Abstract
There is a pressing public health need to find interventions that reduce suicide risk in later life. Psychiatric and physical illness, functional decline, and social factors place seniors at risk for suicide. Reflecting this body of evidence, the Centers for Disease Control and Prevention (CDC) has identified the promotion and strengthening of social connectedness, between and within the individual, family, community, and broader societal levels, as a key strategy for suicide prevention. The Senior Connection, a randomized trial of peer companionship for older adults, is described here, with an emphasis on the most novel features of the study design—grounding in a psychological theory of suicide and intervening at an early stage in the suicide risk trajectory by linking primary care patients with the Aging Services Provider Network.
Keywords: Geriatrics, Elderly, Social connectedness, Suicide, Prevention
1. Introduction
There is a pressing public health need to find interventions that reduce suicide risk in later life. Older adults in the United States have a higher rate of suicide than that of younger adults or adolescents [1,2]. They are the fastest growing segment of the population as well [3]. The leading edge of post-World War II “baby boomers” reached 65 years of age in 2011 [4]. We can anticipate a very large rise, therefore, in the number of older adults who die by suicide in the coming decades [5]. In particular, older men have a markedly elevated suicide rate compared to the other segments of the US population.
Psychiatric and physical illness, functional decline, and social factors place seniors at risk for suicide [6–10]. Social factors include stressful life events [7], family discord [11], insufficient social supports [12], and loneliness [13]. Reflecting this body of evidence, the Centers for Disease Control and Prevention (CDC) has identified the promotion and strengthening of social connectedness, between and within the individual, family, community, and broader societal levels, as a key strategy for suicide prevention [25]. We believe that this approach is especially well-suited to older adults given the mounting evidence that social disconnectedness is associated not only with suicide-related morbidity and mortality, but with a wide range of negative health indicators in later life, including cardiovascular disease [14,15], Alzheimer's disease [16], and all-cause mortality [17]. The goal of our program of research is to reduce late life suicide-related morbidity and mortality by leveraging the resources and expertise of the Aging Services Provider Network (ASPN) to address unmet social needs of community-dwelling older adults. The ASPN is a national network of community-based social service agencies that was initially developed as part of the Older Americans Act to ensure that adults aged 60 years and older have the supportive services necessary to maintain independent living. Our premise is that community-based social service agencies represent an untapped resource for the detection and management of suicide risk among older adults, in part because of the expertise of the ASPN in managing (and ameliorating) social factors such as disconnectedness, that place seniors at risk for suicide. Further, we propose that linking primary care patients with the services of the ASPN represents an innovation in late-life suicide prevention, as primary care is the most common site for older adults at risk to present for care in the years, months, and weeks prior to suicidal crises—and social factors are often modifiable precipitants to these suicidal crises that can be addressed with ASPN services. Lifespan, the Monroe County area's largest aging services provider, University of Rochester researchers, and scientists at the CDC are collaborating partners on the randomized trial described here.
The first research objective is to examine whether linking socially disconnected seniors with peer supports through the Retired and Senior Volunteer Program (RSVP), a division of the Senior Corps, administered by the Corporation for National and Community Service, is effective in reducing risk for suicide (defined both as reduction in suicide ideation and behavior as well as changes in more “distal” factors associated with suicide risk, such as meaning in life). We refer to the intervention as “The Senior Connection” (TSC). The second objective is to test the “mechanism” for the association of social disconnectedness and suicidal ideation and behavior as described by the Interpersonal Theory of Suicide [18,19]. Here we describe the design and rationale of TSC with an emphasis on the most novel features of the design—grounding in a psychological theory of suicide and intervening at an early stage in the suicide risk trajectory by linking primary care patients with the ASPN.
2. Methods
Previous research has identified an abundance of risk, and fewer protective, factors for suicidal behavior [6–13]. However, there are very few suicide prevention strategies that have been shown to be efficacious or effective [20]. Often, evaluations have lacked scientific rigor or neglected to measure actual behavior, relying instead on changes in knowledge and awareness of suicide risk factors, or on the intention to identify and refer at-risk individuals, as measures of program success [21]. Similarly, many strategies have focused only on intervening with those already demonstrated to be at high risk, such as promoting treatment seeking and engagement among suicide attempters [22–24]. While these important endeavors may decrease suicide mortality among those already at risk (i.e. tertiary prevention), they will not prevent new individuals from becoming at risk for suicide. Thus, there is a pressing need for the development and rigorous evaluation, using experimental or strong quasi-experimental study designs, of primary and secondary strategies for preventing suicidal behavior [25].
2.1. Overview of study design
We are in the process of recruiting 400 primary care patients (200 men and 200 women) aged 60 years or older who live in the community and who endorse feeling lonely and/or as if they are a burden on others in the preceding 2 weeks (via a self-report questionnaire). They are randomly assigned to either peer companionship (i.e., The Senior Connection, TSC) or care-as-usual (CAU). Those assigned to TSC are paired with a volunteer peer companion for 2 years. CAU subjects do not receive an intervention (the control condition). Subjects are followed for 24 months with repeated in-home (at baseline, 12 and 24 months) and telephone assessments (at 3, 6, and 18 months).
2.2. Hypothesized mechanisms of action
The Interpersonal Theory of Suicide proposes two proximal causes of the desire for suicide—low belonging and feeling like a burden on others, both of which indicate the presence of perceived social disconnectedness [18,19]. Low (or thwarted) belonging is a psychologically painful mental state that results when the fundamental need for social connectedness—described by Baumeister and Leary [26] and Cacioppo [27] as the “need to belong” (p. 1)—is unmet. The need to belong is satisfied by feeling both positively connected to and cared about by others. The need to belong is most easily met by feeling as if one ‘belongs to’ caring relationships that involve frequent, proximal contact. Feelings of loneliness are one indicator that the need to belong is not fully met. Perceived burdensomeness is a mental state characterized by perceptions that one is not making positive contributions to relationships, and in a more extreme manifestation, the belief that others would be “better off if I were gone.” The most extreme form of perceived burdensomeness involves the mental calculation that, “My death is worth more than my life to others.” The Interpersonal Theory of Suicide proposes that when individuals experience both thwarted belongingness and perceived burdensomeness, they will want to die by suicide.
A common element of interventions that are associated with reduced suicide deaths among older adults is the promotion of connectedness to providers or peers [28]. However, none of the existing intervention studies were designed to test this mechanism. An objective of The Senior Connection trial is to examine whether promoting social connectedness results in reductions in suicide risk in later life. Further, our study utilizes an existing intervention offered by the ASPN. It is our belief that many existing interventions offered by the ASPN, while not conceptualized as suicide prevention interventions, may function to reduce suicide risk in later life.
