Abstract
Many forms of cancer present with a complex metabolic profile characterised by loss of lean body mass known as cancer cachexia. The physical impact of cachexia contributes to decreased patient quality of life, treatment success and survival due to gross alterations in protein metabolism, increased oxidative stress and systemic inflammation. The psychological impact also contributes to decreased quality of life for both patients and their families. Combination therapies that target multiple pathways, such as eicosapentaenoic acid administered in combination with exercise, appetite stimulants, antioxidants or anti-inflammatories, have potential in the treatment of this complex syndrome and require further development.
Keywords: Cancer cachexia, Oxidative stress, Antioxidant, Eicosapentaenoic acid, Oxypurinol
Introduction
Cancer cachexia is a complex condition of tissue wasting which develops as a secondary disorder in cancer patients and leads to progressive functional impairment. Cancer cachexia is characterised by systemic inflammation, negative protein and energy balance and involuntary loss of lean body mass, with or without wasting of adipose tissue [1]. Clinically, cachexia is represented by significant weight loss in adults and failure to thrive in children [2], accompanied by alterations in body composition and disturbed balance of biological systems [3–5]. Whilst the loss of skeletal muscle mass is the most obvious symptom of cancer cachexia, cardiac muscle is also depleted, though other visceral organs tend to be preserved [3].
Cachexia has been recognised as a serious condition for some time; however, due to the complex nature of the condition, guidelines for its definition and diagnosis have only recently begun to emerge [1, 2]. Even so, there is great variation in definitions, which present problems when comparing studies and informing clinical diagnoses [6, 7]. This in turn may affect the ability to identify cachectic patients and appropriate treatment, for which there is no globally recognised ‘gold standard’. Current therapies focus on palliation of symptoms and reduction of distress of patients and families rather than a cure [8]. As such, cachexia remains a largely underestimated and untreated condition [2, 9]. Approximately half of all patients with cancer experience cachexia [10, 11], with the prevalence rising as high as 86 % in the last 1–2 weeks of life [12], and 45 % of patients losing more than 10 % of their original body weight over disease progression [13]. Death usually occurs once weight loss has reached 30 % of the patient’s historic stable body weight [3], with cachexia being directly attributable for 20 % of cancer deaths [14]. Whilst cachexia is seen in several other diseases, such as HIV/AIDS, sepsis, chronic obstructive pulmonary disease and congestive heart failure, the loss of muscle mass has been shown to occur most rapidly in cancer patients [15].
Due to the unique mechanisms involved in each disease, it is likely that factors influencing the onset of skeletal muscle cachexia vary between conditions [16], despite sharing several common pathways [7]. The progression of the disease also varies between cancer types, with cachexia being more prevalent within pancreatic, colon or non-small cell lung malignancies [1]. Whilst loss of adipose tissue often occurs prior to wasting of lean mass [17], unlike anorexia, where adipose tissue is depleted in response to nutritional deficit, cachexia degenerates both adipose tissue and skeletal muscle indiscriminately [16]. It is a profound atrophic response that cannot be directly attributed to lowered calorific or nutrient intake nor fully reversed by increased nutritional support [6, 16]. Cachexia is also considered distinct from conditions of starvation, age-related sarcopenia, malabsorption and other similar pathological states [2, 7].
Currently, most definitions of cachexia focus on weight loss alone. Cachexia is generally defined as being involuntary weight loss of >5 % from historical weight, a body mass index (BMI) <20 kg/m2 with any degree of weight loss >2 % or a skeletal muscle index consistent with sarcopenia with any degree of weight loss >2 % [1]. However, these defining characteristics have yet to be validated in a cancer-specific cachectic population and fail to consider other widely accepted and characterised hallmarks of the condition, such as inflammation, altered body composition, accelerated protein degradation, increased treatment toxicity, fatigue and reduced quality of life [9]. They also do not take into account the severity of the disease, which may be compounded by factors such as weight loss from an already low BMI, where a small change may have a much larger impact than the same loss in someone of higher BMI [1].
These developing definitions should not only describe established cachexia, but provide criteria for the identification of ‘at-risk’ populations. Historically, classification or staging of cachexia has been poorly represented, with most studies focusing on the mid-to-late stages of the disease. Therefore, an improved three-step classification of cachexia has been proposed following international collaboration and development [1]. These steps now include:
Pre-cachexia—when a patient has weight loss <5 %, but has not yet developed serious complications.
Cachexia—where the syndrome is progressing, with weight loss exceeding the above-mentioned parameters, but still potentially able to be treated.
Refractory cachexia—the point at which the disease is no longer responsive to treatment or when treatment benefits are outweighed by burden and risk.
Often, the refractory stage is dictated by the overall stage of underlying illness and condition of the patient, rather than cachexia alone [1], and reflects periods of palliation, where the focus of treatment moves from cure and control to maintenance of quality of life [12]. This type of grading system allows for greater tailoring of treatment to patients in various stages of disease progression and would enable targeted research and therapies to be developed for each stage.
Impact
Quality of life
Cancer cachexia has been shown to impact on patient outcomes, quality of life and survival when compared to weight-stable patients. Cancer cachectic patients experience numerous complications including, but not limited to, reduced effectiveness of chemotherapy, reduced mobility and reduced functionality of muscle-dependent systems, such as the respiratory and cardiovascular systems, leading to decreased quality of life and survival [18–20].
Research by Ravasco et al. [21] indicated that self-rated quality of life scores in patients with cancer were more often determined by issues relating to weight loss and nutritional status (50 %), compared to cancer location, disease duration or cancer stage (30, 3 and 1 %, respectively). Studies using self-assessment questionnaires also tend to show higher prevalence of symptoms than those reported during a standardised review [12]. In particular, quality of life in patients with advanced cancer is most significantly affected by symptoms associated with pain, fatigue and reduced appetite, in particular toward refractory cachexia [22]. Patients may feel they have more time and/or feel free to indicate the presence of symptoms less often mentioned in interview, and as such, questionnaires may identify symptoms not considered important by the patient and thus not addressed [12]. Cachectic patients are also more likely to score lower than their weight-stable counterparts in standard quality of life measures [19]. Decreased quality of life scores have been shown to be accompanied by significant decreases in physical activity and exercise capacity, which is strongly related to weight loss [23].
Cachexia negatively impacts on surgical risk and response to chemotherapy and radiotherapy and ultimately results in decreased quality of life [24]. Cancer patients experiencing weight loss leading up to and during chemotherapy receive a lower initial dose and experience more frequent and severe dose-limiting toxicity when compared to weight-stable patients [25, 26], consequently receiving significantly less treatment [27]. These patients also experienced decreased quality of life, performance status and survival intervals and lowered response to treatment. Importantly, these negative outcomes appear to occur due to decreased treatment and increased toxicity, rather than alterations in the effectiveness of the therapy itself. Cancer patients without weight loss have demonstrated a better chance of survival and a greater response to cancer therapy than their cachectic counterparts [18]. This indicates that an effective treatment for cachexia would result in more positive outcomes for these patients. A reduction in the occurrence or progression of cancer cachexia would have several flow-on effects in terms of health economic outcomes, for example, reduced hospital admissions for adverse effects of cachexia, shorter hospital stays due to greater capacity to regain health sooner or maintain health longer and reduced attendance to emergency departments for cachexia-related complications. The complex interplay of systemic inflammation, metabolic disruption and the presence of numerous factors that are now thought to play an important role in the development and progression of cachexia make it unlikely that a single therapy will have the ability to combat the condition as a whole. Rather, a multi-targeted approach should be considered when developing treatment plans for cachectic patients [28]. This is supported by numerous single modality studies that, whilst showing theoretical merit or some minor improvement, do not produce a substantial change in either quality of life or patient outcomes [3, 4, 24, 29, 30].
Social and psychological
Cancer cachexia has a significant psychological impact on both patients and their families, being identified as one of the top 2 most frequent and devastating problems in advanced cancer [31]. However, in the past, these concerns have taken a back seat to biomedical aspects of research. There is a high prevalence of depression in cancer patients (10–30 %) compared to the general population (5–10 %), with depression leading to reductions in drug compliance and effectiveness [32, 33]. Clinical depression in cachexia appears under-recognised and undertreated, perhaps due to the difficulty in distinguishing between reactive demoralisation and clinical depression or due to overlapping symptoms of illness and depression [34]. However, the increased expression of shared inflammatory cytokine pathways ([32]; see also Section 5) may lead to increased prevalence of clinical depression in a cachectic patient population. As such, treatments that address pro-inflammatory cytokine activity in cachexia may also contribute toward the alleviation of clinical depression in susceptible patients.
Further to clinical (inflammatory) depression, high psychologic distress occurs in response to reduced appetite and food intake, increases in fatigue and significant alterations in appearance [35], which contribute to a cascade of losses experienced by both the patient and their family. Families often rationalise that, if food intake is increased, weight will be regained and survival increased, with a failure to increase intake being equated with expedition of death [36]. This stems partially from a lack of communication with families about the nature and causes of wasting in cachexia, as atrophy is caused by factors independent of nutritional or calorific intake [36, 37], and also from the need to take an active role in treatment, with food preparation being highly symbolic of this need to nurture [36, 38]. This often leads to conflict between the patient and their family, as the patient’s refusal of food is interpreted as a rejection of care and support, increasing anxieties over food and ultimately contributing to a decreased quality of life [35, 36, 38]. Patients, on the other hand, more often associate their weight loss with their decline during disease progression, recognising that increased intake is futile and, as such, view weight loss as inescapable, with pain being of much more immediate concern [39]. It has been noted that many patients, despite an absence of appetite, often retain the motivation to eat, whether to avoid confrontation or to maintain some aspect of normalcy about food [40].
Alterations in body image also have a significant impact on patients, with loss of weight often perceived as undermining identity and self-esteem and alienation from themselves, i.e. ‘not recognising the person in the mirror’ [31, 37]. Given that the severe physical decline of cachexia is quite evident to sufferers and those they engage with, the social consequences of weight loss are also a major source of distress. Self-consciousness acts as a barrier to social engagement, with patients often choosing to isolate themselves from previous social circles rather than be ‘besieged by attention’ [37], with negative reactions highly stigmatising and positive engagement often regarded as a reminder of their illness [31, 37]. Given that conflicts often arise from reduced food intake, patients may further increase social isolation to avoid confrontation with family [36, 41]. The appearance of refractory-stage cachectic patients is often likened to that of death camp victims during World War II, indicating the associations by family and friends that this is a neglect-linked disease that if left untreated will ultimately end in death [37].
It is important to recognise that cachexia is a condition that has profound psychological as well as physiological implications for patients and their families. Better communication from researchers and healthcare professionals with patients and their carers is of great importance to not only reduce the burden of disease but also provide better understanding and support during disease progression.
Anorexia and appetite in cachexia
Unlike many other forms of weight loss, cachexia is not the result of reduced calorific or nutrient intake alone. The term ‘malnutrition’ is often misused with regard to cachexia, as this incorrectly implies that the underlying cause of wasting is associated with diet and nutrition and that increasing intake or absorption of nutrients and calories will solve the problem [40]. Whilst malnutrition is often present for various reasons [21], unlike forms of weight loss such as anorexia nervosa where wasting is caused by decreased energy consumption, it is not the underlying cause in cachexia [2]. It has previously been shown that increasing calorie intake does not replenish the loss of skeletal muscle mass but rather increases total body weight through water retention and replenishment of fat stores, with some steroidal treatments in fact having a negative impact on muscle retention [42–45]. Other studies have shown that, whilst nutritional counselling may improve calorific intake, it did not assist to increase weight, anthropometrics, therapeutic response, quality of life or survival [46–49] and that there is little observed benefit from parenteral nutritional support [50–52]. However, as previously discussed, nutritional counselling and a subsequent increase in calorie intake may help relieve ‘caregivers anxiety’, prevent further decline in nutritional status and even improve patient outcomes during radiotherapy [53, 54], with nutritional counselling increasingly promoted as part of a multimodal approach to therapy [55, 56]. These results indicate that, whilst malnutrition may play an important role in cachexia, it is not the major factor in the development and, although increased intake of nutrients and calories may be considered for the treatment of cachexia, it should not be the only consideration.
Chemosensory alterations in cancer and during cancer therapy are well documented [57–62], with alterations in taste and smell often contributing to the development of food aversion and reduced hedonic response. This in turn may lead to the development of anorexia and acceleration of the disease. Zinc has been shown to play an important role in taste perception, with deficiency linked to a diminished sense of taste among cancer patients undergoing radiation therapy, in particular irradiation of the head and neck [59, 63]. It has been proposed that zinc acts as a cofactor for receptors in the apical pore of taste bud membrane, and therefore, changes in the availability of zinc causes conformational changes to these pores [59]. This in turn reduces the amount of taste stimuli that may pass through the pore, reducing taste response. There has been some argument as to whether this response is linked to low serum zinc levels [59, 63–65]; however, whilst supplementation does not preserve taste perception in those undergoing radiation therapy [65, 66], it does reduce symptom severity and may improve recovery of acuity and response to taste stimuli [59, 65].
