Abstract
Background
Whilst there seem to be available data on blood pressure profiles of South African children, especially in urban areas, few data exist on rural children. The aims of this study were to determine the blood pressure profiles of rural South African children residing in Thohoyandou; and to examine the relationship between body mass index and blood pressure among the children.
Methods:
The study involved 296 (134 boys and 135 girls) children aged 7–13 years. Body weight and height were measured using standard procedures. Overweight was defined by body mass index (BMI) for gender and age. Blood pressure was monitored in each child thrice using validated electronic devices (Omron 7051T). Hypertension was determined as the average of three separate blood pressure readings where the systolic or diastolic blood pressure was ≥ 90th percentile for age and sex.
Results:
Overweight among the girls (4.7%) was higher compared with the boys (3.9%). Both systolic and diastolic pressures (SBP and DBP) increase with age in both sexes. The proportion of children with > 90th percentile occur at only ages 12 and 13 years. The incidence of hypertension (SBP > 90th percentile) was 0.4% and 0.2% in boys and girls, respectively. The SBP and DBP pressures significantly (P<0.05) correlate with age; body mass, height and BMI.
Conclusion:
Elevated blood pressure is prevalent among rural South African children residing in this region. Also, blood pressure increased with age in both boys and girls, and this positively correlated with age, body weight, height and BMI.
Keywords: Overweight, Body mass index, Blood pressure, Rural children, South Africa
Introduction
Alongside obesity, elevated blood pressure has become an increasingly common health problem in children and adolescent. Blood pressure studies in children provide important epidemiological information which may help in controlling or modifying coronary risk factors (1). It is therefore imperative to screen for blood pressure in children in order to identify those at risk of developing hypertension later in life, as studies have shown that levels of blood pressure track over time, and children with elevated blood pressure are more likely to become hypertensive adults (2–3). Similarly, strong associations between overweight and elevated BP have been reported in children and adolescents (4–6).
It is postulated that overweight children and adolescents have a more than twofold increased risk of developing risk of pre-hypertension and more than fourfold increased risk of developing hypertension compared with those with normal weight (7). In South Africa, levels of overweight and obesity among children and adolescents are increasing. A recent study (8) comparing data from the South African National Youth Risk Behaviour Survey in 2002 and 2008 indicates upward trend in the level of overweight and obesity among the South African adolescents. The study revealed that among the male adolescents, overweight rates increased from 6.3% in 2002 to 11.0% in 2008; among female adolescents, overweight rates increased from 24.3% in 2002 to 29.0% in 2008. Obesity rates more than doubled among male adolescents from 1.6% in 2002 to 2.3% in 2008 and rose from 5.0% to 7.5% among female adolescents (8). This findings are of course expected, given that South Africa is undergoing socioeconomic transformation, with increasing urbanization (9,10), coupled with attendant lifestyle habits that tend to promote sedentariness and patronage of fast-foods restaurants, possible determinants of overweight and obesity among children and adolescents in the country. These factors may independently or interact with overweight and obesity to contribute to elevated blood pressure or hypertension among children and adolescents.
Granted that high blood pressure levels are predictive of later hypertension, a major global health problem with its high prevalence and association with increased risk of cardiovascular diseases in the context of the epidemiological transition (11–13), there is need to prevent hypertension in childhood. The American Heart Association recommends that all children aged 3 years and older should have yearly BP measurements (8). However, existing data on the profile of blood pressure in South Africa children are scarce, and have been derived largely from studies conducted in the urban settings. Few have been conducted on rural children. Besides, scanty data exist on BMI and BP in rural South African children.
This study examines the relationship between BMI and BP in primary school children in Thohoyandou. This study will add to the existing information on the profiles of blood pressure in rural South African children. In addition, knowledge of the dangers of overweight, obesity, and high blood pressure among children will help to inform public policy. This will aid in providing intervention strategies to prevent risk factors of life associated with high blood pressure in children.
Methods
The sample size included a total of 296 school children (134 boys and 135 girls) aged 7−13 years, residing in Thohoyandou. The data were collected from August–October 2011. The participants were selected from four schools in the region. The four schools were purposively selected due to logistical problems and it was more feasible to conduct the research in the selected schools in this region with the assistance of trained field workers who were Biokinetics and Sport Science students at the University of Venda, situated in the region. The pupils have similar socio-economic background. The population which is mainly Tshivenda speaking relies mainly on subsistence farming and very meagre financial support from males of the families working as migrant labourers within the mining sectors in the South and Gauteng. Most of Tshivenda live in remote places, characterized by poverty, illiteracy and nutritional disorders.
