Abstract
Background
Several studies have been conducted in Iran in order to investigate the prevalence of depression among infertile couples. However, there is a remarkable diversity among the results. This meta-analysis was conducted to estimate an overall prevalence rate of depression among infertile couples in Iran.
Methods:
International and national electronic databases were searched up to June 2011 including MEDLINE, Science Citation Index Expanded, Scopus, SID, MagIran, and IranMedex as well as conference databases. Furthermore, reference lists of articles were screened and the studies’ authors were contacted for additional references. Cross-sectional studies addressing the prevalence of depression among infertile couples were included in this meta-analysis. We assessed 12 separate studies involving overall 2818 participants of which 1251 had depression.
Results:
Overall prevalence rate of depression among infertile couples was 0.47 (95% CI: 0.40, 0.55). The prevalence rate of depression was 0.44 (95% CI: 0.32, 0.56) during 2000 to 2005 and 0.50 (95% CI: 0.43, 0.57 during 2006 to 2011. The prevalence rate of depression was 0.46 (95% CI: 0.39, 0.53) among women and 0.47 (95% CI: 0.40, 0.54) among men.
Conclusion:
Not only the prevalence of depression in infertile couples was high but also had increasing growth in recent years. Furthermore, despite many studies conducted addressing the prevalence of depression in infertile couples, there is however a remarkable diversity between the results. Thus, one can hardly give a precise estimation of the prevalence rate of depression among infertile couples in Iran now.
Keywords: Depression, Infertility, Sterility, Meta-analysis, Cross-sectional, Prevalence, Iran
Introduction
Infertility is defined as not being able to get pregnant after one year of trying for women younger than 35 years of age or after six months for women equal to or older than 35 years of age (1). Almost 10% to 15% of couples experience infertility (2). Infertility may become a public health problem when its frequency exceeds 15% (3). Prevalence of infertility is highest in South/Central Asia, Sub-Saharan Africa, North Africa/Middle East, and Central/Eastern Europe (4). Prevalence of infertility among young women was estimated 10% in the United State (1), 11.5% to 15.7% in Canada (5), 12.6% in India (6), 1.72% in China (7).
Infertility is not always women’s problem. Both women and men may have problems that result in infertility. Almost one-third of infertility problems are due to women, another one-third of cases are caused by men and the other one-third of cases are caused by a combination of both women and men problems or by unknown reasons (1). However, irrespective of which couple is infertile, infertility is a serious psychological trauma and a terrible emotional distress for infertile couples ever (8). Depression is a common mental disorder affecting about 121 million people worldwide. This psychological disorder is usually diagnosed by a number of signs and symptoms like “depressed mood, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, low energy, and poor concentration”. Depression contributes to the global burden of diseases and is estimated to become the second leading cause of disability by the year 2020 (9).
Infertility has a tremendous psychological impact on infertile couples like anxiety and depression. This disorder may increase the duration of infertility. It is estimated that about 40% of infertile couples experience anxiety and 86% experience depression (10). Infertility has a great impact on quality of life and marital status of the couples that may eventually lead to divorce. Depression among infertile female is related to a number of factors such as cause and duration of infertility as well as education level and occupation (10).
Several studies have been conducted in Iran in order to investigate prevalence of depression among infertile couples. However, there is a remarkable diversity among the results, so that the prevalence of depression in infertile couples is reported from a minimum of <5% (11, 12) to a maximum of >50% (11, 13–17). Accordingly, performing a meta-analysis is invariable to summarize the studies’ results.
Thus, this meta-analysis was conducted in order to estimate an overall summary measure of prevalence rate of depression among infertile couples in Iran.
Methods
Definitions
The participants were considered infertility if they were not able to get pregnant after one year of trying. The women who could get pregnant but were unable to stay pregnant may also be considered as infertile (1). “Depression is a common mental disorder that presents with depressed mood, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, low energy, and poor concentration” (9). The participants were considered depressed if they had Beck Depression Inventory (BDI) score equal to or greater than 10 (18).
Criteria for including studies
We included all cross-sectional studies investigating the prevalence of depression among infertile couples, irrespective of publication status or language. Cohort and case-control studies were excluded. We included infertile couples, irrespective of type of infertility, or which couple was infertile, or whether or not they were under treatment. The exposure of interest was infertility. The outcome of interest was depression irrespective of duration and severity.
