Abstract
Study Design
In vivo three-dimensional facet joint space width measurement.
Objective
To determine lumbar facet joint space width within clinically relevant topographical zones in vivo and its correlations with age, level and presence of lower back pain symptoms.
Summary of Background Data
Narrowing of the facet joint gap, articular cartilage thinning, and subarticular cortical bone hypertrophy are frequently observed age-related changes. Facet joint space width is a well-defined parameter to evaluate osteoarthritis. To the best of our knowledge, there is no other study that quantifies three-dimensional facet joint space width distribution in vivo.
Methods
Three-dimensional measurement to quantify facet joint space width distribution based on five clinically relevant topographic zones in a cohort of healthy and symptomatic low-back-pain volunteers using subject-based three-dimensional CT models with respect to spinal level, subject age, gender and presence/absence of lower back pain.
Results
Facet joint space width was 1.93±0.51 (mean ± standard deviation) mm for the central zone, 1.75±0.48 mm for the superior zone, 1.63±0.49 mm for the inferior zone, 1.48±0.44 mm for the medial and 1.65±0.48 mm for the lateral zone, respectively. There were no significant differences between right and left facet joints. Males showed larger space width than females. Overall, space width of symptomatic subjects was significantly narrower when compared against the asymptomatic group. Facet joints in the peripheral zones were narrower than in the central zone. Age-group comparisons showed local narrowing occurring as early as in the third decade at the inferior zone of L5/S1 with all the remaining zones implicated after the fourth decade.
Conclusions
This in vivo study shows variations in facet joint space width narrowing with spinal level and region within the facet joint and in vivo evidence of localized, age-influenced facet cartilage thinning. Techniques developed in this study may be applied in the detection of early osteoarthritis-related changes in the facet joints.
Keywords: lumbar spine, facet joint, facet joint space width, facet joint degeneration, osteoarthritis, three-dimensional space width distribution
Introduction
Facet joints are synovial joints in the spine which play an important role in controlling kinematics of the motion segment and transmitting loading in the spine 1-3. The facet joints undergo degenerative and osteoarthritic changes similar to those of other weight-bearing joints 4. Extensive motion and loading conditions can contribute to facet joint osteoarthritis (OA) development. Facet joint OA has been considered as a potential source of low back pain and disability and contributes to 15-45% of chronic low back pain 5.
Osteoarthritis is, in general, characterized radiographically by joint space narrowing, subchondral bone sclerosis and osteophyte formation 6, 7. Among these parameters, joint space narrowing has been considered to closely correlate to cartilage degeneration 6, 8. For the facet joint, narrowing of the joint space, thinning of articular cartilage and subarticular cortical bone hypertrophy are frequently observed changes due to the aging process 8, 9.
In clinical practice, plain radiography remains the main screening technique to assess OA changes; however, facet OA evaluation by plain radiogram requires special techniques due to three-dimensional (3D) orientation of the facet joint 8. Ever since computed tomography (CT) made its appearance as a clinical diagnostic tool, it has been commonly used to provide a more accurate and anatomically correct evaluation of the facet joint geometry. Various parameters, such as facet joint orientation and joint area, have been previously reported based on CT methods 3, 10-13. The results of these studies indicated that variation of orientation of the facet joint is associated with age-related changes in load-bearing and development of lumbar facet joint OA 11-13. Pathria et al, Weishaupt et al, and Kalichman et al used transverse CT as the diagnostic methods in the assessment of OA of the lumbar facet joint 8, 14, 15. Using this approach, they were able to identify the abnormalities associated with facet joint OA progression. However, these studies are qualitative only in nature, and facet joint space narrowing was evaluated within a limited number of transverse slices.
Macroscopic evaluation of the whole facet joint surface using mapping systems allowed detailed description of extent and location of the cartilage degeneration 16, 17. Analysis of the topographical patterns within anatomically-defined zones on the surface of the facet joint enables investigation of the effects of segmental lumbar motion on facet joint degeneration process.
We have developed a novel method of precise measurement of the 3D space width distribution of lumbar facet joint using 3D subject-based CT models 18, 19. This method allows measurement of facet joint space width distribution throughout the joint surface; however, a detailed mapping system has not been established to evaluate extent and location of the facet degeneration represented by narrowing of the facet joint space width. The aim of the present study was to determine lumbar facet joint space width within clinically relevant topographical zones in vivo and its correlations with age, level and presence of lower back pain.