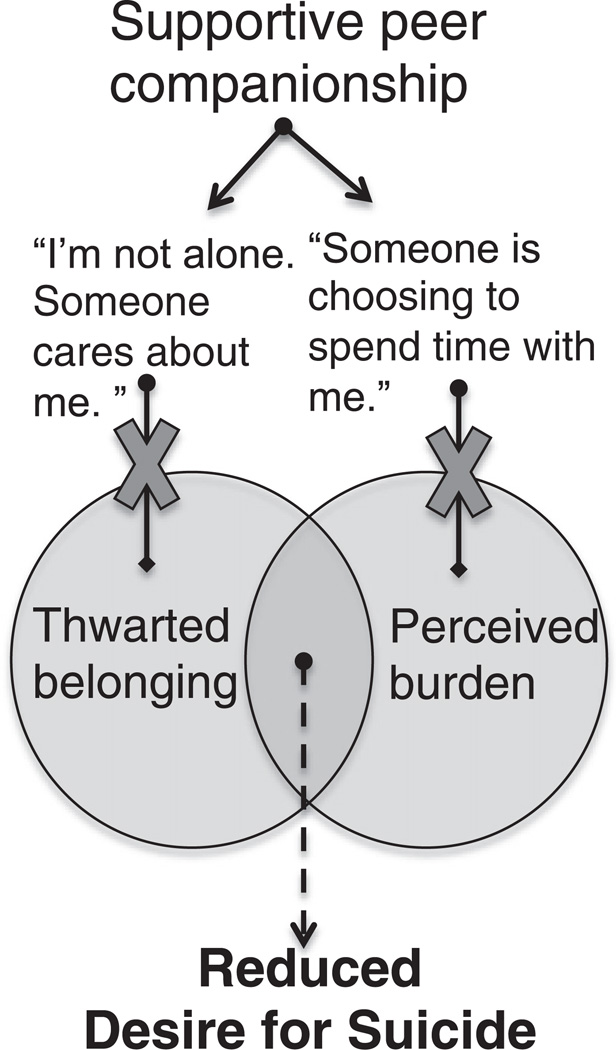
According to the Interpersonal Theory of Suicide [18], an effective suicide prevention intervention must create some degree of social connectedness so that low belongingness (i.e., the internal perception of being disconnected and not cared about) is prevented or ameliorated; according to the theory, even a small degree of belongingness can be life-saving. An even more potent intervention, according to the theory, would be one that facilitates positive relationships in which older adults do not perceive themselves to be a burden—even a minimal degree of making positive contributions to others can be life-saving as perceptions of burdensomeness would not be global. The Senior Connection intervention meets these requirements. We propose to alter the trajectory towards suicide by introducing the potent protective factor of social connectedness. We propose that involving older adults in supportive interpersonal relationships—as a recipient of companionship—will prevent suicide by intervening in the causal pathway proposed by the Interpersonal Theory of Suicide. Specifically, two causes of desire for suicide—low belongingness and perceived burdensomeness—will be prevented, thereby blocking the incidence of proximal risk determinants, including suicidal ideation, death ideation, and depression. See Fig. 1 for a depiction of the proposed psychological processes through which the intervention reduces suicide risk. Our study is both a test of the Interpersonal Theory of Suicide and an examination of the effectiveness of an existing widely implemented social connectedness intervention in the reduction of suicide risk among older adults.
Fig. 1.
Hypothesized psychological impact of peer companionship and the prevention of the key constructs of the Interpersonal Theory of Suicide.
Our primary outcomes are death ideation and suicide ideation—wishing for one's death and thinking about killing oneself, respectively. We selected these outcomes because our goal with this intervention is to target older adults at risk for suicidal crises, on account of endorsement of low belongingness and/or burdensomeness, and intervene before the development of suicidal crises, manifested as suicide ideation with planning and intent. Our rationale for focusing on social connectedness is that older adults are more likely to die on their first suicide attempt [29,30] and risk is difficult to detect because older adults are less likely to report suicidal thoughts to others [31]. Thus, indicated preventive interventions [32]—targeting those with suicidal thoughts and attempts—are less likely to be effective than at younger ages.
2.3. Study aims
Our specific aims are (Aim 1) to compare the impact of TSC (i.e., peer companionship and research assessments) and CAU (i.e., research assessments only) on social connectedness of older adults. We hypothesize that TSC will be more effective than CAU in decreasing older persons' feelings of (a) thwarted belongingness and (b) perceived burdensomeness because peer companionship will create a caring, supportive relationship that thereby fosters belongingness and is not characterized by burdensomeness. A peer companionship relationship may reduce burdensomeness because the companion is there voluntarily and is not in a caregiving role with the subject; therefore the subject may feel that someone is choosing to spend time with him or her, thus suggesting an absence of burden. Alternatively, the subject may begin to also feel like a burden on the volunteer companion, especially if the companion provides instrumental support. Thus, examination of this hypothesis will allow us to potentially uncover potential “side effects” of peer companionship interventions. We did not alter the intervention (e.g., by explicitly promoting reciprocity in the relationship), as we wanted to test an existing intervention.
Our second aim is to compare the effectiveness of TSC versus CAU in reducing factors associated with proximal risk for suicide in older adults, defined by suicide ideation, death ideation, depression, and meaning in life. We hypothesize that compared with CAU, subjects who receive TSC will be less likely to report death ideation and suicide ideation, will report fewer depressive symptoms, and will report greater meaning in life.
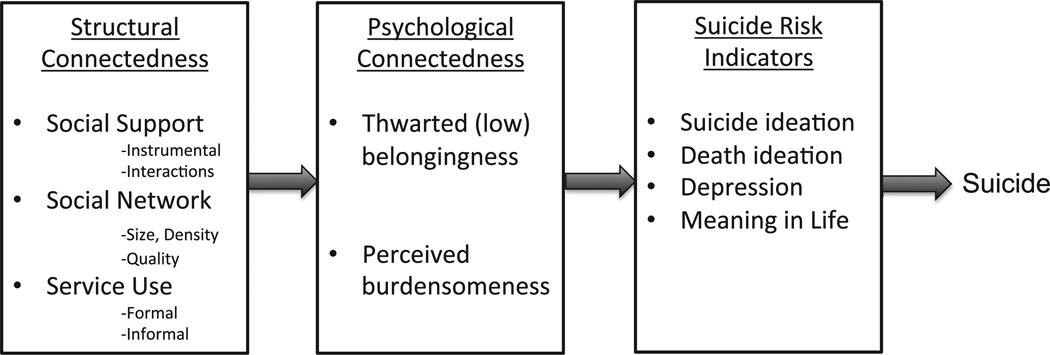
Our third aim is to determine whether changes in older adults' perceptions of low belongingness and perceived burdensomeness mediate the relationship between the effects of peer companionship and suicide risk. We hypothesize that the (structural) connectedness produced by peer companionship results in reduced thwarted belongingness and perceived burdensomeness, which in turn leads to reductions in more proximal risk factors for suicide (see Fig. 2).
