Abstract
Objective
Low Birth Weight [LBW] (1500gr ≤ Birth Weight ≤ 2499 gr) is one of the most serious health problems in neonates. These neonates need complementary interventions (e.g. tactile-kinesthetic stimulation) to promote development. This study was conducted to determine the effect of Tactile-Kinesthetic Stimulation (TKS) on physical and behavioral development of Low Birth Weight neonates.
Methods
This was a randomized controlled trial with equal randomization (1:1 for two groups) and parallel group design. Forty LBW neonates were randomly allocated into test (n = 20) and control (n = 20) groups. TKS was provided for three 15 minute periods per day for 10 consecutive days to the test group, with the massages consisting of moderate pressure strokes in supine and prone position and kinesthetic exercises consisting of flexion and extension of limbs. All measurements were taken before and after completion of the study with the same equipment (Philips electronic weighing scale with an accuracy of ±5 grams and Brazelton Neonatal Behavioral Assessment) and by the same person.
Findings
There was a trend towards increased daily weight gain, but without statistical significance. On the Brazelton scale, the test group showed statistically significant improved scores on the ‘motor’ (P-value <0.001) and ‘regulation of state’ (P-value = 0.039) clusters after the 10 days TKS.
Conclusion
TKS has no adverse effects on physiologic parameters and gives better adaptive behavior of LBW neonates compared to those without TKS.
Keywords: Tactile Stimulation, Kinesthetic Stimulation, Low Birth Weight, Neonatal Behavioral Assessment Scale
Introduction
With developments in medical technology especially in neonatal intensive care, the survival rate of premature and low birth weight infants has been markedly improved. Nevertheless, such infants remain at an increased risk for later poor developmental outcomes as the birth weight decreases and they are at high risk for major developmental disorders such as cerebral palsy and minor motor disorders such as developmental coordination disorder and minor neurological dysfunction[1, 2].
Many studies reported that intervention may be most effective if it is applied during infancy when there is high plasticity of the brain[3]. A number of studies have demonstrated that early intervention can facilitate early mother– infant relationship and results in beneficial developmental outcomes in non-brain-injured low birth weight neonates[4, 5]. Differences in the time of the receiving sensory inputs seem to change the connectivity and the structure of the cerebral cortex and the responsiveness of neonates to tactile stimulation in the first days of life is greater than any other sensory modality because skin is the largest sensory organ and the tactile system is the earliest sensory system to become functional[6, 7]. Furthermore, growth and cerebral maturity depend on neurotransmitters that are responsive to stroke and gentle tactile stimulation[7].
The typical massage used in neonates is a gentle stroking with moderate pressure of parts of the body combined with kinesthetic stimulation that consists of passive motion of the limbs[8]. Early stimulation given to neonates will change the growth of the brain cells, improve adaptive behavior, and finally cause the achievement of the optimal development of their age[6]. Neonates continually communicate their level of stress and stability in relation to what is happening to and around them therefore, caregivers must be sensitive to stress behaviors versus stable behaviors. Behavioral development is very important and is prerequisite for neurodevelopment[9]. Adaptive behaviors are infant's ability to involve with environmental stimulus and show cortical function that examined with Neonatal Behavioral Assessment Scale (NBAS) or Brazelton scale. Brazelton scale is sensitive to changes and is a good scale for evaluation of neonatal behaviors[10].
Despite the several benefits pointed out by studies in the area, lack of consensus on the mechanisms responsible for the clinical and behavioral improvements or the specific intervention scheme which would be more effective and suitable for each situation according to gestational age or birth weight were the reasons why massage was not yet recommended as routine procedure stimulation for neonates. This study was designed to find out the effects of ten-day tactile stimulation on physical and behavioral changes in low birth weight neonates.
