…The gap between supply and demand for organs persists worldwide and consequently the quest to narrow this gap continues to explore issues that court controversy, rewards and compensation. Ghahramani et al.'s article provides an interesting additional medical professional's perspective dimension to the knowledge-base concerning rewards and compensation for kidney donation…
Keywords: donor, incentive, questionnaire, renal, survey, transplantation
Abstract
Background
Payment for organ donation, whether in the form of incentives, rewards or compensation is highly debated and has been denounced by many professional and legislative bodies. Despite the passionate discussion in the literature, there is very limited data on attitudes and perceptions of physicians about providing rewards or compensation to organ donors. We investigated the relationship between demographic and practice characteristics of nephrologists and their perceptions and attitudes about rewards and compensations for organ donation.
Methods
Using a web-based survey, we explored the views of nephrologists around the world about rewards and compensations for kidney donation. The relationship between attitudes and demographic characteristics of 1280 nephrologists from 74 countries was examined by univariate and multivariable analyses.
Results
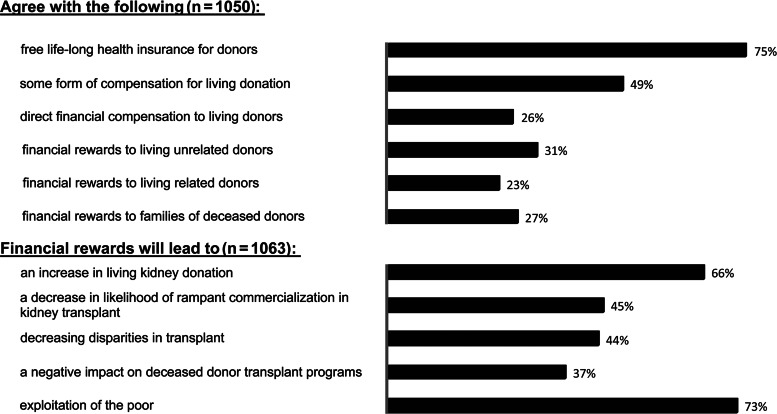
Seventy-five percent agreed with donor health insurance, 26% favored direct financial compensation and 31% agreed with financial rewards for unrelated donors. Sixty-six percent believed that rewards will lead to increased donation. Seventy-three percent indicated that rewards will lead to exploitation of the poor and 78% agreed with legislation prohibiting organ sales. Thirty-seven percent believed that rewards will negatively impact deceased-donor transplantation. Nephrologists from India/Pakistan and the Middle East had more favorable views about rewards, while respondents from Latin America and Europe, older than 50, female nephrologists and those practicing in rural areas had less favorable views.
Conclusions
We conclude that a minority of nephrologists favor rewards for donation, many agree with some compensation and a considerable majority favor donor health insurance. Perceptions of nephrologists about rewards and compensation are influenced by age, sex, urban versus rural location and geographic region of practice.
INTRODUCTION
The incidence of end-stage renal disease (ESRD) is increasing worldwide [1–3]. Compared with dialysis, renal transplantation is associated with a survival advantage and an improved quality of life for the majority of patients with ESRD [4]. Chronic maintenance dialysis is expensive for developed countries and the costs are prohibitive for most emerging economies [4]. In addition to its benefits for the individual patients, from a societal perspective, kidney transplantation is clearly the preferred cost-effective form of treatment for developing as well as developed countries [5, 6]. Although the multiple advantages and benefits of transplantation have been well recognized, there is a clear discrepancy between the number of transplants and the number of patients awaiting transplantation. This disparity has been mainly attributed to the gap between the supply of organs and the increasing prevalence of ESRD [7]. The consistent increase in the gap is expected to continue into the foreseeable future [8]. Therefore, in addition to the need for improvements in maximal utilization of organs from deceased donors, strategies to enhance living organ donation have become essential. Besides alleviating the gap between the supply and demand of organs, living donor transplants are associated with improved outcomes [9, 10], allowing for pre-emptive transplantation, which is associated with improved survival [11, 12]. With growing public awareness of the organ shortage crisis and the benefits of living donor transplants, there has been an increase in living kidney donation over the past decade [13]. Innovative schemes, such as paired kidney exchange, altruistic donation, donor chains and list exchange programs [14], have also contributed to increased living donor kidney transplants. As an increasing number of transplant programs are willing to consider genetically unrelated donor candidates, the number of living unrelated transplants has increased over the past several years. While, in 1986, only 16% of US transplant programs reported accepting unrelated donors, in 2007, all responding programs indicated that they would accept living unrelated donors [15, 16].
The subject of payment, whether in the form of incentives, rewards or compensation for living donation, is a highly controversial topic that has been debated among experts in the field of transplantation. Some authorities believe that any payment will have negative consequences leading to commercialization and would undermine transplant efforts [17–19]. Others have suggested that providing incentives or removing disincentives for organ donation will lead to an increase in organ donation [20–24]. There has also been significant debate surrounding the option of a regulated system of incentives for donation [17, 18, 21, 24–30]. Despite the passionate debate in the medical and bioethics literature, there is very limited data on attitudes and perceptions of physicians about providing rewards or compensation to organ donors [19]. The objective of the present study was to use an international survey to investigate the relationship between demographic and practice characteristics of nephrologists and their perceptions and attitudes toward rewards and compensations for living donation.
MATERIALS AND METHODS
The study design and methods of the International Survey of Physician's Opinion on Renal Transplantation (ISPORT) have been previously described [31]. ISPORT was devised as a comprehensive questionnaire intended to study the perceptions of nephrologists about various aspects of kidney transplantation. Items for the questionnaire were generated through a review of the literature and discussions among investigators. The Institutional Review Board of Penn State College of Medicine approved the research protocol and the survey instrument. The survey was pilot tested by sending a preliminary version via e-mail to a multinational group of 18 nephrologists and 6 nephrology fellows from three nephrology training programs in the USA. We modified the survey instrument based on the comments from this group about the clarity, format and content of the questionnaire. The final questionnaire consisted of 50 items, 20 of which related to opinions of the respondent about donor rewards and compensation. Using an online search method and also lists provided by some national and regional societies of nephrology, we developed a database of 7324 unique e-mail addresses of presumed nephrologists, worldwide [31]. We sent the survey link to these e-mail addresses, followed by two reminder e-mails (2 and 4 weeks after the initial invitation).