Materials and Methods
Subjects
A total of 96 volunteers participated in this IRB-approved study (IRB Approval No. 00042801): Forty-five female and fifty-one males, average age 37.6 years (range; 22-59 years), average weight 75.4 kg (range; 45-129 kg), average height 168.6 cm (range; 145-188 cm). All subjects were screened for presence of lower back pain and preexisting lumbar spine pathology. Subjects with lower back pain were categorized as symptomatic subjects (Table 1) with inclusion criteria defined as recurrent low back pain with at least two episodes of at least 6 weeks. Exclusion criteria for the symptomatic group were prior surgery for back pain, age over 60 years, claustrophobia or other contraindication to magnetic resonance (MR) and CT imaging, severe osteoporosis, severe disc collapse at multiple levels, severe central or spinal stenosis, destructive process involving the spine, litigation, or compensation proceedings, extreme obesity, congenital spine defects, and previous spinal injury. Healthy subjects were categorized as asymptomatic subjects with exclusion criteria for the asymptomatic group defined by the presence of the low back pain, previous spinal surgery, history of low back pain, age over 60 years, obesity, and claustrophobia or other contraindication to MR and CT imaging.
Table 1.
Study population categorized by gender, symptoms and age.
| Male (n = 51) | Female (n = 45) | |||
|---|---|---|---|---|
| Asymptomatic (n = 33) | Symptomatic (n = 18) | Asymptomatic (n = 29) | Symptomatic (n = 16) | |
| 20s | 10 | 3 | 9 | 2 |
| 30s | 11 | 9 | 11 | 5 |
| 40s | 9 | 3 | 7 | 4 |
| 50s | 3 | 3 | 2 | 5 |
Creation of facet joint surface model
Each subject underwent lumbar CT (Volume Zoom, Siemens, Malvern, PA) scans in supine position. Raw imaging data were post-processed in axial plane at 1.0 mm slice thickness and exported in DICOM format. The facet joint surfaces were traced from axial DICOM images in custom-written program (Microsoft Visual C++ 2003 under Microsoft Foundation Class programming environment) using a tablet digitizer (Wacom Intuos 3; Wacom, Saitama, Japan). Particular care was taken to identify and exclude ostophyte formations from the joint surface. Tracing methodology was previously described by Otsuka et al 13. A total of 1,920 individual facet joint surface models were created and exported as point-cloud data sets. Subsequently, triangular surface meshes were created from point-cloud data in the custom-written program.
Definition of a local coordinate system
A local coordinate system was set in order to establish a mapping system on the facet joint. A normal vector was calculated for each mesh element and a mean normal vector of all normal vectors was calculated through the entire surface (Figure 1). The facet joint surface area center was calculated and the origin of the local coordinate system was set on said surface area center. The mean normal vector was defined as one of the coordinate system axes. This axis and the CT coordinate system pointing towards the cranial direction formed a plane. The second coordinate was determined in this plane to be perpendicular to its mean normal vector and directed towards the cranial direction. The third coordinate was determined by the cross product between the first and the second vectors (Figure 2).
Figure 1.
Polygon mesh (red lines) of the facet surface, normal vectors of each polygon (green lines) and average surface normal vector (yellow line). Coordinates represent CT coordinate system.
