Abstract
Background:
Acute urinary retention (AUR) is one of the most serious complications of benign prostatic hypertrophy. This study was done to predict the outcome of trial of voiding without catheter (TWOC) in patients with AUR with intravesical prostatic protrusion (IPP) detected on transabdominal ultrasound. Other factors such as prostatic volume and patient’s age were also assessed.
Methods:
Patients with a first episode of AUR secondary to benign prostatic hypertrophy were assessed with ultrasound following bladder catheterization. The IPP was measured and graded (grade 1 is 5 mm or less, grade 2 is 5–10 mm and grade 3 is more than 10 mm). Success of TWOC was then correlated with the degree of IPP.
Results:
A total of 32 patients with AUR were included in the study. Patients with grade 3 IPP were found to have a significant failure rate compared to grade 1 (P = 0.022) and grade 2 (P = 0.041).
Conclusion:
Intravesical prostatic protrusion is a useful predictor of success of TWOC in patients with AUR. Patients with grade 3 IPP on ultrasound would benefit from TWOC and warrant earlier definitive surgical treatment.
Keywords: acute urinary retention, benign prostatic hypertrophy, intravesical prostatic protrusion, prostate volume, trial of micturation without catheter
Introduction
Acute urinary retention (AUR) is one of the most serious complications of benign prostatic hyperplasia (BPH). Well-controlled studies have estimated the frequency of this complication to be about 5–25 per 1000 person-years or 0.5% to 2.5% per year. However, the risk is cumulative and increases with age (1).
The immediate management of this complication is urethral catheterization. In the past, most of these patients would then undergo transurethral prostate resection (TURP) as the gold standard of definitive treatment. However, studies have shown that the success of trial of voiding without catheter (TWOC), which is defined as the point at which the patient can regain self-voiding and be free of AUR for at least a year (2,3), ranges from 23% to 58% (3–5). Thus, the conventional wisdom of a routine TURP following AUR is questionable (6).
Transabdominal ultrasound has been proven useful in assessment of the prostate gland. Intravesical prostatic protrusion (IPP) seen on ultrasound is defined as the degree of protrusion of the prostate into the urinary bladder. It has been shown to correlate well with predicting bladder outlet obstruction in patients with BPH (7,8).
The purpose of this study is to assess whether the degree of IPP can predict the outcome of a trial of voiding without catheter following a first episode of AUR. If a higher degree of protrusion is associated with a higher failure rate, then these patients can be considered for an earlier invasive TURP.
IPP is not routinely done as part of the assessment on ultrasound in our setting, especially in the radiology department, and the present article serves to emphasize the importance of recording this parameter during scanning.
Materials and Methods
This was a prospective study done for a period of 6 months. Ethical approval was obtained from the Research and Ethics Committee, Faculty of Medicine, Universiti Kebangsaan Malaysia. Written informed consent was taken from all the participants.
The study encompassed all male patients who presented with a first episode of acute urinary retention to the Accident and Emergency Department, Universiti Kebangsaan Malaysia Medical Centre (UKMMC). These patients were catheterised and admitted to the urology ward. Transabdominal ultrasound was done within 48 h after admission using a 3.5 MHz curvilinear probe. The patient’s age was recorded, along with degree of IPP and prostatic volume measurement after urinary bladder filling of 200 mL of normal saline. The upper urinary tracts were also assessed.