For the purpose of the present study, we analyzed the association between demographic factors and responses to items relating to the opinions of physicians about financial rewards and compensations for living donation. For the univariate and multiple logistic regression models, ‘strongly agree/strongly approve’ and ‘agree/approve’ categories of responses from the five-level Likert scale questions were collapsed into a single category, ‘agree/approve’.
The regression model included age, sex, number of years in practice, percent clinical activity, status as transplant nephrologist, academic affiliation, number of transplants performed at the hospital, rural location, geographic region and predominant religion of the respondent's country of practice. Univariate unadjusted logistic regressions of dependent variables were conducted for each independent variable. Significant variables were entered in a stepwise fashion into the final logistic regression model if P < 0.05 and were removed if P > 0.1. Age, sex, rural location, geographic region and predominant religion of the respondent's country of practice were forced into the model independent of the threshold. Odds ratio (OR) and 95% confidence interval (CI) were computed for significant variables.
Reference groups for logistic regression were as follows: age ≤50, male sex, non-transplant nephrologist, urban/suburban location of practice, residence in the Canada/US region and Protestant religion. Outcomes were expressed as unadjusted and adjusted OR and 95% CI. Statistical analyses were performed using MedCalc for Windows, Version 12.3.0.0 (MedCalc Software, Mariakerke, Belgium).
RESULTS
Of the 7324 e-mail invitations, 2856 were undeliverable; 1448 of the 4468 e-mail recipients (response rate of 19.8%) completed the survey. Excluding 168 respondents who indicated that they did not practice any clinical nephrology, we analyzed a total of 1280 responses. Table 1 shows the demographic and practice characteristics of the respondents. The majority of respondents were 50 years of age or younger, male, had more than 10 years of clinical experience, with more than 50% clinical activity, were affiliated with an academic medical center and worked in an urban/suburban setting. Half of the respondents identified themselves as transplant nephrologists. Thirty-seven percent stated that kidney transplantation is performed at the hospital in which they practice, and 51% noted that at least 50 kidney transplants had been performed at their hospital during the previous year. Ninety-five percent of the respondents identified 74 countries within nine geographic regions as their country of practice. The largest proportion of respondents (33%) was from the Canada/US region. Ninety percent indicated that they would donate a kidney to a first degree relative in the event of need and 82% noted that they have consented for deceased organ donation. Associations between respondent characteristics and responses are outlined in Tables 2–4 and the results of the multivariate analyses are detailed below.
Table 1.
Characteristics of respondents
| Characteristic | Number | Percent |
|---|---|---|
| Age (n = 1280) | ||
| ≤50 | 773 | 60 |
| >50 | 507 | 40 |
| Sex (n = 1280) | ||
| Male | 926 | 72 |
| Female | 354 | 28 |
| Years of practice (n = 1266) | ||
| ≤10 | 506 | 40 |
| >10 | 760 | 60 |
| Clinical activity (n = 1259) | ||
| ≤50% | 367 | 29 |
| >50% | 892 | 71 |
| Transplant nephrologist (n = 1267) | ||
| Yes | 643 | 51 |
| No | 624 | 49 |
| Academic affiliation (n = 1268) | ||
| Yes | 805 | 63 |
| No | 463 | 37 |
| Number of transplants performed in the hospital (n = 924) | ||
| <50 per year | 457 | 49 |
| ≥50 per year | 467 | 51 |
| Location of practice (n = 1280) | ||
| Urban/suburban | 1138 | 89 |
| Rural | 142 | 11 |
| Geographic region (n = 1280) | ||
| Eastern Asia | 90 | 7 |
| Australia | 38 | 3 |
| India/Pakistan | 90 | 7 |
| Middle East | 102 | 8 |
| Africa | 64 | 5 |
| Eastern Europe | 51 | 4 |
| Western Europe | 179 | 14 |
| Latin America | 179 | 14 |
| Canada/USA | 422 | 33 |
| Unknown | 65 | 5 |
| Predominant religion of the respondent's country (n = 1280) | ||
| Protestant | 525 | 41 |
| Catholic | 371 | 29 |
| Moslem | 141 | 11 |
| Other/unknown | 243 | 19 |
Table 2.
