Abstract
Objective
We aimed to evaluate clinical features and follow-up data of children with functional and secondary constipation.
Methods
Hospital records of 335 constipated children were evaluated. Children were divided into 2 groups as functional and secondary, and were compared with regard to clinical and anthropometric data.
Findings
Of 335 children (M/F 167/168, mean age 4.3±3.5 years) 91% had functional constipation (group 1). Family history of constipation was significantly higher in group 1. Malnutrition was found in 18% of group 1, 56% in group 2 (p < 0.001).
Conclusion
If a constipated child has a family history of constipation but does not have failure to thrive and constipation begins at an older age, functional constipation is more probable.
Keywords: Constipation, Children, Diagnosis, Functional Gastrointestinal Disorders
Introduction
Constipation is a common health problem in childhood resulting in 3% of general pediatric and 25% of pediatric gastroenterology outpatient clinics visits[1–3]. An organic cause is rarely detected in this prevalent symptom. More than 90% of children are accepted to have functional constipation[4]. Factors underlying functional constipation are multiple as withholding stool, problems during toilet training and lack of fiber[1, 4–6]. In these children warning signs and symptoms should be questioned because it is important to distinguish functional and secondary constipation[5, 7, 8]. Moreover, even though constipation has a high prevalence, long term follow up results are limited[9, 10]. Therefore, in this study we evaluated the clinical features and follow up data of children with functional and secondary constipation.
Subjects and Methods
The study included 335 constipated children who were evaluated between February 2007 and February 2011 at Dr. Behcet Uz Children's Hospital Pediatric Gastroenterology outpatient clinic. Constipation was diagnosed according to Rome III criteria[11, 12]. Hospital records were evaluated retrospectively. Age, gender, age of onset, previous treatments, response to the previous treatment, frequency of defecation, family history, abdominal pain, rectal bleeding, abdominal distension, stool withholding behaviour, fibre intake, aetiology of constipation, anthropometric findings, response to our treatment and relapses were noted. Malnutrition was defined according to Waterlow criteria[13]. Constipated children were divided into 2 groups as functional and secondary according to history, physical exam and laboratory findings. These groups were compared with regard to data mentioned above.
Data analyses were performed using SPSS for Windows, version 15.0 (SPSS Inc., Chicago, USA). Means ± standard deviations (SD) were calculated for measurable variables. An independent t test assessed the relationship between continuous variables and malnutrition, whereas the χ2 test was used for differences in proportions. P<0.05 was considered significant.
Findings
Constipation had started at a mean age of 2.2±2.9 years (median age 1.0 year) in 335 children (male/female: 167/168, mean age: 4.3±3.5 years) enrolled. Of these, 305 (91%) were accepted to have functional constipation (Group 1). Rest of the children (9%) had an underlying disease and formed the group of secondary constipation (Group 2) (Table 1).
Table 1.
Aetiology of constipation in 335 children
| Etiology | n (%) |
|---|---|
| Functional | 305 (91%) |
| Organic | 30 (9%) |
| Cerebral palsy | 19 (6%) |
| Hypothyroidism | 5 (1%) |
| Down syndrome + hypothyroidism | 4 (1%) |
| Meningomyelocele | 1 (0.5%) |
| Hypokalemia | 1 (0.5%) |
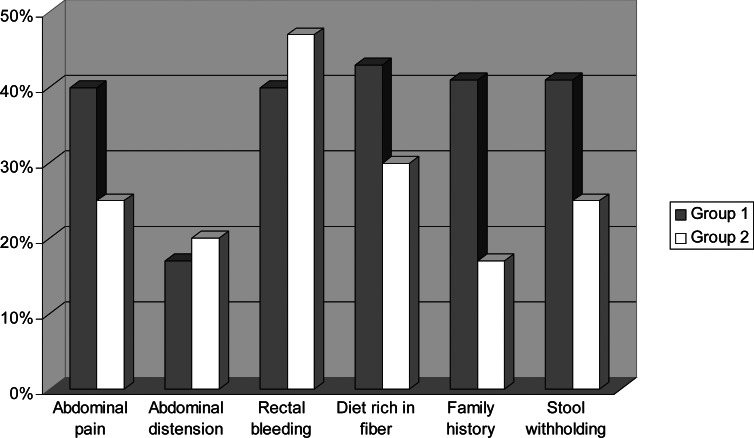
There was no significant difference with regard to sex and mean age between these groups (P=0.2, P=0.5, respectively). Median age of onset was 1 year in group 1 and 0.25 years in group 2, which was significantly lower (P=0.02). Some demographic and anthropometric findings of the groups are given in Table 2. Abdominal pain and stool withholding were seen more frequently in functional constipation group. However, these differences were not significant (P=0.191 and P=0.479, respectively). Family history of constipation was significantly higher in group 1 (41% vs. 17%, P=0.015). These findings are demonstrated in Fig. 1. Comparison of anthropometric findings is shown in Table 2. Malnutrition was found 18% in group 1 and 56% in group 2 (P<0.001). Obesity ratio was similar in both groups (6% in group 1 vs. 11% in group 2, P=0.404).
