Abstract
One of the mechanisms supposed to explain the increasing prevalence of asthma, among children in particular, is the use of antibiotics because they may modify natural microbial exposure and development of the immune system in early childhood. The aim of this study is to investigate the association between the use of various classes of antibiotics (penicillin, cephalosporin and macrolide derivatives) in early childhood and the medical diagnosis of asthma or wheezing reported by mothers over the follow-up after adjustment for potential confounders and respiratory infections. In a population-based sample of 5-year-olds, a part of the ongoing birth cohort study, the standardized interviews on health outcomes, potential confounders (child’s gender, maternal atopy, parity, prenatal and postnatal environmental tobacco smoke) and the use of antibiotics were gathered from mothers of 310 children. While the overall use of antibiotics during the early childhood was insignificantly associated with asthma (adjusted OR = 1.65, 95%CI: 0.93 – 2.93), the risk estimates were significant both for macrolide antibiotics (adjusted OR=2.14, 95%CI: 1.16–3.95) and cephalosporins (OR=1.98, 95%CI: 1.14–3.37). The significant excess in IRR (incident risk ratio) of wheezing episodes was related only to the use of macrolide antibiotics (adjusted IRR=1.91, 95%CI: 1.12–3.27). The use of other classes of antibiotics was found not to be associated with the medical diagnosis of asthma or wheezing episodes recorded in the study period. Conclusion: as early childhood use of broad spectrum antibiotics is associated with an increased risk of developing asthma in 5-year-olds, it may be hypothesized that the antibiotic- related suppression of allergic inflammatory responses in the course of treatment may later lead to greater than before atopic immune response in Th2 children or an impairment of Th1 immune responses in early childhood.
Keywords: antibiotics, asthma, childhood, wheezing, Th1 immune responses, allergic reactions
INTRODUCTION
There is a good body of epidemiologic evidence that the prevalence of asthma and allergic diseases has significantly increased worldwide over the last three decades, particularly in children and young adults, making allergic diseases a very common chronic health problem in childhood (1-6). One of the hypotheses trying to explain the increasing trend of asthma over time is often linked with the effects of the “western lifestyle” i.e., reduced microbial exposure, increased immunization, improved sanitary conditions and smaller family size (7-12). The hygiene context of this hypothesis is associated with the decreasing prevalence and severity of childhood infections, which are assumed to exert a protective effect for the development of allergic diseases. In fact, many findings have suggested that the protective effect of natural infections may be due to their influence on the development of the immune system in early life (13-16).
Another additional reason for the asthma epidemic worldwide may be related to the exposure of children to antibiotics. The wide use of antibiotics in children for treatment of respiratory infections and other diseases of bacterial etiology is supposed to modify natural microbial exposure and the development of the immune system in early childhood (17-23). In fact, several recent studies showed a significant positive association between the use of antibiotics in early life and the subsequent development of atopic disorders such as asthma and wheeze (24-26). On the other hand, the use of antibiotics also may be a consequence of an increased occurrence of respiratory infections in children with an asthmatic or allergic constitution. It is this reverse causation that makes the interpretation of many epidemiologic studies extremely difficult and many studies failed to adjust successfully the risk estimates of given allergic health outcomes for chest infections.
In the present study, we used a population based sample of 5 year-olds who were part of an ongoing birth cohort study in Cracow. The main goal of the study was to investigate the relationship between different classes of antibiotic treatment in early childhood and the medical diagnosis of asthma or wheezing reported by mothers. The primary hypothesis was that broad spectrum antibiotics compared to narrow spectrum may increase the risk for asthma in early childhood. Bearing in mind a possible reverse causation between antibiotic use and the health outcomes in question, the risk estimates were adjusted for respiratory episodes experienced by children in the follow-up period.
MATERIAL AND METHODS
The study sample is a part of the ongoing prospective cohort study described elsewhere (27). Briefly, a group of 505 women attending ambulatory prenatal clinics in the first and second trimesters of pregnancy were recruited in Cracow inner city area from January 2001 to February 2004. The study eligibility criteria included only non-smoking women with singleton pregnancies aged 18-35, and free from chronic diseases such as diabetes and hypertension. Upon enrollment, a detailed questionnaire was administered to each subject to elicit information on demographic data, house characteristics, date of the last menstrual period (LMP), medical and reproductive history, occupational hazards, alcohol consumption, nutritional habits, and smoking practices of others present in the home.
After delivery, every three months in the first 24 months of the newborn’s life and every 6 months later, a detailed standardized face-to-face interview on the infant’s health was administered to each mother by a trained interviewer. All interviews have been performed with the mothers and information on medical diagnosis of asthma and the occurrence of various respiratory infections diagnosed by physician and presence of wheezing or whistling in the chest irrespective of respiratory infection was recorded in each study period. The overall number of respiratory infections and wheezing episodes recorded indicated the severity of the health outcome in question. In the fourth and fifth year of the follow-up the information on the use of antibiotics in each 6 month study period was collected as well. Antibiotic use was defined as positive response to the question, “ Has your child in the last 6 months taken antibiotics?” If yes, detailed information about the number of oral doses and duration of antibiotic therapy with various classes of antibiotics prescribed by physican was obtained from mothers. If the mother was unable to give the specific name of the antibiotic used (N=49), only the number of doses was recorded. Maternal atopy was defined as self-reported medical diagnosis of asthma, eczema or hay fever. Prenatal and postnatal environmental tobacco smoke (ETS) was defined by the presence of at least one cigarette smokers in the household.