Fig. 2.
Hypothesized processes through which TSC reduces suicide risk.
Our fourth aim is to examine whether responsiveness to the intervention differs by gender. Although we do not predict specific gender differences, the final aim is important because the vast majority of older adults who die by suicide are men; further, of the few interventions with effects suggestive of suicide prevention, most have been effective only for older women. Thus, demonstrating that peer companionship is effective in men is a necessary step in testing the intervention. Finally, a qualitative aim involves examining how subjects perceive their roles in the companionship relationship and to obtain additional information on benefits or drawbacks of the program that we may not have anticipated.
2.4. Settings
Two settings are pertinent to this project: primary care practices, from which subjects will be recruited into the study, and Lifespan, the community-based aging services agency that offers the intervention.
2.4.1. Primary care practices for recruitment
The Greater Rochester Practice-Based Research Network (GR-PBRN) is a network of primary care practices coordinated by the University of Rochester's Clinical Translational Science Institute to provide access to subjects and community-based primary care practices for research. We are approaching individual practices for their permission to contact patients on their rolls who are ages 60 years and over. We elected not to randomize at the practice level because our focus is squarely on the patient; we do not have specific hypotheses concerning differences by race/ethnicity in response to the intervention (although we will examine such factors in secondary analyses), and there is no risk of contamination of the intervention condition at the practice level (the intervention is completely separate from and independent of the practice.)
2.4.2. The Aging Services Network delivers the intervention
Lifespan is the largest aging services agency in the Rochester, NY region. In 2004 Dr. Conwell and colleagues at the University of Rochester joined with Lifespan to form a partnership for research called the Senior Health and Research (SHARE) Alliance. SHARE Alliance objectives are (a) to define the prevalence and correlates of depression and other symptoms of mental illness among aging services clients, (b) to examine the role of social services in reducing symptoms of depression in older adult clients, and (c) to develop and test strategies by which social service agencies can participate in the reduction of mental disorders in older adults. SHARE Alliance activities have included training of agency care managers in the detection and basic management of late life mental illness and the assessment and management of suicide risk; adoption of routine screening for mental disorders in agency clients; revision of the agencies' data management systems to support research; and a series of preliminary research studies.
The Senior Connection intervention is delivered by RSVP, one of Lifespan's many programs for seniors in the community. Its objective is to match seniors with volunteer opportunities that match their interests and capabilities. RSVP volunteers interested in serving as companions for other seniors can be placed with our project because The Senior Connection program is one of the available RSVP volunteer “stations” for older adults to volunteer their time. While the volunteers in The Senior Connection are termed “companions” this is not meant to imply that the program is part of the National Senior Corps “Senior Companion”program; The Senior Connection is a local program and connected to the Senior Corps through RSVP. Companions provide non-medical caregiving and support for isolated seniors—“care receivers”—to help promote their health and well-being. Volunteers are aware that the care receivers are part of a research study and that they themselves are not research subjects. Volunteers provide friendly visiting and supportive phone calls. Volunteers are asked to make at least four contacts per month, with at least two occurring in person, while the others can be by phone.
2.5. Participants
The study will recruit and enroll 400 subjects into the study through GR-PBRN practices using the procedures that will be described later. After providing informed consent and completing a baseline assessment, subjects are randomized to receive either the intervention (TSC; n = 200) or care as usual (CAU; n = 200). Because we are interested in whether men and women respond to the intervention differently, we are stratifying the randomization by gender (100 men and 100 women in each group).
2.5.1. Inclusion and exclusion criteria
For inclusion in the study, a subject must be age ≥ 60 years, English speaking, reside in the community (i.e., those residing in assisted living and skilled nursing facilities are ineligible), and endorse low belongingness and/or perceived burdensomeness. These latter criteria are determined by positive responses to two questions extracted from the Interpersonal Needs Questionnaire (INQ) [33], related to how subjects have been feeling over the last 2 weeks. Response options for both are “not at all true for me,” “somewhat true for me,” and “very true for me.” The first screening question assesses perceived burdensomeness: “These days I feel like a burden on the people in my life” (positive screen = “somewhat” or “very true for me”). The second screening question assesses belongingness: “These days, I feel lonely” (positive screen = “somewhat” or “very true for me”). Older adults are eligible if they endorse “somewhat” or “very true” for either loneliness or burdensomeness. At baseline, subjects complete the full Interpersonal Needs Questionnaire, which more fully assesses the psychological constructs of thwarted belongingness and perceived burdensomeness; it is not feasible to administer the full questionnaire as part of screening in busy primary care practices.
Our objective in using these two questions is to identify a group of subjects who report social disconnectedness, and who therefore are members of an at-risk group appropriate for preventive intervention rather than indicated treatments for suicide ideation and/or behavior. Our focus on prevention further “upstream,” rather than targeting people in acute crisis situations, aligns with CDC's approach to the prevention of suicidal behavior, which includes a strong focus on primary and secondary prevention through reducing risk factors and increasing protective factors.
Potential subjects are excluded if they present with active alcohol or drug abuse or dependence, psychosis, or suicidal intent. These individuals are provided with referrals to appropriate agencies. Thoughts of death or suicide are not cause for exclusion as long as the subject has no intent to harm himself or herself. Subjects must be free of significant cognitive impairment (Mini Cog score of ≥3)[34] and hear well enough (with hearing aides as indicated) to allow comfortable communication with the interviewer as well as a volunteer companion if the subject is randomized to the treatment group. These criteria are necessary in order to ensure the safety of the subject and, for those assigned to TSC intervention, to maximize the support of a volunteer companion. Literacy is not an inclusion criterion. Those who reside in long-term care facilities are not invited to participate in the study because the opportunities for social connectedness are systematically different in those settings than in the community. As long as the subject is able to reside safely in the community, there is no exclusion for medical conditions or functional impairment, no exclusion for current or lifetime mood or anxiety disorders, and no exclusion for psychopharmaco-logical or psychosocial treatments. Our rationale is that these physical and mental conditions are common among community dwelling older adults, they track closely with feelings of burdensomeness and low belongingness, and their treatments are delivered completely independent of RSVP participation.