Logistic regression of respondent characteristics and attitudes toward compensation for living donation
| Characteristic | Favor donor health insurance |
Favor some form of compensation |
Favor direct financial compensation |
|||
|---|---|---|---|---|---|---|
| OR (95% CI) | Adjusted OR(95% CI) | OR (95% CI) | Adjusted OR(95% CI) | OR (95% CI) | Adjusted OR(95% CI) | |
| Age | ||||||
| >50 | 1.16 (0.87–1.54) | 1.24 (0.92–1.67) | 0.82* (0.62–0.99) | 0.83 (0.64–1.08) | 0.75* (0.56–0.99) | 0.76 (0.57–1.02) |
| ≤50 | Reference | Reference | Reference | Reference | Reference | Reference |
| Sex | ||||||
| Female | 0.71* (0.52–0.97) | 0.74 (0.54–1.02) | 0.68* (0.50–0.92) | 0.76 (0.58–1.01) | 0.83 (0.60–1.15) | 0.76 (0.54–1.07) |
| Male | Reference | Reference | Reference | Reference | Reference | Reference |
| Rural location of practice | ||||||
| Yes | 1.12 (0.71–1.75) | 1.35 (0.83–2.18) | 0.62* (0.41–0.94) | 0.80 (0.55–1.17) | 0.48** (0.29–0.80) | 0.50* (0.29–0.86) |
| No | Reference | Reference | Reference | Reference | Reference | Reference |
| Geographic region | ||||||
| Latin America | 0.69 (0.46–1.04) | 0.71 (0.46–1.08) | 0.24** (0.15–0.37) | 0.18** (0.10–0.33) | 0.50** (0.30–0.83) | 0.43** (0.25–0.73) |
| Eastern Asia | 1.01 (0.55–1.86) | 1.05 (0.57–1.96) | 1.02 (0.60–1.76) | 0.87 (0.45–1.67) | 1.58 (0.90–2.78) | 0.94 (0.48–1.85) |
| Australia | 0.63 (0.30–1.32) | 0.65 (0.30–1.38) | 0.74 (0.36–1.52) | 0.67 (0.33–1.40) | 1.24 (0.57–2.70) | 1.17 (0.53–2.56) |
| India/Pakistan | 6.78** (2.08–22.08) | 6.40** (1.81–22.65) | 0.99 (0.58–1.74) | 0.92 (0.47–1.81) | 1.60 (0.90–2.84) | 0.93 (0.46–1.89) |
| Middle East | 1.38 (0.75–2.53) | 1.47 (0.79–2.72) | 3.07** (1.69–5.59) | 2.22 (0.98–5.03) | 2.58** (1.55–4.31) | 2.38** (1.41–4.04) |
| Africa | 3.39* (1.32–8.74) | 3.54** (1.36–9.21) | 1.58 (0.85–2.92) | 1.10 (0.52–2.33) | 1.41 (0.76–2.62) | 1.02 (0.47–2.21) |
| Eastern Europe | 3.30* (1.15–9.47) | 3.46* (1.19–10.01) | 0.42* (0.21–0.84) | 0.40* (0.19–0.86) | 0.94 (0.45–1.99) | 0.52 (0.23–1.19) |
| Western Europe | 1.30 (0.84–2.04) | 1.37 (0.86–2.18) | 0.45** (0.31–0.66) | 0.37** (0.23–0.61) | 0.42** (0.25–0.71) | 0.24** (0.13–0.46) |
| Canada/USA | Reference | Reference | Reference | Reference | Reference | Reference |
| Predominant religion of the respondent's country | ||||||
| Catholic | 1.11 (0.80–1.54) | 1.04 (0.72–1.51) | 0.47** (0.35–0.63) | 1.17 (0.72–1.91) | 0.86 (0.60–1.24) | 0.92 (0.62–1.37) |
| Moslem | 2.28** (1.31–3.96) | 2.11 (0.85–5.27) | 2.46** (1.56–3.86) | 1.43 (0.70–2.92) | 2.24** (1.45–3.46) | 1.41 (0.68–2.93) |
| Other | 1.55* (1.03–2.32) | 0.97 (0.57–1.64) | 0.91 (0.65–1.27) | 0.84 (0.52–1.36) | 1.89** (1.31–2.72) | 1.72 (.99–2.92) |
| Protestant | Reference | Reference | Reference | Reference | Reference | Reference |
| Good fit by Hosmer–Lemeshow testing | P = 0.63 | P = 0.76 | P = 0.016 | |||
*P < 0.05; **P ≤ 0.01.
Table 3.
Logistic regression of respondent characteristics and attitudes toward compensation for living donation
| Characteristic | Favor financial rewards to living-unrelated donors |
Favor financial rewards to living related donors |
Favor financial rewards to families of deceased donors |
|||
|---|---|---|---|---|---|---|
| OR (95% CI) | Adjusted OR(95% CI) | OR (95% CI) | Adjusted OR(95% CI) | OR (95% CI) | Adjusted OR(95% CI) | |
| Age | ||||||
| >50 | 0.69** (0.53–0.91) | 0.71* (0.53–0.94) | 0.81 (0.60–1.089) | 0.81 (0.60–1.10) | 0.74* (0.56–0.97) | 0.71* (0.53–0.96) |
| ≤50 | Reference | Reference | Reference | Reference | Reference | Reference |
| Sex | ||||||
| Female | 0.82 (0.61–1.11) | 0.79 (0.57–1.09) | 0.85 (0.61–1.18) | 0.82 (0.58–1.17) | 0.71* (0.52–0.98) | 0.71* (0.51–0.98) |
| Male | Reference | Reference | Reference | Reference | Reference | Reference |
| Transplant nephrologist | ||||||
| Yes | 1.29 (0.99–1.67) | 1.11 (0.84–1.48) | 1.40* (1.05–1.87) | 1.30 (0.98–1.93) | 1.46** (1.16–2.00) | 1.32 (0.98–1.82) |
| No | Reference | Reference | Reference | Reference | Reference | Reference |
| Rural location of practice | ||||||
| Yes | 0.48** (0.30–0.78) | 0.46** (0.28–0.76) | 0.78 (0.48–1.26) | 0.69 (0.42–1.15) | 0.53** (0.32–0.86) | 0.44** (0.26–0.75) |
| No | Reference | Reference | Reference | Reference | Reference | Reference |
| Geographic region | ||||||
| Latin America | 0.45** (0.28–0.74) | 0.35** (0.18–0.70) | 0.33** (0.18–0.60) | 0.23** (0.11–0.50) | 0.42** (0.25–0.71) | 0.63 (0.29–1.33) |
| Eastern Asia | 1.59 (0.92–2.76) | 1.36 (0.70–2.63) | 1.33 (0.74–2.39) | 1.24 (0.61–2.50) | 1.76* (1.02–3.06) | 1.74 (0.89–3.44) |