Search methods
We used and combined the following keywords: “(Depression OR Bipolar Disorder OR Unipolar disorders OR Depressive Disorder) AND (Infertility OR Sterility) AND Iran)”. We searched both international and national electronic databases as follows: MEDLINE (January 1950 to June 2011), Science Citation Index Expanded (January 1945 to June 2011), Scopus (November 2004 to August 2011), SID (January 2000 to August 2011), MagIran (January 2000 to August 2011), and IranMedex (January 2000 to August 2011). The following conference databases were also searched for unpublished data:
The 9th World Congress on Controversies in Obstetrics, Gynecology & Infertility (COGI), Barcelona, Spain, March 22–25, 2007; available from: www.comtecmed.com
The 13th World Congress on Controversies in Obstetrics, Gynecology & Infertility (COGI), German Society of Obstetrics & Gynecology. Berlin, Germany, November 4–7, 2010; available from: www.comtecmed.com
We also scanned the reference lists of all included studies for additional references. We contacted the authors of included studies for additional eligible studies.
Data collection and analysis
Title and abstract of the retrieved studies were screening to decide on which studies met the inclusion criteria of this meta-analysis. Then, the full texts of the eligible studies were reviewed and the necessary data were extracted and entered into an electronic datasheet. Two authors (SZM and JP) did this action. The authors were not blinded to the names of the studies’ authors, journals, and results. Any disagreements were resolved through discussion among the authors until consensus was reached. Eight items of STROBE checklist (19) were used to assess the risk of bias in the included studies. The studies with at most one unclear or inadequate quality component considered studies with low-risk of bias, otherwise as high-risk.
We explored statistical heterogeneity using the chi-squared (Chi2) test at the 5% significance level (P<0.05). We quantified inconsistency across studies results using I2 statistic (20). We also estimated the between-study variance using tau-squared (Tau2) statistic (21). We used funnel plot to investigate publication bias (21). In addition, we used Begg (22) and Egger (23) statistical tests to assess publication bias quantitatively. Both Review Manager 5 (24) and Statistical software Stata 11 (StataCorp, College Station, TX, USA) were employed for data analysis. Meta-analysis was performed to obtain summary measure of ‘prevalence rate’ of depression among infertile couples. Data were analyzed and the results were reported using a random effect model (25) with 95% CI.
Results
We retrieved 56 references up to August 2011, including 34 references through searching national electronic databases and 22 references through international databases. We also found six references through checking reference lists and two references through personal contact with studies’ authors. However, all of them were duplicated. No new reference was found through searching conference databases.
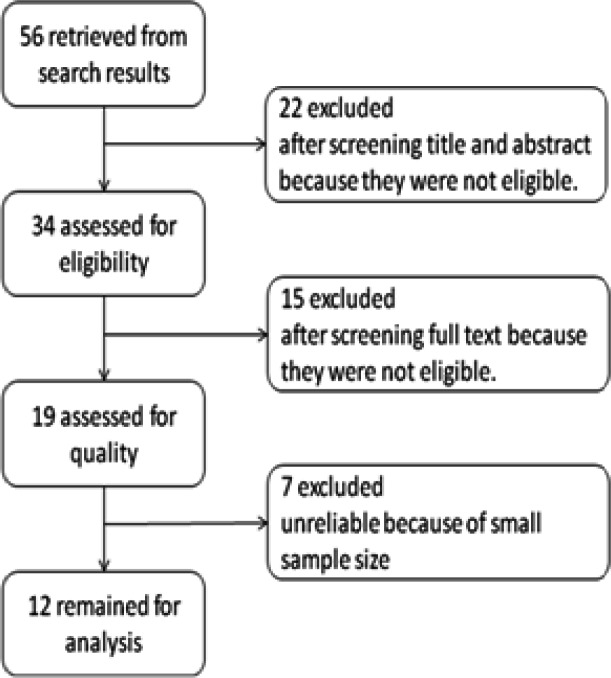
Of 56 references considered potentially eligible for this meta-analysis, 22 studies were excluded after screening the titles and abstracts and 15 studies after reviewing full texts. Furthermore, seven additional studies were excluded because of small sample size. The reason was that, assuming the prevalence rate of depression to be at most 50%, the minimum sample size of 96 would be needed in order to be able to make a correct estimation of the rate with 0.05 significant level and error level of 0.2. Thus, the studies with sample size less than 96 were excluded. Finally, 12 studies included for meta-analysis (Fig. 1).