Out of 505 babies initially recruited to the Krakow birth cohort study, only 310 term-born children completed the 5-year follow-up. The final analysis did not include 49 children for whom mothers were unable to specify the name of the antibiotics. The study was approved by the Bioethical Committee of the Jagiellonian University in Krakow. A written informed consent was obtained from the parents of all participating children.
Statistical methods
The main purpose of the statistical analysis was to assess the association between the postnatal exposure to various classes of antibiotics and the medical diagnosis of asthma in 5-year-olds or the incidence of wheezing episodes monitored over the follow-up. Initially, univariate cross sectional associations between the antibiotics use and health outcomes recorded between 4 and 5 years of age was performed. Subsequently, multivariate logistic regression models were run adjusting for a set of a priori chosen potential confounders (child’s gender, maternal atopy, parity, prenatal and postnatal ETS) and the effect of the number of respiratory infections. For the analysis of the association between the number of wheezing episodes and the use of medication under study, the Poisson multivariable regression model with robust standard error estimates was used. Statistical evaluation of an excess of wheezing episodes associated with the use of antibiotics was evaluated by incidence rate ratio (IRR). In the statistical analysis, each class of antibiotics was divided into three levels based on the respective use at 4 and 5 years of age: 0 – none, 1 – low intake (below or equal the median), 2 – high level (above the median) of their respective use at 4 and 5 years of age. In each regression model children who did not use antibiotics acted as a referential category. The statistical analysis on the health outcomes related to specific antibiotic categories was carried out only in the group of children for whom mothers reported the exact name of antibiotics used. All tests with two-sided, P-values <0.05 were considered to be statistically significant, as were odds ratios with 95% confidence intervals excluding the value 1 (28). Statistical analyses were performed using STATA 11.1 for Windows (STATA Inc. USA).
RESULTS
In the follow-up group we found 29 (9.3%) children with the medical diagnosis of asthma as reported by mothers. The incidence of asthma was higher in boys (11.8%, 95%CI: 7.1–17.9) than in girls (7.0%, 95%CI: 3.5–12.2). The general characteristics of the children grouped by asthma did not differ across the groups (Table 1); however, the asthmatic children reported much higher frequency of episodes of various respiratory infections (Table 2).
Table 1.
Characteristics of the children who completed follow-up and provided information on the use of antibiotics at 4 and 5 years of age, grouped by asthma.
| Medical diagnosis of asthma | Total N=310 |
Difference (p–level) |
||
|---|---|---|---|---|
| No (n=281) | Yes (n=29) | |||
| Maternal age: mean SD |
27.86 3.415 |
27.41 3.670 |
27.82 3.436 |
0.5087 |
| Maternal education: elementary n (%) secondary n (%) higher n (%) |
23( 8.2) 68(24.2) 190(67.6) |
3(10.3) 7(24.1) 19(65.5) |
26( 8.4) 75(24.2) 209(67.4) |
0.9215 |
| Maternal atopy (+): n(%) | 64(22.8) | 9(31.0) | 73(23.5) | 0.3183 |
| Child’s gender: Boys n(%) Girls n(%) |
135(48.0) 146(52.0) |
18(62.1) 11(37.9) |
153 (49.4) 157(50.6) |
0.2137 |
| Gestational age: mean (weeks) >36 S.D. |
39.47 1.128 |
39.90 1.319 |
39.51 1.151 |
0.0593 |
| Birth weight (g): mean S.D. |
3420.7 432.4 |
3570.0 464.4 |
3434.7 436.9 |
0.0798 |
| Length at birth (cm): mean S.D. |
54.78 2.579 |
55.28 2.827 |
54.83 2.602 |
0.3288 |
| Prenatal ETS (+) n(%) | 67(23.8) | 4(13.8) | 71(22.9) | 0.3201 |
| Postnatal (4-5yr) ETS (+) n(%) | 47(16.7) | 5(17.2) | 52(16.8) | 1.0000 |
Table 2.