2.5.2. Recruitment, consent procedures, and follow-up
Several recruitment strategies are in place: in-person recruitment in primary care office waiting rooms, flyers posted in primary care exam rooms, and advertisements and letters targeting patients aged 60 years or older in participating primary care practices.
For those screened who express interest in the study, two members of the research team—a clinical research coordinator (C.R.C.; research interviewer) and a Lifespan staff member (LP.N. or M.S.W.)—conduct a home visit at which informed consent is obtained (by the CRC), the baseline interview is completed, and the subject is randomized. During the home visit, the Lifespan staff member assesses for unmet health and safety needs (e.g., not enough money to pay heating bills, need for grab bars, lack of a carbon monoxide detector), and assists the subject in getting these needs met. Further, if multiple, significant unmet needs are present, the subject is referred for care management services through Lifespan. These needs are met, before randomization so that subjects in both arms of the study are equally likely to receive this intervention. Subjects are maintained in the study, either in the TSC or CAU arm, for 24 months. For subjects assigned to TSC, the intervention begins within 2 weeks of the baseline assessment and study enrollment. Follow-up research assessments are conducted for both TSC and CAU groups by telephone at 3, 6, and 18 months after the baseline interview and by in-person interview at 12 and 24 months. Study staff and Lifespan staff are not blinded to condition. Every 12 months, subjects are asked about services received, including companionship services, and if a subject receives such services this information will be tracked, thus making it available for analyses.
2.6. Intervention—The Senior Connection (TSC)
2.6.1. Senior Companion volunteers
Senior Companions are recruited by RSVP from throughout the Monroe County area. Volunteers are screened by the agency in an individual interview with the program's coordinator who evaluates the person's motivations and “fit” for the role of companion. RSVP volunteers must be aged 55 years or older and agree to complete training, adhere to program policy and procedures, and provide service without compensation. They must be able to supply their own transportation and have drivers' licenses and automobile insurance. Lifespan provides reimbursement for travel and liability insurance to volunteers as needed.
Training, conducted by the volunteer coordinator, includes a detailed orientation to the program's mission, objectives, and policies and procedures. It explores a wide range of issues related to volunteer caregiving and assists the Senior Companion in learning techniques for working with a diverse population of older adults. Topics include confidentiality and reporting requirements, accommodation of disabilities, and common physical and mental conditions that the volunteer is likely to encounter, and how best to respond.
Volunteers are not subjects in the study; thus data will not be available from the volunteers.
2.6.2. Intervention activities
Subjects randomized to TSC are assigned to a Senior Companion by the volunteer coordinator based on characteristics, preferences, and interests of both parties. The Senior Companion and subject then establish a consistent schedule of contacts on which the subject can depend. The target expectation is of interactions in person and/or by telephone at least once per week, with two per month being in person. The exact nature and frequency of the interaction are left to the dyad to determine. It may involve the Senior Companion helping the care receiver (research subject) with instrumental activities (e.g., transportation, shopping, minor housekeeping and repairs, letter writing/correspondence, or meal preparation), but the primary purpose will always emphasize supportive interpersonal interactions conducted in the way the care receiver is most comfortable. The subject and companion are expected to regularly interact throughout the 2-year study period and are encouraged to continue the relationship beyond the study period if the dyad so chooses. Since we aim to test an existing intervention that is already implemented by aging service agencies across the country, we did not modify the intervention by training companions in suicide risk warning signs. However, we did provide the Lifespan staff members with suicide risk gatekeeper training.
2.7. Implementation assessment
TSC is an effectiveness study, examining outcomes in response to a “real world” program delivered by volunteers in a community setting, providing the intervention in the manner that could be replicable by RSVPs throughout the country. With this emphasis on external validity, we do not further constrain the nature of the interactions between the volunteer and subject. However, we will conduct a process evaluation that enables examination in secondary analyses of whether characteristics of the intervention are associated with response in the study's primary outcomes. Volunteers are provided logs with which to document details regarding each contact with their assigned subject.
2.8. Care-as-usual
CAU simply entails no engagement by RSVP during the course of the 24 month follow-up period. Medical or psychiatric interventions are not restricted; neither is any kind of informal social support or social services interventions. The amount and type of services received are measured for all subjects on a yearly basis.
2.8.1. Primary outcomes
See Tables 1–3 for a listing of the primary measures.
Table 1.
Screening and demographic measures.
| Measure name and citation | Construct measured | Psychometric data |
|---|---|---|
| Social connectedness screen | Thwarted belongingness, perceived burdensomeness |
This is a two-item measure used as our initial inclusionary screen. These items are drawn from the Interpersonal Needs Questionnaire (see below), which is a scale demonstrated to have sound psychometric properties. “I feel lonely” and “I feel like a burden on others.” Both rated for the last 2 weeks. |
| Demographic characteristics | Age, race/ethnicity, gender, education, living situation, marital status |
Not applicable |
Table 3.
Suicide risk measures
| Geriatric Suicidal Ideation Scale (GSIS) [40] |
Death ideation (DI), suicidal ideation (SI), personal/social worth (PSW), meaning in life (ML) |
Heisel and Flett reported high internal consistency for both the death ideation (α = .82) and suicide ideation subscales (α = .82), as well as significant criterion validity (i.e., positive correlations with another measure of suicide ideation, depression, and hopelessness). |
| Paykel Suicide Scale [52] | Lifetime and past year suicide ideation and behaviors |
The questions ask, Has there ever been a time in your life when you, (1) felt that life was not worth living; (2) wished you were dead; (3) thought of taking your own life even if you would not really do it; (4) had reached the point where you seriously considered taking your life, or perhaps made plans how you would go about doing it; (5) made an attempt on your life? At the baseline interview, questions reflect lifetime history. At follow-ups, the time frame reflects the time that has elapsed since the last assessment. |
| Patient Health Questionnaire (PHQ-9) [44] |
Depression | Data indicate high sensitivity and specificity (i.e., 88%) with a score of 10 or more in the detection of major depression. |
Social connectedness and suicide risk are the primary outcomes. Social connectedness is measured by subjective and objective indicators. Subjective (i.e., “psychological”) connectedness is measured by the Interpersonal Needs Questionnaire [33], which is a 15-item self-report scale with a subscale that assesses low belongingness and a subscale that assesses perceived burdensomeness. Scores derived from this questionnaire have been shown to be reliable and valid indicators of low belongingness and perceived burdensomeness in both younger and older adults, as well as among community participants and clinical outpatients [33]. A prior study examining the longitudinal association between an indicator of subjective connectedness—loneliness—and an indicator of suicide risk—depressive symptom severity—found that a one standard deviation decrease in loneliness resulted in a clinically significant decrease in depressive symptoms [35]. Thus, we expect that our intervention will result in at least a one standard deviation decrease in subjective disconnectedness—both low belongingness and perceived burdensomeness.