Decreased appetite and early satiety have a high prevalence in the late stages of disease, with decreased appetite described in more than 50 % [14] and early satiety in 23–51 % of patients [12, 67]. These changes suggest a disruption of central and peripheral signalling for regulation of eating behaviour [48, 68] and, together with metabolic abnormalities generated by the disease, drive the negative protein and energy balance thought to be the key contributor of cachexia.
Futile cycling and resting energy expenditure
The condition of cachexia is associated with metabolic disruption from various causes, all of which lead to the eventual increases in energy expenditure, systemic stress and disruption of normal cellular function. The balance of protein synthesis and degradation is one of the most obvious aspects of metabolism disruption in cancer cachexia. It has been widely observed that the rate of muscle protein catabolism increases in cachexia, whilst anabolism of new proteins decreases, resulting in net protein breakdown [15, 69–71]. This increase in protein turnover is higher in cancer cachexia compared to weight loss associated with other diseases and leads to increased energy demand of approximately 100 kcal/day [72–74].
Resting energy expenditure (REE) is also increased in the cachectic state, with futile metabolic cycling accounting for much of this increase. One example of futile cycling is the glucose–pyruvate–lactate transformation seen in the Cori cycle. Lactic acid production from the tumour drives the conversion of lactate to pyruvate and then into glucose in the liver, a process that has high energy expenditure. This glucose is then moved into the circulation and back to the tumour, where it is again transformed into lactate, and the cycle continues [75]. Glucose from this cycle may also serve to feed the tumour, causing it to grow, produce more lactic acid and further drive the cycle. In cachexia patients, the Cori cycle has been described as accounting for 50 % of total glucose turnover, compared to 20 % in cancer patients that are weight stable [75]. Uncoupling proteins (UCPs), related to the regulation of mitochondrial proton gradients and production of reactive oxygen species (ROS) in skeletal muscle and adipose tissue, may also play a role in the increased REE observed in cachexia [15]. In particular, the expression of UCP2 and UCP3, associated with energy expenditure and metabolism in skeletal muscle, are up-regulated in the cachectic state, indicating the involvement of these mechanisms [15].
Increased mass and proportion of high metabolic tissue such as the liver occurs in cachexia and has been shown to contribute significantly to this increase in energy expenditure [76]. Cachectic patients also show an increase in the oxidation of branched-chain amino acids from muscle proteins for use in gluconeogenesis [77], which may be triggered by this increase in energy expenditure, and would ultimately contribute to muscular degeneration in cancer cachexia. However, the traditionally accepted view that increased REE and hypermetabolism are essential factors in the pathogenesis of the disease has been disputed, with a heterogeneous picture of REE emerging that range from 60 to 150 % of the norm [78–81]. Further, whilst REE may be increased, total energy expenditure may be decreased due to reduced physical activity [81, 82]. Assessments of metabolic alteration in cachectic rodents has described a progressive hypermetabolic state in pre-cachexia and early cachexia, passing through a stable metabolic phase and finally progressing to a pre-terminal hypometabolic phase [83]. These differences in metabolic pathology may be attributed to tumour-specific factors, a view which has been supported by preliminary studies in a human cohort [84].
Inflammation and circulating factors
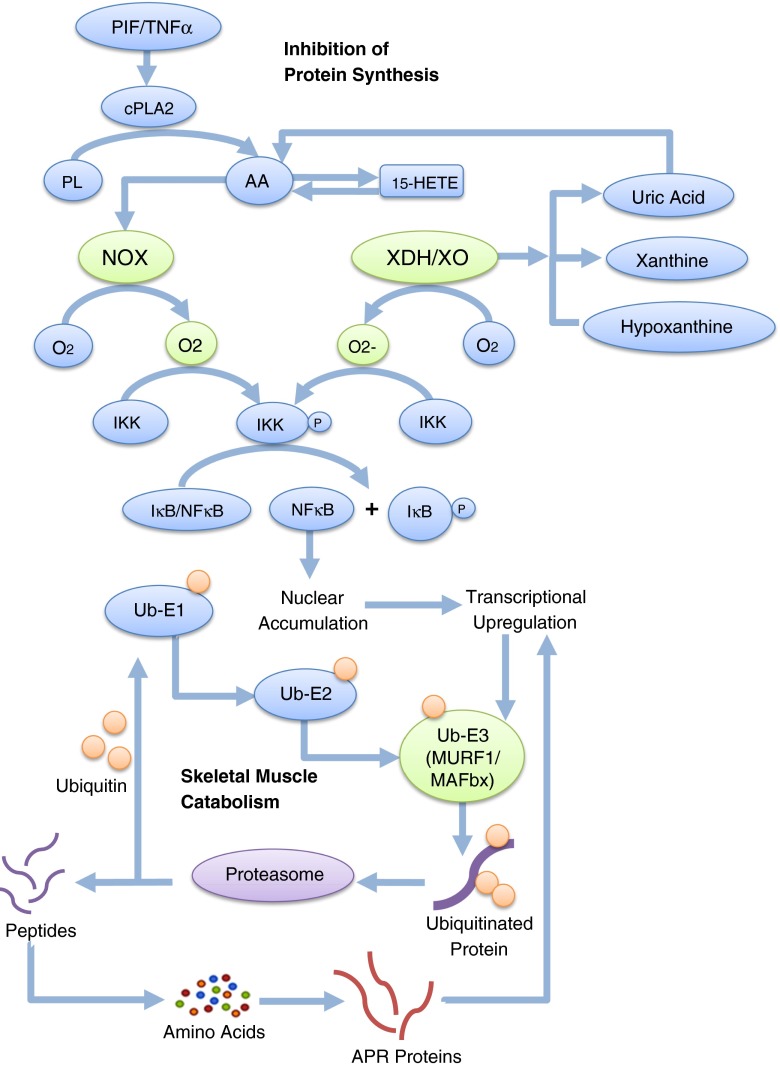
Systemic inflammation is another symptom seen in cancer cachexia, indicated by the production of acute-phase response (APR) proteins such as C-reactive protein (CRP) and fibrinogen. CRP is considered an accurate measure of pro-inflammatory cytokine activity [85] that has been implicated in muscle wasting by its binding to exposed ligands in damaged cells and has been shown to aggravate tissue damage in ischemia–reperfusion injury [86]. The APR has been related to the inflammation seen in cachexia [87, 88] and the reduced quality of life and shortened survival in these patients [89–92], causing increased muscle catabolism and diversion of amino acids from muscle anabolism to feed the amino acid pool required for APR protein anabolism (see Fig. 1) [93, 94]. Whilst these mechanisms are designed for host defence and tissue repair, short-term gain may be outweighed by long-term loss of lean body mass. Increases in CRP have been shown to correlate with increased weight loss in cachectic patients [85], indicating that there is an increase in pro-inflammatory cytokine activity during the progression of the disease [95, 96], with eicosanoid-driven inflammation also implicated [97–99].
Fig. 1.
An example pathway for the induction of the ubiquitin proteasome pathway. Tumour factors and pro-inflammatory mediators initiate a complex signalling cascade that eventuates in increased skeletal muscle catabolism. PL phospholipids, AA arachidonic acid. Adapted from [118]
The presence and severity of cachexia correlates poorly with tumour size [100], and therefore, metabolic alterations are more likely the result of mediators produced by the tumour or by the body in response to the tumour. Several pro-inflammatory cytokines are elevated in patients with cachexia, including tumour necrosis factor-alpha (TNF-α), interleukin-1 (IL-1) and interleukin-6 (IL-6), all of which have been shown to induce cachexia-like effects when administered in the absence of tumours [11]. TNF-α is a circulatory factor which increases gluconeogenesis, lipolysis and proteolysis, whilst causing decreases in protein, lipid and glycogen synthesis, induces the formation of IL-1 [11] and has been demonstrated to stimulate the expression of UCP2 and UCP3 in cachectic skeletal muscle [15]. However, whilst it may induce symptoms of cachexia, the inhibition of TNF-α has been shown to neither stop nor reverse cancer cachexia [100]. This indicates that TNF-α may be involved in the development of cachexia, but is not solely responsible for the effects seen in cachectic patients. IL-1 induces anorexia in cachectic patients as it causes an increase in plasma concentrations of tryptophan, which in turn increases serotonin levels, causing early satiety and suppressing hunger [11]. IL-1 also induces the production of IL-6, an immune-linked cytokine that increases lipolysis and contributes to weight loss. Levels of IL-6 were observed to be lower in weight-stable patients than those with cachexia; however, whilst IL-6 is thought to be important in the development of cachexia, it has been shown not to be solely responsible and works through indirect action [11]. As such, it is likely that a complex interplay of these factors is responsible for cachexia, rather than each working in isolation [101]. However, there is limited variation in circulating cytokines [102], and cytokine production by isolated peripheral mononuclear cells suggests that local production in affected tissues is more important and relevant to cachexia than systemic circulation of these factors [82].
Proteolysis-inducing factor (PIF) is a circulatory factor produced by some tumours and is present in some cohorts of cancer patients with cachexia, but absent in cancer patients without active weight loss or weight-losing patients with benign disease [70, 103–105]. Patients with circulating PIF experience a significant decline in body weight, mainly of lean body mass, accounted for by a 50 % reduction in protein synthesis and a 50 % increase in protein catabolism [106]. PIF has been shown to increase the expression of ubiquitin proteolytic pathway (UPP) elements (see Fig. 1) [103, 106–108], induce the accumulation of ubiquitin-conjugated proteins [15] and play a role in the increased production of the cytokines IL-6 and IL-8, indicating that PIF acts as part of an inflammatory response pathway in the cachectic state [109]. However, there has been some debate over the existence of PIF, with several studies unable to identify the factor outside of the murine adenocarcinoma 16 model and having difficulty in identifying a human homologue through conventional methods, casting doubt as to the relevance of a PIF homologue in a clinical setting [110–112]. Lipid-mobilising factor/zinc-a2-glycoprotein (ZAG) has been demonstrated to play an important role in the lipid depletion that occurs in cachexia and other catabolic states. Whilst ZAG is expressed in normal tissues such as the liver and adipose tissue [113], it is also over-expressed in patients with several types of tumour [114, 115] and acts as a local factor in catabolic states, mobilising lipids from adipose by increased lipolysis for gluconeogenesis [116]. However, whilst there is a strong relationship between adipose ZAG release and nutritional status, it has been indicated that there is no relationship between release of ZAG and BMI or relative fat mass nor circulating levels of ZAG and nutritional status [116]. Whilst stimulating adipose depletion utilising β-adrenoreceptors, ZAG has also been shown to stimulate skeletal muscle hypertrophy via the cAMP-mediated pathway and decreased proteasome activity [117]. Therefore, ZAG may in fact play a protective role in fat-free mass and may explain why depletion of adipose stores often precedes the loss to skeletal muscle protein seen in cachexia [17, 117].
Oxidative stress
ROS are oxygen-derived molecules that have an odd number of valence electrons. As a result, these molecules are highly reactive and, if not neutralised by antioxidant enzymes, may cause damage to DNA, proteins and lipids within the cellular environment [119]. ROS such as superoxide (O−·2), hydrogen peroxide (H2O2) and hydroxyl radicals are normal products of cellular metabolism, commonly utilized in cellular signalling cascades (see Fig. 1); however, increased levels caused by environmental stress, metabolic imbalance or reduced antioxidant activity may lead to a state of oxidative stress, resulting in extensive oxidative damage [119]. Oxidative stress has been uncovered as one of the key players in the development of cachexia, contributing to muscle wasting both directly, through oxidative damage, and indirectly, through redox signalling in degradation pathways [120]. Oxidative damage, ROS levels and mRNA levels for ROS-producing enzymes have all been shown to be elevated in the cachectic state [121, 122], whilst the production and activity of antioxidant enzymes have been shown to decrease [123, 124], indicating a reduced capacity for the conversion of excess ROS into less toxic molecules.
The nicotinamide adenine dinucleotide phosphate (NADPH) oxidase (NOX) is an enzyme system that catalyses the production of O−·2 from NADPH and oxygen and has been implicated as a major contributor of ROS in cancer cachexia [125]. NOX was first described in phagocytes as an immune response against microbial pathogens [126]; however, NOX is now known to function in many non-phagocytic cells and plays a role in cellular signalling [127], in particular with the formation of O−·2. The NOX enzyme is made up of several subunits, and an up-regulation of any one of these components may, therefore, potentially increase enzyme activity in cachexia. The ROS produced by NOX are associated with several negative effects within cells, such as apoptosis and inflammation, which ultimately contribute to the onset and progression of several diseases [128]. NOX also acts as a downstream regulator of several redox signalling pathways, in which the ROS it produces act as steps in a signalling cascade [122] that eventually result in the alteration of expression of target genes (see Fig. 1). In addition, an excess of NOX activity, when coupled with uncompensated antioxidant activity in cancer cachexia, can contribute to oxidative stress and associated damage.