The occurrence of various respiratory diseases and wheezing symptoms (number of episodes) at age 4-5 years grouped by asthma diagnosis.
| Medical diagnosis of asthma | Total N=310 |
Difference (p – level) |
||
|---|---|---|---|---|
| No (n=281) | Yes (n=29) | |||
| Sinusitis episodes (4-5 yr): 0 n (%) 1-3 n (%) |
270 (96.1) 11(3.9) |
28 (96.6) 1(3.4) |
298 (96.1) 12(3.9) |
0.9014 |
| Ear infections episodes (4-5 yr): 0 n(%) 1-3 n(%) ≥4 n(%) |
212(75.4) 64(22.8) 5(1.8) |
19(65.5) 9(31.0) 1(3.4) |
231(74.5) 73(23.5) 6(1.9) |
0.4754 |
| Angina episodes (4-5 yr): 0 n(%) 1-3 n(%) ≥4 n(% |
84(29.9) 148(52.7) 49(17.4) |
7(24.1) 11(37.9) 11(37.9) |
91(29.4) 159(51.3) 60(19.4) |
0.0285 |
| Laryngitis episodes (4 -5 yr): 0 n(%) 1-3 n(%) ≥4 n(%) |
233(82.9) 47(16.7) 1(0.4) |
21(72.4) 6(20.7) 2(6.9) |
254(81.9) 53(17.1) 3(1.0) |
0.0022 |
| Bronchitis episodes (4-5 yr): 0 n(%) 1-3 n(%) ≥ 4 n(%) |
180(64.1) 99(35.2) 2(0.7) |
11(37.9) 15(51.7) 3(10.3) |
191(61.6) 114(36.8) 5(1.6) |
0.0000 |
| Pneumonia episodes (4-5 yr): 0 n(%) 1-3 n(%) ≥ 4 n(%) |
241(85.8) 40(14.2) 0(0.0) |
21(72.4) 7(24.1) 1(3.4) |
262 (84.5) 47(15.2) 1(0.3) |
0.0025 |
| Wheezing episodes: 0 n(%) 1-2 n(%) ≥3 n (%) |
231(82.2) 36(12.8) 14(5.0) |
16(55.2) 5(17.2) 8(27.6) |
247(79.7) 41(13.2) 22(7.1) |
0.0000 |
| Wheezing days: 0 n(%) 1-12 n(%) ≥13 n(%) |
231(82.2) 29(10.3) 21(7.5) |
16(55.2) 5(17.2) 8(27.6) |
247(79.7) 34(11.0) 29(9.4) |
0.0006 |
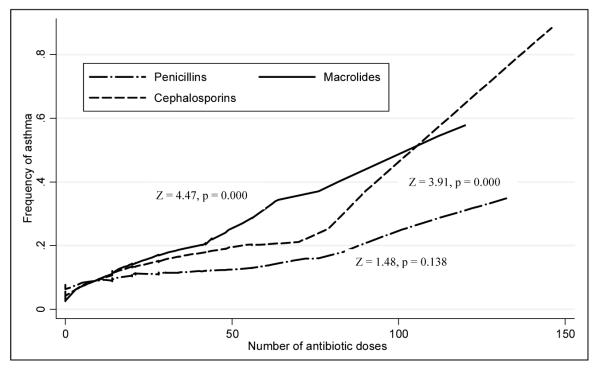
A large proportion of children (78.8%) used oral antibiotics in the follow-up. Among those who did, 17% took only penicillins, 14% only macrolides, 9% only cephalosporins; 37% used two antibiotic classes while 24% all three. There was a significant trend for asthma and the severity of respiratory infections (number of episodes) with the total number of antibiotic doses used in the follow up. While for asthma the significant trend was only observed for macrolide and cephalosporin antibiotics, the use of all antibiotic classes increased with the number of respiratory infections (Table 3).
Table 3.
Nonparametric trend for the number of antibiotic doses grouped by asthma and respiratory infections recorded at 4-5 years of age.
| Antibiotics (doses) |
Asthma | Respiratory infections | ||
|---|---|---|---|---|
| Z value | P level | Z-value | P level | |
| Penicillins | 1,48 | 0.138 | 8.23 | 0.000 |
| Macrolides | 4.47 | 0.000 | 7.83 | 0.000 |
| Cephalosporins | 3.91 | 0.000 | 7.64 | 0.000 |
| Other | 0.63 | 0.531 | 3.36 | 0.001 |
| Total | 3.88 | 0.000 | 11.12 | 0.000 |
On average, the mean number of antibiotic doses used by the children with asthma (mean=94.2, 95%CI: 90.5–98.4) twice exceeded the mean number of doses used by non-asthmatics (mean=40.1, 95%CI: 35.4–46.7). Many more asthmatic children used antibiotics belonging to two or more classes compared with non-asthmatics (64.4% vs. 20.6%). Children who used antibiotics belonging to two or more classes reported threefold higher number of doses (107.1; 95%CI: 104.6–109.6) compared with others (26.0; 95%CI:25.3– 6.7). Fig. 1 suggests a dose-response relationship between the number of macrolide and cephalosporin antibiotics used in early childhood and asthma in 5-year-olds.
Fig. 1.
Frequency of asthma (crude data) related to the exposure of various antibiotic classes expressed in the number of doses. Trends for asthma related to doses were much stronger for macrolides and cephalosporins compared with penicillins (marked z values for trends).