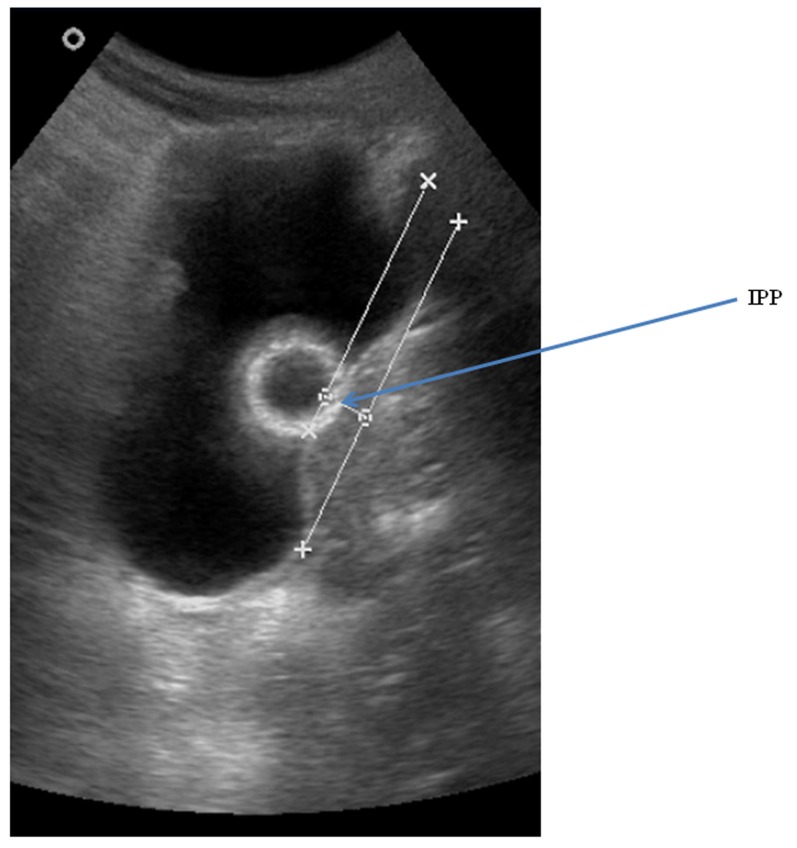
Intravesical prostatic protrusion (IPP) was measured from the protruding prostate tip perpendicularly down to the bladder circumference at prostate base taken at midsagittal view (Figure 1). Grade 1 is assigned if the protruding tip is 5 mm or less, grade 2 when the tip is between 5 mm and 10 mm and grade 3 when the tip is more than 10 mm. Prostate volume is measured in both transverse and sagittal planes using an ellipsoid formula keyed into the computer of the ultrasound machine. The ellipsoid formula of prostate volume (in gram, g) = height (cm) × width (cm) × anteroposterior (AP) diameter (cm) × π/6. Three different measurements were taken for IPP and prostate volume and the average of these measurements was then recorded.
Figure 1:
Intravesical prostatic protrusion (IPP) measured on transabdominal ultrasound.
Patients with diagnoses of prostate cancer, recurrent or chronic urinary retention, urinary tract infection, renal impairment, bladder or urethral stones, bilateral hydronephrosis or those with neurological disorders affecting continence, such as cerebral vascular accident, were excluded from the study.
Trial of voiding without catheter was done in the urology ward or clinic within 10 days after presentation of AUR. Uroflowmetry test was done during voiding and the post-void residual urine was measured by transabdominal ultrasound. Voiding was judged to be unsuccessful if the postvoid residual urine was greater than 150 mL on ultrasound and a maximal flow rate was less than 10 mL per second on the uroflowmetry test.
Patient’s age, degree of IPP and prostate volume were then correlated with the success of trial of voiding without catheter. Statistical analysis was done with computer software SPSS version 12.0. Comparison between grades of IPP with failure of trial voiding was analysed using Fisher’s exact test. An independent t test was used to assess the significance of the success or failure in relation to the age of patients, while the significance of prostate volume was subjected to a Mann-Whitney test in light of the non-normal distribution of data. Two-sided tests were used for all the statistical hypothesis tests mentioned above.
Results
A total of 34 patients were assessed with ultrasound following catheterization for acute urinary retention. Thirty-two patients who later came for the trial of voiding without catheter comprised the total number of patients in this study. The mean age of patient was 70.5 years (range 53–88 years) and the mean (SD) prostatic volume was 57.4 (30.2) g . Sixteen (50%) patients out of 32 had a successful trial of voiding after catheter removal.
Of the 32 patients with AUR, eight (25%) were found to have grade 1 IPP, seven (21.9%) grade 2 and 17 (53.1%) grade 3. The overall results are listed in Table 1.
Table 1.