Whilst some of the pathways involved in the excess production of ROS have been studied at length in cancer cachexia, there are others that have been implicated to induce oxidative insult in other diseases, whose roles have yet to be studied in cancer cachexia. Xanthine oxidoreductase (XOR) is an enzyme with two distinct forms that are responsible for catalysing the conversion of hypoxanthine to xanthine and xanthine to uric acid [129]. Xanthine dehydrogenase (XDH) is expressed in vivo and uses NAD + as an electron acceptor for the reduction reaction, forming NADH. In the presence of pro-inflammatory mediators, XDH readily cleaves into xanthine oxidase (XO), which instead uses molecular oxygen for the conversion of hypoxanthine to xanthine and xanthine to uric acid, producing the highly reactive O−·2 or H2O2 [129]. Uric acid has also been shown to act as an inflammatory agent, stimulating an inflammatory response to cell death in multiple tissues [130], and has been found in high levels in the serum of cachectic patients whose primary disease is not cancer [131, 132]. Whilst XO is not usually present in high levels in skeletal muscle, elevated levels are commonly seen in muscle tissue damage and ischemia–reperfusion injury [133]. High levels of XO have also been observed in the blood of cancer patients compared to patients without cancer [134], though this has yet to be documented in cachectic skeletal muscle. The abundance of pro-inflammatory factors present in cachexia may lead to an increase in the cleavage of XDH to the XO form, explaining higher circulating levels of XO, consequently contributing to increased O−·2 and uric acid levels. The inhibition of XO has recently been shown to improve skeletal muscle dysfunction associated with oxidative stress in a model of sarcopenia in aging rodents [135] and, though preliminary, suggests that it may effectively dampen ROS production that contributes to muscle wasting, an application that may lend itself to the treatment of muscle wasting associated with cachexia. XO has also been suggested to play a role in secondary inflammation in skeletal muscle after eccentric exercise [136], a further possible role for this enzyme in cachexia.
The body has a finely balanced and highly structured antioxidant defence system, which provides protection from ROS-induced damage. If this balance is shifted away from antioxidants by a decrease in antioxidant activity or an increase in ROS production, a state of oxidative stress is observed [119, 120]. Oxidative stress has a detrimental effect on the cellular environment and may be one of the key factors in the development of cachexia [120]. Superoxide dismutase (SOD) is an enzyme responsible for the dismutation of O−·2 into H2O2 and oxygen. In some cachexia studies, the activity of SOD in skeletal muscle is decreased, contributing to oxidative stress and cellular damage [124, 125], whilst others have shown no change in the activity of SOD [121]. Catalase is another antioxidant enzyme, which breaks down H2O2 into oxygen and water. Whilst not as reactive as O−·2, in high levels, H2O2 can also cause damage to cells and disrupt metabolism. A decrease in catalase activity has been observed in cachexia studies [123], indicating that the system would contribute to an increase in oxidative stress. Glutathione peroxidase (GPx) also plays an important role in the metabolism of ROS, utilising glutathione as a reducing substrate to reduce hydroperoxidases. Studies of cachectic tissue have shown no change in the activity of GPx [123, 137]. Collectively, these studies suggest not only the reduced antioxidant capacity of these systems but also their inability to respond to increased oxidative conditions and, therefore, an inability to protect the cell from oxidative stress in the cachectic state, a malfunction that may be the major contributor to the state of oxidative stress observed in cancer cachexia.
Skeletal muscle in cachexia
The loss of lean body mass, in particular skeletal muscle, is the most prevalent and obvious symptom of cancer cachexia, contributing significantly to negative patient outcomes and quality of life, as previously discussed. Muscle atrophy in cachexia results from a combination of increased catabolism by cytokine-dependent hyperactivation of various pathways and reduced protein anabolism [138–142]. Interestingly, muscle protein synthesis may at times be elevated in cachexia due to increased availability of amino acids from accelerated muscle catabolism [1]; however, this is not sufficient to outweigh the net protein loss. There has been some debate as to whether certain muscular elements, such as the myosin heavy chain, are selectively targeted for degradation or whether general, untargeted wasting occurs [71, 143, 144]. As yet, no consensus has been reached and may be dependent upon other factors, such as tumour type or levels of particular circulating factors. Decreased muscle strength has been shown to be a strong predictor of morbidity and mortality in cancer patients [145, 146] and has been linked to fatigue [147–149]. The loss of skeletal muscle mass in cachexia is not restricted to those patients that appear thin, with low muscularity in obese patients recognised as an independent prognostic indicator [1, 150].
Pathways to protein degradation
The progressive catabolism of muscle in cancer cachexia suggests a pivotal role in systems of protein degradation, such as the UPP, which has been found to be up-regulated both in experimental models and patients with cancer cachexia [151–154]. Components of the UPP also increase in patients with pre-cachexia, suggesting that not only does the system contribute to muscle atrophy in cachectic patients but also indicates a causative role early in disease development [151, 155]. Before proteins can be degraded by the UPP, they must first be targeted by conjugation to multiple molecules of ubiquitin. In order for this conjugation to occur, ubiquitin must first be activated by an ubiquitin-activating enzyme (E1) and then transferred to the active site of an ubiquitin carrier protein (E2). The bound E2 recognises ubiquitin-conjugating enzymes (E3 or E3 protein ligase), which allow conjugation reactions to take place, forming a chain of ubiquitins linked to each other and the protein substrate. Only when ubiquitin is targeted to a selected protein can it then be recognized by the proteasome and processed into smaller peptides [15, 156]. In particular, three E3 protein ligases have been shown to be active during proteolysis in muscle atrophy, namely, E3α, muscle-specific F-box (MAFbx)/atrogin-1 and muscle-specific ring finger 1 (MuRF1) [143, 157–162]. Oxidative stress is thought to play a key role in the induction of this system (see Fig. 1) due to the increased redox activation of the transcription factor NF-κB, which in turn increases proteasome expression [154], indicating that excess ROS production plays an important part in increased activity on the UPP and, therefore, muscle degradation. NF-κB, cytokine and proteasome inhibitors such as bortezomib and infliximab initially demonstrated potential to ameliorate cachexia-associated weight loss, however did not impress in trials. These proteasome inhibitors have been deemed ineffective as individual treatments for cachexia and may in fact have a negative effect on patient outcomes [163–165].
Further studies suggest that the UPP may not play a role in the early stages of muscle wasting, where patients with <10 % weight loss showing no increase in UPP mRNA [166, 167] or activity levels [168] compared to control patients. Pre-cachectic patients also had no increase in NF-κB-mediated inflammation in muscle, despite the presence of circulating/systemic inflammatory markers, and may suggest that a transition from systemic to local inflammation is required for the UPP to become active in these patients [168]. In contrast, calpain-dependent proteolysis has been implicated in gastric cancer patients with little or no weight loss, with increased mRNA levels and activity of components of this system [166]. However, the activity of the UPP and calpain systems have not yet been looked at in parallel, and longitudinal studies would be beneficial in determining if these patients developed further weight loss and if the UPP was activated in later stages.
TNF receptor adaptor protein 6 (TRAF6) has also been indicated as a major upstream regulator of muscular atrophy, with its role as an E3 ligase in the ubiquitination of proteins, leading to the induction of autophagy [169]. The autophagy–lysosomal pathway is involved in myofibril degradation through the activation of NF-κB [170], the activity of which is reduced when TRAF6 is knocked out in the skeletal muscle of mice [169]. The inhibition of TRAF6 also resulted in the attenuation of wasting in cachectic mice, with decreased expression of the E3 MuRF1 and the autophagy-related genes LC3B and Beclin1 [169]. TRAF6, therefore, presents another key target for treatment, with inhibition potentially attenuating downstream cytokine signalling cascades leading to UPP and autophagy-mediated wasting.
Treatments
It is generally accepted that the only way to treat cachexia is to cure the cancer [52]. However, this is not always viable, and even after resection, weight loss may continue for as long as 12 months [20]. Due to the complex nature of cancer cachexia and the vast array of contributors to muscle wasting involved, there is as yet no globally effective or accepted treatment for this condition. It has also been recognised that patients may exhibit different catabolic mechanisms, dependent upon various factors, and therefore, it may be appropriate to discriminate between patients in order for the best form of treatment to be applied [99].
Previously, the main focus of treatment development has been in the maintenance and recovery of lean body mass, in particular upstream intervention of cytokine signalling. Whilst interfering with these systems was considered promising, there was limited efficacy in trials [29, 30]. As such, focus has now shifted toward a downstream approach, with inhibition of the UPP of particular interest [158, 171, 172]. Stimulation of anabolism has also been targeted, with testosterone-related hormone therapy shown to increase the expression of skeletal muscle androgen receptors, thereby increasing utilisation of amino acids derived from protein degradation and stimulating muscle synthesis [160]. Non-steroidal anti-inflammatories such as indomethacin and ibuprofen have been trialled and shown to reduce inflammation and lower levels of acute-phase proteins, IL-6 and cortisol [173–177], whilst antioxidant supplementation such as combination α-lipoic acid, carbocysteine lysine salt and vitamins E, A and C also had some success in multimodal phase II trials [178, 179].
Combination trials are becoming increasingly prevalent as better understanding of the mechanisms and pathophysiology of cachexia emerges, with simultaneous, multi-target therapies more likely to elicit desirable outcomes than single agents [9, 180]. This view has been confirmed by a large five-arm study, in which patients were prescribed oral antioxidant supplementation, plus medroxyprogesterone acetate or megestrol acetate, eicosapentaenoic acid (EPA)-enriched nutritional supplement, carnitine or thalidomide [180]. The combination therapy showed improved response over each in isolation, in terms of primary end points (LBM, REE and fatigue) as well as inflammation, suggestive of a compound or synergistic effect when given simultaneously. A combination therapy of this sort, where the intervention is largely diet- or nutrition-based, with the addition of low-cost drugs, may assist with compliance [180]. However, in a population where polypharmacy, in terms of the number of drugs and inappropriate drug use (duplication, underuse, interaction, etc.), is prevalent, the introduction of multiple new therapies increases the risk of adverse interactions [181]. Increased polypharmacy also places a greater burden on patients, both medically and financially, and may lead to non-adherence [181]. A further study from the Mantovani group has highlighted this issue in cachexia, where the individually promising treatments carnitine (amino acid involved in cell energy metabolism), celecoxib (anti-inflammatory, COX2 inhibitor) and megestrol acetate (appetite stimulant) were trialled in combination [182]. The study indicated that carnitine and celecoxib without megestrol acetate was non-inferior to the three in combination, and therefore, the two-drug combination may be more feasible in this instance.
Combination interventions that target cachexia-related pathways in multiple locations, whilst also augmenting treatment of other aspects of patient disease, may assist in reducing the polypharmacy implemented for symptom management. Whilst the search for effective therapy combinations for the treatment of cachexia continues, we propose EPA and oxypurinol as examples of how a combined therapy with common targets may be utilised as part of a broader treatment strategy here.
Eicosapentaenoic acid
EPA is an omega-3 fatty acid which has received much attention in recent years due to the emergence of studies reporting its effects as a broad-spectrum health-promoting agent. EPA supplementation at clinically relevant doses is generally well tolerated in capsule and liquid form, with high doses above clinical relevance having mild side effects of loose bowel movements, bloating and fishy aftertaste, where dose is limited by low-purity fish oils, and sensations of ‘fullness’ rather than toxicity [183, 184]. Along with this high tolerability, EPA’s intersection with multiple pathways involved in cancer cachexia makes it an ideal candidate as a treatment for the condition.
EPA has exhibited anti-tumour properties, inhibiting cancer growth during tumourigenesis and early stages of development through a variety of mechanisms, such as apoptosis, cell signalling and gene expression The anti-tumour properties of EPA continue with disease progression, improving the efficacy of chemotherapy by protecting non-target tissues and improving its effect on tumour tissue, and may be responsible for stabilisation in dose-limiting toxicity, seen with the addition of EPA supplementation [99, 185].
In recent years, EPA has been trialled as a treatment for cancer cachexia due to its upstream regulation of the expression and activity of the UPP. EPA may alter the balance of eicosanoids toward the production of less inflammatory compounds than those produced by omega-6 fatty acids such as arachidonic acid [186, 187]. EPA replaces arachidonic acid in phospholipid membranes when consumed at high levels [188] and has also been shown to inhibit the production of the eicosanoid 15-HETE from arachidonic acid, which has been implicated in UPP regulation in murine models of cachexia [191]. The administration of EPA attenuates the activation of NF-κB by upstream stabilisation of the IκB/NF-κB complex [98, 189, 190] and reducing nuclear accumulation, which in turn reduces transcriptional activation of proteasome subunits involved in protein degradation [191]. EPA is the only nutritional supplement known to interfere with the UPP [24, 192], but results from trials investigating its anti-cachectic effects are contradictory and often suffer from high attrition [194].
Recent research has shown that EPA can act as an agonist of SOD, with supplementation leading to increased SOD activity in mice treated with chemotherapeutics [195], and has been hypothesised to preserve adipose tissue though interference in glucocorticoid signalling in the regulation of ZAG [196].