In each school, the classes were listed numerically (e.g. grades 7A, 7B, 7C, etc.) and a simple ballot system was used to select four classes whose pupils were eventually assessed. Also, using the official class registers, a stratified random sample of children was drawn from each class according to their age category and gender. Specifically, those who were aged 7−13 years; had no disability or suffering from serious ailments that could impair anthropometric measurement were included. Also, only children who were present on the day of measurement were measured.
The nature and scope of the study were explained to the children and their parents who gave informed consent. The study was approved by the Centre for Biokinetics, Recreation and Sport Science, University of Venda, South Africa. An information leaflet and informed consent form were administered to the head teachers, pupils and their parents or guardians who consented that the study be carried out.
Four trained research assistants, who were final-year students in the Centre for Biokinetics, Recreation and Sport Science, University of Venda, participated in the data collection. The research assistants have a specialized training in anthropometric and blood pressure measurements. None of the research assistants wore a white coat during examinations. Before data collection commenced, the pupils filled the demographic section of the data form indicating their age and gender.
Measures
Blood pressure was monitored using the Omron electronic blood pressure equipment recommended by the World Hypertension Society. It consists of a bladder which measures 13 × 25 cm and a snugly wrap. Hypertension was determined as the average of three separate BP readings where the systolic or diastolic BP was ≥ 90th percentile for age and sex (14).
A Martin anthropometer was used to measure height to the last 0.1 cm. Weight was measured using Tanita TBF 611 scales (Tanita UK Ltd., Middlesex, UK) to the nearest 0.1 kg. All measurements were taken according to the standard procedures suggested by the International Society for the Advancement of Kinanthropometry (ISAK) (15). Body mass index (BMI) was calculated as weight in kilograms divided by squared height in meters. International recommended BMI cut-off points for overweight and obesity for both boys and girls based on age were applied to the data (16).
Data analysis
Anthropometric and BP data were expressed as means, standard deviation and 95% confidence intervals (95% CI). The parametric t-test was used for comparisons of these variables stratified by sex. To determine the relationship between BP and anthropometric parameters, the Pearson correlation coefficient was applied. Data were analyzed using Statistical Package for the Social Sciences (SPSS) version 17.0. The level of statistical significance was set at P<0.05.
Results
The mean age of the participants was 9.7 ± 1.7 years. No significant difference was found for age between boys and girls (P = 0.205). The anthropometric and blood pressure measurements of the participants are shown in Table 1. There were no significant (P >0.05) gender differences in all the variables (body weight, height, BMI, systolic blood pressure, diastolic blood pressure) measured. Both systolic and diastolic pressures (SBP and DBP) seem to increase with age in both sexes (Table 2).