Parameters/factors studied that affect the outcome of trial of voiding without catheter
| Successful TWOC | Failed TWOC | P value | |
|---|---|---|---|
| No. of patients | 16.0 | 16.0 | |
| Mean age in years (range) | 72.5 (57–88) | 68.5 (53–84) | 0.973 |
| Mean prostate volume, g | 12.38 (20–90.1) | 20.63 (32.8–194) | 0.013 |
| No. of IPP grade (%) | |||
| Grade 1 | 7.0 (87.5%) | 1.0 (12.5%) | |
| Grade 2 | 6.0 (85.7%) | 1.0 (14.3%) | |
| Grade 3 | 3.0 (17.6%) | 14.0 (82.4%) |
The failure rate of TWOC was 12.5% (1 of 8), 14.3% (1 of 7) and 82.4% (14 of 17) for grade 1, grade 2 and grade 3 IPP, respectively. Grade 3 IPP was found to be a significant factor in those who had successful as opposed to failed trial of voiding. The difference was also significant when an intergrade comparison was made in patients with failed TWOC. A significant difference was noted when comparing grades 1 and 3 (P = 0.022), as well as grades 2 and 3 (P = 0.041), using a two-sided Fisher’s exact test in these patients. No significant difference was calculated between grade 1 and 2 (P = 1.000) in this similar group.
Mean prostate volume in the successful group and the failed group was 12.38 g and 20.63 g, respectively. This parameter was found to be a significant factor in predicting the outcome of a voiding trial in our study (P = 0.013).
Age of patients had no significant influence in the outcome of TWOC (P = 0.973).
Discussion
Benign prostatic hyperplasia (BPH) is one of the commonest diseases of ageing men. It is associated with lower urinary tract symptoms such as incomplete emptying, frequency of urination and intermittent urination and urgency (9). Acute urinary retention (AUR) is one of the most serious complications of BPH. Current standard management of AUR is initial bladder catheterization for decompression. Alpha-blocker medication is started at the same time, which has been shown to improve the success rate during trial of voiding without catheter (TWOC) (10,11). The patient should then undergo at least one TWOC (usually within 10 days post-catheterization) before TURP is considered.
The previous practice of subjecting all patients to TWOC following an episode of AUR has been questioned, as up to 23% of patients with AUR secondary to BPH do not require surgery (12). Thus, useful parameters seen on ultrasound that can predict the outcome of TWOC are beneficial. Those who have a high risk of failure of TWOC can be more selectively considered and counselled for an urgent or earlier TURP procedure, even without TWOC.
Our present study revealed that, grade 3 IPP is a strong predictor in the failure outcome of a TWOC. This finding concurs with results from other studies (6,13), notably one done in Singapore by Foo et al. (6). The study also did a six months follow up, in which four patients who initially had successful TWOC had a repeated episode of AUR. Three of these patients were of grade 3 and one of grade 2 IPP. Grade 3 IPP is also associated with a higher bladder outlet obstruction index than grade 1 and 2 patients with BPH (7).
This indicates that prostatic configuration, i.e. IPP, which represents the median and/or lateral lobes of the prostate that are protruding into the bladder base, does contribute to bladder obstruction. Thus, a higher degree of IPP results in a higher failure rate of TWOC.
A limitation to this study is the small number of subjects owing to time constraint. No significant difference was noted between patients with grade 1 and 2 IPP in those with failed TWOC in our study. A previous study by Foo et al., demonstrated that there were significantly more patients with higher grade IPP in the group with failed TWOC than those with successful TWOC (Chi-square trend P = 0.007). Their failure rate of TWOC was reported as 36% (13 of 36), 58% (11 of 19) and 67% (30 of 45) for grades 1, 2 and 3 IPP, respectively. A larger study population may yield better results.
Prostatic size is another factor that was found to be significant in influencing the outcome of TWOC in our study (P = 0.013). The larger the prostate size, the greater the resultant obstruction. However, this parameter is still controversial, with a few contradictory negative results (3,6), although other studies, including one done by Seo et al., involving a large study population of 238 patients, concluded that prostate volume was a significant predictor of the outcome of TWOC (5,11,14).
Even though BPH patients with a prostate volume of 40 g seem to have three times the risk of developing AUR (12), there is no specific cutoff value of prostate volume that has been consistently proven to correlate with the success of TWOC (3,5,6,11). As seen in this study, there can be a wide range of prostate volume measurements in patients presenting with AUR. AUR can occur even though the prostate is not diffusely enlarged (< 25 g); this may happen when the disease process occurs focally in the periurethral zone of the gland.
Age at the time of AUR presentation is not a significant factor in the prediction of outcome of TWOC in this study, consistent with others (2,4,6,11).