Animal trials of EPA have been largely successful [192], as has its combination with other therapeutic approaches, such as leucine supplementation and a high protein diet [77], and in conjunction to other drugs as detailed previously [180]. Several small-scale human trials have demonstrated EPA to significantly reduce the production of cytokines and concentration of CRP and PIF, improve overall weight and functional status and increase appetite in refractory cancer cachexia patients, and in contrast to megestrol acetate, improved lean body mass [184, 186, 187, 193, 197–199]. Jatoi and colleagues demonstrated that EPA scored well against megestrol acetate in areas of overall weight gain, increased survival and improved quality of life, although the proportion of patients gaining <10 % of the body weight was lower in the EPA group [194]. It has further been confirmed that EPA-associated weight gain or stabilisation in cachectic patients is not due to water retention [186, 193]. EPA’s amelioration of cachexia has been shown to be particularly effective in the presence of a targeted exercise regime [77, 200, 201], supporting the inclusion of physical activity in multimodality treatments.
Oxypurinol
Oxypurinol is a non-competitive, irreversible inhibitor of XO, considered more potent than allopurinol, of which it is a metabolite [202]. Currently, oxypurinol is used as a treatment for conditions where XO is a contributor and has been shown to decrease tissue wasting and increase cardiac function in cachectic animals [203]; however, its specific action in cachexia is yet to be elucidated. Oxypurinol indirectly inhibits XOR through feedback inhibition of amidophosphoribosyltransferase, the first step in purine synthesis, caused by products of increased salvage of hypoxanthine and xanthine [204]. A decrease in purine production and associated metabolism requirements may prompt the reduction of XDH expression and, therefore, downstream activity of this enzyme. Uric acid, produced by XO, increases the conversion of arachidonic acid into its biologically active metabolites (see Fig. 1) [205]. This in turn increases the activation of NOX, perpetuating the signalling cascade that results in the activation of increased transcription of the components of the muscle degradation systems. A combination of the well-documented effect of EPA on attenuation of this pathway, with further inhibition of XO, may have the potential to compound this effect and presents itself as a possible candidate for multimodal treatment of cancer cachexia in conjunction with nutritional support, targeted exercise and further pharmacological intervention.
Conclusion
Our understanding of cancer cachexia has improved dramatically in the past 10–15 years, as the mechanisms involved in the development and progression of the condition continue to be elucidated. However, there still exists a gap in the clinical management of cachexia due to the complex nature of the condition. As pathways continue to be identified, the development of multimodal therapies becomes more effective, with potential for the treatment of muscle wasting not only in cancer patients but also in other pathologies, such as sarcopenia, sepsis, HIV/AIDS and ischemia–reperfusion injury. EPA continues to display promise for inclusion, in particular as part of a broad approach including targeted exercise, nutritional counselling, social support and pharmaceutical intervention.
Acknowledgments
Ms. Vaughan is the recipient of the Victorian Cancer Agency Palliative and Supportive Care Scholarship through the Victorian Cancer Agency funded by the State Government of Victoria, Australia and the Bellberry Support Scholarship through Bellberry Ltd. The authors of this manuscript certify that they comply with the ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle [206].
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Fearon KCH, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12(5):489–495. doi: 10.1016/S1470-2045(10)70218-7. [DOI] [PubMed] [Google Scholar]
- 2.Evans WJ, Morley JE, Argilés J, Bales C, Baracos V, Guttridge DC, et al. Cachexia: a new definition. Clin Nutr. 2008;27(6):793–799. doi: 10.1016/j.clnu.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 3.Tisdale MJ. Cachexia in cancer patients. Nat Rev Cancer. 2002;2(11):862–871. doi: 10.1038/nrc927. [DOI] [PubMed] [Google Scholar]
- 4.Congleton J. The pulmonary cachexia syndrome: aspects of energy balance. Proc Nutr Soc. 1999;58(2):321–328. doi: 10.1017/S0029665199000439. [DOI] [PubMed] [Google Scholar]
- 5.von Haehling S, Lainscak M, Springer J, Anker SD. Cardiac cachexia: a systematic overview. Pharmacol Ther. 2009;121(3):227–252. doi: 10.1016/j.pharmthera.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 6.Springer J, von Haehling S, Anker SD. The need for a standardized definition for cachexia in chronic illness. Nat Clin Pract Endocrinol Metabol. 2006;2(8):416–417. doi: 10.1038/ncpendmet0247. [DOI] [PubMed] [Google Scholar]
- 7.Lainscak M, Filippatos GS, Gheorghiade M, Fonarow GC, Anker SD. Cachexia: common, deadly, with an urgent need for precise definition and new therapies. Am J Cardiol. 2008;101(11A):8E–10E. doi: 10.1016/j.amjcard.2008.02.065. [DOI] [PubMed] [Google Scholar]
- 8.Hopkinson JB, Wright DNM, McDonald JW, Corner JL. The prevalence of concern about weight loss and change in eating habits in people with advanced cancer. J Pain Symptom Manag. 2006;32(4):322–331. doi: 10.1016/j.jpainsymman.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 9.von Haehling S, Anker SD. Cachexia as a major underestimated and unmet medical need: facts and numbers. J Cachexia Sarcopenia Muscle. 2010;1(1):1–5. doi: 10.1007/s13539-010-0002-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diffee GM, Kalfas K, Al-Majid S, McCarthy DO. Altered expression of skeletal muscle myosin isoforms in cancer cachexia. Am J Physiol Cell Physiol. 2002;283(5):C1376–C1382. doi: 10.1152/ajpcell.00154.2002. [DOI] [PubMed] [Google Scholar]
- 11.Tijerina AJ. The biochemical basis of metabolism in cancer cachexia. Dimens Crit Care Nurs. 2004;23(6):237–243. doi: 10.1097/00003465-200411000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Teunissen SCCM, Wesker W, Kruitwagen C, de Haes HCJM, Voest EE, de Graeff A. Symptom prevalence in patients with incurable cancer: a systematic review. J Pain Symptom Manag. 2007;34(1):94–104. doi: 10.1016/j.jpainsymman.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 13.Argilés JM. Cancer-associated malnutrition. Eur J Oncol Nurs. 2005;9(Suppl 2):S39–S50. doi: 10.1016/j.ejon.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 14.Skipworth RJE, Stewart GD, Dejong CHC, Preston T, Fearon KCH. Pathophysiology of cancer cachexia: much more than host–tumour interaction? Clin Nutr. 2007;26(6):667–676. doi: 10.1016/j.clnu.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 15.Giordano A, Calvani M, Petillo O, Carteni M, Melone MRAB, Peluso G. Skeletal muscle metabolism in physiology and in cancer disease. J Cell Biochem. 2003;90(1):170–186. doi: 10.1002/jcb.10601. [DOI] [PubMed] [Google Scholar]
- 16.Tisdale MJ. Cancer cachexia: metabolic alterations and clinical manifestations. Nutrition. 1997;13(1):1–7. doi: 10.1016/S0899-9007(96)00313-9. [DOI] [PubMed] [Google Scholar]
- 17.Fouladiun M, Körner U, Bosaeus I, Daneryd P, Hyltander A, Lundholm KG. Body composition and time course changes in regional distribution of fat and lean tissue in unselected cancer patients on palliative care—correlations with food intake, metabolism, exercise capacity, and hormones. Cancer. 2005;103(10):2189–2198. doi: 10.1002/cncr.21013. [DOI] [PubMed] [Google Scholar]
- 18.DeWys WD, Begg C, Lavin P, Band P. Prognostic effect of weight loss prior to chemotherapy in cancer patients. Am J Med. 1980;69(4):491–497. doi: 10.1016/S0149-2918(05)80001-3. [DOI] [PubMed] [Google Scholar]
- 19.Fearon KCH, Voss AC, Hustead DS. Cancer Cachexia Study Group. Definition of cancer cachexia: effect of weight loss, reduced food intake, and systemic inflammation on functional status and prognosis. Am J Clin Nutr. 2006;83(6):1345–1350. doi: 10.1093/ajcn/83.6.1345. [DOI] [PubMed] [Google Scholar]
- 20.Bachmann J, Heiligensetzer M, Krakowski-Roosen H, Büchler MW, Friess H, Martignoni ME. Cachexia worsens prognosis in patients with resectable pancreatic cancer. J Gastrointest Surg. 2008;12(7):1193–1201. doi: 10.1007/s11605-008-0505-z. [DOI] [PubMed] [Google Scholar]
- 21.Ravasco P, Monteiro-Grillo I, Vidal PM, Camilo ME. Cancer: disease and nutrition are key determinants of patients’ quality of life. Support Care Canc. 2004;12(4):246–252. doi: 10.1007/s00520-003-0568-z. [DOI] [PubMed] [Google Scholar]
- 22.Caissie A, Culleton S, Nguyen J, Zhang L. What QLQ-C15-PAL symptoms matter most for overall quality of life in patients with advanced cancer? World J Oncol. 2011;2(4):166–174. doi: 10.4021/wjon330w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fouladiun M, Körner U, Gunnebo L, Sixt-Ammilon P, Bosaeus I, Lundholm K. Daily physical-rest activities in relation to nutritional state, metabolism, and quality of life in cancer patients with progressive cachexia. Clin Cancer Res. 2007;13(21):6379–6385. doi: 10.1158/1078-0432.CCR-07-1147. [DOI] [PubMed] [Google Scholar]
- 24.Muscaritoli M, Bossola M, Aversa Z, Bellantone R, Rossi Fanelli F. Prevention and treatment of cancer cachexia: new insights into an old problem. Eur J Cancer. 2006;42(1):31–41. doi: 10.1016/j.ejca.2005.07.026. [DOI] [PubMed] [Google Scholar]
- 25.Prado CMM, Baracos VE, McCargar LJ, Mourtzakis M, Mulder KE, Reiman T, et al. Body composition as an independent determinant of 5-fluorouracil-based chemotherapy toxicity. Clin Cancer Res. 2007;13(11):3264–3268. doi: 10.1158/1078-0432.CCR-06-3067. [DOI] [PubMed] [Google Scholar]
- 26.Prado CMM, Baracos VE, McCargar LJ, Reiman T, Mourtzakis M, Tonkin K, et al. Sarcopenia as a determinant of chemotherapy toxicity and time to tumor progression in metastatic breast cancer patients receiving capecitabine treatment. Clin Cancer Res. 2009;15(8):2920–2926. doi: 10.1158/1078-0432.CCR-08-2242. [DOI] [PubMed] [Google Scholar]
- 27.Andreyev HJ, Norman AR, Oates J, Cunningham D. Why do patients with weight loss have a worse outcome when undergoing chemotherapy for gastrointestinal malignancies? Eur J Cancer. 1998;34(4):503–509. doi: 10.1016/S0959-8049(97)10090-9. [DOI] [PubMed] [Google Scholar]
- 28.Fearon KCH. Cancer cachexia: developing multimodal therapy for a multidimensional problem. Eur J Cancer. 2008;44(8):1124–1132. doi: 10.1016/j.ejca.2008.02.033. [DOI] [PubMed] [Google Scholar]
- 29.Lissoni P, Paolorossi F, Tancini G, Barni S, Ardizzoia A, Brivio F, et al. Is there a role for melatonin in the treatment of neoplastic cachexia? Eur J Cancer. 1996;32A(8):1340–1343. doi: 10.1016/0959-8049(96)00136-0. [DOI] [PubMed] [Google Scholar]
- 30.Goldberg RM, Loprinzi CL, Mailliard JA, O’Fallon JR, Krook JE, Ghosh C, et al. Pentoxifylline for treatment of cancer anorexia and cachexia? A randomized, double-blind, placebo-controlled trial. J Clin Oncol. 1995;13(11):2856–2859. doi: 10.1200/JCO.1995.13.11.2856. [DOI] [PubMed] [Google Scholar]