Table 1:
Mean and standard deviation (sd) for anthropometric measurements of the participants
| Variable | Boys (n = 134) Mean ± SD | Girls (n =135) Mean ± SD | Combined (n = 269) Mean ± SD | 95% CI | P-value |
|---|---|---|---|---|---|
| Age (yr) | 9.9±1.9 | 9.6±1.5 | 9.7±1.7 | 9.5–9.9 | 0.205 |
| Body mass (kg) | 36.5± 13.5 | 35.7 ±13.1 | 36.1 ±13.3 | 34.5–37.9 | 0.596 |
| Height (cm) | 139.4±5.2 | 140.7±5.8 | 139.8±5.6 | 137.8–142.1 | 0.871 |
| BMI (kg/m2) | 20.2±5.0 | 19.7±5.1 | 20.0±5.1 | 18.9–20.6 | 0.452 |
| SBP (mmHg) | 93.6±10.1 | 94.4±9.9 | 94.0±1.0 | 92.8–95.2 | 0.488 |
| DBP (mmHg) | 56.9±6.7 | 56.5±7.0 | 56.7±6.8 | 55.9–57.6 | 0.630 |
CI = Confidence Interval; SD = standard deviation; BMI = Body mass index; SBP = Systolic blood pressure; DBP = Diastolic blood pressure
Table 2:
Systolic and diastolic blood pressure of the participants according to age groups
| Age (yr) | Boys | Girls | Systolic blood pressure (mmHg) | P-value | Diastolic blood pressure (mmHg) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Boys (Mean±SD) | 95% CI | Girls (Mean±SD) | 95% CI | Boys (Mean±SD) | 95% CI | Girls (Mean±SD) | 95% CI | P-value | ||||
| 7 | 20 | 8 | 85.4±7.6 | 81.8–89.0 | 88.3±6.7 | 82.7–93.9 | 0.355 | 51.4±5.4 | 48.9–53.9 | 52.3±4.7 | 48.3–56.2 | 0.704 |
| 8 | 14 | 24 | 87.5±6.6 | 83.7–91.2 | 87.4±8.6 | 83.8–91.1 | 0.995 | 52.5±5.3 | 49.4–55.6 | 52.0±6.7 | 49.2–54.9 | 0.821 |
| 9 | 24 | 39 | 92.5±8.4 | 89.0–95.9 | 92.9±9.3 | 89.8–95.9 | 0.887 | 57.0±6.0 | 54.5–59.5 | 55.5±5.2 | 53.8–57.1 | 0.280 |
| 10 | 27 | 29 | 93.9±9.3 | 90.2–97.6 | 95.4±6.4 | 93.0–97.8 | 0.480 | 57.5±4.9 | 55.6–59.5 | 57.0±5.4 | 54.7–59.2 | 0.682 |
| 11 | 18 | 16 | 96.0±10.1 | 91.0–101.1 | 96.5±7.4 | 92.5–100.5 | 0.880 | 57.6±7.3 | 54.0–61.2 | 58.2±5.5 | 55.3–61.2 | 0.774 |
| 12 | 15 | 14 | 99.5±10.7 | 93.5–105.4 | 105.6±6.4 | 101.9–109.3 | 0.074 | 51.4±5.4 | 48.9–53.9 | 52.3±4.7 | 48.3–56.2 | 0.704 |
| 13 | 16 | 5 | 102.0±8.0 | 97.7–106.3 | 106.5±16.9 | 85.5–127.5 | 0.415 | 52.5±5.3 | 49.4–55.6 | 52.0±6.7 | 49.2–54.9 | 0.821 |
Statistically significant (P ≤ 0.05); CI = Confidence Interval
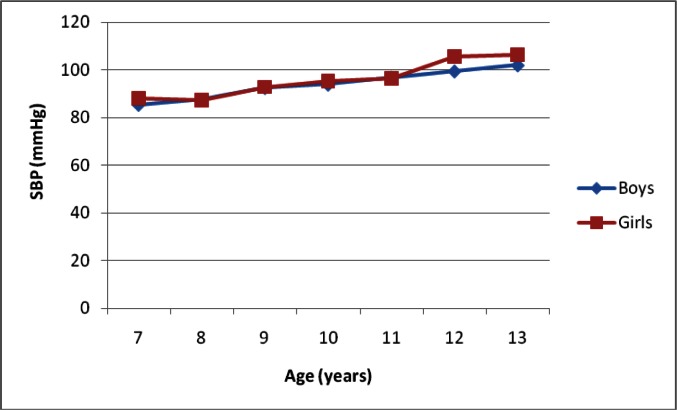
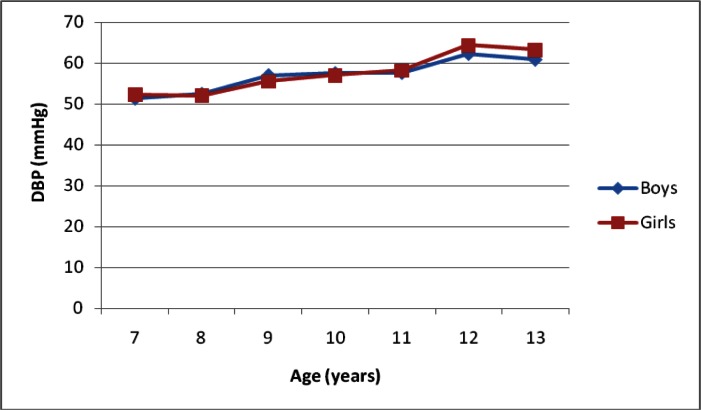
For both SBP and DBP, there was no significant difference (P ≥ 0.05) in both boys and girls at all ages. The SBP and DBP of the participants according to age and gender indicate a steady increase with age (Fig. 1 and 2). The SBP and DBP pressures significantly (P<0.05) correlate with age, body weight, height and BMI (Table 3). Shown in Table 4 is the distribution of the incidence of hypertension and the prevalence of overweight among the children according to sex and age. The proportion of children with > 90th percentile occur at only ages 12 and 13 years. The incidence of hypertension (SBP > 90th percentile) was 0.4% and 0.2% in boys and girls, respectively. In both sexes, overweight increases with age, declining at age 10 in boys, whereas in the girls a decline in overweight was observable at age 12 years. The percentage of children who were overweight were higher in girls (4.7%) compared with the boys (3.9%).
