Abstract
A 42-year-old man from Ghana presented with bilateral painful corneal perforations following ingestion of a sulphur-based antibiotic. Emergency bilateral penetrating keratoplasty was performed, with restoration of globe integrity. However, surgical complications arose such as non-healing epithelial defect, secondary infection, graft dehiscence, and mounting intraocular pressure. This case illustrates the challenges faced in managing corneal grafts in patients with already compromised ocular surfaces.
Keywords: corneal perforation, epithelial defect, graft dehiscence, Stevens-Johnson syndrome, penetrating keratoplasty
Introduction
Stevens-Johnson syndrome (SJS) is a life-threatening skin condition. Corneal perforations have been reported (1), associated with corneal melting, and eventual blindness. The underlying pathology is thought to arise from an immune system disorder, resulting in inflammation, and its sequelae. In majority of cases, the cause is unknown, but certain medications, infections, and cancers have been implicated (2). Herein, we report a case of bilateral simultaneous corneal perforation in a patient not previously known to have SJS. We also discuss the complications following emergency bilateral penetrating keratoplasty in this case.
Case Presentation
A 42-year-old man from Ghana presented with bilateral ocular pain and rapid deterioration of vision over the past week, after having taken a course of a sulphur-based antibiotic three months earlier to treat an upper respiratory tract infection. The ocular symptoms of progressive discomfort, grittiness, and severe dryness, had reportedly commenced approximately one month after completing the antibiotic course. There were no respiratory symptoms. He also noticed blistering skin lesion on his hands and on regions of the oral mucosa, at the same time, he noticed the initial ocular symptoms. However, the patient did not seek any treatment for his skin or eye conditions prior to this presentation. He sought medical attention only after the sudden onset of significant impairment of vision in both his eyes, and the associated pain.
Examination of the eyes revealed copious bilateral mucus discharge, associated with central corneal perforations. There was iris plugging in the perforated sites, with corneal melting and thinning (Figure 1 and Figure 2). His visual acuity was light perception in the right eye, and hand motions in the left eye. Blistering skin lesions were noted on the extremities of both of the upper and lower limbs. There were no signs of infection.
Figure 1:
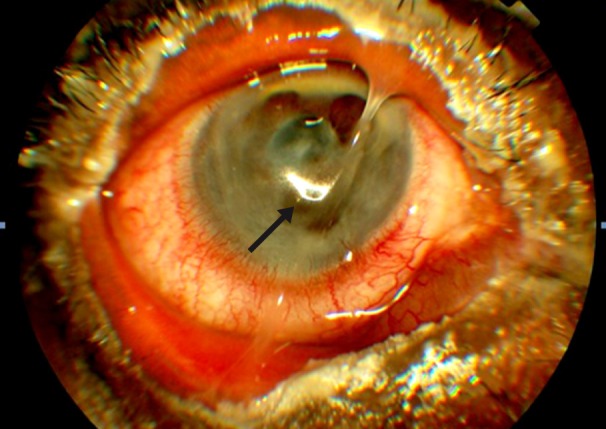
Left eye photo shows copius mucous discharge, corneal melting and perforation plugged by mucous (arrow).
Figure 2:
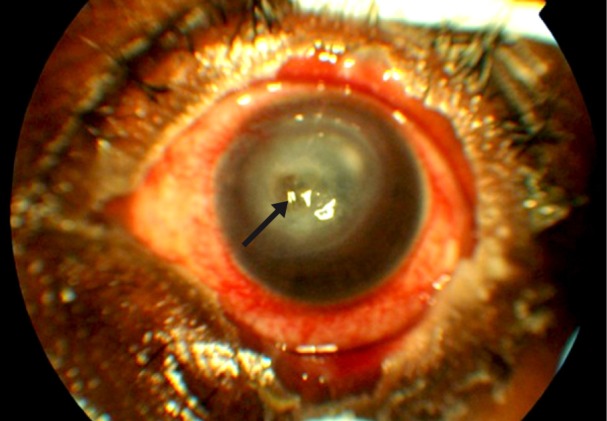
Right eye photo shows slighly less mucous discharge with obvius perforation plugged by iris (arrow).
Swabs were obtained from both eyes and sent for microbiology investigation. Culture and sensitivity was negative for any microbial infections. He was started on an immunosuppressive dose of oral corticosteroids and referred to a dermatology service. A diagnosis of Stevens- Johnson syndrome was made, mainly affecting the ocular system.
Emergency bilateral penetrating keratoplasties, and fresh-frozen amniotic membrane transplants were performed, as were cataract extraction and lens implantation of the right eye. The amniotic membrane, with the epithelial membrane facing up, was transplanted in an overlaying manner covering the entire corneal surface and part of the conjunctival surface, and sutured with 10-0 absorbable sutures. Post-operatively, visual acuity was counting fingers in the right eye, and 6/36 in the left eye, with resolution of pain (Figure 3). Mucuos discharge was also improved, and he reported feeling more comfortable. He was administered a topical preservative-free corticosteroid, antibiotic and cycloplegic agents, with continuation of the oral corticosteroid.