To assess the relationship between asthma occurrence and antibiotic use we ran three separate multivariable regression models for each antibiotics class. While in the univariate analysis (model I) only crude estimates of the association were calculated, in the model II the risk estimates were adjusted for a set of a priori chosen potential confounders (child’s gender, maternal age and education, maternal atopy, parity, prenatal and postnatal ETS), and in the final stage of the analysis (model III) in addition to the confounders mentioned earlier, the total number of respiratory infection episodes ranked in tertiles (≤2, 3–4, >4) were included as well.
Crude logistic OR estimate for asthma related to the overall intake of antibiotics (model I) was found to be significant (OR=2.14, 95%CI: 1.37–3.34) and OR did not change very much in the model II (OR=2.08, 95%CI: 1.32–3.28). However in the model III, which was additionally adjusted for respiratory infections, OR lost its statistical significance (OR=1.65; 95%CI: 0.93–2.93) (Table 5). The same approach applied for the separate classes of antibiotics has shown that beside macrolide antibiotics (adjusted OR=2.14, 95%CI: 1.16–3.95) only cephalosporins were significantly associated with asthma (adjusted OR=1.98; 95%CI: 1.14–3.37).
Table 5.
Association between asthma and use of antibiotics at 4–5 years of age, adjusted for potential confounders. ORs (odds ratio) estimated from various models of multivariable logistic regression.
| Antibiotic class | Crude OR | Adjusted OR* | Adjusted OR** |
|---|---|---|---|
| Penicillins | 1.56(0.94–2.57) | 1.49(0.89–2.49) | 1.05(0.60–1.84) |
| Macrolides | 2.75(1.63–4.62) | 2.71(1.58–4.63) | 2.14(1.16–3.95) |
| Cephalosporins | 2.51(1.55–4.05) | 2.45(1.49–4.02) | 1.98(1.14–3.37) |
| Other | 1.60(0.34–7.56) | 1.52(0.31–7.54) | 0.88(0.17–4.47) |
| Total | 2.14(1.37–3.34) | 2.08(1.32–3.28) | 1.65(0.93–2.93) |
OR adjusted for age, education, maternal atopy, parity and ETS.
OR adjusted for age, education, maternal atopy, parity, ETS, respiratory infections and antibiotic doses.
Table 6 presents incidence risk ratios (IRR) for wheezing episodes associated with the exposure to antibiotics, which were based on the Poisson robust regression models. While the univariate regression analysis has shown a significant association between the use of all antibiotic classes and frequency of wheezing episodes, the adjusted IRRs (model III) confirmed only the significant effect of macrolide antibiotics (IRR=1.91; 95%CI: 1.12–3.27). The overall number of antibiotic doses was also significantly associated with wheezing episodes (adjusted IRR=2.17, 95%CI: 1.57–2.99).
Table 6.
Association between the frequency of wheezing episodes and use of antibiotics at 4–5 years of age adjusted for potential confounders. Incidence rate ratio (IRR) estimated from various multivariate robust Poisson regression models.
| Antibiotic class | Crude IRR | Adjusted IRR* | Adjusted IRR** |
|---|---|---|---|
| Penicillins | 1.85(1.22–2.83) | 1.81(1.21–2.71) | 1.33(0.88–2.03) |
| Macrolides | 2.52(1.69–3.77) | 2.46(1.63–3.70) | 1.91(1.12–3.27) |
| Cephalosporins | 1.54(1.06–2.24) | 1.47(1.05–2.04) | 1.08(0.77–1.52) |
| Others | 2.74(1.04–7.20) | 2.57(1.07–6.20) | 1.60(0.65–3.93) |
| Total | 2.17(1.57–2.99) | 2.15(1.59–2.91) | 2.17(1.57–2.99) |
OR adjusted for age, education, maternal atopy, parity and ETS.
OR adjusted for age, education, maternal atopy, parity, ETS, respiratory infections and antibiotic doses.
DISCUSSION
Our study confirmed the significant dose-effect relationship between the use of the broad spectrum antibiotics (macrolide and cephalosporin) in early childhood and the development of asthma in 5-year-olds. The interpretation of the results is not easy as there is a much higher susceptibility among asthmatic subjects to both viral and bacterial respiratory infections, for which antimicrobial drugs may be prescribed. Both macrolide and cephalosporin antibiotics are nowadays often prescribed for the treatment of step throat, tonsillitis, bronchitis, pneumonia or other infections even as initial therapy (29, 30). In these circumstances, the association between asthma and the use of antibiotics could have resulted from the reverse causation bias. To minimize this kind of bias, all risk estimates of asthma attributable to antibiotics use were adjusted for respiratory episodes. Therefore, we believe that our findings on the association between the broad spectrum antibiotics and the development of asthma in early childhood would be independent of the effect of respiratory infections and provide an additional argument in favor of the causal association between the use of antibiotics and childhood asthma.