Several dimensions of structural (or objective) connectedness are measured (i.e., as opposed to perceived or “subjective” measures). First, the National Social Life, Health, and Aging Project Social Network Module (NSL-SN) [36] is used to measure social network density and quality (closeness) and was chosen, in part, because it was designed for use with older adults. In support of the construct validity of its scores, previous examinations show that density and quality were significantly related, but the magnitude was small (r = .27), as would be expected. Second, the Berkman Social Network Index (SNI)[37] is used to assess social integration, including measurement of social network size and frequency of contact; this set of self-report questions has been shown to predict all-cause mortality (e.g., more connections are associated with reduced premature mortality by all causes) [38].
Several dimensions of suicide risk are measured. Specifically, three indices of death ideation and suicide ideation are utilized. First, the Geriatric Suicide Ideation Scale (GSIS) is a self-report scale designed for, and validated with, older adults. It yields subscale scores for death ideation, suicidal ideation, personal/social worth, and meaning in life. Heisel and Flett [39] reported high internal consistency for both the death ideation (α = .82) and suicide ideation subscales (α = .82), as well as significant criterion validity (i.e., positive correlations with another measure of suicide ideation, depression, and hopelessness). We hypothesize that a one-standard deviation decrease in low belongingness and perceived burdensomeness will result in a one-standard deviation decrease in death ideation and suicide ideation on the GSIS (i.e., approximately 3 points on the subscales, equivalent to the absolute difference between the mean score for primary care patients and psychiatric outpatients on the death ideation subscale) [40]. Second, the Paykel Suicide items are administered at each in-person visit (see Table 3 for specific items). At the first (baseline) interview, the questions reflect the lifetime history of suicide ideation and behavior. At each follow-up, the time frame reflects the time that has elapsed since the last assessment. Finally, the PHQ-9 (the Patient Health Questionnaire-9), a measure of depressive symptomatology [41], includes an item that assesses death/suicide ideation: “In the past two weeks, how often have you been bothered by thoughts that you would be better off dead or of hurting yourself in some way?” The response options are “not at all, several days, more than half the days, or nearly every day.” Responses other than “not at all” indicate the presence of death/suicide ideation and require following up with additional questions to manage suicide risk.
Questions in the GSIS that involve active suicide ideation and planning also initiate the risk assessment protocol that involves routinized procedures for additional assessment and clinical management actions. Our assessors enter data on tablet computers, which allows direct data entry into a database housed on a university server. If a subject indicates that he or she has had thoughts about being better off dead in the past 2 weeks, the data entry program requires that the assessor completes the risk assessment protocol. The assessors are extensively trained in the study's suicide risk screening protocol, which involves the PHQ-9, Geriatric Suicide Ideation Scale, and clinical interview. Any subject who endorses death or suicidal ideation is asked additional questions to assess his or her safety. Any endorsements of active suicidal ideation involve notifying the principal investigator for review of risk and protective factors and consideration of emergency psychiatric services.
2.8.2. Secondary outcomes
Social connectedness is associated not only with suicide ideation, attempt, and deaths, but also numerous indices of health, including blood pressure, sleep, and subjective ratings of health, as well as premature mortality (due to all causes) [38,42,43]. Thus, while death ideation and suicide ideation are our primary outcome, we are also interested in measuring and examining other variables that are associated with both suicide risk and physical health. These additional outcomes include depressive symptoms (Patient Health Questionnaire-9, PHQ-9) [44], physical functioning (client self-report of ability to perform activities of daily living [45] and instrumental activities of daily living) [46] and physical health burden based on subject report and chart evidence of a list of common medical conditions.
2.9. Data analytic strategy
Study data are collected and managed using REDCap electronic data capture tools hosted by the Clinical and Translational Science Institute at the University of Rochester Medical Center [47]. REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies, providing (1) an intuitive interface for validated data entry; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for importing data from external sources.
The basic analytic approach will consist of regression analyses based on general and generalized linear models. The intervention groups will be compared to determine if imbalances occur in demographics and other pre-treatment measures (i.e., the degree to which randomization was successful) and any potential confounders will be included in all subsequent analytic models. All analyses will be conducted for the intent-to-treat sample on the primary outcomes and other secondary outcomes of interest.
Aim 1 proposes to examine the effect of the intervention— The Social Connection—on several social connectedness outcomes. We predict that across all follow-up time points (3, 6, 12, 18 and 24 months), the TSC group will demonstrate higher scores on the NSL-SN compared to the CAU group and lower scores on the INQ-TB and INQ-PB. This prediction involves examining the main effect of intervention group on means of the outcomes over time in four separate models (i.e., one model per outcome). The effect of time (as well as any preexisting differences between conditions) will also be included in the models. To examine the possibility that the effect of the intervention is more “potent” over time, we will also examine the intervention by time interaction effect. Aim 2 proposes to examine the effect of the intervention—TSC—on factors associated with proximal risk for suicidal ideations and behaviors and involves an identical analytic approach to Aim 1.
Aim 3 proposes to model the mechanisms of the intervention's effects on proximal risk for suicidal ideations and behaviors. Specifically, we hypothesize that reductions in thwarted belongingness and perceived burdensomeness mediate the relationship between increased social connectedness created by TSC and suicide risk. Specifically, we propose that a structural equation model with three latent variables will provide adequate fit to our data. We predict that an observed variable representing intervention condition will predict levels of a latent variable representing social connectedness at the structural level (i.e., observed indicators of ISEL, NSL-SN) which will then predict levels of a latent variable representing psychological connectedness (i.e., observed variables of INQ-TB and INQ-PB), which will in turn predict levels of a latent variable representing proximal risk for suicidal ideations and behaviors (i.e., observed variables of GSIS-DI, PHQ-9, GSIS-PSW, GSIS-ML). We will apply methods for mediation analysis to examine these pathways over the study's time points. Using MPlus, we will follow recommended procedures for SEM with longitudinal data [48,49] using a lagged time approach to model changes in connectedness over time.
Aim 4 proposes to examine the role of gender as a potential moderator of the intervention's effectiveness. The moderation analysis will be examined by including gender and the interaction of treatment and gender in regression analyses for each of the primary outcomes described in Aims 1 and 2. A significant interaction indicates that gender moderates the effect of treatment condition on the primary outcomes.