Subjects and Methods
This was a Randomized Controlled Trial (RCT) study type. The study was carried out on LBW neonates in Akbar-Abadi hospital, Tehran. The study sample was consisted of 40 inborn LBW neonates, who had to meet the following selection criteria for inclusion: 1) Birth weight (BW) >1500 g and <2499g, 2) Age of neonates 1 day, 3) Absence of congenital anomalies and neuromuscular disorders, 4) Medically stable with no requirement of drugs (other than mineral and vitamin supplements) or any specific inter-ventions. We excluded neonates whose parents tended to draw their neonates of the study for any reason and at any time.
Change in habituation was selected to calculate sample size with an α-value of 5% and power of 80%. The analysis accounted for a 20% dropout rate. Twenty neonates per group were needed to detect clinically worthwhile effects. It seemed difficult to choose the participants with such inclusion criteria but many eligible neonates were actually hospitalized for a long time because of bad parenting and/or economic and cultural issues. After informed consent was taken from the parents, neonates were randomly assigned to the treatment and control group (n = 20) based on a stratification of gestational age, birth weight, birth length, head circumference at birth, gender, Apgar (1 and 5 min), premature or IUGR. The treatment group received TKS for three 15 minute periods per day for 10 consecutive days.
The study was approved by the Research Ethics Committee of Rehabilitation College of Tehran University of Medical Sciences. After gathering of clinical data, all neonates were evaluated by NBAS and clinical data and results of evaluation were collected.
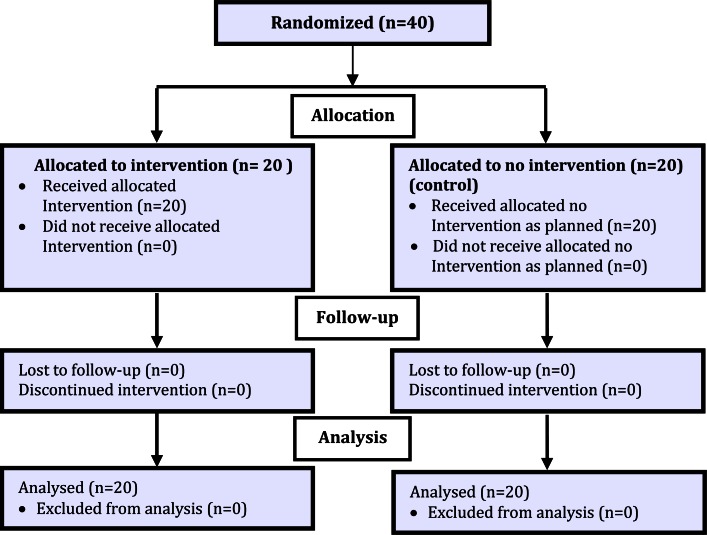
This study used the massage therapy protocol according to Field et al[11]. Massage therapy was begun on the first day of life and continued for 10 consecutive days. The massage sessions comprised three segments which were two five-minute phases of tactile stimulation and one five-minute phase of kinesthetic stimulation given during the middle phase. During tactile stimulation, the neonate was placed in prone position and stroked with the fingers of both hands of therapist for 5 one-minute periods over each region in the following sequence: 1) from the top of the head to the neck, 2) from the neck across the shoulders and back to the neck, 3) from the upper back to the buttocks and revere to the upper back, 4) from the thigh to the foot to the thigh on both legs simultaneously, and 5) from the shoulder to the hand to the shoulder on both arms simultaneously. For the kinesthetic phase, neonatewas placed in supine position. This phase consisted of six passive flexion/extension movements, each lasting approximately 10 seconds. These movements occurred in the following sequence: 1) right arm, 2) left arm, 3) right leg, 4) left leg, and 5) both legs simultaneously. Finally tactile stimulation was repeated in third phase. At the end of treatment period (10 days), NBAS was administered again and results of first and second evaluations were compared (Fig. 1).
Fig. 1.
Flow diagram of patients
Neonates’ characteristics were compared using the Mann-Whitney U-test and t-test for continuous data and Fisher's exact test for discrete data. The independent t-test was used to analyze the difference between pre and post intervention in the cluster scores of the NBAS and weight (between groups) and the paired t-test was used to analyze the difference within group. The statistical software SPSS (version 18) was used for statistical analysis. All values were tabulated as averages (mean) with standard deviation (SD). For all analyses, the significance level was 0.05 and confidence interval 95%.