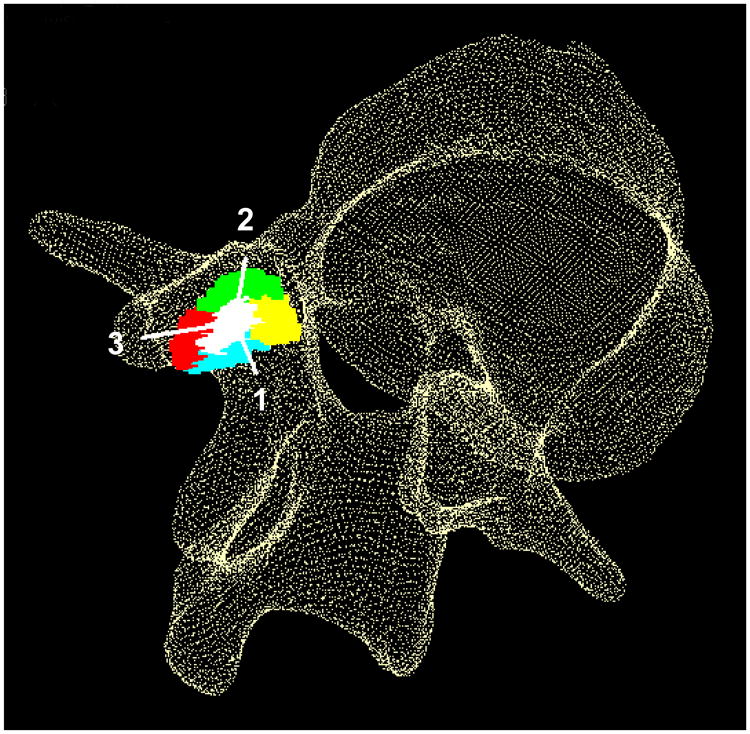
Figure 2.
Local coordinate system and five zones on facet joint surface. 1: direction of mean surface normal vector, 2: cranial direction, 3: direction orthogonal to Axis 1 and Axis 2. Green: superior zone, Red: lateral zone, Cyan: inferior zone, Yellow: medial zone, White: central zone.
Determination of five topographic zones
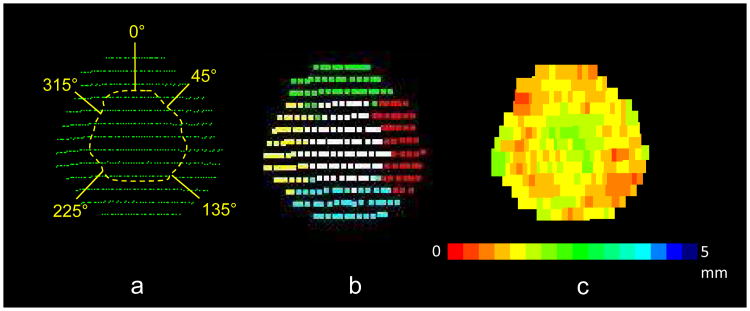
Five topographic zones consisting of central, superior, inferior, medial and lateral zones were determined in 3D space as described next. Cartesian coordinates for each point-cloud data point were converted to a spherical coordinate system with the origin set at each facet joint surface model's area center (Figure 2). The outer margin of the facet joint surface was defined by the points which have the longest distance from the origin within a virtual cone with a vertex angle of 30° 20. The margin of the central zone was defined so that its shape is analogue (concentric) to the outer margin of the facet joint surface and the area of the central zone is one-fifth of the whole facet joint surface area. The peripheral area, outside of the central zone, was divided into four zones defined by an angular parameter in the spherical coordinate of each point (superior zone; ±45°, medial zone; 45°-135°, inferior zone; 135°-225°, lateral zone; 225°-315°) from the cranial axis (Figure 3a). The angles represent projected angles on a plane perpendicular to the mean normal vector of the facet joint surface.
Figure 3.
Facet joint surface zoning. a: Definition of peripheral zones based on angular parameters. The 0° direction corresponds to Axis 2′s (cranial) direction in Figure 2. b: The five zones based on the facet-based coordinate system. c: Facet joint space width distribution map.
Facet joint space width calculation
Facet joint space width was calculated as the least-distances between each pair of opposing surfaces (inferior facet, superior facet). Distances between one point in the point-cloud model of the inferior facet surface and all points in the superior facet surface were calculated in 3D space using a custom-written program 21, 22. The algorithm computes the distance between the point in question and each of its neighbors. Then it records the shortest distance, which will be eventually termed “the least distance”. The inferior facet surface under analysis was set as the reference frame for a least-distance search directed towards the opposing point-cloud data representing the superior facet surface. This least-distance at the point in question on the inferior facet surface was defined as the least-distance at the point in the inferior facet surface. This procedure was repeated for all points in the inferior facet surface. The mean facet joint space width for each zone was calculated by averaging the least facet joint distances within each zone.
Statistical analysis
ANOVA and Fisher post hoc tests were used to evaluate differences between zones, levels, age and symptoms. Differences between right and left sides and gender comparison were carried out with an unpaired t-test. Results were reported as mean and standard deviation. Significance was set to alpha = 0.05.