3. Results
Screening for inclusion in the trial has commenced in four primary care clinics. Study staff has screened a total of 1091 older adults (although not every older adult completed all questions, due to refusals, cognitive impairment, or needing to end the screening early due to commencement of the doctor appointment). The majority screened was female (58.82%), with an average age of 74.70 years. Loneliness was endorsed by 30.91% (n = 332 out of 1074 complete responses) and burdensomeness by 17.46% (n = 188 out of 1077 complete responses). The majority of those screened were reached via in-person screening in primary care offices. Other recruitment methods involve phone screening, with the potential subject reached initially via either informational letter signed by the primary care physician, or advertisement in a local penny saver magazine.
Out of the 1091 screened, 701 were ineligible (64.25%), 359 were eligible (32.90%) and 31 (2.84%) did not provide enough information during the screen to determine eligibility. To be eligible, potential subjects had to endorse social disconnectedness (i.e., loneliness or burdensomeness), live in Monroe County, not identify as a seasonal resident who lives out of the area for 2 or more months, speak English, and have cognitive capacity to provide verbal consent to release contact information. The key inclusion screen items regarding connectedness (i.e., loneliness and burdensomeness) were not answered by n = 13 potential subjects (1.19%). Of the remaining 1078 potential subjects, n = 413 endorsed disconnectedness (i.e., 38.31%). Thus, of those ineligible (n = 701), the majority was ineligible because they denied disconnectedness (i.e., n = 665, 94.86%).
A total of 153 older adults have enrolled in the study (i.e., out of 359 eligible, 42.61%) and completed the baseline interview, and 139 have been randomized, 71 to TSC (51%) and 68 to CAU (49%). The remaining 14 subjects withdrew prior to randomization because they did not want to receive a peer companion.
Characteristics of this baseline sample (i.e., the total 153 subjects) are presented in Table 4. Of note, the PHQ-9 score of 7.74 is elevated, approaching the commonly used clinical cutoff of 10, despite the fact that we did not screen for depression in the inclusion screen. The sample is also characterized by high endorsements of death and suicide ideation, as evidenced by GSIS scores in Table 4 and both Paykel Suicide Scale and GSIS items in Table 5. The GSIS subscale scores in Table 4 are indicative of clinically significant death and suicide ideation, as these scores are elevated compared to both community and primary care samples as reported by Heisel and colleagues [40]. The sample is characterized by a strikingly high proportion of subjects with previous suicide attempts in their lifetimes (i.e., 19%).
Table 4.
Characteristics of the sample at baseline
| Mean (SD)/Proportion | Range | |
|---|---|---|
| Age | 70.74 (9.01) | 60–100 |
| Gender (proportion male) | 0.29 | |
| Live alone | 0.62 | |
| White | 0.76 | |
| Years of education | 14.15 (3.12) | 3–21 |
| PHQ-9 total score | 7.74 (4.99) | 0–22 |
| INQ thwarted belongingness | 5.26 (3.86) | 0–18 |
| INQ perceived burdensomeness | 0.61 (1.36) | 0–6 |
| GSIS suicide ideation | 18.37 (7.19) | 10–74 |
| GSIS death ideation | 10.38 (4.23) | 5–29 |
| GSIS perceived meaning in life | 32.61 (5.41) | 14–58 |
INQ = Interpersonal Needs Questionnaire; GSIS = Geriatric Suicide Ideation Scale. All continuous scores indicate greater scores on the respective construct, including greater thwarted belongingness, greater perceived burdensomeness, greater suicide ideation, greater death ideation, and greater perceived meaning in life.
Table 5.
Lifetime prevalence of suicide ideation and attempts.
| Proportion endorsing |
|
|---|---|
| Paykel 1: life not worth living | .52 |
| Paykel 2: wished you were dead | .41 |
| Paykel 3: thought of taking own life | .41 |
| Paykel 4: seriously considered/made plans | .26 |
| Paykel 5: attempted suicide | .19 |
| PHQ-9 item 9: current death/suicide ideation | .07 |
| GSIS item 4: I want to end my life | .06 |
| GSIS item 11: At times I think that If things get much worse for me, I will end my life. |
.06 |
| GSIS item 12: I have recently been thinking a great deal about specific ways of killing myself. |
.04 |
| GSIS item 25: I might do something to end it all if I could only muster the energy to do so. |
.02 |
For Paykel items, responses are yes/no and endorsement reflects a “yes” response. For GSIS items, responses are on a 5-point Likert scale: strongly disagree (1), disagree (2), neither agree nor disagree (3), agree (4), strongly agree (5); for these items endorsement reflects a response of 3 or greater.
4. Discussion
The objective of The Senior Connection is to reduce suicide-related morbidity among a group of socially disconnected older adults who are at elevated risk for suicide. Our findings thus far regarding the characterization of the sample support our proposal that socially disconnected older adults are at risk for suicide: Nearly one fifth of our sample endorsed a previous suicide attempt, one of the strongest risk factors for suicide deaths, the average depression score is elevated, and levels of death and suicide ideation were higher than expected for a primary care sample.
Research on suicide in later life is hampered by two problems: First, although suicide in later life represents a significant public health problem, it nonetheless remains a relatively low base rate event, making suicide deaths difficult to measure in randomized trials, where typical sample sizes are not large enough to yield reliable differences in numbers of suicide deaths. Second, suicide attempts are more often fatal among older adults [6]. Thus, indicated interventions that have been shown to be effective at younger ages by intervening with those in suicidal crises may not be as effective with older adults.
The Senior Connection attempts to address these two barriers through its study design as a selective preventive intervention. Specifically, empirical data and theoretical rationale (the Interpersonal Theory of Suicide) indicate that socially disconnected older adults are at risk for suicide. By targeting older adults who report loneliness and feeling like a burden on others, we are attempting to intervene earlier in the trajectory towards suicide—before the development of suicidal crises. In other words, by ameliorating more distal risk factors for suicide, we hope to prevent and reduce the development of a desire for suicide and intention for suicidal behavior. We suggest that carefully designed trials that are based in both theory and empirical knowledge can inform suicide prevention even if suicide deaths are not a measured outcome (i.e., due to low base rates). A key design feature is examining theory-based (i.e., falsifiable) mechanisms for how the intervention is hypothesized to be effective and how its outcomes relate to suicide risk. Knowing how an intervention works allows us to understand how to implement it with new populations (i.e., dissemination of key ingredients), increase its effectiveness with subpopulations not evidencing positive effects (i.e., improve the intervention), and hypothesize how it may have broader effects beyond the outcomes directly examined in the trial (i.e., grounding in a theory-based, empirically supported, causal process). As the results from this trial are both a test of an intervention and a test of a theory, results therefore also speak to the validity and utility of a theory that links suicide desire to attempts and deaths by suicide. Thus, regarding broader effects, we suggest that reducing or eliminating empirically and theoretically linked variables in the suicidal process allows us to hypothesize how the results may influence unmeasured outcomes, such as suicide deaths.