Findings
As shown in Table 1 and 2, neonates in both the treatment and the control group were matched evenly for all parameters: gestational age, birth weight, birth length, head circumference at birth, gender, Apgar (1 and 5 min), premature or IUGR and neonatal behavior. Also two groups were matched for socio-economic and cultural status. The mean birth weight and gestational age for neonates were 2015 (±309.95) grams and 33.65 (±1.93) weeks. According to the results (Table 3), treatment group was more mature in ‘motor’ and ‘state regulation’ and there was statistically significant difference between the 2 groups in these clusters. Weight at 10th day (after study) was 1930.0 (±338.5) gr and 1945.5 (±299.8) in treatment and control group, respectively. There was no significant difference in weight gain in the two groups (P= 0.2).
Table 1.
Sample's descriptive data and clinical results
| Characteristics | Control group Mean (SD) | Treatment group Mean (SD) | P. value |
|---|---|---|---|
| Birth Weight | 2051.50 (305.96) | 1978.50 (317.46) | 0.5 |
| Head Circumference | 31.40 (2.15) | 31.10 (1.85) | 0.6 |
| Birth Length | 44.72 (2.90) | 44.77 (4.12) | 1 |
| Apgar 1 st min | 8.35 (0.67) | 8.50 (0.69) | 0.5 |
| Apgar 5 th min | 9.35 (0.67) | 9.60 (0.502) | 0.2 |
| Gestational Age | 33.67 (1.91) | 33.64 (2.06) | 1 |
SD: Standard deviation
Table 2.
Comparison of NBAS in treatment and control group (Before study)
| Parameters | Treatment group Mean (SD) | Control group Mean (SD) | P. value |
|---|---|---|---|
| Habituation | 3.59 (0.70) | 3.61 (0.50) | 0.9 |
| Orientation | 2.23 (0.34) | 2.24 (0.24) | 0.9 |
| Motor | 2.96 (0.42) | 2.73 (0.29) | 0.06 |
| Range of State | 3.72 (0.57) | 3.57 (0.47) | 0.4 |
| State Regulation | 3.00 (0.71) | 2.35 (0.57) | 0.07 |
| Autonomic Stability | 6.50 (0.97) | 6.65 (0.56) | 0.5 |
| Reflexes | 22.65 (1.98) | 22.85 (1.72) | 0.7 |
NBAS: Neonatal Behavioral Assessment Scale / SD: Standard Deviation
Table 3.
Comparison of NBAS in treatment and control group (After study)
| Parameters | Treatment group Mean (SD) | Control group Mean (SD) | P. value |
|---|---|---|---|
| Habituation | 4.36 (0.53) | 4.56 (0.54) | 0.3 |
| Orientation | 3.46 (0.359) | 3.44 (0.39) | 0.8 |
| Motor | 4.65 (0.25) | 3.98 (0.35) | <0.001 |
| Range of State | 4.312 (0.50) | 4.61 (0.43) | 0.08 |
| State Regulation | 4.30 (0.74) | 3.31 (0.74) | 0.04 |
| Autonomic Stability | 6.63 (1.08) | 7.01 (0.62) | 0.5 |
| Reflexes | 22.60 (1.09) | 22.90 (1.37) | 0.9 |
NBAS: Neonatal Behavioral Assessment Scale / SD: Standard Deviation
Discussion
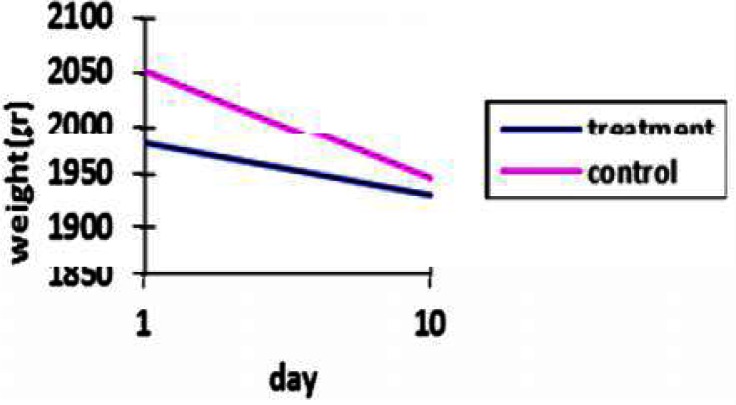