- 31.McClement S. Cancer anorexia–cachexia syndrome: psychological effect on the patient and family. J Wound Ostomy Continence Nurs. 2005;32(4):264–268. doi: 10.1097/00152192-200507000-00012. [DOI] [PubMed] [Google Scholar]
- 32.Illman J, Corringham R, Robinson D, Jr, Davis HM, Rossi J, Cella D, et al. Are inflammatory cytokines the common link between cancer-associated cachexia and depression? J Support Oncol. 2005;3(1):37–50. [PubMed] [Google Scholar]
- 33.Chochinov HM. Depression in cancer patients. Lancet Oncol. 2001;2(8):499–505. doi: 10.1016/S1470-2045(01)00456-9. [DOI] [PubMed] [Google Scholar]
- 34.Raison CL, Miller AH. Depression in cancer: new developments regarding diagnosis and treatment. Biol Psychiatry. 2003;54(3):283–294. doi: 10.1016/S0006-3223(03)00413-X. [DOI] [PubMed] [Google Scholar]
- 35.Strasser F, Binswanger J, Cerny T, Kesselring A. Fighting a losing battle: eating-related distress of men with advanced cancer and their female partners. A mixed-methods study. Palliat Med. 2007;21(2):129–137. doi: 10.1177/0269216307076346. [DOI] [PubMed] [Google Scholar]
- 36.Reid J, McKenna H, Fitzsimons D, McCance T. Fighting over food: patient and family understanding of cancer cachexia. Oncol Nurs Forum. 2009;36(4):439–445. doi: 10.1188/09.ONF.439-445. [DOI] [PubMed] [Google Scholar]
- 37.Reid J, McKenna H, Fitzsimons D, McCance T. The experience of cancer cachexia: a qualitative study of advanced cancer patients and their family members. Int J Nurs Stud. 2009;46(5):606–616. doi: 10.1016/j.ijnurstu.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 38.Hughes N, Neal RD. Adults with terminal illness: a literature review of their needs and wishes for food. J Adv Nurs. 2000;32(5):1101–1107. doi: 10.1046/j.1365-2648.2000.01580.x. [DOI] [PubMed] [Google Scholar]
- 39.Feuz A, Rapin C-H. An observational study of the role of pain control and food adaptation of elderly patients with terminal cancer. J Am Diet Assoc. 1994;94(7):767–770. doi: 10.1016/0002-8223(94)91945-3. [DOI] [PubMed] [Google Scholar]
- 40.Shragge JE, Wismer WV, Olson KL, Baracos VE. Shifting to conscious control: psychosocial and dietary management of anorexia by patients with advanced cancer. Palliat Med. 2007;21(3):227–233. doi: 10.1177/0269216307077172. [DOI] [PubMed] [Google Scholar]
- 41.McClement SE, Degner LF, Harlos M. Family responses to declining intake and weight loss in a terminally ill relative. Part 1: fighting back. J Palliat Care. 2004;20(2):93–100. [PubMed] [Google Scholar]
- 42.Evans WK, Makuch R, Clamon GH, Feld R, Weiner RS, Moran E, et al. Limited impact of total parenteral nutrition on nutritional status during treatment for small cell lung cancer. Cancer Res. 1985;45(7):3347–3353. [PubMed] [Google Scholar]
- 43.Loprinzi CL, Schaid DJ, Dose AM, Burnham NL, Jensen MD. Body-composition changes in patients who gain weight while receiving megestrol acetate. J Clin Oncol. 1993;11(1):152–154. doi: 10.1200/JCO.1993.11.1.152. [DOI] [PubMed] [Google Scholar]
- 44.Simons JPFHA, Schols AMWJ, Hoefnagels JMJ, Westerterp KR, ten Velde GPM, Wouters EFM. Effects of medroxyprogesterone acetate on food intake, body composition, and resting energy expenditure in patients with advanced, nonhormone-sensitive cancer: a randomized, placebo-controlled trial. Cancer. 1998;82(3):553–560. doi: 10.1002/(SICI)1097-0142(19980201)82:3<553::AID-CNCR18>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 45.Morley JE, Thomas DR, Wilson M-MG. Cachexia: pathophysiology and clinical relevance. Am J Clin Nutr. 2006;83(4):735–743. doi: 10.1093/ajcn/83.4.735. [DOI] [PubMed] [Google Scholar]
- 46.Evans WK, Nixon DW, Daly JM, Ellenberg SS, Gardner L, Wolfe E, et al. A randomized study of oral nutritional support versus ad lib nutritional intake during chemotherapy for advanced colorectal and non-small-cell lung cancer. J Clin Oncol. 1987;5(1):113–124. doi: 10.1200/JCO.1987.5.1.113. [DOI] [PubMed] [Google Scholar]
- 47.Ovesen L, Allingstrup L, Hannibal J, Mortensen EL, Hansen OP. Effect of dietary counseling on food intake, body weight, response rate, survival, and quality of life in cancer patients undergoing chemotherapy: a prospective, randomized study. J Clin Oncol. 1993;11(10):2043–2049. doi: 10.1200/JCO.1993.11.10.2043. [DOI] [PubMed] [Google Scholar]
- 48.Laviano A, Meguid MM, Rossi Fanelli F. Improving food intake in anorectic cancer patients. Curr Opin Clin Nutr Metab Care. 2003;6(4):421–426. doi: 10.1097/01.mco.0000078985.18774.4b. [DOI] [PubMed] [Google Scholar]
- 49.Pascual López A, Roqué i Figuls M, Urrútia Cuchi G, Berenstein EG, Almenar Pasies B, Balcells Alegre M, et al. Systematic review of megestrol acetate in the treatment of anorexia–cachexia syndrome. J Pain Symptom Manag. 2004;27(4):360–369. doi: 10.1016/j.jpainsymman.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 50.American College of Physicians. McGreer AJ, Detsky AS, O’Rourke K. Parenteral nutrition in patients receiving cancer chemotherapy. American College of Physicians. Ann Intern Med. 1989;110(9):734–736. doi: 10.7326/0003-4819-110-9-734. [DOI] [PubMed] [Google Scholar]
- 51.Kotler DP. Nutritional alterations associated with HIV infection. J Acquir Immune Defic Syndr. 2000;25(Suppl 1):S81–S87. doi: 10.1097/00042560-200010001-00013. [DOI] [PubMed] [Google Scholar]
- 52.Barber MD. Cancer cachexia and its treatment with fish-oil-enriched nutritional supplementation. Nutrition. 2001;17(9):751–755. doi: 10.1016/S0899-9007(01)00631-1. [DOI] [PubMed] [Google Scholar]
- 53.Bozzetti F, Gavazzi C, Mariani L, Crippa F. Artificial nutrition in cancer patients: which route, what composition? World J Surg. 1999;23(6):577–583. doi: 10.1007/PL00012350. [DOI] [PubMed] [Google Scholar]
- 54.Bruera E, Sweeney C. Cachexia and asthenia in cancer patients. Lancet Oncol. 2000;1(3):138–147. doi: 10.1016/S1470-2045(00)00033-4. [DOI] [PubMed] [Google Scholar]
- 55.Ravasco P, Monteiro-Grillo I, Vidal PM, Camilo ME. Dietary counseling improves patient outcomes: a prospective, randomized, controlled trial in colorectal cancer patients undergoing radiotherapy. J Clin Oncol. 2005;23(7):1431–1438. doi: 10.1200/JCO.2005.02.054. [DOI] [PubMed] [Google Scholar]
- 56.Muscaritoli M, Molfino A, Gioia G, Laviano A, Rossi Fanelli F. The parallel pathway: a novel nutritional and metabolic approach to cancer patients. Int Emerg Med. 2011;6(2):105–112. doi: 10.1007/s11739-010-0426-1. [DOI] [PubMed] [Google Scholar]
- 57.DeWys WD, Walters K. Abnormalities of taste sensation in cancer patients. Cancer. 1975;36(5):1888–1896. doi: 10.1002/1097-0142(197511)36:5<1888::AID-CNCR2820360546>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 58.Nielsen SS, Theologides A, Vickers ZM. Influence of food odors on food aversions and preferences in patients with cancer. Am J Clin Nutr. 1980;33(11):2253–2261. doi: 10.1093/ajcn/33.11.2253. [DOI] [PubMed] [Google Scholar]
- 59.Ripamonti C, Zecca E, Brunelli C, Fulfaro F, Villa S, Balzarini A, et al. A randomized, controlled clinical trial to evaluate the effects of zinc sulfate on cancer patients with taste alterations caused by head and neck irradiation. Cancer. 1998;82(10):1938–1945. doi: 10.1002/(SICI)1097-0142(19980515)82:10<1938::AID-CNCR18>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 60.Johnson FM. Alterations in taste sensation: a case presentation of a patient with end-stage pancreatic cancer. Canc Nurs. 2001;24(2):149–155. doi: 10.1097/00002820-200104000-00011. [DOI] [PubMed] [Google Scholar]
- 61.Ravasco P. Aspects of taste and compliance in patients with cancer. Eur J Oncol Nurs. 2005;9(Suppl 2):S84–S91. doi: 10.1016/j.ejon.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 62.Wickham RS, Rehwaldt M, Kefer C, Shott S, Abbas K, Glynn-Tucker E, et al. Taste changes experienced by patients receiving chemotherapy. Oncol Nurs Forum. 1999;26(4):697–706. [PubMed] [Google Scholar]
- 63.Sherry V. Taste alterations among patients with cancer. Clin J Oncol Nurs. 2002;6(2):1–5. doi: 10.1188/02.CJON.73-77. [DOI] [PubMed] [Google Scholar]
- 64.Wright AL, King JC, Baer MT, Citron LJ. Experimental zinc depletion and altered taste perception for NaCl in young adult males. Am J Clin Nutr. 1981;34(5):848–852. doi: 10.1093/ajcn/34.5.848. [DOI] [PubMed] [Google Scholar]
- 65.Silverman JE, Weber CW, Silverman S, Coulthard SL, Manning MR. Zinc supplementation and taste in head and neck cancer patients undergoing radiation therapy. J Oral Med. 1983;38(1):14–16. [PubMed] [Google Scholar]
- 66.Halyard MY, Jatoi A, Sloan JA, Bearden JD, III, Vora SA, Atherton PJ, et al. Does zinc sulfate prevent therapy-induced taste alterations in head and neck cancer patients? Results of phase III double-blind, placebo-controlled trial from the North Central Cancer Treatment Group (N01C4) Int J Radiat Oncol Biol Phys. 2007;67(5):1318–1322. doi: 10.1016/j.ijrobp.2006.10.046. [DOI] [PubMed] [Google Scholar]
- 67.Strasser F. The silent symptom early satiety: a forerunner of distinct phenotypes of anorexia/cachexia syndromes. Support Care Canc. 2006;14(7):689–692. doi: 10.1007/s00520-006-0061-6. [DOI] [PubMed] [Google Scholar]
- 68.Davis MP, Walsh D, Lagman R, Yavuzsen T. Early satiety in cancer patients: a common and important but underrecognized symptom. Support Care Canc. 2006;14(7):693–698. doi: 10.1007/s00520-005-0015-4. [DOI] [PubMed] [Google Scholar]
- 69.Dworzak F, Ferrari P, Gavazzi C, Maiorana C, Bozzetti F. Effects of cachexia due to cancer on whole body and skeletal muscle protein turnover. Cancer. 1998;82(1):42–48. doi: 10.1002/(SICI)1097-0142(19980101)82:1<42::AID-CNCR5>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 70.Tisdale MJ. Loss of skeletal muscle in cancer: biochemical mechanisms. Front Biosci. 2001;6:D164–D174. doi: 10.2741/Tisdale. [DOI] [PubMed] [Google Scholar]
- 71.Acharyya S, Ladner KJ, Nelsen LL, Damrauer J, Reiser PJ, Swoap S, et al. Cancer cachexia is regulated by selective targeting of skeletal muscle gene products. J Clin Invest. 2004;114(3):370–378. doi: 10.1172/JCI20174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jeevanandam M, Horowitz GD, Lowry SF, Brennan MF. Cancer cachexia and protein metabolism. Lancet. 1984;1(8392):1423–1426. doi: 10.1016/S0140-6736(84)91929-9. [DOI] [PubMed] [Google Scholar]
- 73.Fearon KC, Hansell DT, Preston T, Plumb JA, Davies J, Shapiro D, et al. Influence of whole body protein turnover rate on resting energy expenditure in patients with cancer. Cancer Res. 1988;48(9):2590–2595. [PubMed] [Google Scholar]
- 74.Rossi Fanelli F, Cangiano C, Muscaritoli M, Conversano L, Torelli GF, Cascino A. Tumor-induced changes in host metabolism: a possible marker of neoplastic disease. Nutrition. 1995;11(5 Suppl):595–600. [PubMed] [Google Scholar]
- 75.Holroyde CP, Gabuzda TG, Putnam RC, Paul P, Reichard GA. Altered glucose metabolism in metastatic carcinoma. Cancer Res. 1975;35(12):3710–3714. [PubMed] [Google Scholar]