The National Strategy for Suicide Prevention [50], authored by a diverse group of public and private partners, outlined a comprehensive and integrated approach to addressing suicide as a public health problem. Based on the research evidence, this document identified the critical role of connectedness in suicide prevention. In accordance with the NSSP, CDC, as the nation's public health agency, outlined its strategic direction for suicide prevention [25] and includes a focus on the promotion and strengthening of individual, family, and community connectedness. CDC's strategy includes the testing of new approaches to suicide prevention that similar to TSC use enhanced connectedness to interrupt the development of suicidal behavior. By examining the Interpersonal Theory of Suicide and its proposed mechanisms, the TSC trial will contribute to the current knowledge base of understanding the relationship between social disconnectedness and suicidal ideation and behavior set forth in the NSSP and in CDC's strategic direction. Evidence for the impact of connectedness on suicide ideation and behavior can guide future research directions and help further enhance a public health approach focused on primary prevention and promotion of protective factors that build resilience across and within communities.
Table 2.
Social connectedness measures.
| Measure name and citation | Construct measured | Psychometric data |
|---|---|---|
| National Social Life, Health, and Aging Project Social Network Module (NSL-SN) [36] |
Social network density and quality (closeness) |
Cornwell et al. reported that these measures of the social network were designed for use with older adults. In support of their construct validity, density and quality were significantly related, but the magnitude was small (r = .27), as would be expected. |
| Modified Cornell Services Index (CSI) [51] |
Formal and informal health/social services usage | Adequate test–retest (r = .54–1.00) and inter-rater (modal intraclass coefficient for all items was 1.00) reliabilities are reported. |
| Interpersonal Needs Questionnaire (INQ) [33] |
Thwarted belongingness (TB), perceived burdensomeness (PB) |
Van Orden et al. reported high internal consistency coefficients for the thwarted belongingness (α = .85) and perceived burdensomeness subscales (α = .89). In support of construct validity, both subscales were found to positively correlate with suicidal ideation. |
Acknowledgements
The authors acknowledge the hard work and dedication of the other members of the TSC team: Judy Sroka, Connie Bowen, Nicole Driffill, Kathleen Jividen, and Carol Knapp.
Footnotes
This research was supported in part by Grants No. 1U01CE001942-01 from the Centers for Disease Control and Prevention, T32MH20061 and R24MH07610 from the National Institute of Mental Health, and 2KL2RR024136-06 and RR024160 from the National Institutes of Health.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heron MP, Hoyert DL, Murphy SL, Jiaquan X, Kochanek KD, Tejada-Vera B. Deaths: Final data for 2006. Natl Vital Stat Rep. 2009;57:1–135. [PubMed] [Google Scholar]
- 3.Kinsella K, Wan H. International Population Reports, P95/09-1. Washington, DC: U.S. Government Printing Office; 2009. U.S. Census Bureau. An aging world: 2008. [Google Scholar]
- 4.He W, Sengupta M, Velkoff VA, DeBarros KA. Current Population Reports. Washington, DC: 2005. Bureau USC.65+ in the United States: 2005; pp. 23–209. [Google Scholar]
- 5.Conwell Y, Dubertstein PR, Caine ED. Risk factors for suicide in later life. Biol Psychiatry. 2002;52:193–204. doi: 10.1016/s0006-3223(02)01347-1. [DOI] [PubMed] [Google Scholar]
- 6.Conwell Y, Lyness JM, Duberstein P, Cox C, Seidlitz L, DiGiorgio A, et al. Completed suicide among older patients in primary care practices: a controlled study. J Am Geriatr Soc. 2000;48:23–29. doi: 10.1111/j.1532-5415.2000.tb03024.x. [DOI] [PubMed] [Google Scholar]
- 7.Harwood DM, Hawton K, Hope T, Harriss L, Jacoby R. Life problems and physical illness as risk factors for suicide in older people: a descriptive and case–control study. Psychol Med. 2006;36:1265–1274. doi: 10.1017/S0033291706007872. [DOI] [PubMed] [Google Scholar]
- 8.Rubenowitz E, Waern M, Wilhelmson K, Allebeck P. Life events and psychosocial factors in elderly suicides—a case–control study. Psychol Med. 2001;31:1193–1202. doi: 10.1017/s0033291701004457. [DOI] [PubMed] [Google Scholar]
- 9.Waern M, Runeson BS, Allebeck P, Beskow J, Rubenowitz E, Skoog I, et al. Mental disorder in elderly suicides: a case–control study. Am J Psychiatry. 2002;159:450–455. doi: 10.1176/appi.ajp.159.3.450. [DOI] [PubMed] [Google Scholar]
- 10.Conwell Y, Duberstein PR, Hirsch JK, Conner KR, Eberly S, Caine ED. Health status and suicide in the second half of life. Int J Geriatr Psychiatry. 2009;25(4):371–379. doi: 10.1002/gps.2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duberstein PR, Conwell Y, Conner KR, Eberly S, Caine ED. Suicide at 50 years of age and older: perceived physical illness, family discord and financial strain. Psychol Med. 2004;34:137–146. doi: 10.1017/s0033291703008584. [DOI] [PubMed] [Google Scholar]
- 12.Duberstein PR, Conwell Y, Conner KR, Eberly S, Evinger JS, Caine ED. Poor social integration and suicide: fact or artifact? A case-control study. Psychol Med. 2004;34:1331–1337. doi: 10.1017/s0033291704002600. [DOI] [PubMed] [Google Scholar]
- 13.Waern M, Rubenowitz E, Wilhelmson K. Predictors of suicide in the old elderly. Gerontology. 2003;49:328–334. doi: 10.1159/000071715. [DOI] [PubMed] [Google Scholar]
- 14.Ong AD, Rothstein JD, Uchino BN. Loneliness accentuates age differences in cardiovascular responses to social evaluative threat. Psychol Aging. 2012;27:190–198. doi: 10.1037/a0025570. [DOI] [PubMed] [Google Scholar]
- 15.Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging. 2010;25:132–141. doi: 10.1037/a0017805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, et al. Loneliness and risk of Alzheimer disease. Arch Gen Psychiatry. 2007;64:234–240. doi: 10.1001/archpsyc.64.2.234. [DOI] [PubMed] [Google Scholar]
- 17.Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2012:1–7. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr. The Interpersonal Theory of Suicide. Psychol Rev. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joiner T. Why people die by suicide. Cambridge, MA, US: Harvard University Press; 2005. [Google Scholar]