Table 2.
Demographic and anthropometric findings of children with functional and secondary constipation
| Functional constipation | Secondary constipation | P. Value | |
|---|---|---|---|
| Male/female | 148/157 | 19/11 | 0.2 |
| Mean age (year) | 4.2 (3.5) | 4.6 (4.1) | 0.5 |
| Onset of constipation (year) | 2.2 (3.0) | 1.1 (2.0) | 0.02 |
| Defecation interval (day) | 4.1 (2.3) | 4.8 (2.7) | 0.1 |
| Weight/age (%) | 103 (17) | 83 (23) | <0.001 |
| Height/age (%) | 101 (5) | 93 (10) | <0.001 |
| Weight/height (%) | 103 (14) | 97 (19) | 0.046 |
| Body Mass Index | 17 (3) | 16 (3) | 0.08 |
Fig. 1.
Clinical findings of children with functional (group 1) and secondary (group 2) constipation
Most of the patients had received treatment before (67% in group 1, 70% in group 2). Only 48% of these patients in group 1 and 38% in group 2 had succeeded. Our treatment was successful in 83% and 84%, respectively. Patients were followed-up for 4.5±3.5 months. Some patients relapsed during follow-up (30% in group 1 vs. 44% in group 2, P=0.715).
Discussion
Constipation is a prevalent problem[8, 14]. Peak incidence in childhood constipation is reported to be before 4 years of age, especially at the toilet training age[4, 5]. Constipation had started at the age of 2.2 years in our study also. Secondary constipation is stated to be less than 10% similar to our result[4, 5]. Even though the secondary constipation is not frequent, it is important to recognize organic diseases.
Abdominal pain and stool withholding were more common in functional constipation group even this difference was not significant. In other studies abdominal pain is seen in a wide range like 10-70% which also covers our result[2, 5]. However, abdominal pain is a subjective symptom. Withholding stool is accepted to be an indicator of functional constipation[8]. Rate of withholding stool behaviour is similar to literature findings. Family history is also frequent (13.9-39.3%) in children with functional constipation[14–16]. This may be due to genetic factors or environmental factors in common[16]. In the present study family history was present in 40.9% of children with functional constipation and it is found helpful in distinguishing functional and secondary constipation.
Failure to thrive is an alarm symptom to recognize organic causes[7]. In our study also, children with secondary constipation had failure to thrive. Children with cerebral palsy in group 2 may be affecting the anthropometric findings. This may explain the difference between two groups. Malnutrition rate is still high in group one. However, this is in concordant with other studies from our region[17].
Parents were educated about constipation, diet, and regular defecation habits as recommended[4, 6–8]. Afterwards, drug therapy was started. Other therapies were given if needed for organic diseases. Response rates were higher afterwards. We suppose that understanding the course of the disease and supporting the diet is important in this difference. However, there are relapses also. Relapse rates in the present study were similar to the results of van Ginkel et al[18]. However, follow-up period is not long enough to give long-term results. This is another limitation of our study.
Conclusion
If a constipated child has a family history of constipation but does not have failure to thrive and constipation begins at an older age, functional constipation is more probable. Furthermore, displaying a stool withholding behaviour may strengthen this diagnosis.