Conclusion
Our study concludes that IPP and prostate volume are good predictors of the outcome of TWOC in patients with AUR. Patients with high grade IPP (> 10 mm) would benefit from TWOC and can be considered for more immediate or urgent TURP following an episode of AUR.
Acknowledgments
The authors thank Siti Farizwana Mohd Ridzwan for editing and formatting the manuscript.
Footnotes
Authors’ contributions
Drafting and final approval of the article: OSS
Conception and design, provision of study materials or patients: ZZ
Critical revision of the article for important intellectual content: AHH
Conflict of interest
We declare no conflicts of interest for this study.
Funds
None.
References
- 1.Roehrborn CG. Acute urinary retention: risks and management. Rev Urol. 2005;7(4):31–41. [PMC free article] [PubMed] [Google Scholar]
- 2.Blandy J. Emergency situations: acute retention of urine. Br J Hosp Med. 1978;19(2):109–111. [PubMed] [Google Scholar]
- 3.Bae JH, Kang SH, Cheon J, Ko YH, Cho DY, Lee G, editors. Determinant factors affecting successful voiding trial without catheter (TWOC) after single intermittent catheterization for the acute urinary retention patients due to benign prostatic obstruction. ICS 38th Scientific Meeting; 2008 Oct 20–24; Cairo, Egypt. ICS 2008. [Google Scholar]
- 4.Hastie KJ, Dickinson AJ, Ahmad R, Moisey CU. Acute retention of urine: is trial without catheter justified? J R Coll Surg Edinb. 1990;35(4):225–227. [PubMed] [Google Scholar]
- 5.Kumar V, Marr C, Bhuvangiri A, Irwin P. A prospective study of conservatively managed acute urinary retention: prostate size matters. BJU Int. 2000;86(7):816–819. doi: 10.1046/j.1464-410x.2000.00918.x. [DOI] [PubMed] [Google Scholar]
- 6.Foo KT, Tan YH. Intravesical prostatic protrusion predicts the outcome of a trial without catheter following acute urinary retention. J Urol. 2003;170(6):2339–2341. doi: 10.1097/01.ju.0000095474.86981.00. [DOI] [PubMed] [Google Scholar]
- 7.Chia SJ, Heng CT, Foo KT. Correlation of intravesical prostatic protrusion with bladder outlet obstruction. BJU Int. 2003;91(4):371–374. doi: 10.1046/j.1464-410x.2003.04088.x. [DOI] [PubMed] [Google Scholar]
- 8.Reis LO, Barreiro GC, Baracat J, Prudente A, D’Ancona CA. Intravesical protrusion of the prostate as a predictive method of bladder outlet obstruction. Int Braz J Urol. 2008;34(5):627–637. doi: 10.1590/s1677-55382008000500012. [DOI] [PubMed] [Google Scholar]
- 9.Agrawal CS, Chalise PR, Bhandari BB. Correlation of prostate volume with international prostate symptom score and quality of life in patient with benign prostatic hyperplasia. Nepal Med Coll. 2008;10(2):104–107. [PubMed] [Google Scholar]
- 10.Claus GR. Current medical therapies for men with lower urinary tract symptoms and benign prostatic hyperplasia: Achievements and limitations. Rev Urol. 2008;10(1):14–25. [PMC free article] [PubMed] [Google Scholar]
- 11.Shanmugasundaram R, Kekre NS. Is there a better indicator for predicting the outcome of trial without catheter? Indian J Urol. 2007;23(4):485–486. [PMC free article] [PubMed] [Google Scholar]
- 12.Claus GR. The epidemiology of acute urinary retention in benign prostatic hyperplasia. Rev in Urol. 2001;3(4):187–192. [PMC free article] [PubMed] [Google Scholar]
- 13.Mariappan P, Brown DJ, McNeill DS. Intravesical prostatic protrusion is better than prostate volume in predicting the outcome of trial without catheter in white men presenting with acute urinary retention: a prospective clinical study. J Urol. 2007;178(2):573–577. doi: 10.1016/j.juro.2007.03.116. [DOI] [PubMed] [Google Scholar]
- 14.McNeill AS, Rizvi S, Byrne DJ. Prostate size influences the outcome after presenting with acute urinary retention. BJU Int. 2004;94(4):559–562. doi: 10.1111/j.1464-410X.2004.05000.x. [DOI] [PubMed] [Google Scholar]