Figure 3:

Left eye photo post penetrating keratoplasty. Less mucous was noted, with persistent clean epithelial defect.
Both eyes suffered multiple post-operative complications. The right eye surgery was complicated by persistently high intraocular pressure. The patient also exhibited non-healing epithelial defect, further compounded by dendritic ulcer secondary to herpes simplex infection. He underwent right eye trabeculectomy without mitomycin C, two months after keratoplasty following resolution of the dendritic ulceration. Intraocular pressure was controlled with two antiglaucoma medications, namely gutt timolol maleate 0.5%, and gutt brimonidine tartarate 0.15%. A few weeks later, he developed a suture abscess. This led to suture loosening with eventual graft dehiscence on the left eye, necessitating resuturing of the graft. After sterilisation of the infection, the post-operative epithelial defect was successfully treated with topical umbilical cord serum.
Currently, he is still undergoing treatment for his ocular conditions with topical antibiotics, topical corticosteroid, and the two above mentioned antiglaucoma eye drops. Systemically, he is maintained on a slow taper of oral corticosteroids. There has been complete resolution of the skin lesions. At present, the best corrected visual acuity is 1/60 for the right eye, and 6/60 for the left.
Discussion
Stevens-Johnson syndrome (SJS) may result from hypersensitivity reactions to certain drugs, most notably sulphur-based medications. Ocular involvement accompanying SJS can include dry eyes, symblepharon formation, corneal conjunctivalisation, corneal melt, and even corneal perforation (3). These complications are difficult to treat, and treatment may require comprehensive interventions, including ocular surface reconstruction, limbal stem cells, and corneal transplant (3).
Spontaneous corneal perforations in SJS have been reported (4) as sequelae of the disease process, or adverse reactions to non-steroidal anti-inflammatory eyedrops. Rarely, corneal perforations occur simultaneously in both eyes due to severe and profound ocular inflammation, as in the case reported herein. Mucous membrane and skin involvement in SJS may occur simultaneously or in isolation. However, the severity of ocular involvement in SJS does not predict the development of subsequent complications (5). Likewise, the extensiveness of muco-cutaneous lesions does not predict the severity of ocular complications, often resulting in significant ocular morbidity occurring before patients eventually present to an ophthalmologist. Patients may present with sterile corneal melts, and secondary infections.
The acute phase of SJS may persists for up to six weeks, with less than 10% of patients presenting to an eye service within that period (3). Corneal melt in SJS with eventual ulcer formation may become infected, resulting in a poorer prognosis. In cases of corneal perforation, emergency tectonic and therapeutic full thickness penetrating keratoplasty is a necessity, in order to preserve globe integrity. Visual rehabilitation often becomes a secondary objective in these instances (6). However, a corneal graft may not be readily available at some centres, and a delay in performing this potentially vision -salvaging procedure is sometimes inevitable. The result of corneal graft surgery depends on many factors;, including tear film integrity, lid and conjunctival scarring, and corneal neovascularisation, all of which may be compromised in cases of SJS.
Epithelial defect following penetrating keratoplasty is common. Non-healing ulcers should be further investigated with regard to secondary infection or neurotrophic ulcer formation. Even if there is no previous history of herpes simplex virus infection, dendritic ulcer may still develop. The most common form of corneal involvement from herpes simplex virus infection is a geographic ulcer, followed by the classic dendritic type (7).
Healing of corneal epithelial defects occurs in stages, and requires adhesion to the underlying corneal stromal (8). Normal corneal wound healing requires growth factors, such as an epidermal growth factor, transforming growth factor β, and other cytokines, to induce proliferation of residual stem cells (9). Umbilical cord serum has been shown to be non-toxic and effective in expediting epithelial wound healing in neurotrophic corneal ulcers (10). Neurotrophic components, essential tear components, and growth factors contained in umbilical cord serum are also useful for the treatment of many other ocular surface diseases including dry eye syndrome (11), which is another component of ocular SJS.
Intraocular pressure elevation following penetrating keratoplasty is an expected, yet serious complication, and management of it can prove challenging. The incidence of glaucoma has been reported to be as high as 34% within 39 months following penetrating keratoplasty (12). Diagnosis is usually made within a year after the corneal transplant surgery, and patients may require surgery to control the rise in intraocular pressure. However, the results of glaucoma filtering surgery in such cases are variable (13). While trabeculectomy with adjunctive use of mitomycin C has been shown to achieve lower intraocular pressure compared to that achieved without using antiproliferative agents, corneal epithelial defect is a major concern (13). In patients with an already compromised ocular surface coupled with persistent epithelial defect following penetrating keratoplasty, trabeculectomy without antifibrotic agents may be a wise decision.