The present study assessed the clinical and behavioral aspects of low birth weight neonates during hospital stay. There are many studies about the effect of tactile stimulation on growth development of infants. The majority of studies have shown improvement in the clinical parameters specially weight gain because of increasing of ornithine decarboxylase, an important enzyme involved in protein synthesis, with tactile stimulation[11–15]. Also, a Cochrane meta-analysis has shown in average a greater weight gain of 5 g/day in treatment groups than in controls[15]. The results of the present study point to a tendency for an increase in weight gain for LBW neonates who received tactile-kinesthetic stimulation, but without statistical significance (Fig. 2). This is consistent with the reports of Lee (2006)[5] and Andreia et al (2010)[7]. One factor which might have contributed to this result is the weight loss due to loss of extracellular fluid during the first week of neonate's life[18].
Fig. 2.
Comparison of weight in treatment and control group during study
Some studies have reported that stimulation may adversely affect physiologic parameters in preterms and produce apnea[17] while others have not shown these[13, 14]. In the present study, according to necessary monitoring for each neonate and also opinion of expert supervisor of NICU, the stimulation had no adverse effects on physiologic parameters like temperature, heart rates, apnea and respiratory rate.
In the behavioral aspects, there are some studies. A number of studies have reported better state regulation with tactile-kinesthetic stimulation for 10 days in neonates[4, 6, 13] and the result of this study shows treatment infants are more mature in state regulation compared to control group. In other words, the neonates who received TKS improved their abilities to be less irritable and fussy and showed less stress behaviors. These neonates had a higher capacity for maintaining stable state organization.
Also our results in motor is consistent with those of Wahyutami et al[6] and Field et al[11]. They reported that treatment infants showed better performance in motor behavior. The other behavioral results (orientation, habituation, range of state, autonomic stability and reflexes) in this study are inconsistent with Wahyutami et al[6], Field et al[11] and Mathai et al[13] and only consistent with Ohgi et al[4]. It seems possible that reasons which have contributed to these results are participation of mothers in interventions and their interaction with their neonates and long term follow up.
Our study had some limitations. Some of selected neonates were discharged before 10 days and did not continue their intervention and were drawn from sample. It was also very difficult to match the two groups due to the inclusion criteria.
Conclusion
TKS has no adverse effects on physiologic parameters and gives better adaptive behavior of LBW neonates compared to those without TKS. These data provide evidence for the effectiveness of TKS in improving infant's behavior and a trend to enhance mature behavior.
Acknowledgments
This research has been supported by Tehran University of Medical Sciences and Health Services grant and registered at www.irct.ir (identifier IRCT201105016352N1). This article is based on a thesis written by the Corresponding Author in partial fulfillment of the requirements for the Advanced Master of Science Degree in Occupational Therapy from School of Rehabilitation, Tehran University of Medical sciences.