To our knowledge this is the one of few prospective observational study, which has compared the effect of various antibiotics classes on asthma in early childhood adjusted for the severity of respiratory infections. Although macrolides and cephalosporins were associated with asthma, however, the significant relationship between severity of wheezing episodes and the use of macrolide antibiotics may point to macrolide antibiotics as having a stronger proallergic effect. It is important to mention that interactions term between the use of macrolide and cephalosporin antibiotics was found to be statistically insignificant.
There may be several possible mechanisms whereby antibiotic use may be associated with an increased risk of asthma. First, antibiotics may increase the risk of asthma by reducing the intensity and duration of bacterial infections. In this sense, the study would be in agreement with the “hygiene hypothesis,” which assumes that reducing exposure to bacteria or living in a hygienic environment with the low microbial exposure may bring about an unbalance resulting in an increase atopic immune responses (Th2), which subsequently show the way to the development of allergic reactions (31). Moreover, some antibiotic classes such as macrolides have been found to have a number of potential immunomodulatory ability to suppress the production of proinflammatory cytokines, decrease mucus synthesis and promote inflammatory cell apoptosis in bronchial epithelium (32, 33). As the modulation of the immune system appears to follow cycles of activation and suppression around some homeostasis level, one may hypothesize that the antibiotic-related suppression of allergic inflammatory responses within bronchial tract in the course of antibiotic treatment may later follow an activation phase possibly leading to greater than before atopic immune response in Th2 children or the impairment of Th1 immune responses. An alternate explanation for the increased risk of asthma associated with various types of antibiotic used in infancy may be explained by the changes in bowel flora (25). Although all antibiotics decrease anaerobic microflora in infants, but use of the broad spectrum cephalosporins leads to the significant suppression of lactobacilli and bifidobacteria, which lead to the impairment of TH1 immune responses (34).
Our results would fit very well within the pooled range of risk estimates for asthma linked with the use of antibiotics derived from a very big sample of children population taken from different countries where similar methodological study approach was used. The comprehensive metaanalysis of observational retrospective and prospective studies published recently by Marra et al. (35) has already documented that one or more courses of antibiotics during the first year of life appeared to be a risk factor for the development of childhood asthma, defined as medical diagnosis between the age of 1 to 18 years. In the dose-response analysis that included data from a total of 27,167 children and 3,392 asthma cases, the pooled odds ratio (OR) was 2.05 (95%CI: 1.41–2.99). The association was significantly stronger in the retrospective studies (OR, 2.82; 95% CI, 2.07–-3.85) than the prospective studies (OR, 1.12; 95% CI: 0.88–1.42). The overall OR for the dose-response analysis was 1.16 (95% CI, 1.05–1.28) for each additional course of antibiotics; however, this association was not significantly stronger in the retrospective studies (OR, 1.37; 95% CI, 1.18–1.60) relative to the prospective studies (OR, 1.07; 95% CI, 0.95–1.20). There were some discrepancies between studies under comparison, which could mainly have been caused by the different study designs and the lack of adjustment for important confounders including respiratory tract infections.
An excellent example of retrospective study design is very large international ISAAC study with the objective to investigate the associations between the use of antibiotics in the first year of life and symptoms of asthma or other allergies in children 6 and 7 years old (26). In this study parents or guardians of children 6 and 7 years old recruited from 29 countries were approached to collect information on health outcomes and environmental exposures such as antibiotics use in the first year of life. Reported use of antibiotics in the first year of life was associated with an increased risk of current asthma symptoms adjusted for confounders (OR=1.70; 95%CI: 1.60–1.80). Retrospective design of the study is extremely prone to recall bias, particularly if parents of children with asthma were more likely to recall antibiotic use in the first year of life than parents of children without asthma. One of the most important limitation of this study design was also the fact that information on the use of antibiotics failed to consider types of antibiotics used, in particular whether they were broad-spectrum or narrow-spectrum.
An example of prospective design of the study based on administrative records is recently published paper based on almost a quarter of a million children followed for up to 7 years, which aimed at exploring the association between antibiotic exposure before 1 year of age and development of childhood asthma (36). The study was able to adjust for many potential confounding factors that have not been previously examined such as method of delivery, surgery during the first year, and the presence of birth complications. The results have also shown that antibiotic exposure in the first year of life was associated with a small risk of developing asthma in early childhood, however, the risk of asthma was not associated with any particular type or class of antibiotics. In the additional analysis the authors excluded from the analysis antibiotics prescribed for respiratory tract infections such as bronchitis, or otitis media, and, in another one, all children with a diagnosis for these conditions. The additional analyses performed by authors indicated that the association was in fact larger than in the primary analysis. As the study was based on administrative records and not upon the data collected for the purpose of research, the results may suffer from problems concerning quality and comparability of data collected from various medical institutions or extracted from physician billings (different specialists). Moreover, in this kind of the study the data regarding the number of doses or type of antibiotics prescribed by doctors may not reflect the real doses of particular antibiotics administered to the child being on home care. Some antibiotics may be available over counter and mothers may treat mild infections in their children without medical prescriptions if antibiotics were kept in the household. Moreover, epidemiologic studies based on administrative records offer no possibility to adjust the results for very relevant confounders such as parental or household characteristic potentially implicated in the development of asthma (maternal atopy, smoking habits, mites, nutrition etc.).