Fig. 1:
Variations in systolic blood pressure of the participants according to age and gender
Fig. 2:
Variations in diastolic blood pressure of the participants according to age and gender
Table 3:
Pearson correlation of systolic and diastolic blood pressure with age, stature, body mass, body mass index and body fat
| Variables | SBP (mmHg) | DBP (mm Hg) | ||
|---|---|---|---|---|
| R | P-value | R | P-value | |
| Age (years) | 0.515 | 0.001 | 0.485 | 0.001 |
| Height (cm) | 0.500 | 0.001 | 0.477 | 0.001 |
| Body mass (kg) | 0.622 | 0.001 | 0.635 | 0.001 |
| BMI (kg/m2) | 0.482 | 0.001 | 0.521 | 0.001 |
BMI = Body mass index; SBP = systolic blood pressure; DBP = diastolic blood pressure
Table 4:
Incidence of hypertension and overweight among the participants
| Age (years) | Gender (n) | Elevated blood pressure* | Overweight† | |||
|---|---|---|---|---|---|---|
| Boys | Girls | Boys % | Girls % | Boys % | Girls % | |
| 7 | 20 | 8 | 0 | 0 | 1.1 | 1.2 |
| 8 | 14 | 24 | 0 | 0 | 2.0 | 1.8 |
| 9 | 24 | 39 | 0 | 0 | 3.2 | 2.2 |
| 10 | 27 | 29 | 0 | 0 | 3.0 | 5.2 |
| 11 | 18 | 16 | 0 | 0 | 2.1 | 5.0 |
| 12 | 15 | 14 | 0.2 | 0.1 | 3.1 | 4.2 |
| 13 | 16 | 5 | 0.2 | 0.1 | 2.0 | 2.1 |
| Total | 134 | 135 | 0.4 | 0.2 | 3.9 | 4.7 |
The average SDP and DBP was determined as ≥ 90th percentile for age and sex [14];
Internationally recommended BMI cut-off points in children [16].
Discusssion
The present study presents the blood pressure profiles of rural South African school children attending primary schools in Thohoyandou, South Africa. High blood pressure is a serious risk factor. It is simply an elevated pressure of the blood in the arteries (17). The study demonstrates elevated BP in the children. This finding is not a new phenomenon among children. Previous similar studies conducted among South African children and adolescents (17–21) and elsewhere (22–26) have confirmed the existence of elevated or presence of hypertension among children and adolescents of similar ages with our sample in the present study. High blood pressure is a major risk factor for heart diseases and stroke in adulthood (27). As such, the presence of elevated BP found among the children in this region is worrisome. Early detection of high BP by regular montoring of the children is warranted and would help to improve the health care of the children.
Although overweight occur more in girls (4.7%), boys were found to be have higher levels of elevated BP (0.4%) compared to girls. Several studies (18, 23–26) have reported gender differences in the risk of developing elevated BP in different populations. It is difficult to explain the gender differences in elevated BP among our sample in the present study. There are several factors that have been thought to influence gender differences in the elevated BP among children.
The gendered pattern in the risk of elevated BP can be explained by the impact of sex steriods on BP (25); a factor strongly suggested by experimental models (28). It has been postulated too, that lifestyle behaviours such as physical and sedentary behaviour, could account for sex difference in elevated BP among children (29,30). Pate et al. (31) study invovling preschool-aged children found boys were more likely to engage in moderate-to-vigorous physical activity than girls (P = 0.01). We expect boys to be more physically active compared to girls. If this is the case, the direct BP-lowering effects of physical activity, such as increased capilliary formation (32) could have possibly results to a lower prevalence of high BP in boys. Nothwithstanding, physical activity was not assessed among our study sample, therefore, we cannot draw conclusion on the direct BP-lowering effects of physical activity. Identifying the factors influencing sex differences in the prevalence of high BP among young children is needed.