Results
The average facet joint space width (±SD) was 1.93±0.51 mm for the central zone, 1.75±0.48 mm for the superior zone, 1.63±0.49 mm for the inferior zone, 1.48±0.44 mm for the medial zone and 1.65±0.48 mm for the lateral zone.
Statistical correlation between facet joint space width distribution in right and left facet joints showed no side preference; therefore we used all facet joints individually in the analysis of level, gender, age, and symptoms. Gender comparison showed greater width distribution in males in all zones (p<0.0001). Overall space width was significantly lower in symptomatic subjects (p<0.0001).
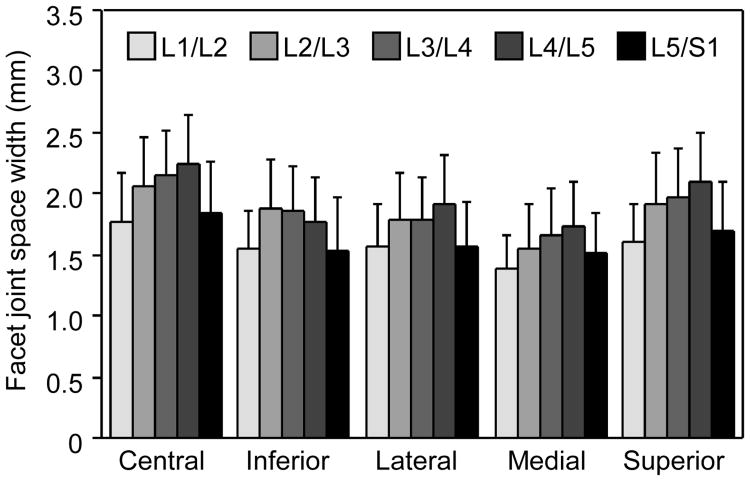
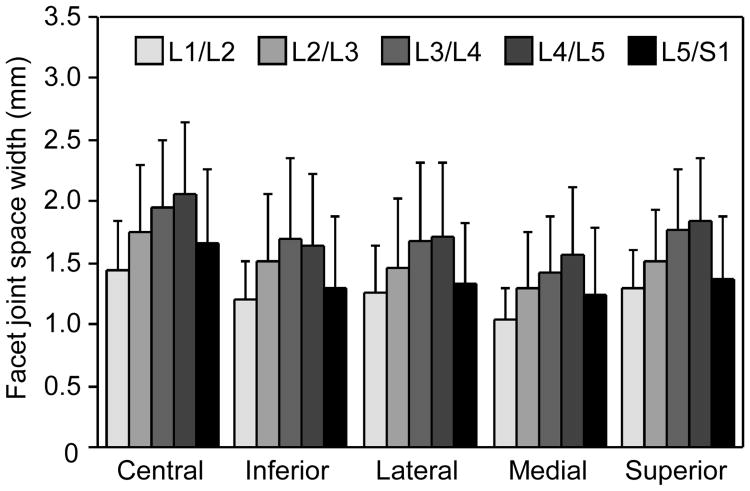
Level comparison showed significant differences. The average facet joint space width for asymptomatic group (Figure 4) was 1.58±0.36 mm at L1/L2; 1.84±0.42 mm at L2/L3; 1.88±0.41 mm at L3/L4; 1.95±0.43 mm at L4/L5 and 1.63±0.41 mm at L5/S1. The facet joint space width at L4/L5 was significantly greater than all levels (p<0.0001) except L3/L4 (p<0.003). The narrowest facet joint space width was measured at L1/L2 and L5/S1 levels with mutual significant difference (p<0.02). When compared with other levels, L1/L2 and L5/S1 were significantly smaller (p<0.0001). The average facet joint space width for symptomatic group was 1.24±0.36 mm at L1/L2; 1.51±0.53 mm at L2/L3; 1.7±0.59 mm at L3/L4; 1.76±0.59 mm at L4/L5; and 1.38±0.56 mm at L5/S1. Similar to the asymptomatic group (Figure 5), facet joint space width at L4/L5 was significantly larger than that at the other levels (p<0.0001) except L3/L4 (p=0.1). The smallest facet joint space widths were again measured at L1/L2 and L5/S1, however there were significant differences between them (p<0.001). L1/L2 was different than every other level (p<0.0001), while L5/S1 was different than L3/L4, L4/L5 level (p<0.0001), and L2/L3 (p<0.003).