Fig. 1:
Flow diagram of the progress through the phases of meta-analysis
Of 12 included studies, six studies were published in English (10, 13, 15, 26–28) and six studies in Persian (11, 14, 16, 24, 29, 30). Six studies (10, 11, 15, 16, 28, 30) were conducted during 2000 to 2005 and six studies during 2006 to 2011 (13, 14, 17, 26, 27, 29). Eight studies were carried out specifically on women (10, 11, 13–15, 17, 27, 30), one on men alone (26), two on both sex (16, 28) and one on both men and women separately (29). The less prevalence rate of depression among the infertile couples (25%) was reported by Yassini et al. (28) in Yazd city and the highest prevalence rate (79%) were related to the study, which was conducted by Najmi et al. in Isfahan city (16).
Prevalence of depression
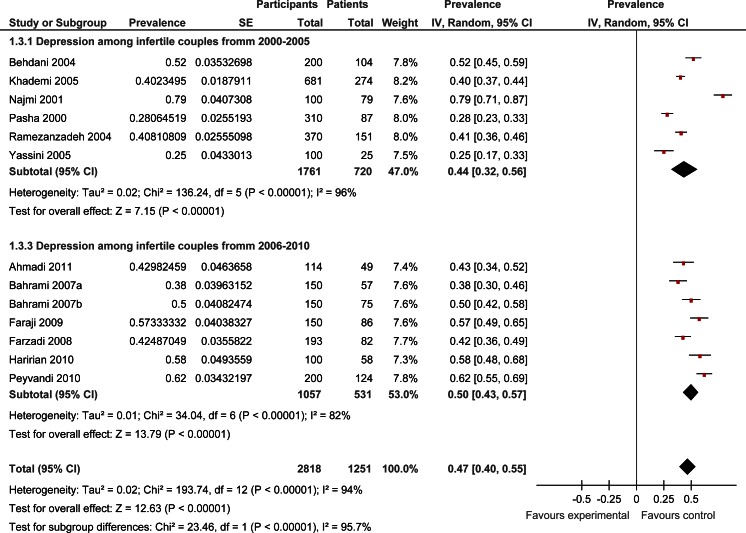
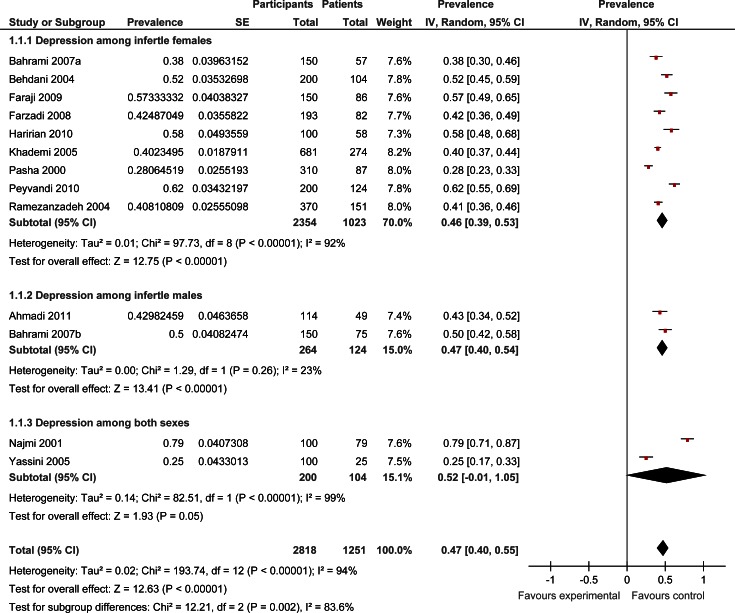
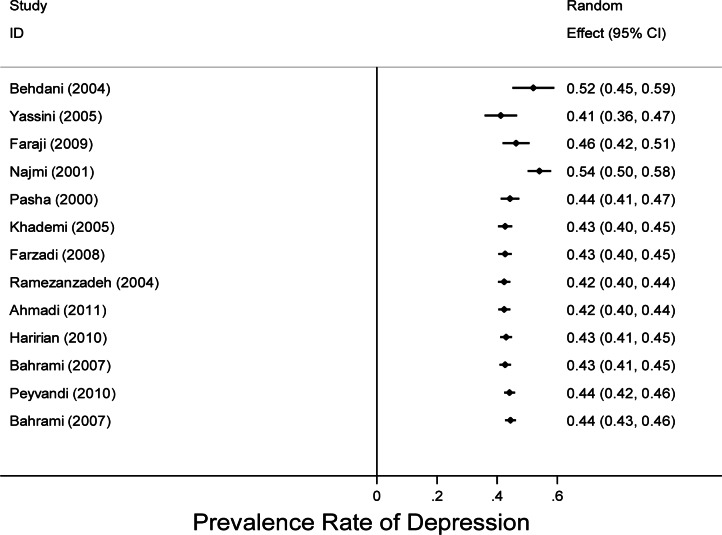
We included in the meta-analysis 12 studies with overall 2818 participants of which 1251 had depression. As shown in Fig. 2, the overall prevalence rate of depression among infertile couples was 0.47 (95% CI: 0.40, 0.55). The prevalence rate of depression was 0.44 (95% CI: 0.32, 0.56) during 2000 to 2005. However, the rate increased during subsequent years and reached 0.50(95% CI: 0.43, 0.57) during 2006 to 2011. In addition, as shown in Fig. 3, the prevalence rate of depression was 0.46 (95% CI: 0.39, 0.53) among women and 0.47 (95% CI: 0.40, 0.54) among men.