The issue of reverse causation or confounding by respiratory infections is the key problem in establishing the causality of antibiotic treatment and asthma because more frequent diagnosis of respiratory infections in asthmatic children could subsequently lead to more frequent administration of antibiotics. Fortunately, this problem was already considered in some previous studies. For example, Celedon et al. (23) found some attenuation of risk estimates for asthma attributable to antibiotics after additional adjustment for the presence of lower respiratory infections and the number of office visits in the first year of life. In other studies (26, 37) the confounding effect of chest infections have been avoided in the analysis by excluding antibiotics prescribed for lower respiratory infections. Yet, in another study the association between antibiotics and asthma was adjusted for the presence of lower respiratory infections in the first 2 years of life (18). However, most epidemiologic studies on antibiotics and asthma did not consider the impact of that reverse causation on the association between antibiotics asthma in early childhood.
Our study has some limitations, which mainly resulted from the small study sample. In addition, information gathered from mothers on the use of antibiotic classes, medical diagnosis of asthma or respiratory infections occurring in the follow-up were not validated by medical records. We did not applied spirometric procedures either, which could have refined the asthma phenotype and its stage (38, 39). Information gathered from mothers on the use of antibiotic classes and medical diagnosis of asthma were not validated by medical records, but the interviewers always stressed the point that only the medical diagnosis of attending doctor is valid for the study. We do not think that confrontation of medical records on prescriptions is an ideal way of validation of antibiotics use, since the factual use of drugs by children, may be different from that prescribed by physician and documented in medical records. In this sense, our study provides the factual information about the use of antibiotics by children. We have to add that all records, where mothers were not certain about the name of antibiotics were excluded from the analysis. We believe that the regular interviews of mothers in relatively short intervals over the follow-up gave us a valid information about the pattern of respiratory infections and factual data about the use of antibiotics in children. Nevertheless, the differential recall bias may be potential explanation for our findings on antibiotics and asthma since mothers of children with asthma might be more likely to recall the use of antibiotics. However, this seems unlikely because of the lack of association between certain antibiotic classes and asthma or wheezing.
Our study sample may not be representative of the entire urban children population in the country because enrollment covered children born to nonsmoking mothers with singleton pregnancies between the ages of 18 and 35 years who were free from such chronic diseases as diabetes and hypertension. On the other hand, these inclusion criteria helped us eliminate from the study those children who were at a greater risk for atopy due to maternal chronic diseases or active smoking.
Concluding, we believe that the hypothesis on the use of broad spectrum antibiotics in early childhood as a potential risk of asthma found some new arguments in our study. Given the limitations of the study, further large-scale prospective observational studies are needed to decide whether this association is causal. To what extent the results may have practical implications for prevention of allergic diseases is a problem to be further elucidated. If the results are repeated, the use of narrower spectrum antibiotics should be considered.
Table 4.
Mean number of reported antibiotic doses used in asthmatic and non-asthmatic children at 4-5 years of age
| Antibiotics (doses) |
Asthma (−) | Asthma (+) | ||||
|---|---|---|---|---|---|---|
| Mean | Poisson exact 95%CI | Mean | Poisson exact 95%CI | |||
| Penicillins | 18.6 | 18.0 | 19.1 | 30.2 | 28.2 | 32.4 |
| Macrolides | 10.4 | 10.3 | 10.8 | 27.7 | 25.7 | 29.8 |
| Cephalosporins | 10.9 | 10.5 | 11.3 | 32.8 | 30.6 | 35.0 |
| Other | 1.2 | 1.1 | 1.3 | 3.5 | 2.8 | 4.3 |
| Total | 40.1 | 35.4 | 46.7 | 94.2 | 90.5 | 98.4 |
Acknowledgment
The study received funding from an RO1 grant entitled, “Vulnerability of the Fetus/ Infant to PAH, PM2,5 and ETS” (5 RO1 ES10165 NIEHS; 02/01/00-01/31/04) and The Gladys and Roland Harriman Foundation N. York. Principal investigator: Prof. FP Perera, Co-investigator: Prof. WA Jedrychowski. The study was partly financed by the Centre for Research and Studies in Biomedicine in Luxembourg.
Footnotes
A preliminary report of this work was presented at the 5th Symposium on “Brain - Viscera Axis: Basic and Clinical Aspects”, Cracow, Poland, September 25th, 2010.
Conflict of interests: None declared.