Conflict of Interest
None
References
- 1.Vohr BR, Wright L, Dusick AM, et al. Neurodevelopmental and functional outcomes of extremely low birth weight infant in the National Institue of Child Health and Human Development Neonatal Research Network 1993-1994. Pediatrics. 2000;105(6):1216–26. doi: 10.1542/peds.105.6.1216. [DOI] [PubMed] [Google Scholar]
- 2.Mcdonald AD. Cerebral palsy in children of very low birth weight. Arch Dis Child. 1963;38:579–88. doi: 10.1136/adc.38.202.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heineman KR, Hadders-Algra M. Evaluation of Neuromotor Function in Infancy- A Systematic Review of Available Methods. J Dev Behav Pediatr. 2008;29(4):315–23. doi: 10.1097/DBP.0b013e318182a4ea. [DOI] [PubMed] [Google Scholar]
- 4.Ohgi S, Fukuda M, Akiyama T, et al. Effect of an early intervention program on low birth weight infants with cerebral injuries. J Paediatr Child Health. 2004;40(12):689–95. doi: 10.1111/j.1440-1754.2004.00512.x. [DOI] [PubMed] [Google Scholar]
- 5.Lee HK. The effects of infant massage on weight, height and mother-infant interaction. Taehan Kanho Hakhoe Chi. 2006;36(8):1331–9. doi: 10.4040/jkan.2006.36.8.1331. [DOI] [PubMed] [Google Scholar]
- 6.Wahyutami TS, Soedjatmiko, Firmansyah A, et al. Effects of massage on behavior of full-term newborns. Paediatrica Indonesiana. 2010;50(4):187–92. [Google Scholar]
- 7.Ferreira AM, Bergamasco NH. Behavioral analysis of preterm neonates included in a tactile and kinesthetic stimulation program during hospitalization. Rev Bras Fisioter. 2010;14(2):141–8. [PubMed] [Google Scholar]
- 8.Procianoy RS, Mendes EW, Silveira RC. Massage therapy improves neurodevelopment outcome at two years corrected age for very low birth weight infants. Early Hum Dev. 2010;86(1):7–11. doi: 10.1016/j.earlhumdev.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Hunter JG. Neonatal Intensive Care Unit. In: Case-Smith J, editor. Occupational Therapy for Children. 5th ed. St Louis: Mosby; 2005. pp. 688–770. [Google Scholar]
- 10.Lundqvist C, Sabel KG. Brief report: the Brazelton Neonatal Behavioral Assessment Scale detects differences among newborn infants of optimal health. J Pediatr Psychol. 2000;25(8):577–82. doi: 10.1093/jpepsy/25.8.577. [DOI] [PubMed] [Google Scholar]
- 11.Field T, Saul M, Schanberg S, et al. Tactile/kinesthetic stimulation effects on preterm neonates. Pediatrics. 1986;77(5):654–8. [PubMed] [Google Scholar]
- 12.Massaro AN, Hammad TA, Jazzo B, et al. Massage with Kinesthetic Stimulation Improves Weight Gain in Preterm Infants. J Perinatol. 2009;29(5):352–7. doi: 10.1038/jp.2008.230. [DOI] [PubMed] [Google Scholar]
- 13.Mathai Sh, Fernandez A, Mondkar J, et al. Effects of Tactile-Kinesthetic Stimulation in Preterms- A controlled Trial. Indian Pediatr. 2001;38(10):1091–8. [PubMed] [Google Scholar]
- 14.Keshavarz M, Babaee Gh, Dieter J. Effect of tactile-kinesthetic stimulation in weight gaining of preterm infants hospitalized in intensive care unit. Tehran Uni Med J. 2009;67(5):347–52. [In Persian] [Google Scholar]
- 15.Golchin M, Rafati P, Taheri P, et al. Effect of deep massage on increasing body weight in low birth weight infants. Feyz. 2010;4(1):46–50. [In Persian] [Google Scholar]
- 16.Vickers A, Ohlsson A, Lacy JB, et al. Massage for promoting growth and development of preterm and/or low birth-weight infants. Cochrane Database Syst Rev. 2000;(2):CD000390. doi: 10.1002/14651858.CD000390. [DOI] [PubMed] [Google Scholar]
- 17.Gorski PA, Huntington L, Lewkowitz D. Handling preterm infants in hospital- Stimulating controversy about timing of stimulation. Clin Perinatol. 1990;17(1):103–12. [PubMed] [Google Scholar]
- 18.Marcdante K, Kliegman RM, Behrman RE. Nelson Essentials of Pediatrics. 6th ed. Philadelphia, PA: WB Saunders; 2011. pp. 13–5. [Google Scholar]