and McMahon et al (27) reported the prevalence of HCV in an Alaskan Native community-based population to be 0.82%, which is below the estimated United States national prevalence of 1.6%. Nonetheless, the investigators also found that the majority of HCV-infected persons were female (55%) and most resided in urban areas.
The present study also documented significantly higher and increasing rates of newly diagnosed HCV infection among the First Nations compared with non-First Nations population. Similar findings have been reported in which HCV infection rates among First Nations populations accounted for 0.4% to 29.3% of all reported cases within various provinces (6,28). Similarly, a 2010 Epi-Update also demonstrated that between 2002 and 2008, the overall reported rate of newly diagnosed HCV was 4.7 times higher among Aboriginal Canadians than among those of other ethnicities (29). Wu at al (21) described the incidence of newly acquired HCV infection to be 6.7 times higher in Aboriginal than non-Aboriginal Canadians (18.9 versus 2.8 cases per 100,000 population, respectively). Similarly, the incidence of hepatitis C among American Indians/Alaska Natives was 2.8 times higher than among the Caucasian population (30).
There have been no published reports describing hepatitis C prevalence among First Nations populations nationally. However, Remis (28) estimated the prevalence of hepatitis C in the First Nations of Canada to be 3%, an estimate supported by our results.
The present study had several strengths. Population-based data regarding HCV infection in North America is largely limited to the two National Health and Nutrition Examination Survey (NHANES) conducted in the United States from 1988 to 1994, and 1999 to 2002, which reported the prevalence of HCV infection to be 1.8% and 1.6%, respectively (2,3). Even more limited are population-based data regarding hepatitis C in North American Indigenous populations. The majority of studies published to date involve either specific high-risk populations (IDU, prison inmates, etc) or are based on various clinical settings with highly selected populations. To our knowledge, the present study was the first to use large population-based data on HCV infection in an Indigenous population. Using a combination of public health and administrative data created a comprehensive database of HCV infection in a defined and stable population. The relatively long time interval of 12 years also permitted an examination of time trends in rates of newly diagnosed hepatitis C and prevalence data.
The present study was, however, not without limitations. First, the data were derived from a public health database for estimates of rate of newly diagnosed HCV infection and prevalence of hepatitis C. This approach underestimates the actual incidence and prevalence of hepatitis C because it is contingent on infected persons being tested, diagnosed and reported to the public health department through interaction with the health care system, and is not based on a population-based sampling. Therefore, the results of the present study are not directly comparable with the results of seroepidemiological surveys such as NHANES-derived data. What is reported here is the lowest bound of the epidemic and the true number of cases may only be greater. As suggested by Sherman et al (31), upwards of one-third of cases in Canada remain undiagnosed. Second, it is unknown what proportion of the provinces’ population had undergone HCV testing in addition to the rates of HCV testing in different demographic groups. The differential rates of testing across population subgroups will influence the number of cases found and reported. However, the surveillance data capture only positive test results and, in absence of data on actual numbers of persons tested or those who tested negative, our reported estimates represent demographics of hepatitis C cases that are diagnosed and enter the health care system in Manitoba. Third, the restriction of First Nations designation in the present study to individuals registered under the Indian Act of Canada and the under-recording of First Nation status in the Manitoba Health Registry likely diminished the observed differences between the First Nations and non-First Nations populations. Finally, the estimated prevalence of hepatitis C was based on the balance of incoming incident and outgoing cases due to death or moving out of province (data reliably provided by the population registry); however, a small number of persons with chronic hepatitis C who were successfully treated for their infection (estimated to be <5%) could not be identified from the administrative sources and, therefore, would have been retained within the prevalence calculations.
CONCLUSION
The present large population-based study spanned a 12-year period of data accrual and described a North American Indigenous population in which HCV infections occur in a significantly younger age group, that are more often female and residents of urban communities. It also described a burden of hepatitis C that is increasing at a greater rate than in the non-First Nations population. These findings should serve as an important baseline for future primary prevention and therapeutic intervention strategies.