Fig. 2:
Forest plot of prevalence rate of depression among infertile couples by year
Fig. 3:
Forest plot of prevalence rate of depression among infertile couples by sex
Heterogeneity and publication bias
There was considerable heterogeneity among the included studies so that the result of Chi2 test for heterogeneity was highly significant. In addition, the I2 statistic was 94% (Fig. 2 and 3). In order to reduce the heterogeneity, we divided the studies into subgroups by year and gender. Nonetheless, homogeneity was not achieved except for subgroup of men. On the other hand, despite this significant heterogeneity, tau2 statistic was small and equal to 0.02 (Fig. 2 and 3).
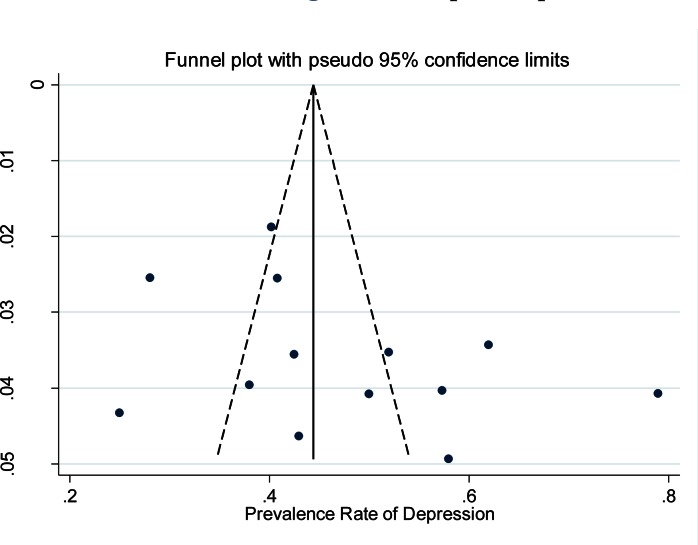
We assessed reporting bias using the funnel plot. The studies were distributed symmetrically around the vertical line indicating that no publication bias had occurred (Fig. 4). The statistical test for publication bias including Begg and Egger tests were not significant confirming absence of publication bias (P=0.272 and P=0.147 respectively).
Fig. 4:
Funnel plot for assessing publication bias in the included studies
The result of cumulative meta-analysis is presented in Fig. 5. The forest plot was not stable and turned either to the left or to the right. That means the available evidences are insufficient and additional studies are required.