Elevated BP was found to be associated with age, weight, height and BMI in the children. Similar findings have been reported elsewhere (18,17,33–36). A direct relationship between high BP in childhood and subsequent development of the metabolic syndrome in adulthood has been observed (4,37). This stresses the need to screen and monitor the weight and BMI of children in order to safeguard their future health.
The present study has several limitations. The sampled population does not represent the children in Thohoyandou region, nor is it reflective of the province, or national level. As such, given the area and size of the sample, the generalization of study‘s findings must be done with caution. Additionally, due to financial and practical reasons, assessment of BP status was measured only at one visit, at difference with the NHBPEP criteria that require BP to be measured at least on three occasions. This could have affected the estimate of the prevalence of elevated BP in the sampled children. However, we measured BP in non-stress condition (no white coat); and in the analysis, BP was mainly considered as a continuous variable thus minimizing misclassification problems. Again, salt intake and urinary sodium excretion of the participants were not assessed nor were the birth weights of the children scrutinized as most of them were born in rural hospitals and clinics where accurate records are hardly kept (17). However, the strengths of the study include the examination of this phenomenon in an understudied rural region, using standardized anthropometric and BP measurement protocols.
Conclusion
The study affirm the occurrence of elevated blood pressure among rural South African children in Thohoyandou, South Africa; a finding which is consistent with other previous studies. Additionally, blood pressure increased with age among the boys and girls, and this is positively correlated with age, body weight, height and BMI. Given that elevated BP in children is a precursor to the development of cardiovascular diseases later in life; our findings highlight the need for routine measurement of BP as part of physical examination in school children. This would aid in identifying children with elevated BP, with the aim of instituting appropriate intervention measures.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgments
The authors declare that there is no conflict of interests.
References
- 1.Kamath VG, Parthage PM, Pattanshetty S, Kamath A, Balakrishnan A, Mishra T, et al. Prevalence of hypertension in the paediatric population in Coastal South India. Aust Med J. 2010;3(11):695–8. [Google Scholar]
- 2.Cheng X, Wang Y. Tracking of blood pressure from childhood to adulthood: A systematic review and meta-regulation analysis. J Cir. 2008;117(25):3171–80. doi: 10.1161/CIRCULATIONAHA.107.730366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vos LE, Oren A, Bots ML, Gorissen WH, Grobbee DE, Uiterwaal CS. Does a routinely measured blood pressure in young adolescence accurately predict hypertension and total cardiovascular risk in young adulthood? J Hypertens. 2003;21(11):2027–34. doi: 10.1097/00004872-200311000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Sun SS, Grave GD, Siervogel RM, Pickoff AA, Arslanian SS, Daniel SR. Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. J Paediatr. 2006;119(2):237–46. doi: 10.1542/peds.2006-2543. [DOI] [PubMed] [Google Scholar]
- 5.Moore WE, Stephens A, Wilson T, Eichner JE. Body mass index and blood pressure screening in a rural public school system: The Healthy Kids Project. Prev Chronic Dis. 2006;3(4):A114. [PMC free article] [PubMed] [Google Scholar]
- 6.Tarlton PA. Prevalence of elevated blood pressure in Hispanic versus non-Hispanic 6thgraders. J Sch Nurs. 2007;23(1):47–52. doi: 10.1177/10598405070230010801. [DOI] [PubMed] [Google Scholar]