| Australia | 0.74 (0.33–1.69) | 0.67 (0.29–1.55) | 1.13 (0.51–2.50) | 1.04 (0.46–2.35) | 0.46 (0.17–1.21) | 0.36* (0.14–0.97) |
| India/Pakistan | 2.94** (1.69–5.13) | 2.26* (1.13–4.53) | 1.44 (0.80–2.59) | 1.18 (0.56–2.48) | 3.26** (1.87–5.69) | 2.43* (1.20–4.92) |
| Middle East | 4.03** (2.40–6.76) | 4.23** (1.95–9.20) | 1.50 (0.89–2.53) | 1.68 (0.75–3.80) | 2.40** (1.46–3.97) | 2.24* (1.04–4.83) |
| Africa | 1.64 (0.91–2.93) | 1.58 (0.76–3.27) | 0.79 (0.39–1.59) | 0.80 (0.35–1.84) | 1.10 (0.59–2.04) | 0.98 (0.46–2.11) |
| Eastern Europe | 0.70 (0.33–1.46) | 0.53 (0.24–1.20) | 0.58 (0.25–1.33) | 0.49 (0.19–1.22) | 0.67 (0.31–1.45) | 0.64 (0.27–1.51) |
| Western Europe | 0.32** (0.19–0.55) | 0.26** (0.14–0.49) | 0.36** (0.21–0.63) | 0.23** (0.14–0.53) | 0.25** (0.14–0.45) | 0.27** (0.14–0.55) |
| Canada/USA | Reference | Reference | Reference | Reference | Reference | Reference |
| Predominant religion of the respondent's country | ||||||
| Catholic | 0.62** (0.44–0.88) | 1.13 (0.65–1.96) | 0.57** (0.39–0.84) | 1.31 (0.73–2.33) | 0.44** (0.30–0.65) | 0.52* (0.28–0.96) |
| Moslem | 2.58** (1.70–3.90) | 0.78 (0.38–1.58) | 1.19 (0.75–1.89) | 0.72 (0.33–1.58) | 1.97** (1.29–3.00) | 0.78 (0.38–1.61) |
| Other | 1.91** (1.35–2.71) | 1.15 (0.70–1.89) | 1.23 (0.85–1.80) | 1.00 (0.58–1.71) | 1.81** (1.27–2.57) | 0.94 (0.56–1.57) |
| Protestant | Reference | Reference | Reference | Reference | Reference | Reference |
| Good fit by Hosmer–Lemeshow testing | P = 0.81 | P = 0.64 | P = 0.80 | |||
*P < 0.05; **P ≤ 0.01.
Table 4.
Logistic regression of respondent characteristics and favoring legislation banning organ sales
| Characteristic | OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|
| Age | ||
| >50 | 1.67** (1.23–2.28) | 1.61** (1.17–2.22) |
| ≤50 | Reference | Reference |
| Sex | ||
| Female | 0.89 (0.64–1.24) | 0.98 (0.70–1.39) |
| Male | Reference | Reference |
| Rural location of practice | ||
| Yes | 1.40 (0.85–2.29) | 1.13 (0.66–1.91) |
| No | Reference | Reference |
| Geographic region | ||
| Latin America | 0.46** (0.30–0.70) | 0.58 (0.30–1.14) |
| Eastern Asia | 0.67 (0.36–1.26 | 0.68 (0.36–1.30) |
| Australia | 1.60 (0.55–4.68) | 1.60 (0.54–4.74) |
| India/Pakistan | 0.94 (0.46–1.88) | 1.19 (0.52–2.74) |
| Middle East | 0.29** (0.17–0.49) | 0.38* (0.17–0.87) |
| Africa | 0.81 (0.40–1.65) | 0.83 (0.40–1.73) |
| Eastern Europe | 0.76 (0.35–1.66 | 0.78 (0.35–1.74) |
| Western Europe | 1.46 (0.85–2.49) | 1.42 (0.81–2.47) |
| Canada/USA | Reference | Reference |
| Predominant religion of the respondent's country | ||
| Catholic | 0.60** (0.42–0.87) | 0.77 (0.42–1.42) |
| Moslem | 0.39** (0.25–0.62) | 0.76 (0.34–1.70) |
| Other | 0.69 (0.45–1.05) | 0.82 (0.46–1.47) |
| Protestant | Reference | Reference |
| Good fit by Hosmer–Lemeshow testing | P = 0.87 | |
*P < 0.05; **P ≤ 0.01.
Health insurance for donors
Thirty-seven percent of the respondents agreed with the provision of free life-long health insurance to donors (Figure 1; Table 2). Nephrologists from India/Pakistan (OR: 6.40; 95% CI: 1.81–22.65; P < 0.01), Africa (OR: 3.54; 95% CI: 1.36–9.21; P < 0.01) and Eastern Europe (OR: 3.46; 95% CI: 1.19–10.01, P < 0.05) were more likely to agree with health insurance for donors.
FIGURE 1:
Attitudes toward compensation and rewards for organ donation and perceptions about the effects of financial rewards. Top panel: percentage of nephrologists who agree with statements about providing compensation and rewards to living donors or to families of deceased donors. Lower panel: percentage of nephrologists who agree with the statements about the effects of financial rewards on living organ donation. The first three bars indicate positive perceptions, the lower two bars indicate negative perceptions about financial rewards.
Compensation for donation
Forty-nine percent of the participants agreed with some form of compensation, and 26% agreed with direct financial compensation for living donors (Figure 1; Table 2). Respondents from Latin America (OR: 0.18; 95% CI: 0.10–0.33; P < 0.01), Eastern Europe (OR: 0.40; 95% CI: 0.19–0.86; P < 0.05) and Western Europe (OR: 0.37; 95% CI: 0.23–0.61; P < 0.01) were less likely to agree with any form of compensation for living donation. Respondents from the Middle East (OR: 2.38; 95% CI: 1.41–4.04; P < 0.01) were more likely, while those from Latin America (OR: 0.43; 95% CI: 0.25–0.73; P < 0.01) and Western Europe (OR: 0.24; 95% CI: 0.13–0.46; P < 0.01) and nephrologists practicing in rural locations (OR: 0.50; 95% CI: 0.29–0.86; P < 0.05) were less likely to favor direct financial compensation for living donation.