Fig. 5:
Forest plot of cumulative meta-analysis for estimating the prevalence rate of depression among infertile couples
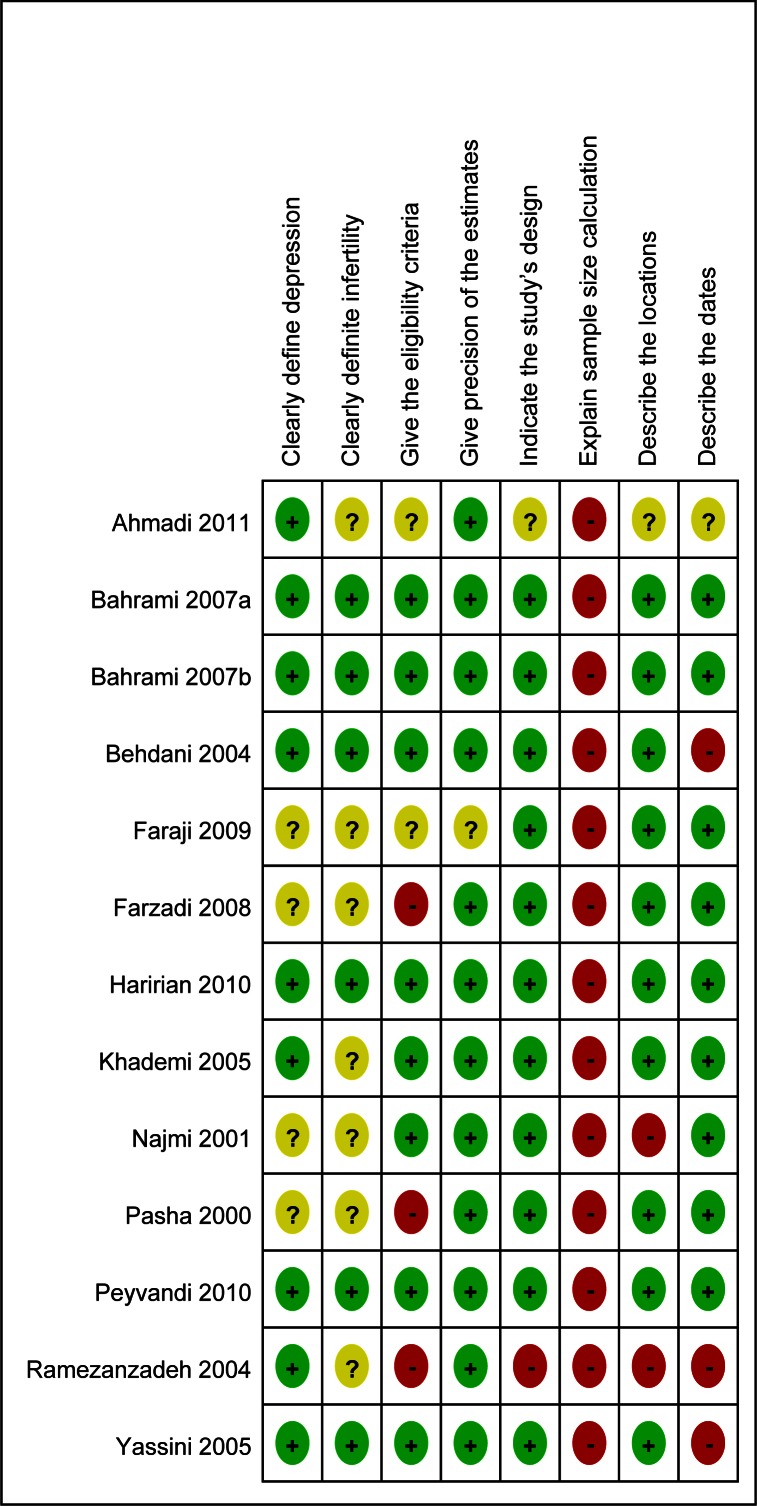
Quality of the included studies
There were three low-risk studies (14, 17, 29) and nine high-risk studies (10, 11, 13, 15, 16, 26–28, 30) among the included studies (Fig. 6). The subgroup analysis across the quality of the studies indicated that prevalence rate of depression among infertile couples was 0.52 (95% CI: 0.41, 0.63) based on the results of low-risk studies and 0.45 (95% CI: 0.36, 0.54) based on results of high-risk studies.