- 7.Liang YJ, Xi B, Hu YH, Wang C, Liu JT, Yan YK, et al. Trends in the blood pressure and hypertension among Chinese children and adolescents: China Health and Nutrition Surveys 1991–2004. J Blood Pressure. 2011;20(1):45–53. doi: 10.3109/08037051.2010.524085. [DOI] [PubMed] [Google Scholar]
- 8.Reddy SP, Resnicow K, James S, Funani IN, Kambaran NS, Omardien RG, et al. Rapid increases in overweight and obesity among South African adolescents: comparison of data from the South African National Youth Risk Behaviour Survey in 2002 and 2008. Am J Publ Health. 2012;102(2):202–68. doi: 10.2105/AJPH.2011.300222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Armstrong MEG, Lambert MI, Sharwood KA, Lambert EV. Obesity and overweight in South African primary school children-the Health of the Nation Study. SA Med J. 2006;96(5):439–44. [PubMed] [Google Scholar]
- 10.Kruger R, Kruger HS, Macintyre UE. The determinants of overweight and obesity among 10-to- 15-year-old schoolchildren in the North West Province, South Africa-the THUSA BANA (Transitional and Health during Urbanisation of South Africans; BANA, children) study. Publ Health Nutr. 2005;9(3):351–358. doi: 10.1079/phn2006849. [DOI] [PubMed] [Google Scholar]
- 11.Mehio Sibai A, Nasreddine L, Mokdad AH, Adra N, Tabet M, Hwalla N. Nutrition transition and cardiovascular disease risk factors in Middle East and North Africa countries: reviewing the evidence. Ann Nutr Metab. 2010;5793–4:193–203. doi: 10.1159/000321527. [DOI] [PubMed] [Google Scholar]
- 12.Mittal BV, Singh AK. Hypertension in the developing world: challenges and opportunities. Am J Kidney Dis. 2010;55(3):590–8. doi: 10.1053/j.ajkd.2009.06.044. [DOI] [PubMed] [Google Scholar]
- 13.Lee DE, Cooper RS. Recommendations for global hypertension monitoring and prevention. Curr Hypertens Rep. 2009;11(6):444–9. doi: 10.1007/s11906-009-0075-9. [DOI] [PubMed] [Google Scholar]
- 14.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents The fourth report on the diagnosis, evaluation and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 Suppl 4th Report):555–76. [PubMed] [Google Scholar]
- 15.Marfell-Jones M, Olds T, Stew A, Carter L. International standards for anthropometric assessment. The International Society for the Advancement of Kinanthropometry; Australia: 2006. [Google Scholar]
- 16.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. Br Med J. 2000;320(7244):1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Amusa LO, Goon DT. Blood pressure among overweight aged 7–13 years in 10 rural communities in South Africa: The Tshannda Longitudinal Study. Pak J Med Sci. 2010;27(3):664–7. [Google Scholar]
- 18.Mkhonto SS, Mabaso MLH. Relationship between obesity and blood pressure in school-going adolescents in Limpopo Province of South Africa. J Obes Res Clin Pract. 2012 doi: 10.1016/j.orcp.2012.02.001. [DOI] [Google Scholar]
- 19.Makgae PJ, Monyeki KD, Brits JS, Kemper HCG, Mashita J. Somatotype and blood pressure of rural South African children aged 9–13 years: Ellisras Longitudinal Growth and Health Study. Ann Hum Biol. 2007;34(4):240–51. doi: 10.1080/03014460601144219. [DOI] [PubMed] [Google Scholar]
- 20.Mostswagole BS, Kruger HS, Faber M, Van Rooyen JM, De Ridder JH. The sensitivity of waist-to-height ration in identifying children with high blood pressure. CVJ Africa. 2011;22(4):208–11. doi: 10.5830/CVJA-2010-062. [DOI] [PubMed] [Google Scholar]
- 21.Monyeki KD, Kemper HCG, Makgae PJ. The association of fat patterning with blood pressure in rural South African children: the Ellisras Longitudinal Growth and Health Study. Int J Epidemiol. 2005;35(1):114–20. doi: 10.1093/ije/dyi219. [DOI] [PubMed] [Google Scholar]
- 22.Shahid A, Ramzan A, Mustufa MA, Nasim S, Pirzada AG. Blood pressure, body mass index and waist circumference of school going children of Karachi. Pak J Med Res. 2010;49(4):116–20. [Google Scholar]