Footnotes
DISCLOSURES: This research was supported by the Health Canada/CIHR Research Initiative on Hepatitis C – Operating grant. The results and conclusions presented are those of the authors. No official endorsement by Manitoba Health is intended or should be inferred
REFERENCES
- 1.WHO. Viral Cancers. < www.who.int/vaccine_research/diseases/viral_cancers/en/print.html> (Accessed June 24, 2008)
- 2.Alter MJ, Kruszon-Moran D, Nainan OV, et al. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med. 1999;341:556–62. doi: 10.1056/NEJM199908193410802. [DOI] [PubMed] [Google Scholar]
- 3.Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The prevalence of hepatitis C virus infections in the United States, 1999 through 2002. Ann Intern Med. 2006;144:705–14. doi: 10.7326/0003-4819-144-10-200605160-00004. [DOI] [PubMed] [Google Scholar]
- 4.Remis R. Estimating the number of blood transfusion recipients infected by hepatitis C virus in Canada, 1960–85 and 1990–92. Ottawa: Health Canada; 1998. [Google Scholar]
- 5.Patrick DM, Tyndall MW, Cornelisse PG, et al. Incidence of hepatitis C virus infection among injection drug users during an outbreak of HIV infection. CMAJ. 2001;165:889–95. [PMC free article] [PubMed] [Google Scholar]
- 6.Riben P, Bailey G, Hudson S, McCulloch K, Dignan T, Martin D. Hepatitis C in Canada’s First Nations and Inuit populations: An unknown burden. Can J Publ Health. 2000;91(Suppl 1):S16–S17. [PubMed] [Google Scholar]
- 7.Moses S, Mestery K, Kaita KDE, Minuk GY. Viral hepatitis in a Canadian street-involved population. Can J Publ Health. 2002;93:123–8. doi: 10.1007/BF03404552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Siushansian J, Archibald CP, Lior LY, Sutherland D, Hudson S, Vooght M, Young E. Northern Exposures: HIV and HCV spread among injection drug users in a small Canadian community. Int Conf AIDS. 2000 Jul 9 to 14;13 (abstract #ThPeD5482) < ww1.aegis.org/conferences/iac/2000/ThPeD5482.html> (Accessed November 30, 2012) [Google Scholar]
- 9.Higgins B. Issues relating to hepatitis C and HIV infection in prison; Proceedings from the First Aboriginal Hepatitis C Conference; April 30 to May 3, 2002; Edmonton. [Google Scholar]
- 10.Strathdee SA, Patrick DM, Currie SL, et al. Needle exchange is not enough: Lessons from the Vancouver injecting drug use study. AIDS. 1997;11:F59–65. doi: 10.1097/00002030-199708000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Ford PM, White C, Kaufmann H, et al. Voluntary anonymous linked study of the prevalence of HIV infection and hepatitis C among inmates in a Canadian federal penitentiary for women. CMAJ. 1995;153:1605–9. [PMC free article] [PubMed] [Google Scholar]
- 12.Ford PM, Pearson M, Sankar-Mistry P, Stevenson T, Bell D, Austin J. HIV, Hepatitis C and risk behaviour in a Canadian medium-security federal penitentiary. QJM. 2000;93:113–9. doi: 10.1093/qjmed/93.2.113. [DOI] [PubMed] [Google Scholar]
- 13.Manitoba Centre for Health Policy. Concept Dictionary and Glossary: Residential Mobility. <http://mchp-appserv.cpe.umanitoba.ca/viewConcept.php?conceptID=1216> (Accessed January 5, 2012)
- 14.Roos LL, Mustard CA, Nicol JP, et al. Registries and administrative data: Organization and accuracy. Med Care. 1993;31:201–12. doi: 10.1097/00005650-199303000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Dawood M, Smart G, Wood M, Wu H-X, Paton S, Wu J. Hepatitis C virus infection among First Nation and non-First Nation people in Manitoba, Canada – a public health laboratory study. Can J Microbiol. 2006;52:999–1005. doi: 10.1139/w06-056. [DOI] [PubMed] [Google Scholar]
- 16.Jebamani LS, Burchill CA, Martens PJ. Using data linkage to identify First Nations Manitobans. Can J Publ Health. 2005;96(Suppl 1):S28–32. doi: 10.1007/BF03405313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martens PJ, Bond R, Jebamani L, et al. The Health and Health Care Use of Registered First Nations People Living in Manitoba: A Population-based study. < http://mchp-appserv.cpe.umanitoba.ca/deliverablesList.html> (Accessed January 5, 2012).