- 76.Lieffers JR, Mourtzakis M, Hall KD, McCargar LJ, Prado CMM, Baracos VE. A viscerally driven cachexia syndrome in patients with advanced colorectal cancer: contributions of organ and tumor mass to whole-body energy demands. Am J Clin Nutr. 2009;89(4):1173–1179. doi: 10.3945/ajcn.2008.27273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.van Norren K, Kegler D, Argilés JM, Luiking Y, Gorselink M, Laviano A, et al. Dietary supplementation with a specific combination of high protein, leucine, and fish oil improves muscle function and daily activity in tumour-bearing cachectic mice. Br J Cancer. 2009;100(5):713–722. doi: 10.1038/sj.bjc.6604905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Knox LS, Crosby LO, Feurer ID, Buzby GP, Miller CL, Mullen JL. Energy expenditure in malnourished cancer patients. Ann Surg. 1983;197(2):152–162. doi: 10.1097/00000658-198302000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fredrix EW, Soeters PB, Wouters EF, Deerenberg IM, von Meyenfeldt MF, Saris WH. Effect of different tumor types on resting energy expenditure. Cancer Res. 1991;51(22):6138–6141. [PubMed] [Google Scholar]
- 80.Dempsey DT, Knox LS, Mullen JL, Miller C, Feurer ID, Buzby GP. Energy expenditure in malnourished patients with colorectal cancer. Arch Surg. 1986;121(7):789–795. doi: 10.1001/archsurg.1986.01400070055011. [DOI] [PubMed] [Google Scholar]
- 81.Gibney E, Elia M, Jebb S, Murgatroyd P, Jennings G. Total energy expenditure in patients with small-cell lung cancer: results of a validated study using the bicarbonate–urea method. Metabolism. 1997;46(12):1412–1417. doi: 10.1016/S0026-0495(97)90140-2. [DOI] [PubMed] [Google Scholar]
- 82.Falconer JS, Ross JA, Fearon KCH, Hawkins RA, O’Riordain MG, Carter DC. Effect of eicosapentaenoic acid and other fatty acids on the growth in vitro of human pancreatic cancer cell lines. Br J Cancer. 1994;69(5):826–832. doi: 10.1038/bjc.1994.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zylicz Z, Schwantje O, Wagener DJ, Folgering HT. Metabolic response to enteral food in different phases of cancer cachexia in rats. Oncology. 1990;47(1):87–91. doi: 10.1159/000226793. [DOI] [PubMed] [Google Scholar]
- 84.Cao D-X, Wu G-H, Zhang B, Quan Y-J, Wei J, Jin H, et al. Resting energy expenditure and body composition in patients with newly detected cancer. Clin Nutr. 2010;29(1):72–77. doi: 10.1016/j.clnu.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 85.Fearon KCH, Barber MD, Falconer JS, McMillan DC, Ross JA, Preston T. Pancreatic cancer as a model: inflammatory mediators, acute-phase response, and cancer cachexia. World J Surg. 1999;23(6):584–588. doi: 10.1007/PL00012351. [DOI] [PubMed] [Google Scholar]
- 86.Pepys MB, Hirschfield GM, Tennent GA, Gallimore JR, Kahan MC, Bellotti V, et al. Targeting C-reactive protein for the treatment of cardiovascular disease. Nature. 2006;440(7088):1217–1221. doi: 10.1038/nature04672. [DOI] [PubMed] [Google Scholar]
- 87.den Brekel AJ S-v, Dentener MA, Schols AM, Buurman WA, Wouters EF. Increased resting energy expenditure and weight loss are related to a systemic inflammatory response in lung cancer patients. J Clin Oncol. 1995;13(10):2600–2605. doi: 10.1200/JCO.1995.13.10.2600. [DOI] [PubMed] [Google Scholar]
- 88.Scott HR, McMillan DC, Crilly A, McArdle CS, Milroy R. The relationship between weight loss and interleukin 6 in non-small-cell lung cancer. Br J Cancer. 1996;73(12):1560–1562. doi: 10.1038/bjc.1996.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Blay JY, Negrier S, Combaret V, Attali S, Goillot E, Merrouche Y, et al. Serum level of interleukin 6 as a prognosis factor in metastatic renal cell carcinoma. Cancer Res. 1992;52(12):3317–3322. [PubMed] [Google Scholar]
- 90.Falconer JS, Fearon KC, Ross JA, Elton R, Wigmore SJ, Garden OJ, et al. Acute-phase protein response and survival duration of patients with pancreatic cancer. Cancer. 1995;75(8):2077–2082. doi: 10.1002/1097-0142(19950415)75:8<2077::AID-CNCR2820750808>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 91.O’Gorman P, McMillan D, McArdle C. Impact of weight loss, appetite, and the inflammatory response on quality of life in gastrointestinal cancer patients. Nutr Canc. 1998;32(2):76–80. doi: 10.1080/01635589809514722. [DOI] [PubMed] [Google Scholar]
- 92.Barber MD, Ross JA, Fearon KCH. Changes in nutritional, functional, and inflammatory markers in advanced pancreatic cancer. Nutr Canc. 1999;35(2):106–110. doi: 10.1207/S15327914NC352_2. [DOI] [PubMed] [Google Scholar]
- 93.Reeds PJ, Fjeld CR, Jahoor F. Do the differences between the amino acid compositions of acute-phase and muscle proteins have a bearing on nitrogen loss in traumatic states? J Nutr. 1994;124(6):906–910. doi: 10.1093/jn/124.6.906. [DOI] [PubMed] [Google Scholar]
- 94.Barber MD, Fearon KC, McMillan DC, Slater C, Ross JA, Preston T. Liver export protein synthetic rates are increased by oral meal feeding in weight-losing cancer patients. Am J Physiol Endocrinol Metab. 2000;279(3):E707–E714. doi: 10.1152/ajpendo.2000.279.3.E707. [DOI] [PubMed] [Google Scholar]
- 95.Argilés JM, Busquets S, Toledo M, López-Soriano FJ. The role of cytokines in cancer cachexia. Curr Opin Support Palliat Care. 2009;3(4):263–268. doi: 10.1097/SPC.0b013e3283311d09. [DOI] [PubMed] [Google Scholar]
- 96.MacDonald N, Easson AM, Mazurak VC, Dunn GP, Baracos VE. Understanding and managing cancer cachexia. J Am Coll Surg. 2003;197(1):143–161. doi: 10.1016/S1072-7515(03)00382-X. [DOI] [PubMed] [Google Scholar]
- 97.Ross JA, Fearon KCH. Eicosanoid-dependent cancer cachexia and wasting. Curr Opin Clin Nutr Metab Care. 2002;5(3):241–248. doi: 10.1097/00075197-200205000-00002. [DOI] [PubMed] [Google Scholar]
- 98.Tisdale MJ. The ‘cancer cachectic factor’. Support Care Canc. 2003;11(2):73–78. doi: 10.1007/s00520-002-0408-6. [DOI] [PubMed] [Google Scholar]
- 99.Baracos VE, Mazurak VC, Ma DWL. n-3 Polyunsaturated fatty acids throughout the cancer trajectory: influence on disease incidence, progression, response to therapy and cancer-associated cachexia. Nutr Res Rev. 2004;17(2):177–192. doi: 10.1079/NRR200488. [DOI] [PubMed] [Google Scholar]
- 100.Tisdale MJ. Biology of cachexia. J Natl Canc Inst. 1997;89(23):1763–1773. doi: 10.1093/jnci/89.23.1763. [DOI] [PubMed] [Google Scholar]
- 101.Barber MD, Fearon KCH, Tisdale MJ, McMillan DC, Ross JA. Effect of a fish oil-enriched nutritional supplement on metabolic mediators in patients with pancreatic cancer cachexia. Nutr Canc. 2001;40(2):118–124. doi: 10.1207/S15327914NC402_7. [DOI] [PubMed] [Google Scholar]
- 102.Socher SH, Martinez D, Craig JB, Kuhn JG, Oliff A. Tumor necrosis factor not detectable in patients with clinical cancer cachexia. J Natl Cancer Inst. 1988;80(8):595–598. doi: 10.1093/jnci/80.8.595. [DOI] [PubMed] [Google Scholar]
- 103.Todorov PT, Cariuk P, McDevitt TM, Coles B, Fearon KCH, Tisdale MJ. Characterization of a cancer cachectic factor. Nature. 1996; [DOI] [PubMed]
- 104.Todorov PT, Deacon M, Tisdale MJ. Structural analysis of a tumor-produced sulfated glycoprotein capable of initiating muscle protein degradation. J Biol Chem. 1997;272(19):12279–12288. doi: 10.1074/jbc.272.19.12279. [DOI] [PubMed] [Google Scholar]
- 105.Wigmore SJ, Todorov PT, Barber MD, Ross JA, Tisdale MJ, Fearon KCH. Characteristics of patients with pancreatic cancer expressing a novel cancer cachectic factor. Br J Surg. 2000;87(1):53–58. doi: 10.1046/j.1365-2168.2000.01317.x. [DOI] [PubMed] [Google Scholar]
- 106.Tisdale MJ. Molecular pathways leading to cancer cachexia. Physiology. 2005;20:340–348. doi: 10.1152/physiol.00019.2005. [DOI] [PubMed] [Google Scholar]
- 107.Lorite MJ. Activation of ATP-ubiquitin-dependent proteolysis in skeletal muscle in vivo and murine myoblasts in vitro by a proteolysis-inducing factor (PIF) Br J Cancer. 2001;85(2):297–302. doi: 10.1054/bjoc.2001.1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cariuk P, Lorite MJ, Todorov PT, Field WN, Wigmore SJ, Tisdale MJ. Induction of cachexia in mice by a product isolated from the urine of cachectic cancer patients. Br J Cancer. 1997;76(5):606–613. doi: 10.1038/bjc.1997.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Watchorn TM, Waddell I, Dowidar N, Ross JA. Proteolysis-inducing factor regulates hepatic gene expression via the transcription factors NF-(kappa)B and STAT3. FASEB J. 2001;15(3):562–564. doi: 10.1096/fj.00-0534fje. [DOI] [PubMed] [Google Scholar]
- 110.Baracos VE. Reply to letter to the editor: a response to the letter of M. Tisdale. Clin Cancer Res. 2008;14(7):2245–2245. doi: 10.1158/1078-0432.CCR-08-0021. [DOI] [PubMed] [Google Scholar]
- 111.Wieland BM, Stewart GD, Skipworth RJE, Sangster K, Fearon KCH, Ross JA, et al. Is there a human homologue to the murine proteolysis-inducing factor? Clin Cancer Res. 2007;13(17):4984–4992. doi: 10.1158/1078-0432.CCR-07-0946. [DOI] [PubMed] [Google Scholar]
- 112.Monitto CL, Dong SM, Jen J, Sidransky D. Characterization of a human homologue of proteolysis-inducing factor and its role in cancer cachexia. Clin Cancer Res. 2004;10(17):5862–5869. doi: 10.1158/1078-0432.CCR-04-0435. [DOI] [PubMed] [Google Scholar]
- 113.Tada T, Ohkubo I, Niwa M, Sasaki M, Tateyama H, Eimoto T. Immunohistochemical localization of Zn-alpha 2-glycoprotein in normal human tissues. J Histochem Cytochem. 1991;39(9):1221–1226. doi: 10.1177/39.9.1918940. [DOI] [PubMed] [Google Scholar]
- 114.Hale LP, Price DT, Sanchez LM, Demark-Wahnefried W, Madden JF. Zinc alpha-2-glycoprotein is expressed by malignant prostatic epithelium and may serve as a potential serum marker for prostate cancer. Clin Cancer Res. 2001;7(4):846–853. [PubMed] [Google Scholar]
- 115.Díez-Itza I, Sánchez LM, Allende MT, Vizoso F, Ruibal A, López-Otín C. Zn-alpha 2-glycoprotein levels in breast cancer cytosols and correlation with clinical, histological and biochemical parameters. Eur J Cancer. 1993;29A(9):1256–1260. doi: 10.1016/0959-8049(93)90068-Q. [DOI] [PubMed] [Google Scholar]
- 116.Rydén M, Agustsson T, Andersson J, Bolinder J, Toft E, Arner P. Adipose zinc-2-glycoprotein is a catabolic marker in cancer and noncancerous states. J Intern Med. 2012;271(4):414–420. doi: 10.1111/j.1365-2796.2011.02441.x. [DOI] [PubMed] [Google Scholar]
- 117.Islam-Ali BS, Tisdale MJ. Effect of a tumour-produced lipid-mobilizing factor on protein synthesis and degradation. Br J Cancer. 2001;84(12):1648–1655. doi: 10.1054/bjoc.2001.1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tisdale MJ. Mechanisms of cancer cachexia. Physiol Rev. 2009;89:381–410. [DOI] [PubMed]
- 119.Bandyopadhyay U, Das D, Banerjee RK. Reactive oxygen species: oxidative damage and pathogenesis. Curr Sci. 1999;77(5):658–666. [Google Scholar]
- 120.Arthur PG, Grounds MD, Shavlakadze T. Oxidative stress as a therapeutic target during muscle wasting: considering the complex interactions. Curr Opin Clin Nutr Metab Care. 2008;11(4):408–416. doi: 10.1097/MCO.0b013e328302f3fe. [DOI] [PubMed] [Google Scholar]