Figure 4.
Facet joint space width for asymptomatic subjects.
Figure 5.
Facet joint space width for symptomatic subjects.
The facet joint space width was always larger in the central zone than in the peripheral zones (p<0.0001) for both symptomatic and asymptomatic group. Inferior zone space width was significantly narrower in the asymptomatic group (p<0.0001), and in the symptomatic group (p<0.04) when compared to the superior zone. Space width within the medial zone was the smallest for both groups (p<0.0001).
The data presented in Figure 6 show changes in facet joint space width distribution at different levels with respect to age. Facet joint space width changes started in the fourth decade in the peripheral zones for L1/L2. For L2/L3, narrowing occurred only at the lateral zone in the fifth decade. At L3/L4, narrowing occurred during the fourth decade in lateral and superior zones and facet joint space width increased in the fifth decade. Changes in the L4/L5 level involved all lateral zones in the fourth and fifth decade and central zone in the fifth decade. For L5/S1, narrowing started as early as in the third decade in the inferior zones and implicates all remaining zones after the fourth decade.
Figure 6.
Changes in facet space width with age. Color code indicates significant differences (p<0.05) among different age groups within each spinal level and each zone.
Discussion
The present study measured facet joint space width distribution in vivo to estimate extent and location of the facet joint degeneration using subject-based facet joint 3D CT models. The results of the present study showed that overall facet joint space width at L5/S1 was narrower than that in L3/4 and L4/5. This finding is consistent with a previous study which evaluated facet degeneration using CT grading 23. The zonal analysis in the present study demonstrated that facet joint space width was narrower in the inferior and medial regions of the facet joint. Furthermore, our data shows narrowing of the facet joint space width in the inferior region evident as early as in the third decade. Although previous cadaver-based studies demonstrated that the facet joint cartilage degeneration occurred in younger age population, the present study is the first to demonstrate early degenerative changes in the facet joint in vivo using clinically-available CT by evaluating age-related changes in facet joint space width distribution in a quantitative manner.
Topographic analysis of the whole facet joint area allows for a detailed description of extent and location of the joint degeneration. Macroscopic studies of the whole cartilage surface have been conducted using human cadaveric lumbar spines 16, 17. Although microscopic histological studies evaluate early changes in cartilage degeneration, this analysis is usually performed in arbitrarily-selected slices taken from the specimens. The analysis of the whole facet joint surface is beneficial for comparisons between cartilage degeneration and three-dimensional characteristics of facet joint structure and its biomechanical functions, such as restriction of the segmental motion and load transmission as described later.
In order to describe extent and location of the cartilage lesions in the facet joint, it is crucial to define a mapping system specific to the facet joint. Swanepoel et al defined the central and peripheral regions in the facet joint surface based on the distance of the center of the damaged area from the center of the whole facet joint surface in a quantitative manner 16. Tischer et al further divided the facet joint surface into five topographic zones including the central, superior, medial, inferior and lateral regions; in spite of this, a detailed mapping method was not described 17. In a cadaveric study, the exposed facet joint surface can be rotated manually so that the joint surface becomes parallel to a graphical image plane for analysis. However, the facet joint surface orientation must be defined in space for 3D in vivo analyses. In the present study, joint surface 3D orientation was defined by the mean normal vector calculated by averaging all normal vectors from the elements comprising the surface joint mesh 13. A local coordinate system was determined by using the mean normal vector as one axis of the coordinate. The second coordinate was determined in the anatomical cranio-caudal direction in the present study. A vector product between these two perpendicular directions provides the third axis and completes the coordinate system. The geometry of the facet joint is often assumed as an ellipse and a local facet joint coordinate system can be set to coincide with the axes of such ellipse 3, 24. Under the elliptical shape assumption, eigenvectors can be used to determine the local coordinates in 3D 20; however, the shape of the facet joint is not always elliptical and the directions of the axes other than the normal direction of the facet surface cannot be determined if the shape of the facet is close to a circle. Furthermore, the orientation of the axis of the ellipse declines from the anatomical axis 24, which may obscure the interpretation of the topographic differences in relation to the lumbar spine segmental motion.