Financial rewards to living donors
Thirty-one percent of the respondents believed that living-unrelated donors should receive financial rewards, while 23% favored rewards to related donors (Figure 1; Table 3). Respondents from the Middle East (OR: 4.23; 95% CI: 1.95–9.20; P < 0.01) and India/Pakistan (OR: 2.26; 95% CI: 1.13–4.53; P < 0.05) were more likely, while nephrologists from Latin America (OR: 0.35; 95% CI: 0.18–0.70; P < 0.01) and Western Europe (OR: 0.26; 95% CI: 0.14–0.49; P < 0.01) and nephrologists older than 50 years of age (OR: 0.71; 95% CI: 0.53–0.94; P < 0.05) and those practicing in a rural setting (OR: 0.46; 95% CI: 0.28–0.76; P < 0.01) were less likely to agree with financial rewards to living-unrelated donors. Physicians from Latin America (OR: 0.23; 95% CI: 0.11–0.50; P < 0.01) and Western Europe (OR: 0.23; 95% CI: 0.14–0.53; P < 0.01) were less likely to agree with financial rewards for living-related donors.
Financial rewards for families of deceased donors
Twenty-seven percent were in favor of financial rewards for families of deceased donors (Figure 1; Table 3). Respondents from India/Pakistan (OR: 2.43; 95% CI: 1.20–4.92; P < 0.05) and the Middle East (OR: 2.24; 95% CI: 1.04–4.83; P < 0.05) were more likely, while nephrologists from Australia (OR: 0.36; 95% CI: 0.14–0.97; P < 0.05) and Western Europe (OR: 0.27; 95% CI: 0.14–0.55; P < 0.01), those older than 50 years of age (OR: 0.71; 95% CI: 0.53–0.96; P < 0.05), female nephrologists (OR: 0.71; 95% CI: 0.51–0.98; P < 0.05) and those practicing in a rural setting (OR: 0.44; 95% CI: 0.26–0.75; P < 0.01) were less likely to agree with providing financial rewards to families of deceased donors. In a post hoc analysis of the association between the predominant religion of the respondents' country and the responses, respondents from predominantly Catholic countries were less likely to agree with rewards to families of deceased donors (OR: 0.52; 95% CI: 0.28–0.96; P < 0.05).
Perceptions about the effects of financial rewards for living organ donation
Sixty-six percent believed that financial rewards for living organ donation will lead to an increase in living kidney donation, 45% felt that it will lead to a decrease in the likelihood of rampant commercialization and a similar proportion (44%) believed that it will lead to decreasing disparities in transplantation (Figure 1). Thirty-seven percent of the nephrologists believed that financial rewards will have a negative impact on deceased-donor organ transplantation programs and the majority (73%) were concerned that rewards will lead to exploitation of the poor. Forty-seven percent (504) agreed with both statements that ‘financial rewards for living organ donation will lead to an increase in living kidney donation’ and ‘financial rewards for living organ donation will lead to exploitation of the poor’.
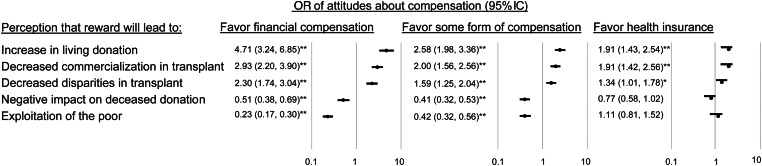
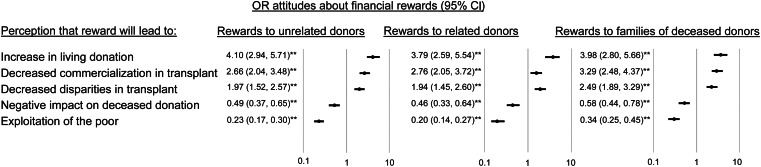
Association between perceptions about the effects of rewards and attitudes about donor compensation and rewards
Respondents who perceived that rewards will lead to an increase in living donation, decreased commercialization in transplantation and decreased disparities in transplantation were more likely to have favorable views about providing compensation, health insurance and rewards to the living donor and to families of deceased donors (Figures 2 and 3). Perceptions that providing rewards will have a negative impact on deceased donation or that it will lead to exploitation of the poor were associated with unfavorable attitudes toward financial compensation and rewards to the living donors or to families of deceased donors.
FIGURE 2:
Association between perceptions of the effect of rewards and attitudes toward compensation and health insurance for living donors. OR of attitudes favoring financial compensation, some form of compensation and donor health insurance as related to perceptions about the effects of providing rewards to the donors. The top three rows indicate positive perceptions and the lower two rows indicate negative perceptions about the effect of rewards (data shown as OR, 95% CI; *P < 0.05; **P ≤ 0.01).
FIGURE 3:
Association between perceptions of the effect of rewards and attitudes toward financial rewards for organ donation. OR of attitudes favoring rewards to living donors and families of deceased donors as related to perceptions about the effects of providing rewards to the donors. The top three rows indicate positive perceptions and the lower two rows indicate negative perceptions about the effect of rewards (data shown as OR, 95% CI; *P < 0.05; **P ≤ 0.01).
Opinions about legislation banning organ sales
From 1050 respondents to the question about legislation banning organ sales, 819 (78%) agreed with such legislation (Table 4). Age >50 was associated with a higher likelihood (OR: 1.61; 95% CI: 1.17–2.22; P < 0.01), while practice in the Middle East was associated with a lower likelihood (OR: 0.38; 95% CI: 0.17–0.87; P < 0.05) of agreement with such legislation.
DISCUSSION
In this study, we used an international online survey to evaluate the opinions of nephrologists about rewards and compensation for kidney donation. We found that while 75% of nephrologists favored provision of health insurance to donors, and nearly half agreed with some form of compensation, only a minority agreed with financial rewards or compensation for organ donation.