Fig. 6:
Risk of bias indicating the review authors’ judgments about each risk of bias item for each included study
Discussion
The results of this meta-analysis revealed that the prevalence of depression among infertile couples was very high so that nearly 50% of the infertile couples were affected with some degrees of mild, moderate or severe depression. Interestingly, the prevalence of depression in infertile couples had increased in recent years from 44% in the first half of the decade of the 2000s to 50% in the second half. This is should considered a serious warning that threat mental health of the infertile couples and should be the focus of special attention particularly by psychologists.
There was evidence of heterogeneity (small P value of Chi2 test and large I2 statistic) among the results of the included studies. However, care must be taken in the interpretation of the statistical tests for heterogeneity. The Chi2 test has low power when the sample size is small. On the other hand, the test has high power in detecting a small amount of heterogeneity that may be clinically unimportant when there are many studies in a meta-analysis (21), as was the case in our review. Therefore, we can attribute part of the observed heterogeneity to number of the studies (12 studies) included in the meta-analysis and large sample sizes (2818 participants). Another reason that can be posed to explain the observed heterogeneity is the presence of remarkable difference between the studies’ results. Despite several studies which have been conducted recently to address the prevalence of depression among infertile couples, the results were however much different. I2 statistic was 96% for the studies conducted in the first half of the decade. Whereas it decreased to 82% for the studies conducted in the second half. That means the discrepancy between the studies’ results is reducing in recent years. Nonetheless, there is still considerable diversity between the results, which may explain the observed heterogeneity.
Despite the significant observed heterogeneity, the tau2 statistic, which was used to investigate the between studies variance, was small and equal to 0.02. The reason that may explain this paradox is that tau2 would decrease when between-studies variance is low and hence within-studies variance is high (31), as was the case in this meta-analysis.
The prevalence rate of depression among infertile couples based on the results of low-risk studies was higher than that of high-risk studies (52% versus 45%). This discrepancy may be attributed to the quality of the studies. However, care must be taken for this interpretation. Because all low-risk studies were conducted in the second half of the decade of the 2000s, whereas, most of the high-risk studies were carried out in the first half. Thus, this increase in prevalence rate can also be attributed to the year of the studies rather than their quality.
Of 12 studies which were included in this meta-analysis, eight studies were carried out especially on women, three on both sexes and only one study on men alone. Accordingly, the overall prevalence of depression reported in this review has been more influenced by the prevalence of depression in women than in men, although there was no significant difference between the two sexes in terms of prevalence of depression (46% in women versus 47% in men).
The observed prevalence of depression among infertile couples was high. However, this problem is not unique to Iran. There are many evidences that show similar results in most parts of the world. A study conducted by Omu et al. (32) in Kuwait, showed that prevalence of depression was 5.2% in infertile women and 14.9% in men. Another study (33) in Taiwan, indicated that 40.2% of the infertile women had psychological disorders and 17% suffered from severe depression. A third study in Sweden on infertile couples, reported that major depression was the most common mood disorder among infertile couples with a prevalent rate of 10.9% in females and 5.1% in males (34). In addition, Upkong et al. carried out a cross-sectional study on infertile women in Nigeria and indicated that the prevalence of anxiety and depression in the infertile women was 37.5% and 42.9% respectively (35).
There were a few limitations and potential biases in this meta-analysis. First, the number of included studies investigating depression among infertile women was much more than that of men. This issue may raise the possibility of selection bias. Second, the BDI score equal to or greater than 10 was defined as standard cut-off for detecting patients with depression irrespective of the severity of the disease. Indeed, we could not categorize the depression among infertile couples. The reason was that some studies did not reported depression categorically or categorized depression differently. Third, we planned to perform subgroup analysis according to the duration of infertility and education level of the couples, but we could not, because data on the items were not stated in most of the studies.