The results of the present study showed smaller widths in the facet joint peripheral zones, consisting of superior, lateral, inferior and medial zones, when compared to the central zone. This finding is consistent with previous cadaveric studies which observed distribution of cartilage degeneration in vitro16, 17. Tischer et al observed that most cartilage defects are located in the superior region of the superior facet and in the inferior region of the inferior facet 17. The authors postulated that cartilage degeneration in the superior portion of the superior facet was caused by more cartilage contact with the opposing inferior facet in this region during full flexion, whereas the cartilage degeneration in the inferior portion of the inferior facet with pressure accumulation originated from bone-to-bone contact of inferior portion of inferior facet with superior facet during full extension 1, 17. Increased load transmission through the inferior portion of the inferior facet is also postulated in lordotic posture and erect posture with heavy loads 1. Since segmental lordosis is reported to be higher at L5/S1 25, early onset of the facet joint space narrowing in the inferior region at L5/S1 measured in the present study may be explained by the higher lordosis in this level in addition to the higher load transmission in the lower lumbar levels. This study has shown lateral region facet joint narrowing at L3/L4, L4/L5 and L5/S1 in the fourth decade. Segmental lumbar axial rotation movement is mainly restricted by the facet joint 1 and high contact pressures in the lateral region of the facet joint have been estimated during axial rotation 26. This loading pattern during axial rotation may cause relatively early onset of facet joint space narrowing in the lateral region of the facet joint.
Fibrillation of the joint cartilage has been considered as an early sign of joint degeneration 4, 16, 27. Previous macroscopic studies using cadaveric lumbar spines have made possible early detection of facet joint degeneration by visualizing cartilage fibrillation and demonstrated that facet joint degeneration is initiated at an earlier age than that postulated by studies using clinical CT and MR imaging 8, 14, 15, 28. While fibrillation of the joint cartilage surface can be observed in vivo via arthroscopic images for the synovial joints in the extremities, such technique is not feasible for the facet joint in the present clinical setting. Although joint space narrowing corresponds to a more advanced stage than the cartilage fibrillation in the cartilage degeneration cascade, the zonal analysis of the facet joint space width used in the present study may be useful for early detection of the facet cartilage degeneration using currently available imaging modalities.
This report shows that narrowing of the facet joint width was more prominent for symptomatic subjects. Since average facet joint space width and disc height were found to be linearly-correlated in this study 19, low back pain symptoms should involve low back pain associated with intervertebral disc degeneration. It is believed that facet joint degeneration is secondary to intervertebral disc degeneration and several studies have supported this theory 4, 29. However, macroscopic studies on facet joint degeneration using cadaveric specimens demonstrated early initiation of facet degeneration and did not support the correlation between the facet degeneration and intervertebral degeneration 16, 30. Adams and Hutton addressed different mechanisms of facet joint regional damages and causes for pain under different motion segment movement 1. Future studies are required to clarify relationships between extent and location of facet degeneration and facet joint kinematics in vivo and to identify possible causes for low back pain associated with facet joint degeneration.
This study is not without limitations. Particularly, the small sample sizes on some age groups can lead to less than ideal statistical power. This can happen when too many subgroups are used in the data analysis. Secondly, joint space width was measured by the least distances between the superior and inferior facet joint surfaces in the present study; therefore, thinning of cartilage at individual facet joint could not be estimated in this technique.
Although normal vectors for all polygons were calculated throughout each facet joint surface, only the mean normal vector was used to determine the facet-based local coordinate system in the present study. Regional variation of the normal vector orientation could be used for analyses of curvature of the facet surface, which may be an important factor causing regional differences in cartilage degeneration via different loading conditions within a facet joint surface. Future studies will address contribution of the regional curvature variations to regional differences in facet joint degeneration.
Key Points
Facet joint space width is an important parameter in evaluating facet joint osteoarthritis.
Facet joint space width is larger in males than females; and it is also larger in asymptomatic subjects than symptomatic subjects.
First signs of facet joint narrowing occur as early as in the third decade.
Significant changes of facet joint space width occur in the joint periphery rather than in the joint center.