- 121.Barreiro E, de la Puente B, Busquets S, López-Soriano FJ, Gea J, Argilés JM. Both oxidative and nitrosative stress are associated with muscle wasting in tumour-bearing rats. FEBS Lett. 2005;579(7):1646–1652. doi: 10.1016/j.febslet.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 122.Russell ST, Eley H, Tisdale MJ. Role of reactive oxygen species in protein degradation in murine myotubes induced by proteolysis-inducing factor and angiotensin II. Cell Signal. 2007;19(8):1797–1806. doi: 10.1016/j.cellsig.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 123.Rubin H. Cancer cachexia: its correlations and causes. Proc Natl Acad Sci USA. 2003;100(9):5384–5389. doi: 10.1073/pnas.0931260100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Valko M, Leibfritz D, Moncol J, Cronin MTD, Mazur M, Telser J. Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol. 2007;39(1):44–84. doi: 10.1016/j.biocel.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 125.Sullivan-Gunn MJ, Campbell-O’Sullivan SP, Tisdale MJ, Lewandowski PA. Decreased NADPH oxidase expression and antioxidant activity in cachectic skeletal muscle. J Cachexia Sarcopenia Muscle. 2011;2(3):181–188. doi: 10.1007/s13539-011-0037-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Gauss KA, Nelson-Overton LK, Siemsen DW, Gao Y, DeLeo FR, Quinn MT. Role of NF-kappaB in transcriptional regulation of the phagocyte NADPH oxidase by tumor necrosis factor-alpha. J Leukoc Biol. 2007;82(3):729–741. doi: 10.1189/jlb.1206735. [DOI] [PubMed] [Google Scholar]
- 127.Groemping Y, Rittinger K. Activation and assembly of the NADPH oxidase: a structural perspective. Biochem J. 2005;386(Pt 3):401–416. doi: 10.1042/BJ20041835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Frey RS, Ushio Fukai M, Malik AB. NADPH oxidase-dependent signaling in endothelial cells: role in physiology and pathophysiology. Antioxidants & Redox Signal. 2009;11(4):791–810. doi: 10.1089/ars.2008.2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Meneshian A, Bulkley GB. The physiology of endothelial xanthine oxidase: from urate catabolism to reperfusion injury to inflammatory signal transduction. Microcirculation. 2002;9:161–175. doi: 10.1038/sj.mn.7800136. [DOI] [PubMed] [Google Scholar]
- 130.Kono H, Chen C-J, Ontiveros F, Rock KL. Uric acid promotes an acute inflammatory response to sterile cell death in mice. J Clin Invest. 2010;120(6):1939–1949. doi: 10.1172/JCI40124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Doehner W, Rauchhaus M, Florea VG, Sharma R, Bolger AP, Davos CH, et al. Uric acid in cachectic and noncachectic patients with chronic heart failure: relationship to leg vascular resistance. Am Hear J. 2001;141(5):792–799. doi: 10.1067/mhj.2001.114367. [DOI] [PubMed] [Google Scholar]
- 132.Pasupathi P, Ramachandran T, Sindhu P, Saravanan G, Bakthavathsalam G. Enhanced oxidative stress markers and antioxidant imbalance in HIV infection and AIDS patients. J Sci Res. 2009;1(2):370–380. doi: 10.3329/jsr.v1i2.2295. [DOI] [Google Scholar]
- 133.Smith JK, Carden DL, Korthuis RJ. Role of xanthine oxidase in postischemic microvascular injury in skeletal muscle. Am J Physiol. 1989;257(6 Pt 2):H1782–H1789. doi: 10.1152/ajpheart.1989.257.6.H1782. [DOI] [PubMed] [Google Scholar]
- 134.Kaynar H, Meral M, Turhan H, Keles M, Celik G, Akcay F. Glutathione peroxidase, glutathione-S-transferase, catalase, xanthine oxidase, Cu-Zn superoxide dismutase activities, total glutathione, nitric oxide, and malondialdehyde levels in erythrocytes of patients with small cell and non-small cell lung cancer. Cancer Lett. 2005;227(2):133–139. doi: 10.1016/j.canlet.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 135.Ryan MJ, Jackson JR, Hao Y, Leonard SS, Alway SE. Inhibition of xanthine oxidase reduces oxidative stress and improves skeletal muscle function in response to electrically stimulated isometric contractions in aged mice. Free Radic Biol Med. 2011;51(1):38–52. doi: 10.1016/j.freeradbiomed.2011.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hellsten Y, Frandsen U, Orthenblad N, Sjödin B, Richter EA. Xanthine oxidase in human skeletal muscle following eccentric exercise: a role in inflammation. J Physiol. 1997;498(Pt 1):239–248. doi: 10.1113/jphysiol.1997.sp021855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Mantovani G, Maccio A, Madeddu C, Mura L, Gramignano G, Lusso MR, et al. Antioxidant agents are effective in inducing lymphocyte progression through cell cycle in advanced cancer patients: assessment of the most important laboratory indexes of cachexia and oxidative stress. J Mol Med. 2003;81(10):664–673. doi: 10.1007/s00109-003-0476-1. [DOI] [PubMed] [Google Scholar]
- 138.Williams A, Sun X, Fischer JE, Hasselgren PO. The expression of genes in the ubiquitin–proteasome proteolytic pathway is increased in skeletal muscle from patients with cancer. Surgery. 1999;126(4):744–749. doi: 10.1016/S0039-6060(99)70131-5. [DOI] [PubMed] [Google Scholar]
- 139.Costelli P, Tullio RD, Baccino FM, Melloni E. Activation of Ca(2+)-dependent proteolysis in skeletal muscle and heart in cancer cachexia. Br J Cancer. 2001;84(7):946–950. doi: 10.1054/bjoc.2001.1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Costelli P, Bossola M, Muscaritoli M, Grieco G. Anticytokine treatment prevents the increase in the activity of ATP-ubiquitin-and Ca2 + -dependent proteolytic systems in the muscle of tumour-bearing rats. Cytokine. 2002;19(1):1–5. doi: 10.1006/cyto.2002.1036. [DOI] [PubMed] [Google Scholar]
- 141.Langhans W. Peripheral mechanisms involved with catabolism. Curr Opin Clin Nutr Metab Care. 2002;5(4):419–426. doi: 10.1097/00075197-200207000-00011. [DOI] [PubMed] [Google Scholar]
- 142.Costelli P, Baccino FM. Mechanisms of skeletal muscle depletion in wasting syndromes: role of ATP-ubiquitin-dependent proteolysis. Curr Opin Clin Nutr Metab Care. 2003;6(4):407–412. doi: 10.1097/01.mco.0000078984.18774.02. [DOI] [PubMed] [Google Scholar]
- 143.Cohen S, Brault JJ, Gygi SP, Glass DJ, Valenzuela DM, Gartner C, et al. During muscle atrophy, thick, but not thin, filament components are degraded by MuRF1-dependent ubiquitylation. J Cell Biol. 2009;185(6):1083–1095. doi: 10.1083/jcb.200901052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Cosper PF, Leinwand LA. Myosin heavy chain is not selectively decreased in murine cancer cachexia. Int J Cancer. 2011;130(11):2722–2727. doi: 10.1002/ijc.26298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Rolland Y, Lauwers-Cances V, Cesari M, Vellas B, Pahor M, Grandjean H. Physical performance measures as predictors of mortality in a cohort of community-dwelling older French women. Eur J Epidemiol. 2006;21(2):113–122. doi: 10.1007/s10654-005-5458-x. [DOI] [PubMed] [Google Scholar]
- 146.Gale CR, Martyn CN, Cooper C, Sayer AA. Grip strength, body composition, and mortality. Int J Epidemiol. 2007;36(1):228–235. doi: 10.1093/ije/dyl224. [DOI] [PubMed] [Google Scholar]
- 147.Evans WJ, Lambert CP. Physiological basis of fatigue. Am J Phys Med Rehabil. 2007;86(1 Suppl):S29–S46. doi: 10.1097/PHM.0b013e31802ba53c. [DOI] [PubMed] [Google Scholar]
- 148.Cella D, Lai J-S, Chang C-H, Peterman A, Slavin M. Fatigue in cancer patients compared with fatigue in the general United States population. Cancer. 2002;94(2):528–538. doi: 10.1002/cncr.10245. [DOI] [PubMed] [Google Scholar]
- 149.Anker SD, Swan JW, Volterrani M, Chua TP, Clark AL, Poole-Wilson PA, et al. The influence of muscle mass, strength, fatigability and blood flow on exercise capacity in cachectic and non-cachectic patients with chronic heart failure. Eur Heart J. 1997;18(2):259–269. doi: 10.1093/oxfordjournals.eurheartj.a015229. [DOI] [PubMed] [Google Scholar]
- 150.Tan BHL, Birdsell LA, Martin L, Baracos VE, Fearon KCH. Sarcopenia in an overweight or obese patient is an adverse prognostic factor in pancreatic cancer. Clin Cancer Res. 2009;15(22):6973–6979. doi: 10.1158/1078-0432.CCR-09-1525. [DOI] [PubMed] [Google Scholar]
- 151.Bossola M, Muscaritoli M, Costelli P, Grieco G, Bonelli G, Pacelli F, et al. Increased muscle proteasome activity correlates with disease severity in gastric cancer patients. Ann Surg. 2003;237(3):384–389. doi: 10.1097/01.SLA.0000055225.96357.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Khal J, Wyke SM, Russell ST, Hine AV, Tisdale MJ. Expression of the ubiquitin–proteasome pathway and muscle loss in experimental cancer cachexia. Br J Cancer. 2005;93(7):774–780. doi: 10.1038/sj.bjc.6602780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Khal J, Hine AV, Fearon KCH, Dejong CHC, Tisdale MJ. Increased expression of proteasome subunits in skeletal muscle of cancer patients with weight loss. Int J Biochem Cell Biol. 2005;37(10):2196–2206. doi: 10.1016/j.biocel.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 154.Wyke SM, Tisdale MJ. NF-kappaB mediates proteolysis-inducing factor induced protein degradation and expression of the ubiquitin–proteasome system in skeletal muscle. Br J Cancer. 2005;92(4):711–721. doi: 10.1038/sj.bjc.6602402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Bossola M, Muscaritoli M, Costelli P, Bellantone R, Pacelli F, Busquets S, et al. Increased muscle ubiquitin mRNA levels in gastric cancer patients. Am J Physiol Reg I. 2001;280(5):R1518–R1523. doi: 10.1152/ajpregu.2001.280.5.R1518. [DOI] [PubMed] [Google Scholar]
- 156.Glickman MH, Ciechanover A. The ubiquitin–proteasome proteolytic pathway: destruction for the sake of construction. Physiol Rev. 2002;82(2):373–428. doi: 10.1152/physrev.00027.2001. [DOI] [PubMed] [Google Scholar]
- 157.Solomon V, Baracos V, Sarraf P, Goldberg AL. Rates of ubiquitin conjugation increase when muscles atrophy, largely through activation of the N-end rule pathway. Proc Natl Acad Sci USA. 1998;95(21):12602–12607. doi: 10.1073/pnas.95.21.12602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Bodine SC, Latres E, Baumhueter S, Lai VK, Nunez L, Clarke BA, et al. Identification of ubiquitin ligases required for skeletal muscle atrophy. Science. 2001;294(5547):1704–1708. doi: 10.1126/science.1065874. [DOI] [PubMed] [Google Scholar]
- 159.Lecker SH, Jagoe RT, Gilbert A, Gomes M, Baracos V, Bailey J, et al. Multiple types of skeletal muscle atrophy involve a common program of changes in gene expression. FASEB J. 2004;18(1):39–51. doi: 10.1096/fj.03-0610com. [DOI] [PubMed] [Google Scholar]
- 160.Muscaritoli M, Bossola M, Doglietto GB, Fanelli FR, et al. The ubiquitin/proteasome system in cancer cachexia. In: Mantovani G, Anker SD, et al., editors. Cachexia and wasting: a modern approach. Italy: Springer; 2006. [Google Scholar]
- 161.de Palma L, Marinelli M, Pavan M, Orazi A. Ubiquitin ligases MuRF1 and MAFbx in human skeletal muscle atrophy. Joint Bone Spine. 2007;75(1):53–57. doi: 10.1016/j.jbspin.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 162.Fischer D. The gene expression of ubiquitin ligase E3α is upregulated in skeletal muscle during sepsis in rats—potential role of glucocorticoids. Biochem Biophys Res Commun. 2000;267(2):504–508. doi: 10.1006/bbrc.1999.1987. [DOI] [PubMed] [Google Scholar]
- 163.Jatoi A, Alberts SR, Foster N, Morton R, Burch P, Block M, et al. Is bortezomib, a proteasome inhibitor, effective in treating cancer-associated weight loss? Preliminary results from the North Central Cancer Treatment Group. Support Care Canc. 2005;13(6):381–386. doi: 10.1007/s00520-005-0787-6. [DOI] [PubMed] [Google Scholar]
- 164.Wiedenmann B, Malfertheiner P, Friess H, Ritch P, Arseneau J, Mantovani G, et al. A multicenter, phase II study of infliximab plus gemcitabine in pancreatic cancer cachexia. J Support Oncol. 2008;6(1):18–25. [PubMed] [Google Scholar]