Despite it limitation, the results of this meta-analysis could highlight an important and growing mental disorder among infertile couples that may be ignored. Depression, as a major mental disorder, should be the focus of special attention by gynecologists, who manage infertile couples, as policy makers, who plan preventive programs. However, many individual, social, and cultural characteristics play important role in both occurrence and exacerbation of depression especially among infertile couples. Depression may occur in people of any age, genders, or backgrounds. According to the reported of world health organization, depression contributes to the global burden of diseases and is estimated to become the second leading cause of disability by the year 2020 (9).
Conclusion
The result of this review showed that not only the prevalence of depression in infertile couples was high but also had increasing growth in recent years. In addition, despite many studies had been conducted addressing the prevalence of depression in infertile couples, there were however a remarkable diversity between the results. Thus, one can hardly give a precise estimation the prevalence rate of depression among infertile couples now in Iran. However, conduction a national survey may be helpful.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgments
This article is a part of PhD thesis supported by Shahroud University of Medical Sciences. We would like to thank Vic-Chancellor of Education as well as Vic-Chancellor of Research and Technology of Shahroud University of Medical Sciences for financial support of this study. The authors declare that they have no conflicts of interest.
References
- 1.Infertility FAQ’s. Centers for Disease Control and Prevention; Atlanta: CDC; 2012. [updated September 14, 2011; cited January 27, 2012]; Available: http://www.cdc.gov/reproductivehealth/Infertility/index.htm#1. [Google Scholar]
- 2.Schmidt L. Infertility and assisted reproduction in Denmark. Dan Med Bull. 2006;53:390–417. [PubMed] [Google Scholar]
- 3.World Health Organization. The Epidemiology of Infertility. WHO; Geneva: 1975. pp. 5–8. [Google Scholar]
- 4.Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. PLoS Med. 2012;9(12):e1001356. doi: 10.1371/journal.pmed.1001356. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bushnik T, Cook JL, Yuzpe AA, Tough S, Collins J. Estimating the prevalence of infertility in Canada. Hum Reprod. 2013;27(3):738–46. doi: 10.1093/humrep/der465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adamson PC, Krupp K, Freeman AH, Klausner JD, Reingold AL, Madhivanan P. Prevalence & correlates of primary nfertility among young women in Mysore, India. Indian J Med Res. 2011;134:440–6. [PMC free article] [PubMed] [Google Scholar]
- 7.Yang YQ, Shen H, Chen J, Chen ZW. A prevalence survey of infertility in Beijing, China. Zhongguo Bing Du Bing Za Zhi. 2011;91(5):313–6. [PubMed] [Google Scholar]
- 8.Boivin J, Griffiths E, Venetis CA. Emotional distress in infertile women and failure of assisted reproductive technologies: meta-analysis of prospective psychosocial studies. BMJ. 2011;342:d223. doi: 10.1136/bmj.d223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization . Depression. WHO; 2012. [cited January 26, 2012]; Available from: http://www.who.int/mental_health/management/depression/definition/en/. [Google Scholar]
- 10.Ramezanzadeh F, Aghssa MM, Abedinia N, Zayeri F, Khanafshar N, Shariat M, et al. A survey of relationship between anxiety, depression and duration of infertility. BMC Womens Health. 2004;4(1):9. doi: 10.1186/1472-6874-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Behdani F, Erfanian M, Hbrani P, Hogat K. Prevalence of depression and risk factors in infertile women referred to Montaserieh infertility clinic in Mashhad. The Journal of Fundamentals of Mental Health. 2004;6(23 & 24):141–6. [Google Scholar]
- 12.Behjati Ardekani Z, Mehdi Akhondi M, Kamali K, FazliKhalaf Z, Skandari S, Ghorbani B. Mental health status of patients attending Avecinna Infertility Clinic. Journal of Reproduction & Infertility. 2010;11(4):319–24. [Google Scholar]
- 13.Faraji R, Milani F, Danesh M. Realative frequeny of depression in infertile women, Rasht, Iran. Int J Gynecol Obstet. 2009;107(Supp 2):S174–S5. [Google Scholar]