- 20.Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294:2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 21.Brown CH, Wyman PA, Brinales JM, Gibbons RD. The role of randomized trials in testing interventions for the prevention of youth suicide. Int Rev Psychiatry. 2007;19:617–631. doi: 10.1080/09540260701797779. [DOI] [PubMed] [Google Scholar]
- 22.Pan YJ, Chang WH, Lee MB, Chen CH, Liao SC, Caine ED. Effectiveness of a nationwide aftercare program for suicide attempters. Psychol Med. 2012:1–8. doi: 10.1017/S0033291712002425. [DOI] [PubMed] [Google Scholar]
- 23.Vaiva G, Walter M, Al Arab AS, Courtet P, Bellivier F, Demarty AL, et al. ALGOS: the development of a randomized controlled trial testing a case management algorithm designed to reduce suicide risk among suicide attempters. BMC Psychiatry. 2011;11:1. doi: 10.1186/1471-244X-11-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatr Serv. 2001;52:828–833. doi: 10.1176/appi.ps.52.6.828. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. Strategic direction for the prevention of suicidal behavior: promoting individual, family, and community connectedness to prevent suicidal behavior. Atlanta, GA: National Center for Injury Prevention and Control; 2008. [Google Scholar]
- 26.Baumeister RF, Leary MR. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychol Bull. 1995;117:497–529. [PubMed] [Google Scholar]
- 27.Cacioppo JT, Patrick W. Loneliness: human nature and the need for social connection. New York: W.W.Norton & Company; 2008. [Google Scholar]
- 28.Conwell Y, Van Orden K, Caine ED. Suicide in older adults. Psychiatr Clin North Am. 2011;34:451–468. doi: 10.1016/j.psc.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McIntosh JL, Santos JF. Methods of suicide by age: sex and race differences among the young and old. Int J Aging Hum Dev. 1985;22:123–139. doi: 10.2190/tx1p-5pxc-k4g5-1vug. [DOI] [PubMed] [Google Scholar]
- 30.Conwell Y, Rotenberg M, Caine ED. Completed suicide at age 50 and over. J Am Geriatr Soc. 1990;38:640–644. doi: 10.1111/j.1532-5415.1990.tb01422.x. [DOI] [PubMed] [Google Scholar]
- 31.Duberstein PR, Conwell Y, Seidlitz L, Lyness JM, Cox C, Caine ED. Age and suicidal ideation in older depressed inpatients. Am J Geriatr Psychiatry. 1999;7:289–296. [PubMed] [Google Scholar]
- 32.Goldsmith SK, Pellmar TC, Kleinman M, Bunney WE. Reducing suicide: a national imperative (Institute of Medicine) 2002 [PubMed] [Google Scholar]
- 33.Van Orden KA, Cukrowicz KC, Witte TK, Joiner TE. Thwarted belonging-ness and perceived burdensomeness: construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychol Assess. 2012;24:197–215. doi: 10.1037/a0025358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Borson S, Scanlan JM, Chen P, Ganguli M. The Mini-Cog as a screen for dementia: validation in a population-based sample. J Am Geriatr Soc. 2003;51:1451–1454. doi: 10.1046/j.1532-5415.2003.51465.x. [DOI] [PubMed] [Google Scholar]
- 35.VanderWeele TJ, Hawkley LC, Thisted RA, Cacioppo JT. A marginal structural model analysis for loneliness: implications for intervention trials and clinical practice. J Consult Clin Psychol. 2011;79:225–235. doi: 10.1037/a0022610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cornwell B, Schumm LP, Laumann EO, Graber J. Social networks in the NSHAP study: rationale, measurement, and preliminary findings. J Gerontol B Psychol Sci Soc Sci. 2009;64(Suppl. 1):47–55. doi: 10.1093/geronb/gbp042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Loucks EB, Sullivan LM, D'Agostino Sr RB, Larson MG, Berkman LF, Benjamin EJ. Social networks and inflammatory markers in the Framing-ham Heart Study. J Biosoc Sci. 2006;38:835–842. doi: 10.1017/S0021932005001203. [DOI] [PubMed] [Google Scholar]
- 38.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 39.Heisel MJ, Flett GL. A psychometric analysis of the Geriatric Hopelessness Scale (GHS): towards improving assessment of the construct. J Affect Disord. 2005;87:211–220. doi: 10.1016/j.jad.2005.03.016. [DOI] [PubMed] [Google Scholar]
- 40.Heisel MJ, Flett GL. The development and initial validation of the Geriatric Suicide Ideation Scale. Am J Geriatr Psychiatry. 2006;14:742–751. doi: 10.1097/01.JGP.0000218699.27899.f9. [DOI] [PubMed] [Google Scholar]
- 41.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7:e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40:218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. J Am Med Assoc. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 45.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. JAMA. Vol. 185. The index of ADL: a standardized measure of biological and psychosocial function; 1963. Studies of illness in the aged; pp. 914–919. [DOI] [PubMed] [Google Scholar]
- 46.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 47.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cole DA, Maxwell SE. Testing mediational models with longitudinal data: questions and tips in the use of structural equation modeling. J Abnorm Psychol. 2003;112:558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- 49.Gollob HF, Reichardt CS. Interpreting and estimating indirect effects assuming time lags really matter. In: Collins LM, Horn JL, editors. Best Methods for the Analysis of Change: Recent Advances, Unanswered Questions, Future Directions. Washington, DC: American Psychological Association; 1991. pp. 243–259. [p. (1991). Best methods for the analysis of change: Recent advances, unanswered questions, future directions. xx, 355] [Google Scholar]
- 50.U.S. Department of Heath and Human Services. National Strategy for Suicide Prevention: Goals and Objectives for Action. Washington, DC: SAMSHA, CDC, NIH, HRSA; 2001. [Google Scholar]
- 51.Sirey JA, Meyers BS, Teresi JA, Bruce ML, Ramirez M, Raue PJ, et al. The Cornell Service Index as a measure of health service use. Psychiatr Serv. 2005;56:1564–1569. doi: 10.1176/appi.ps.56.12.1564. [DOI] [PubMed] [Google Scholar]
- 52.Paykel ES, Myers JK, Lindenthal JJ, Tanner J. Suicidal feelings in the general population: a prevalence study. Br J Psychiatry. 1974;124:460–469. doi: 10.1192/bjp.124.5.460. [DOI] [PubMed] [Google Scholar]