Conclusion
Rarely, Stevens-Johnson syndrome may present with severe ocular complications such as bilateral spontaneous corneal perforation, with minimal skin involvement. Careful history including recent medications is important in diagnosing the condition. The management of perforated cornea in such cases is invariably difficult and challenging. Post-operative complications following penetrating keratoplasty also pose a management issue, with regard to ensuring graft survival. Preservation of the globe is the main objective in performing penetrating keratoplasty in such cases, and visual rehabilitation becomes an important but secondary objective.
Acknowledgments
Encik Saiful Bahari (Science Officer) and Puan Nurul Azlina (Science Officer) for the photographs.
Footnotes
Authors’ Contributions
Conception and design, drafting of the article, and critical revision of the article for the important intellectual content: UKMN
Final approval of the article: TKY
References
- 1.Isawi H, Dhaliwal DK. Corneal melting and perforation In Stevens Johnson syndrome following topical bromfenac use. J Cat Ref Surg. 2007;33(9):1644–1646. doi: 10.1016/j.jcrs.2007.04.041. [DOI] [PubMed] [Google Scholar]
- 2.Teo L, Tay YK, Liu TT. Stevens- Johnson syndrome and toxic epidermal necrolysis: efficacy of intravenous immunoglobulin and a review of treatment options. Singapore Med J. 2009;50(1):29–33. [PubMed] [Google Scholar]
- 3.Kompella VB, Sangwan VS, Bansal AK, Garg P, Aasuri MK, Rao GN. Ophthalmic complications and management of Stevens– Johnson syndrome at a tertiary eye care centre in South India. Indian J Ophthalmol. 2002;50(4):283–286. [PubMed] [Google Scholar]
- 4.Tabarra KF, Shammas HS. Bilateral corneal perforation ins Stevens- Johnson Syndrome. Can J Ophthalmol. 1975;10(4):514–517. [PubMed] [Google Scholar]
- 5.Yip LW, Thong BY, Tan AW, Lim J, Wong HB, Handa S, et al. Ocular manifestations and complications of Stevens- Johnson syndrome and toxic epidermal necrolysis: an Asian series. Allergy. 2007;62(5):527–531. doi: 10.1111/j.1398-9995.2006.01295.x. [DOI] [PubMed] [Google Scholar]
- 6.Boujemaa C, Souissi K, Daghfous F, Marrakchi S, Jeddi A, Ayed S. Urgent penetrating keratoplasty in perforated infectious corneal ulcers. J Fr Ophthalmol. 2005;28(3):267–272. doi: 10.1016/s0181-5512(05)81053-8. [DOI] [PubMed] [Google Scholar]
- 7.Rezende RA, Uchoa UB, Raber IM, Rapuano CJ, Lainson PR, Cohen EJ, et al. New onset of herpes simplex virus epithelial keratitis after penetrating keratoplasty. Am J Ophthalmol. 2004;137(3):415–419. doi: 10.1016/j.ajo.2003.09.057. [DOI] [PubMed] [Google Scholar]
- 8.Dua HS, Forrester JV. Clinical patterns of corneal epithelial wound healing. Am J Ophthalmol. 1987;104(5):481–489. doi: 10.1016/s0002-9394(14)74105-4. [DOI] [PubMed] [Google Scholar]
- 9.Dua HS, Blanco AA. Amniotic membrane transplantation. Br J Ophthalmol. 1999;83(6):748–752. doi: 10.1136/bjo.83.6.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vajpayee RB, Mukerji N, Tandon R, Sharma N, Mollon JD, Maher ER, et al. Evaluation of cord serum therapy for persistent corneal epithelial defects. Br J Ophthalmol. 2003;87(11):1312–1316. doi: 10.1136/bjo.87.11.1312. doi: 10.1136/bjo.87.11.1312 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoon KY, You IC, Im SK, Jeong TS, Park YG, Choi J, et al. Application of umbilical cord serum eyedrops for the treatment of neurothrophic keratitis. J Ophthalmol. 2007;114(9):1637–1642. doi: 10.1016/j.ophtha.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 12.Yildirim N, Gursoy H, Sahin A, Ozer A, Colak E. Glaucoma after penetrating keratoplasty: incidence, risk factors and management. J Ophthalmol. 2011;2011(951294):6. doi: 10.1155/2011/951294. doi: doi:10.1155/2011/951294 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ishioka M, Shimazaki J, Yamagami J, Fujishima H, Shimmura S, Tsubota K. Trabeculectomy with mitomycin C for post- keratoplasty glaucoma. Br J Ophthalmol. 2000;84(7):714–717. doi: 10.1136/bjo.84.7.714. [DOI] [PMC free article] [PubMed] [Google Scholar]