One of the concerns of transplant candidates pursuing living donor kidney transplant is the potential financial impact on the donor [32]. For the donor, the decision to donate entails an intricate process involving conscious and subconscious calculations about the risks and benefits to self and others. Financial concerns are likely tangible components of this process. Kidney donors face direct and indirect, expected and unexpected costs and negative financial consequences related to donation [33–35]. Among the financial concerns, the ability to obtain or maintain health insurance following donation has been identified as a source of stress among 11–14% of donors in the USA, Japan, Germany and Canada [33, 36–38]. In a study of 10 021 living kidney donors in the USA, 18% were uninsured; among the younger sub-group (18–34 years), the proportion of uninsured donors was even higher (26.2%) [39]. In a survey of US transplant programs, 42% considered lack of donor health insurance as a relative contraindication for donation and 15% indicated that they will not accept donor candidates without health insurance [40]. Taking into consideration the concerns of the donors about future insurability and the emphasis of the transplant professionals on the clear need for donor follow-up [41–43], the finding in our study that the vast majority of nephrologists favor donor health insurance is not surprising. In multivariate analysis, the geographic region of practice was the only variable independently associated with favoring donor health insurance. The finding is likely reflective of national and regional differences in factors such as the existence or lack of universal health insurance, as well as differences in the relative cost (i.e. ‘value’) of healthcare. However, in the absence of a detailed study of existing healthcare and insurance infrastructure in the individual countries, it is difficult to arrive at firm conclusions about the significance of this finding.
In multivariate analysis, there was a significant geographic difference in attitudes toward rewards and compensation for organ donation. Respondents from Latin America and Europe were less likely to agree with providing compensation or financial rewards for living donation, while those from the Middle East were more likely to agree with direct financial compensation for living donation, financial rewards to living unrelated donors and to families of deceased donors. Nephrologists from India/Pakistan were also more likely to agree with financial rewards to living-unrelated donors and to families of deceased donors. The findings relating to the influence of geographic factors on physician's attitudes might be explained by acceptance of current local practices, as well as a multitude of other cultural and socioeconomic variables present in each region.
Practice in rural areas was associated with the decreased likelihood of approval of direct financial compensation, rewards for living-unrelated donation and rewards to families of deceased donors. We are not aware of any studies that have explored the influence of practice location on physicians' expectation of altruism; however, urban dwellers, in general, have been shown to be less willing to contribute altruistically than those in rural areas [44]. It might be hypothesized that practice in rural areas will influence physicians' attitudes and expectations. Just as physicians influence attitudes of their patients, it is very likely that their own attitudes and perceptions are at least partially influenced and even shaped by the beliefs and expectations of the community within which they practice. It is also possible that nephrologists practicing in rural areas are less inclined to be advocates of transplantation, partially due to concerns about loss of involvement in care [45]. We have previously demonstrated that rural nephrologists have an overall less likelihood of recommending transplantation [31].
During the past two decades, countries commonly known as exporters of organs, such as India and Pakistan, have enacted legislation aimed at curtailing transplant tourism by prohibiting organ sales [19, 46–48]. Although necessary, these legislations are deemed as insufficient. Issues relating to organ sales and transplant tourism cross national borders, and to reduce exploitation of the poor in these countries, strict enforcement and consistent global monitoring are required [47]. In our study, a significant majority of the respondents agreed with legislation prohibiting organ sales. Nephrologists older than 50 were more likely to agree with legislation banning sale of organs, and those practicing in the Middle East were less likely to agree with such legislation.
A majority of the nephrologists felt that financial rewards will lead to an increase in kidney donation. Nearly half perceived it to lead to a decrease in commercialization and disparities in transplantation. A significant majority were concerned that financial rewards would lead to exploitation of the poor. It is interesting that 47% of the respondents agreed with the statement that financial rewards will lead to an increase in living kidney donation, at the same time, acknowledging concerns that it will lead to exploitation of the poor. These findings mirror the controversy in the literature regarding incentivized organ donation. While some authorities have suggested that incentives will increase living donation and will curtail rampant commercialization, others are concerned that they will lead to coercion and exploitation of the poor [17, 21, 49–53].
While the healthcare providers' religious beliefs, personal values and moral attitudes are felt to play a major role in perceptions and clinical decision-making, most of the literature is limited to issues relating to end-of-life [54, 55], abortion [56] and euthanasia [57]. In areas of moral controversy, many physicians face challenges about their obligations. The more religious physicians are more likely to believe that they are never professionally obligated to do what they personally believe is wrong [58, 59]. In the field of organ transplantation, when providers believe that their religion favors donation, there is a positive effect on attitudes toward donation compared with those who believe that their religion is not in favor of living donation [60]. In our study, the significant geographic variation in opinions of nephrologists regarding rewards and compensation for organ donation was highly suggestive of the impact of socio-cultural factors on perceptions. One such potential factor which was considered in the post hoc analysis was religion. Since no data were available about the individual respondents' religion, we considered the dominant religion of the respondent's country. While a significant variable in univariate unadjusted analysis, in multivariate analysis, religion was only independently associated with the likelihood of agreement with providing financial rewards to families of deceased donors. Respondents from predominantly Catholic countries were less likely to agree with rewards to families of deceased donors. This is congruent with official Catholic view on transplantation which specifically considers commercialization of human organs as items of exchange or trade as morally unacceptable [61].
Some have expressed concerns that active incentivized living kidney donation will hinder development and expansion of deceased-donor transplantation and, particularly, have a negative impact on non-renal solid organ transplantation [62]. We have previously presented evidence that confirms this notion [48]. In the present study, 37% of the nephrologists indicated that providing financial rewards for organ donation will have a negative impact on deceased-donor organ transplantation.