- 18.Uhanova J, Tate RB, Tataryn DJ, Minuk GY. A population-based study of the epidemiology of hepatitis C in a North American population. J Hepatol. 2012;57:736–42. doi: 10.1016/j.jhep.2012.05.018. [DOI] [PubMed] [Google Scholar]
- 19.Statistics Canada. Profile of Age and Sex, for Canada, Provinces, Territories, Census Divisions and Census Subdivisions, 2001 Census. < www12.statcan.ca/english/census01/products/standard/themes/Rp-eng.cfm?LANG=E&APATH=3&DETAIL=0&DIM=0&FL=A&FREE=0&GC=0&GID=0&GK=0&GRP=1&PID=55522&PRID=0&PTYPE=55430,53293,55440,55496,71090&S=0&SHOWALL=0&SUB=0&Temporal=2001&THEME=37&VID=0&VNAMEE=&VNAMEF> (Accessed December 15, 2012) [Google Scholar]
- 20.Manitoba Health. Population Reports. < www.gov.mb.ca/health/population/index.html> (Accessed December 15, 2012)
- 21.Wu H-X, Wu J, Wong T, et al. Enhanced surveillance of newly acquired hepatitis C virus infection in Canada, 1998 to 2004. Scand J Infect Dis. 2006;38:482–9. doi: 10.1080/00365540500525161. [DOI] [PubMed] [Google Scholar]
- 22.Elliott L, Blanchard J, Dawood M, Beaudoin C, Dinner K. The Winnipeg Injection Drug Epidemiology (WIDE): A study of the epidemiology of injection use and HIV infection in Winnipeg, Manitoba: Final Report. Winnipeg: Epidemiology Unit, Public Health and Epidemiology, Manitoba Health; 1999. [Google Scholar]
- 23.Callaghan RC, Cull R, Vettese LC, Taylor L. A gendered analysis of Canadian Aboriginal individuals admitted to inpatient substance abuse detoxification: A three-year medical chart review. Am J Addict. 2006;15:380–6. doi: 10.1080/10550490600860270. [DOI] [PubMed] [Google Scholar]
- 24.Mehrabadi A, Craib KJP, Patterson K, et al. The Cedar Project: A comparison of HIV-related vulnerabilities amongst young Aboriginal women surviving drug use and sex work in two Canadian cities. Int J Drug Policy. 2008;19:159–68. doi: 10.1016/j.drugpo.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 25.Mehrabadi A, Paterson K, Pearce M, et al. for the Cedar Project Partnership Gender differences in HIV and hepatitis C related vulnerabilities among Aboriginal young people who use street drugs in two Canadian cities. Women Health. 2008;48:235–60. doi: 10.1080/03630240802463186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilson C. Hepatitis C infection and type 2 diabetes in American-Indian women. Diabetes Care. 2004;27:2116–9. doi: 10.2337/diacare.27.9.2116. [DOI] [PubMed] [Google Scholar]
- 27.McMahon BJ, Hennessy TW, Christensen C, et al. Epidemiology and risk factors for hepatitis C in Alaska Natives. Hepatology. 2004;39:325–32. doi: 10.1002/hep.20046. [DOI] [PubMed] [Google Scholar]
- 28.Remis RS. Modelling the Incidence and Prevalence of Hepatitis C Infection and its Sequelae in Canada, 2007 Final Report. Community Acquired Infections Division Centre for Communicable Diseases and Infection Control Infectious Disease and Emergency Preparedness Branch Public Health Agency of Canada 2009; Catalogue NumberHP40-39/2009E-PDF; ISBN 978-1-100-12614-2. < www.phac-aspc.gc.ca/sti-its-surv-epi/model/pdf/model07-eng.pdf> (Accessed October 5, 2012)
- 29.Epi-Update. Hepatitis C virus (HCV) among Aboriginal people surveyed by three national enhanced surveillance systems in Canada. Her Majesty the Queen in Right of Canada, 2010. Cat.: HP40-52/2010E-PDF. ISBN: 978-1-100-17219-4 <www.phac-aspc.gc.ca/sti-its-surv-epi/pdf/hepcaboriginal-autochtones-eng.pdf> (Accessed January 12, 2012)
- 30.US department of Human Services, Office of Minority Health. Hepatitis and American Indians/Alaska Natives <http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=3&lvlid=541> (Accessed February 3, 2012).
- 31.Sherman M, Shafran SK, Burak K, et al. Management of chronic Hepatitis C: Consensus guidelines. Can J Gastroenterol. 2007;21(Suppl C):25C–34C. [PMC free article] [PubMed] [Google Scholar]