Acknowledgments
The manuscript submitted does not contain information about medical device(s)/drug(s). NIH National Institute on Arthritis and Musculoskeletal and Skin Diseases Grant (5P01 AR048152-10) funds were received in support of this work. One or more of the author(s) has/have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this manuscript: e.g., honoraria, gifts, consultancies.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
IRB-approved study (IRB Approval No. 00042801)
References
- 1.Adams MA, Hutton WC. The mechanical function of the lumbar apophyseal joints. Spine (Phila Pa 1976) 1983;8:327–330. doi: 10.1097/00007632-198304000-00017. [DOI] [PubMed] [Google Scholar]
- 2.Varlotta GP, Lefkowitz TR, Schweitzer M, et al. The lumbar facet joint: A review of current knowledge: Part 1: Anatomy, biomechanics, and grading. Skeletal Radiol. 2011;40:13–23. doi: 10.1007/s00256-010-0983-4. [DOI] [PubMed] [Google Scholar]
- 3.Panjabi MM, Oxland T, Takata K, et al. Articular facets of the human spine. quantitative three-dimensional anatomy. Spine (Phila Pa 1976) 1993;18:1298–1310. doi: 10.1097/00007632-199308000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Vernon-Roberts B, Pirie CJ. Degenerative changes in the intervertebral discs of the lumbar spine and their sequelae. Rheumatol Rehabil. 1977;16:13–21. doi: 10.1093/rheumatology/16.1.13. [DOI] [PubMed] [Google Scholar]
- 5.Boswell MV, Singh V, Staats PS, et al. Accuracy of precision diagnostic blocks in the diagnosis of chronic spinal pain of facet or zygapophysial joint origin. Pain Physician. 2003;6:449–456. [PubMed] [Google Scholar]
- 6.Buckland-Wright C. Subchondral bone changes in hand and knee osteoarthritis detected by radiography. Osteoarthritis Cartilage. 2004;12(A):S10–9. doi: 10.1016/j.joca.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Lynch JA, Buckland-Wright JC, Macfarlane DG. Precision of joint space width measurement in knee osteoarthritis from digital image analysis of high definition macroradiographs. Osteoarthritis Cartilage. 1993;1:209–218. doi: 10.1016/s1063-4584(05)80327-9. [DOI] [PubMed] [Google Scholar]
- 8.Pathria M, Sartoris DJ, Resnick D. Osteoarthritis of the facet joints: Accuracy of oblique radiographic assessment. Radiology. 1987;164:227–230. doi: 10.1148/radiology.164.1.3588910. [DOI] [PubMed] [Google Scholar]
- 9.Gries NC, Berlemann U, Moore RJ, et al. Early histologic changes in lower lumbar discs and facet joints and their correlation. Eur Spine J. 2000;9:23–29. doi: 10.1007/s005860050004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Masharawi Y, Rothschild B, Dar G, et al. Facet orientation in the thoracolumbar spine: Three-dimensional anatomic and biomechanical analysis. Spine (Phila Pa 1976) 2004;29:1755–1763. doi: 10.1097/01.brs.0000134575.04084.ef. [DOI] [PubMed] [Google Scholar]
- 11.Kalichman L, Suri P, Guermazi A, et al. Facet orientation and tropism: Associations with facet joint osteoarthritis and degeneratives. Spine (Phila Pa 1976) 2009;34:E579–85. doi: 10.1097/BRS.0b013e3181aa2acb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang J, Yang X. Age-related changes in the orientation of lumbar facet joints. Spine (Phila Pa 1976) 2009;34:E596–8. doi: 10.1097/BRS.0b013e3181abbf1e. [DOI] [PubMed] [Google Scholar]
- 13.Otsuka Y, An HS, Ochia RS, et al. In vivo measurement of lumbar facet joint area in asymptomatic and chronic low back pain subjects. Spine (Phila Pa 1976) 2010;35:924–928. doi: 10.1097/BRS.0b013e3181c9fc04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weishaupt D, Zanetti M, Boos N, et al. MR imaging and CT in osteoarthritis of the lumbar facet joints. Skeletal Radiol. 1999;28:215–219. doi: 10.1007/s002560050503. [DOI] [PubMed] [Google Scholar]