The major limitation of our study is respondent bias. A large number of e-mails returned as being undeliverable. Possible reasons for an undeliverable e-mail are incorrect or outdated e-mail address. Although there is no reliable way to determine the characteristics of the intended recipients of undeliverable invitations, considering inter-institution mobility of professionals, we suspect that a significant number of undeliverable addresses are due to outdated institutional e-mail addresses. Since the final list of e-mail addresses is a compilation from various overlapping sources, it is likely that a respondent with an undeliverable address actually participated in the study through a more current e-mail address. Furthermore, the denominator (potential respondents) is unknown. There is no single universal reliable source for the total number of clinical nephrologists. The International Society of Nephrology (ISN) [63] has a membership of ∼9000 [64]; however, the ISN membership includes basic scientists, fellows-in-training and non-nephrologists. Also, not all nephrologists worldwide are members of the ISN or national nephrology societies. A lack of reliable information regarding the denominator (potential respondents) adds to the challenge of an accurate calculation of the response rate in studies such as ours [65]. Acknowledging the difficulty in making assumptions about eligibility or interest in participation based upon the number of respondents, we considered all intended recipients of undeliverable messages as potentially eligible non-responders. Using this conservative approach, our response rate is 19.8%, which is within the previously reported range of 11–52% for internet surveys of healthcare providers [66, 67]. The web-based nature of the survey excluded respondents without access to the internet, resulting in sampling a less representative group of nephrologists. Furthermore, using publications as one of the sources for e-mail addresses of nephrologists is likely to have led to an over-sampling of nephrologists with academic affiliation as evident in Table 1, which shows that 63% of the respondents practiced in an academic setting. Similarly, the subject heading of the invitation e-mail, which included the term ‘transplantation’, appears to have preferentially attracted transplant nephrologists. Other limitations include the self-declared definitions of some of the categories (‘transplant nephrologist’ and ‘rural location’), ambiguity of some terms used in the questionnaire (‘reward’ and ‘compensation’) and collapsing the response categories from the five-level scale to two categories. While collapsing provides a more straightforward look at the data, it is potentially associated with loss of information. Finally, in our post hoc analysis of religion as an independent variable, we considered the dominant religion of the respondent's country. While the pivotal role of the dominant religion as a foundation for ethical conduct has precedence in the literature [68], more detailed information about individual respondents' religious affiliations would allow for more accurate analysis of the impact of this variable. The main strength of the study is the inclusion of a large number of participants with diverse practice patterns from over 70 countries. The sample includes transplant and general nephrologists, academic and private nephrologists, nephrologists practicing in rural and urban settings and throughout the world. The diversity in practice patterns and demographic characteristics allows for detailed sub-group analyses of various factors with the dependent variables [31].
In conclusion, while only a minority of nephrologists favors financial rewards for donation, many agree with some form of compensation and a considerable majority favors provision of health insurance to donors. A vast majority of nephrologists are concerned that financial rewards will lead to exploitation of the poor and agree with legislation prohibiting organ sales. Many nephrologists believe that financial rewards will have a negative impact on deceased-donor organ transplantation. Attitudes about rewards and compensation are influenced by age, sex, rural versus urban location and geographic region of practice. Possible areas for future study include the association between attitudes toward donor rewards and regional differences in healthcare costs, and the influence of provider beliefs and religious affiliations on these attitudes. The hypothesis of the bidirectional nature of community—physician influence on perceptions also requires further research.
CONFLICT OF INTEREST STATEMENT
None declared.
See related article by Randhawa. Policy perspectives: international survey of nephrologists’ perceptions of and attitudes towards rewards and compensation for kidney donation. Nephrol Dial Transplant 2013; 28: 1343–1345.)
ACKNOWLEDGEMENTS
N. G. is supported by Award Number K23DK084300 from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health.
REFERENCES
- 1.White SL, Chadban SJ, Jan S, et al. How can we achieve global equity in provision of renal replacement therapy? Bull World Health Organ. 2008;86:229–237. doi: 10.2471/BLT.07.041715. doi:10.2471/BLT.07.041715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang L, Wang H. Chronic kidney disease epidemic: cost and health care implications in China. Semin Nephrol. 2009;29:483–486. doi: 10.1016/j.semnephrol.2009.06.012. doi:10.1016/j.semnephrol.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 3.Agarwal SK, Srivastava RK. Chronic kidney disease in India: challenges and solutions. Nephron Clin Pract. 2009;111:c197–c203. doi: 10.1159/000199460. discussion c doi:10.1159/000199460. [DOI] [PubMed] [Google Scholar]
- 4.Garcia GG, Harden P, Chapman J. The global role of kidney transplantation. Lancet. 2012;379:e36–e38. doi: 10.1016/S0140-6736(12)60202-5. doi:10.1016/S0140-6736(12)60202-5. [DOI] [PubMed] [Google Scholar]
- 5.Perovic S, Jankovic S. Renal transplantation vs hemodialysis: cost-effectiveness analysis. Vojnosanit Pregl. 2009;66:639–644. doi: 10.2298/vsp0908639p. doi:10.2298/VSP0908639P. [DOI] [PubMed] [Google Scholar]