REFERENCES
- 1.Burr ML, Butland BK, King S, Vaughan-Williams E. Changes in asthma prevalence: two surweys 15 years apart. Arch Dis Child. 1989;64:1452–1456. doi: 10.1136/adc.64.10.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yunginger J, Reed CE, O’Connel EJ, Melton LJ, O’Fallon WM, Silverstein MD. A community-based study of the epidemiology of asthma. Incidence rates, 1964–1983. Am Rev Respir Dis. 1992;146:888–894. doi: 10.1164/ajrccm/146.4.888. [DOI] [PubMed] [Google Scholar]
- 3.Woolcock A, Peat JK. Evidence for the increase in asthma worldwide. In: Chadwick DJ, Cardew G, editors. The Rising Trends in Asthm. Ciba Foundation, J. Wiley and Sons; Chichester: 1997. pp. 122–134. [DOI] [PubMed] [Google Scholar]
- 4.von Mutius E, Illi S, Hirsch T, et al. Frequency of infections and risk of asthma, atopy and airway hyperresponsiveness in children. Eur Respir J. 1999;14:4–11. doi: 10.1034/j.1399-3003.1999.14a03.x. [DOI] [PubMed] [Google Scholar]
- 5.Jedrychowski W, Wojtyniak B, Szafraniec K, Gorynski P. Trends in hospitalization rates of childchood asthma in Poland. Central Europ J Occup Environ Med. 2004;10:275–282. [Google Scholar]
- 6.Pawlinska-Chmara R, Wronka I, Muc M. Prevalence and correlates of allergic diseases among children. J Physiol Pharmacol. 2008;59(Suppl 6):549–556. [PubMed] [Google Scholar]
- 7.Martinez FD, Holt PG. Role of microbial burden in etiology of allergy and asthma. Lancet. 1999;354(Suppl):SII12–SII15. doi: 10.1016/s0140-6736(99)90437-3. [DOI] [PubMed] [Google Scholar]
- 8.Wickens K, Crane J, Pearce N, Beasley R. The magnitude of the effect of smaller family sizes on the increase in the prevalence of asthma and hay fever in the UK and New Zealand. J Allergy Clin Immunol. 1999;104:554–558. doi: 10.1016/s0091-6749(99)70323-4. [DOI] [PubMed] [Google Scholar]
- 9.Faniran AO, Peat JK, Woolcock AJ. Prevalence of atopy, asthma symptoms and diagnosis, and the management of asthma: comparison of an affluent and a non-affluent country. Thorax. 1999;54:606–610. doi: 10.1136/thx.54.7.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bali TM, Castro-Rodriguez JA, Griffith KA, Holberg CJ, Martinez FD, Wright AL. Siblings, day-care attendance, and the risk of asthma and wheezing during childhood. N Engl J Med. 2000;343:538–543. doi: 10.1056/NEJM200008243430803. [DOI] [PubMed] [Google Scholar]
- 11.Strachan DP. Family size, infection and atopy: the first decade of the “hygiene hypothesis”. Thorax. 2000;55(Suppl 1):S2–S10. doi: 10.1136/thorax.55.suppl_1.s2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McKeever TM, Lewis SA, Smith C, et al. Siblings, multiple births, and the incidence of allergic disease: a birth cohort study using the West Midlands General Practice Research Database. Thorax. 2001;56:758–762. doi: 10.1136/thorax.56.10.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farooqi IS, Hopkin JM. Early childhood infection and atopic disorder. Thorax. 1998;53:927–932. doi: 10.1136/thx.53.11.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pekkanen J, Remes S, Kajosaari M, Husman T, Soininen L. Infections in early childhood and risk of atopic disease. Acta Paediatr. 1999;88:710–714. doi: 10.1080/08035259950168964. [DOI] [PubMed] [Google Scholar]
- 15.Ponsonby AL, Couper D, Dwyer T, Carmichael A, Kemp A. Relationship between early life respiratory illness, family size over time, and the development of asthma and hay fever: a seven year follow up study. Thorax. 1999;54:664–669. doi: 10.1136/thx.54.8.664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tantisira KG, Weiss ST. Childhood infections and asthma: at the crossroads of the hygiene and Barker hypotheses. Respir Res. 2001;2:324–327. doi: 10.1186/rr81. T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wickens K, Pearce N, Crane J, et al. Antibiotic use in early childhood and the development of asthma. Clin Exp Allergy. 1999;29:766–777. doi: 10.1046/j.1365-2222.1999.00536.x. [DOI] [PubMed] [Google Scholar]
- 18.Droste JH, Wieringa MH, Weyler JJ, et al. Does the use of antibiotics in early childhood increase the risk of asthma and allergic disease? Clin Exp Allergy. 2000;30:1547–1553. doi: 10.1046/j.1365-2222.2000.00939.x. [DOI] [PubMed] [Google Scholar]
- 19.Wjst M, Hoelscher B, Frye C, et al. Early antibiotic treatment and later asthma. Eur J Med Res. 2001;6:263–271. [PubMed] [Google Scholar]