Conflict of Interest
None
References
- 1.Loening-Baucke V. Constipation in early childhood: patient characteristics, treatment, and longterm follow up. Gut. 1993;34(10):1400–4. doi: 10.1136/gut.34.10.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benninga MA, Voskuijl WP, Taminiau JA. Childhood constipation: is there new light in the tunnel? J Pediatr Gastroenterol Nutr. 2004;39(5):448–64. doi: 10.1097/00005176-200411000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Loening-Baucke V. Constipation in children. Curr Opin Pediatr. 1994;6(5):556–61. doi: 10.1097/00008480-199410000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Benninga MA. Children with constipation: What happens to them when they grow up? Scand J Gastroenterol. 2004;(241):23–6. doi: 10.1080/00855920410010933-1. [DOI] [PubMed] [Google Scholar]
- 5.Afzal NA, Tighe MP, Thomson MA. Constipation in children. Ital J Pediatr. 2011;37:28. doi: 10.1186/1824-7288-37-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajindrajith S, Devanarayana NM. Constipation in children: novel insight into epidemiology, pathophysiology and management. J Neurogastroenterol Motil. 2011;17(1):35–47. doi: 10.5056/jnm.2011.17.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Constipation Guideline Committee of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. Evaluation and treatment of constipation in infants and children: Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2006;43(3):1–13. doi: 10.1097/01.mpg.0000233159.97667.c3. [DOI] [PubMed] [Google Scholar]
- 8.Tabbers MM, Boluyt N, Berger MY, et al. Clinical practice: diagnosis and treatment of functional constipation. Eur J Pediatr. 2011;170(8):955–63. doi: 10.1007/s00431-011-1515-5. [DOI] [PubMed] [Google Scholar]
- 9.Michaud L, Lamblin MD, Mairesse S, et al. Outcome of functional constipation in childhood: a 10-year follow-up study. Clin Pediatr (Phila) 2009;48(1):26–31. doi: 10.1177/0009922808320599. [DOI] [PubMed] [Google Scholar]
- 10.Van den Berg MM, van Rossum CH, de Lorijn F, et al. Functional constipation in infants: a follow-up study. J Pediatr. 2005;147(5):700–4. doi: 10.1016/j.jpeds.2005.05.032. [DOI] [PubMed] [Google Scholar]
- 11.Hyman PE, Milla PJ, Benninga MA, et al. Childhood functional gastrointestinal disorders: neonate/toddler. Gastroenterology. 2006;130(5):1519–26. doi: 10.1053/j.gastro.2005.11.065. [DOI] [PubMed] [Google Scholar]
- 12.Rasquin A, Di Lorenzo C, Forbes D, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006;130(5):1527–37. doi: 10.1053/j.gastro.2005.08.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Waterlow JC. Classification and definition of protein-calorie malnutrition. Br Med J. 1972;3(5826):566–9. doi: 10.1136/bmj.3.5826.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Inan M, Aydiner CY, Tokuc B, et al. Factors associated with childhood constipation. J Pediatr Child Health. 2007;43(10):700–6. doi: 10.1111/j.1440-1754.2007.01165.x. [DOI] [PubMed] [Google Scholar]
- 15.Aydoğdu S, ÇakIr M, Yüksekkaya HA, et al. Chronic constipation in Turkish children: clinical findings and applicability of classification criteria. Turk J Pediatr. 2009;51(2):146–53. [PubMed] [Google Scholar]
- 16.Ip KS, Lee WTK, Chan JSH, et al. A community-based study of the prevalence of constipation in young children and the role of dietary fibre. Hong Kong Med J. 2005;11(6):431–6. [PubMed] [Google Scholar]
- 17.Tunçbilek E, Unalan T, Coçkun T. Indicators of nutritional status in Turkish preschool children: results of Turkish Demographic and Health Survey 1993. J Trop Pediatr. 1996;42(2):78–84. doi: 10.1093/tropej/42.2.78. [DOI] [PubMed] [Google Scholar]
- 18.van Ginkel R, Reitsma JB, Buller HA, et al. Childhood constipation: Longitudinal follow-up beyond puberty. Gastroenterology. 2003;125(2):357–63. doi: 10.1016/s0016-5085(03)00888-6. [DOI] [PubMed] [Google Scholar]