- 165.Jatoi A, Ritter HL, Dueck A, Nguyen PL, Nikcevich DA, Luyun RF, et al. A placebo-controlled, double-blind trial of infliximab for cancer-associated weight loss in elderly and/or poor performance non-small cell lung cancer patients (N01C9) Lung Cancer. 2010;68(2):234–239. doi: 10.1016/j.lungcan.2009.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Smith IJ, Aversa Z, Hasselgren P, Pacelli F, Rosa F, Doglietto GB, et al. Calpain activity is increased in skeletal muscle from gastric cancer patients with no or minimal weight loss. Muscle Nerve. 2011;43(3):410–414. doi: 10.1002/mus.21893. [DOI] [PubMed] [Google Scholar]
- 167.Jagoe RT, Redfern CP, Roberts RG, Gibson GJ, Goodship TH. Skeletal muscle mRNA levels for cathepsin B, but not components of the ubiquitin–proteasome pathway, are increased in patients with lung cancer referred for thoracotomy. Clin Sci. 2002;102(3):353–361. doi: 10.1042/CS20010270. [DOI] [PubMed] [Google Scholar]
- 168.Op den Kamp CM, Langen RC, Minnaard R, Kelders MC, den CM OdK, et al. Pre-cachexia in patients with stages IIII non-small cell lung cancer: systemic inflammation and functional impairment without activation of skeletal muscle ubiquitin proteasome system. Lung Cancer. 2012;76(1):112–117. doi: 10.1016/j.lungcan.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 169.Paul PK, Gupta SK, Bhatnagar S, Panguluri SK, Darnay BG, Choi Y, et al. Targeted ablation of TRAF6 inhibits skeletal muscle wasting in mice. J Cell Biol. 2010;191(7):1395–1411. doi: 10.1083/jcb.201006098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Sandri SM. Autophagy in skeletal muscle. FEBS Lett. 2010;584(7):1411–1416. doi: 10.1016/j.febslet.2010.01.056. [DOI] [PubMed] [Google Scholar]
- 171.Muscaritoli M, Bossola M, Bellantone R, Fanelli FR. Therapy of muscle wasting in cancer: what is the future? Curr Opin Clin Nutr Metab Care. 2004;7(4):459–466. doi: 10.1097/01.mco.0000134366.07148.2e. [DOI] [PubMed] [Google Scholar]
- 172.Sacheck JM, Ohtsuka A, McLary SC, Goldberg AL. IGF-I stimulates muscle growth by suppressing protein breakdown and expression of atrophy-related ubiquitin ligases, atrogin-1 and MuRF1. Am J Physiol Endocrinol Metab. 2004;287(4):E591–E601. doi: 10.1152/ajpendo.00073.2004. [DOI] [PubMed] [Google Scholar]
- 173.McMillan DC, O’Gorman P, Fearon KCH, McArdle CS. A pilot study of megestrol acetate and ibuprofen in the treatment of cachexia in gastrointestinal cancer patients. Br J Cancer. 1997;76(6):788–790. doi: 10.1038/bjc.1997.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Preston T, Fearon KC, McMillan DC, Winstanley FP, Slater C, Shenkin A, et al. Effect of ibuprofen on the acute-phase response and protein metabolism in patients with cancer and weight loss. Br J Surg. 1995;82(2):229–234. doi: 10.1002/bjs.1800820233. [DOI] [PubMed] [Google Scholar]
- 175.McMillan DC, Wigmore SJ, Fearon KCH, O’Gorman P, Wright CE, McArdle CS. A prospective randomized study of megestrol acetate and ibuprofen in gastrointestinal cancer patients with weight loss. Br J Cancer. 1999;79(3–4):495–500. doi: 10.1038/sj.bjc.6690077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Lundholm K, Gelin J, Hyltander A, Lönnroth C, Sandström R, Svaninger G, et al. Anti-inflammatory treatment may prolong survival in undernourished patients with metastatic solid tumors. Cancer Res. 1994;54(21):5602–5606. [PubMed] [Google Scholar]
- 177.Wigmore SJ, Falconer JS, Plester CE, Ross JA, Maingay JP, Carter DC, et al. Ibuprofen reduces energy expenditure and acute-phase protein production compared with placebo in pancreatic cancer patients. Br J Cancer. 1995;72(1):185–188. doi: 10.1038/bjc.1995.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Mantovani G, Madeddu C. Cyclooxygenase-2 inhibitors and antioxidants in the treatment of cachexia. Curr Opin Support Palliat Care. 2008;2(4):275–281. doi: 10.1097/SPC.0b013e32830f47e4. [DOI] [PubMed] [Google Scholar]
- 179.Mantovani G, Maccio A, Madeddu C, Gramignano G, Lusso MR, Serpe R, et al. A phase II study with antioxidants, both in the diet and supplemented, pharmaconutritional support, progestagen, and anti-cyclooxygenase-2 showing efficacy and safety in patients with cancer-related anorexia/cachexia and oxidative stress. Canc Epidemiol Biomarkers Prev. 2006;15(5):1030–1034. doi: 10.1158/1055-9965.EPI-05-0538. [DOI] [PubMed] [Google Scholar]
- 180.Mantovani G, Maccio A, Madeddu C, Serpe R, Massa E, Dessi M, et al. Randomized phase III clinical trial of five different arms of treatment in 332 patients with cancer cachexia. Oncologist. 2010;15(2):200–211. doi: 10.1634/theoncologist.2009-0153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Maggiore RJ, Gross CP, Hurria A. Polypharmacy in older adults with cancer. Oncologist. 2010;15(5):507–522. doi: 10.1634/theoncologist.2009-0290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Madeddu C, Dessì M, Panzone F, Serpe R, Antoni G, Cau MC, et al. Randomized phase III clinical trial of a combined treatment with carnitine + celecoxibmegestrol acetate for patients with cancer-related anorexia/cachexia syndrome. Clin Nutr. 2012;31(2):176–182. doi: 10.1016/j.clnu.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 183.Burns CP, Halabi S, Clamon GH, Hars V, Wagner BA, Hohl RJ, et al. Phase I clinical study of fish oil fatty acid capsules for patients with cancer cachexia: cancer and leukemia group B study 9473. Clin Cancer Res. 1999;5(12):3942–3947. [PubMed] [Google Scholar]
- 184.Barber MD, Fearon KC. Tolerance and incorporation of a high-dose eicosapentaenoic acid diester emulsion by patients with pancreatic cancer cachexia. Lipids. 2001;36(4):347–351. doi: 10.1007/s11745-001-0726-4. [DOI] [PubMed] [Google Scholar]
- 185.Murphy RA, Mourtzakis M, Chu QSC, Baracos VE, Reiman T, Mazurak VC. Supplementation with fish oil increases first-line chemotherapy efficacy in patients with advanced nonsmall cell lung cancer. Cancer. 2011;117(16):3774–3780. doi: 10.1002/cncr.25933. [DOI] [PubMed] [Google Scholar]
- 186.Wigmore SJ, Ross JA, Falconer JS, Plester CE, Tisdale MJ, Carter DC, et al. The effect of polyunsaturated fatty acids on the progress of cachexia in patients with pancreatic cancer. Nutrition. 1996;12(1 Suppl):S27–S30. doi: 10.1016/0899-9007(96)90014-3. [DOI] [PubMed] [Google Scholar]
- 187.Wigmore SJ, Fearon KCH, Maingay JP, Ross JA. Down-regulation of the acute-phase response in patients with pancreatic cancer cachexia receiving oral eicosapentaenoic acid is mediated via suppression of interleukin-6. Clin Sci. 1997;92(2):215–221. doi: 10.1042/cs0920215. [DOI] [PubMed] [Google Scholar]
- 188.Donohoe CL, Ryan AM, Reynolds JV. Cancer cachexia: mechanisms and clinical implications. Gastroenterol Res Pract. 2011;2011:1–13. doi: 10.1155/2011/601434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Smith HJ, Tisdale MJ. Induction of apoptosis by a cachectic-factor in murine myotubes and inhibition by eicosapentaenoic acid. Apoptosis. 2003;8(2):161–169. doi: 10.1023/A:1022970609579. [DOI] [PubMed] [Google Scholar]
- 190.Whitehouse AS, Tisdale MJ. Increased expression of the ubiquitin–proteasome pathway in murine myotubes by proteolysis-inducing factor (PIF) is associated with activation of the transcription factor NF-kappaB. Br J Cancer. 2003;89(6):1116–1122. doi: 10.1038/sj.bjc.6601132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Bhoj VG, Chen ZJ. Ubiquitylation in innate and adaptive immunity. Nature. 2009;458(7237):430–437. doi: 10.1038/nature07959. [DOI] [PubMed] [Google Scholar]
- 192.Whitehouse AS, Smith HJ, Drake JL, Tisdale MJ. Mechanism of attenuation of skeletal muscle protein catabolism in cancer cachexia by eicosapentaenoic acid. Cancer Res. 2001;61(9):3604–3609. [PubMed] [Google Scholar]
- 193.Wigmore SJ, Barber MD, Ross JA, Tisdale MJ, Fearon KCH. Effect of oral eicosapentaenoic acid on weight loss in patients with pancreatic cancer. Nutr Canc. 2000;36(2):177–184. doi: 10.1207/S15327914NC3602_6. [DOI] [PubMed] [Google Scholar]
- 194.Jatoi A, Rowland K, Loprinzi CL, Sloan JA, Dakhll SR, MacDonald N, et al. An eicosapentaenoic acid supplement versus megestrol acetate versus both for patients with cancer-associated wasting: a North Central Cancer Treatment Group and National Cancer Institute of Canada collaborative effort. J Clin Oncol. 2004;22(12):2469–2476. doi: 10.1200/JCO.2004.06.024. [DOI] [PubMed] [Google Scholar]
- 195.Li M, Zhu Q, Hu C, Giesy JP, Kong Z, Cui Y. Protective effects of eicosapentaenoic acid on genotoxicity and oxidative stress of cyclophosphamide in mice. Environ Toxicol. 2011;26(3):217–223. doi: 10.1002/tox.20546. [DOI] [PubMed] [Google Scholar]
- 196.Russell ST, Tisdale MJ. The role of glucocorticoids in the induction of zinc-alpha2-glycoprotein expression in adipose tissue in cancer cachexia. Br J Cancer. 2005;92(5):876–881. doi: 10.1038/sj.bjc.6602404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Barber MD, McMillan DC, Preston T, Ross JA, Fearon KCH. Metabolic response to feeding in weight-losing pancreatic cancer patients and its modulation by a fish-oil-enriched nutritional supplement. Clin Sci. 2000;98(4):389–399. doi: 10.1042/CS19990273. [DOI] [PubMed] [Google Scholar]
- 198.Barber MD, Ross JA, Preston T, Shenkin A, Fearon KCH. Fish oil-enriched nutritional supplement attenuates progression of the acute-phase response in weight-losing patients with advanced pancreatic cancer. J Nutr. 1999;129(6):1120–1125. doi: 10.1093/jn/129.6.1120. [DOI] [PubMed] [Google Scholar]
- 199.Laviano A, Muscaritoli M, Rossi Fanelli F. Phase II study of high-dose fish oil capsules for patients with cancer-related cachexia: a Cancer and Leukemia Group B study. Cancer. 2005;103(3):651–652. doi: 10.1002/cncr.20817. [DOI] [PubMed] [Google Scholar]
- 200.Tiryaki-Sönmez G, Schoenfeld B, Vatansever-Ozen S. Omega-3 fatty acids and exercise: a review of their combined effects on body composition and physical performance. Biomed Hum Kinet. 2011;3(3):23–29. [Google Scholar]
- 201.Penna F, Busquets S, Pin F, Toledo M, Baccino FM, López-Soriano FJ, et al. Combined approach to counteract experimental cancer cachexia: eicosapentaenoic acid and training exercise. J Cachexia Sarcopenia Muscle. 2011;2(2):95–104. doi: 10.1007/s13539-011-0028-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Pacher P, Nivorozhkin A, Szabó C. Therapeutic effects of xanthine oxidase inhibitors: renaissance half a century after the discovery of allopurinol. Pharmacol Rev. 2006;58(1):87–114. doi: 10.1124/pr.58.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Springer J, Hartmann A, Palus S, Adams V, von Harsdorf R, Anker SD, et al. The xanthine oxidase inhibitors oxypurinol and allopurinol reduce wasting and improve cardiac function in experimental cancer cachexia. J Card Fail. 2009;15(6):S22–S22. doi: 10.1016/j.cardfail.2009.06.381. [DOI] [Google Scholar]
- 204.Day RO, Graham GG, Hicks M, McLachlan AJ, Stocker SL, Williams KM. Clinical pharmacokinetics and pharmacodynamics of allopurinol and oxypurinol. Clin Pharmacokinet. 2007;46(8):623–644. doi: 10.2165/00003088-200746080-00001. [DOI] [PubMed] [Google Scholar]
- 205.Deby C, Deby-Dupont G, Noël FX, Lavergne L. In vitro and in vivo arachidonic acid conversions into biologically active derivatives are enhanced by uric acid. Biochem Pharmacol. 1981;30(16):2243–2249. doi: 10.1016/0006-2952(81)90094-0. [DOI] [PubMed] [Google Scholar]
- 206.von Haehling S, Morley JE, Coats AJ, Anker SD. Ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle. J Cachexia Sarcopenia Muscle. 2010;1:7–8. [DOI] [PMC free article] [PubMed]