- 23.Aounallah-Skhiri H, El Ati J, Traissac P, Romdhane HB, Eymard-Duvernay S, Delpeuch F, et al. Blood pressure and associated factors in a North African adolescent population. A national cross-sectional study in Tunisia. BMC Publ Health. 2012;12:98. doi: 10.1186/1471-2458-12-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kollias A, Antonodimitrakis P, Grammatikos E, Chatziantonakis N, Grammatikos EE, Stergiou GS. Trends in high blood pressure prevalence in Greek adolescents. J Hum Hypertens. 2009;23(6):385–90. doi: 10.1038/jhh.2008.166. [DOI] [PubMed] [Google Scholar]
- 25.Dasgupta K, O’Loughlin J, Chen S, Karp I, Paradis G, Tremblay J, Hamet P, et al. Emergence of sex differences in prevalence of high systolic blood pressure: analysis of a longitudinal adolescent cohort. J Cir. 2006;114(24):2663–70. doi: 10.1161/CIRCULATIONAHA.106.624536. [DOI] [PubMed] [Google Scholar]
- 26.Tirosh A, Afek A, Rudich A, Percik R, Gordon B, Ayalon N, et al. Progression of normotensive adolescents to hypertensive adults: a study of 26,980 teenagers. J Hypertens. 2010;56(2):203–9. doi: 10.1161/HYPERTENSIONAHA.109.146415. [DOI] [PubMed] [Google Scholar]
- 27.Lane DA, Gill P. Ethnicity and tracking blood pressure in children. J Hum Hypertens. 2004;18(4):223–8. doi: 10.1038/sj.jhh.1001674. [DOI] [PubMed] [Google Scholar]
- 28.Grigore D, Ojeda NB, Alexander BT. Sex differences in the fetal programming of hypertension. Gend Med. 2008;5(suppl A):S121–32. doi: 10.1016/j.genm.2008.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Owen CG, Nightingale CM, Rudnicka AR, Sattar N, Cook DG, Ekelund U, et al. Physical activity, obesity and cardiometabolic risk factors in 9-to-10-year-old UK children of white European, South Asian and black African-Caribbean origin: The Child Heart and Health Study in England (CHASE) Diabetologia. 2010;53(8):1620–30. doi: 10.1007/s00125-010-1781-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leary SD, Ness AR, Smith GD, Mattocks C, Deere K, Blair SN, Riddoch C. Physical activity and blood pressure in children: Findings from a population-based study. Hypertens. 2008;51(1):92–8. doi: 10.1161/HYPERTENSIONAHA.107.099051. [DOI] [PubMed] [Google Scholar]
- 31.Pate RR, Mclver K, Dowda M, Brown WH, Addy C. Directly observed physical activity levels in preschool children. J Sch Health. 2008;78(8):438–44. doi: 10.1111/j.1746-1561.2008.00327.x. [DOI] [PubMed] [Google Scholar]
- 32.Brage S, Wedderkopp N, Ekelund U, Franks PW, Wareham NJ, Andersen LB, et al. Features of the metabolic syndrome are associated with objectively measured physical activity and fitness in Danish children: The European Youth Heart Study (EYHS) Diabetes Care. 2004;27(9):2141–8. doi: 10.2337/diacare.27.9.2141. [DOI] [PubMed] [Google Scholar]
- 33.Manu R, Sundaram KR, Paul M, Deepa AS, Kumar RK. Obesity in Indian children: time trends and relationships with hypertension. Natl Med J India. 2007;20(6):288–93. [PubMed] [Google Scholar]
- 34.Taksande A, Chaturvedi P, Vilhekar K, Jain M. Distribution of blood pressure in school children in rural area of Wardha District, Maharashtra, India. Ann Paediatr Card. 2008;1(2):101–6. doi: 10.4103/0974-2069.43874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reddy MD, Kushwaha AS, Kotwal A, Basannar DR, Mahen A. Study of blood pressure profile of school children 6–15 years in a rural setting of Maharashtra. Med J Armed Forces India. 2012;68(3):222–5. doi: 10.1016/j.mjafi.2012.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hosseini M, Ataei N, Aghmohammadi A, Yousefifard M, Taslimi S, Ataei F. The relation of body mass index and blood pressure in Iranian children and adolescents aged 7–18 years old. Iranian J Publ Health. 39(4):126–34. [PMC free article] [PubMed] [Google Scholar]
- 37.Flores-Huerta S, Klunder-Klunder M, Reyes DIC, Santos JI. Increase in body mass index and waist circumference is associated with high blood pressure in children and adolescents in Mexico City. Arch Med Res. 2009;40(3):208–13. doi: 10.1016/j.arcmed.2009.02.009. [DOI] [PubMed] [Google Scholar]