- 14.Haririan HR, Mohammadpour Y, Aghajanloo A. Prevalence of depression and contributing factors of depression in the infertile women referred to Kosar Infertility Center, 2009. Int J Gynecol Obstet. 2010;13(2):45–9. [Google Scholar]
- 15.Khademi A, Alleyassin A, Aghahosseini M, Ramezanzadeh F, Abhari AA. Pretreatment Beck depression inventory score is an important predictor for post-treatment score in infertile patients: a before-after study. BMC Psychiatry. 2005;5(25) doi: 10.1186/1471-244X-5-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Najmi S, Ahmadi S, Ghassemi G. Psychological characteristic of infertile couples referring to Isfahan fertility and infertility center (IFIC) Jounal of Reproduction and Infertility. 2001;4(8):40–5. [Google Scholar]
- 17.Peyvandi S, Hosseini SH, Daneshpoor SMM, Mohammadpour RA, Qolami N. The prevalence of depression, anxiety and marital satisfaction and related factors in infertile women reffered to infertility clinics of Sari city in 2008. Journal of Mazandaran University of Medical Sciences. 2010;20(80):26–32. [Google Scholar]
- 18.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4(6):561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 19.Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4(10):1628–54. doi: 10.1371/journal.pmed.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Higgins JPT, Thompson SG, Deeks JJ, Altman D. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions Version 5.0.0: The Cochrane Collaboration. 2008. Available from: www.cochrane-handbook.org. [Google Scholar]
- 22.Begg CB, Mazumdar M. Operating characteristics of a rank cor relation test for publication bias. Biometrics. 1994;50(4):1088–101. [PubMed] [Google Scholar]
- 23.Egger M, Davey SG, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.RevMan. Review Manager (RevMan) [Computer program] (2008) RevMan. Version 5.0 for Windows. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; [Google Scholar]
- 25.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 26.Ahmadi H, Montaser-Kouhsari L, Nowroozi MR, Bazargan-Hejazi S. Male infertility and depression: a neglected problem in the Middle East. J Sex Med. 2011;8(3):824–30. doi: 10.1111/j.1743-6109.2010.02155.x. [DOI] [PubMed] [Google Scholar]
- 27.Farzadi L, Ghasemzadeh A. Two main independent predictors of depression among infertile women: an Asian experience. Taiwan J Obstet Gynecol. 2008;47(2):163–7. doi: 10.1016/S1028-4559(08)60074-1. [DOI] [PubMed] [Google Scholar]
- 28.Yassini M, Khalili MA, Hashemian Z. The level of anxiety and depression among Iranian infertile couples undergoing in vitro fertilization or intra cytoplasmic sperm injection cycles. J Res Med Sci. 2005;10(6):358–62. [Google Scholar]
- 29.Bahrami N, Sattarzadeh N, Koochaksaraiie F, Ghogazadeh M. Comparing depressin and sexual satisfaction in couple fertile & infertile. Journal of Reproduction & Infertility. 2007;8(1):52–9. [Google Scholar]
- 30.Pasha H. Evaluation of depression among infertile women using Beck and Hamilton test. Journal of Babol University of Medical Sciences. 2000;2(3):37–42. [Google Scholar]
- 31.Borenstein M, Hedges L, Rothstein H. Introduction to meta-analysis. In: Borenstein M, Hedges LV, Higgins JPT, Rothstein H, editors. Meta-analysis: fixed effect vs random effects. John Wiley and Sons Ltd; Chichester: 2007. pp. 11–21. [Google Scholar]
- 32.Omu FE, Omu AE. Emotional reaction to diagnosis of infertility in Kuwait and successful clients’ perception of nurses’ role during treatment. BMC Nursing. 2010;9(5) doi: 10.1186/1472-6955-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen TH, Chang SP, Tsai CF, Juang KD. Prevalence of depressive and anxiety disorders in an assisted reproductive technique clinic. Hum Reprod. 2004;19(10):2313–8. doi: 10.1093/humrep/deh414. [DOI] [PubMed] [Google Scholar]
- 34.Volgsten H, Skoog Svanberg A, Ekselius L, Lundkvist O, Sundstrom Poromaa I. Prevalence of psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment. Hum Reprod. 2008;23(9):2056–63. doi: 10.1093/humrep/den154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Upkong D, ORJİ EO. Mental Health of Infertile Women in Nigeria. Turk J Psychiat. 2006;17(4):1–7. [PubMed] [Google Scholar]