- 15.Kalichman L, Li L, Hunter DJ, et al. Association between computed tomography-evaluated lumbar lordosis and features of spinal degeneration, evaluated in supine position. Spine J. 2011;11:308–315. doi: 10.1016/j.spinee.2011.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Swanepoel MW, Adams LM, Smeathers JE. Human lumbar apophyseal joint damage and intervertebral disc degeneration. Ann Rheum Dis. 1995;54:182–188. doi: 10.1136/ard.54.3.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tischer T, Aktas T, Milz S, et al. Detailed pathological changes of human lumbar facet joints L1-L5 in elderly individuals. Eur Spine J. 2006;15:308–315. doi: 10.1007/s00586-005-0958-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang KH, An HS, Ochia R, et al. In vivo measurement changes in lumbar facet joint width during torsion. Trans Orthopaedic Research Society; In 51st Annual Meeting of the Orthopaedic Research Society; 2005; Washington, D.C.. p. 690. [Google Scholar]
- 19.Takatori R, An HS, Ochia RS, et al. Relationship between lumbar disc height and facet joint space width in asymptomatic and chronic low back pain subjects. Trans Orthopaedic Research Society; In 53rd Annual Meeting of the Orthopaedic Research Society; 2007; San Diego, CA. p. 426. [Google Scholar]
- 20.Sugisaki K, An HS, Espinoza Orias AA, et al. In vivo three-dimensional morphometric analysis of the lumbar pedicle isthmus. Spine (Phila Pa 1976) 2009;34:2599–2604. doi: 10.1097/BRS.0b013e3181b52a37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duan CY, Espinoza Orias AA, Shott S, et al. In vivo measurement of the subchondral bone thickness of lumbar facet joint using magnetic resonance imaging. Osteoarthritis Cartilage. 2011;19:96–102. doi: 10.1016/j.joca.2010.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Watanabe S, Inoue N, Yamaguchi T, et al. Three-dimensional kinematic analysis of the cervical spine after anterior cervical decompression and fusion at an adjacent level: A preliminary report. Eur Spine J. 2011 doi: 10.1007/s00586-011-2090-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abbas J, Hamoud K, Peleg S, et al. Facet joints arthrosis in normal and stenotic lumbar spines. Spine (Phila Pa 1976) 2011 doi: 10.1097/BRS.0b013e318210c889. [DOI] [PubMed] [Google Scholar]
- 24.Kunkel ME, Schmidt H, Wilke HJ. Prediction of the human thoracic and lumbar articular facet joint morphometry from radiographic images. J Anat. 2011;218:191–201. doi: 10.1111/j.1469-7580.2010.01323.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Espinoza Orias AA, Udayakumar R, An HS, et al. Three-dimensional characterization of segmental lumbar lordosis in healthy and low-back pain patients. Trans Orthopaedic Research Society; In 56th Annual Meeting of the Orthopaedic Research Society; 2010; New Orleans, LA. p. 1391. [Google Scholar]
- 26.Yukawa Y, Genda E. Contact stress of lumbar facet. Trans Orthopaedic Research Society; In 46th Annual Meeting of the Orthopaedic Research Society; 2000; Orlando, FL. p. 385. [Google Scholar]
- 27.Taylor JR, Twomey LT. Age changes in lumbar zygapophyseal joints. observations on structure and function. Spine (Phila Pa 1976) 1986;11:739–745. doi: 10.1097/00007632-198609000-00014. [DOI] [PubMed] [Google Scholar]
- 28.Fujiwara A, Lim TH, An HS, et al. The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine (Phila Pa 1976) 2000;25:3036–3044. doi: 10.1097/00007632-200012010-00011. [DOI] [PubMed] [Google Scholar]
- 29.Butler D, Trafimow JH, Andersson GB, et al. Discs degenerate before facets. Spine (Phila Pa 1976) 1990;15:111–113. doi: 10.1097/00007632-199002000-00012. [DOI] [PubMed] [Google Scholar]
- 30.Li J, Muehleman C, Abe Y, et al. Prevalence of facet joint degeneration in association with intervertebral joint degeneration in a sample of organ donors. J Orthop Res. 2011;29:1267–1274. doi: 10.1002/jor.21387. [DOI] [PMC free article] [PubMed] [Google Scholar]