- 20.McKeever TM, Lewis SA, Smith C, et al. Early exposure to infections and antibiotics and the incidence of allergic disease: a birth cohort study with the West Midlands General Practice Research Database. J Allergy Clin Immunol. 2002;109:43–50. doi: 10.1067/mai.2002.121016. [DOI] [PubMed] [Google Scholar]
- 21.Thomas M, Murray CS, Simpson B, et al. Early life antibiotic exposure and subsequent risk of asthma: a case control study [abstract] Thorax. 2003;58:67. [Google Scholar]
- 22.Cullinan P, Harris J, Mills P, et al. Early prescriptions of antibiotics and the risk of allergic disease in adults: a cohort study. Thorax. 2004;59:11–15. [PMC free article] [PubMed] [Google Scholar]
- 23.Celedon JC, Fuhlbrigge A, Rifas-Shiman S, et al. Antibiotic use in the first year of life and asthma in early childhood. Clin Exp Allergy. 2004;34:1011–1016. doi: 10.1111/j.1365-2222.2004.01994.x. [DOI] [PubMed] [Google Scholar]
- 24.Custovic TM, Woodcock A, Morris A. Atopic wheezing and early life antibiotics exposure: a nested case-control study. Pedatr Allergy Pulmonol. 2006;17:184–188. doi: 10.1111/j.1399-3038.2006.00389.x. [DOI] [PubMed] [Google Scholar]
- 25.Kozyrskyj AL, Ernst P, Becker AB. Increased risk of childhood asthma from antibiotic use in early life. Chest. 2007;131:1753–1759. doi: 10.1378/chest.06-3008. [DOI] [PubMed] [Google Scholar]
- 26.Foliaki S, Pearce N, Bjorkstein B, et al. Antibiotic use in infancy and symptoms of asthma, rhinoconjunctivitis, and eczema in children 6 and 7 yeyars old: International Study on Asthma and Allergies in Childhood Phase III. J Allergy Clin Immunol. 2009;124:982–989. doi: 10.1016/j.jaci.2009.08.017. [DOI] [PubMed] [Google Scholar]
- 27.Jedrychowski W, Whyatt R, Camann D, et al. Effect of prenatal PAH exposure on birth outcomes and neurocognitive development in a cohort of newborns in Poland. Study design and preliminary ambient data. Int J Occup Med Environ Health. 2003;16:21–29. [PubMed] [Google Scholar]
- 28.Dixon WJ, editor. BMDP Statistical Software Manual. University of California Press; Berkeley: 1992. [Google Scholar]
- 29.Stille CJ, Antrade SE, Huang SS, et al. Increased use of second-generation macrolide antibiotics for children in nine health plans in the United States. Pediatrics. 2004;114:1206–1211. doi: 10.1542/peds.2004-0311. [DOI] [PubMed] [Google Scholar]
- 30.Cohet C, Cheng S, MacDonald C, et al. Infections, medication use, and the prevalence of symptoms of asthma, rhinitis, and eczema in childhood. J Epidemiol Commun Health. 2004;58:852–857. doi: 10.1136/jech.2003.019182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Romagnani S. Human TH1 and TH2 subjects: regulation of differentiation and role of protection and immunopathology. Int Arch Allergy Immunol. 1992;98:279–285. doi: 10.1159/000236199. [DOI] [PubMed] [Google Scholar]
- 32.Shinkai M, Henke MO, Rubin BK. Macrolide antibiotics as immunomodulatory medications: proposed mechanism of action. Pharmacol Ther. 2008;117:393–405. doi: 10.1016/j.pharmthera.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 33.Friedlander AL, Richard KA. Chronic macrolide therapy in inflammatory airways disease. Chest. 2010;138:1202–1212. doi: 10.1378/chest.10-0196. [DOI] [PubMed] [Google Scholar]
- 34.Pulverer G, Ko H, Beuth J. Immunomodulating effects of antibiotics influencing digestive flora. Pathol Biol (Paris) 1993;41:253–258. [PubMed] [Google Scholar]
- 35.Marra F, Lynd L, Coombes M, et al. Does antibiotic exposure during infancy lead to development of asthma? A systematic review and metaanalysis. Chest. 2006;129:610–618. doi: 10.1378/chest.129.3.610. [DOI] [PubMed] [Google Scholar]
- 36.Marra F, Marra CA, Richardson K, et al. Antibiotic use in children is associated with increased risk of asthma. Pediatrics. 2009;123:1003–1010. doi: 10.1542/peds.2008-1146. [DOI] [PubMed] [Google Scholar]
- 37.Illi S, von Mutius E, Frye C, et al. Early childhood infectious diseases and the development of asthma up to school age: a birth cohort study. BMJ. 2001;322:390–395. doi: 10.1136/bmj.322.7283.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jesenaki M, Babusikova E, Petrikova M, et al. Cough reflex sensitivity in various phenotypes of childhood asthma. J Physiol Pharmacol. 2009;60(Suppl 5):61–65. [PubMed] [Google Scholar]
- 39.Kosciuch J, Krenke R, Gorska K, et al. Relationship between airwaywall thickness assessed by high resolution computed tomography and lung function in patients with asthma and chronic obstructive pulmonary disease. J Physiol Pharmacol. 2009;60(Suppl 6):71–76. [PubMed] [Google Scholar]