- 6.Wong G, Howard K, Chapman JR, et al. Comparative survival and economic benefits of deceased donor kidney transplantation and dialysis in people with varying ages and co-morbidities. PLoS One. 2012;7:e29591. doi: 10.1371/journal.pone.0029591. doi:10.1371/journal.pone.0029591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wynn JJ, Alexander CE. Increasing organ donation and transplantation: the U.S. experience over the past decade. Transpl Int. 2011;24:324–332. doi: 10.1111/j.1432-2277.2010.01201.x. doi:10.1111/j.1432-2277.2010.01201.x. [DOI] [PubMed] [Google Scholar]
- 8.Spasovski G, Vanholder R. Kidney transplantation in emerging countries: do we know all issues? Minerva Urol Nefrol. 2012;64:183–189. [PubMed] [Google Scholar]
- 9.Lee S, Kim J, Shin M, et al. Comparison of outcomes of living and deceased donor kidney grafts surviving longer than 5 years in Korea. Transplant Proc. 2010;42:775–777. doi: 10.1016/j.transproceed.2010.02.032. doi:10.1016/j.transproceed.2010.02.032. [DOI] [PubMed] [Google Scholar]
- 10.Suzuki A, Kenmochi T, Maruyama M, et al. Changes in quality of life in deceased versus living-donor kidney transplantations. Transplant Proc. 2012;44:287–289. doi: 10.1016/j.transproceed.2011.11.056. doi:10.1016/j.transproceed.2011.11.056. [DOI] [PubMed] [Google Scholar]
- 11.Meier-Kriesche HU, Port FK, Ojo AO, et al. Effect of waiting time on renal transplant outcome. Kidney Int. 2000;58:1311–1317. doi: 10.1046/j.1523-1755.2000.00287.x. doi:10.1046/j.1523-1755.2000.00287.x. [DOI] [PubMed] [Google Scholar]
- 12.Kasiske BL, Snyder JJ, Matas AJ, et al. Preemptive kidney transplantation: the advantage and the advantaged. J Am Soc Nephrol. 2002;13:1358–1364. doi: 10.1097/01.asn.0000013295.11876.c9. doi:10.1097/01.ASN.0000013295.11876.C9. [DOI] [PubMed] [Google Scholar]
- 13.Klein AS, Messersmith EE, Ratner LE, et al. Organ donation and utilization in the United States, 1999–2008. Am J Transplant. 2010;10:973–986. doi: 10.1111/j.1600-6143.2009.03008.x. doi:10.1111/j.1600-6143.2009.03008.x. [DOI] [PubMed] [Google Scholar]
- 14.Yee J. Living kidney donation: more than two to tango. Adv Chronic Kidney Dis. 2012;19:203–204. doi: 10.1053/j.ackd.2012.05.007. doi:10.1053/j.ackd.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 15.Spital A, Spital M, Spital R. The living kidney donor. Alive and well. Arch Intern Med. 1986;146:1993–1996. doi:10.1001/archinte.1986.00360220153026. [PubMed] [Google Scholar]
- 16.Mandelbrot DA, Pavlakis M, Danovitch GM, et al. The medical evaluation of living kidney donors: a survey of US transplant centers. Am J Transplant. 2007;7:2333–2343. doi: 10.1111/j.1600-6143.2007.01932.x. doi:10.1111/j.1600-6143.2007.01932.x. [DOI] [PubMed] [Google Scholar]
- 17.Danovitch G. Cash, rewards, and benefits in organ transplantation: an open letter to Senator Arlen Specter. Curr Opin Organ Transplant. 2009;14:129–133. doi: 10.1097/MOT.0b013e32832917b3. doi:10.1097/MOT.0b013e32832917b3. [DOI] [PubMed] [Google Scholar]
- 18.Epstein M. Sociological and ethical issues in transplant commercialism. Curr Opin Organ Transplant. 2009;14:134–139. doi: 10.1097/MOT.0b013e3283219d8e. [DOI] [PubMed] [Google Scholar]
- 19.Mathiharan K. Ethical and legal issues in organ transplantation: Indian scenario. Med Sci Law. 2011;51:134–140. doi: 10.1258/msl.2011.010134. doi:10.1258/msl.2011.010134. [DOI] [PubMed] [Google Scholar]
- 20.Vlaicu S, Klarenbach S, Yang RC, et al. Current Canadian initiatives to reimburse live organ donors for their non-medical expenses. Can J Public Health. 2007;98:481–483. doi: 10.1007/BF03405443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matas AJ, Hippen B, Satel S. In defense of a regulated system of compensation for living donation. Curr Opin Organ Transplant. 2008;13:379–385. doi: 10.1097/MOT.0b013e328308b2d9. doi:10.1097/MOT.0b013e328308b2d9. [DOI] [PubMed] [Google Scholar]
- 22.Omar F, Tinghog G, Welin S. Incentivizing deceased organ donation: a Swedish priority-setting perspective. Scand J Public Health. 2011;39:156–163. doi: 10.1177/1403494810391522. doi:10.1177/1403494810391522. [DOI] [PubMed] [Google Scholar]
- 23.Roff SR. We should consider paying kidney donors. BMJ. 2011;343:d4867. doi: 10.1136/bmj.d4867. doi:10.1136/bmj.d4867. [DOI] [PubMed] [Google Scholar]
- 24.Matas AJ, Satel S, Munn S, et al. Incentives for organ donation: proposed standards for an internationally acceptable system. Am J Transplant. 2012;12:306–312. doi: 10.1111/j.1600-6143.2011.03881.x. doi:10.1111/j.1600-6143.2011.03881.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Radcliffe-Richards J, Daar AS, Guttmann RD, et al. The case for allowing kidney sales. International forum for transplant ethics. Lancet. 1998;351:1950–1952. doi: 10.1016/s0140-6736(97)08211-1. doi:10.1016/S0140-6736(97)08211-1. [DOI] [PubMed] [Google Scholar]
- 26.Ghods AJ, Savaj S. Iranian model of paid and regulated living-unrelated kidney donation. Clin J Am Soc Nephrol. 2006;1:1136–1145. doi: 10.2215/CJN.00700206. doi:10.2215/CJN.00700206. [DOI] [PubMed] [Google Scholar]
- 27.Haghighi AN, Ghahramani N. Living unrelated kidney donor transplantation in Iran. Nat Clin Pract Nephrol. 2006;2:E1. doi: 10.1038/ncpneph0364. doi:10.1038/ncpneph0364. [DOI] [PubMed] [Google Scholar]
- 28.Daar AS. The case for a regulated system of living kidney sales. Nat Clin Pract Nephrol. 2006;2:600–601. doi: 10.1038/ncpneph0320. doi:10.1038/ncpneph0320. [DOI] [PubMed] [Google Scholar]
- 29.Halpern SD, Raz A, Kohn R, et al. Regulated payments for living kidney donation: an empirical assessment of the ethical concerns. Ann Intern Med. 2010;152:358–365. doi: 10.1059/0003-4819-152-6-201003160-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Strosberg MA, Gimbel RW. Kidney donation: when all else fails, try a regulated market. J Natl Med Assoc. 2010;102:44–45. doi: 10.1016/s0027-9684(15)30476-4. [DOI] [PubMed] [Google Scholar]
- 31.Ghahramani N, Karparvar ZY, Ghahramani M, et al. Nephrologists' perceptions of renal transplant as treatment of choice for end-stage renal disease, preemptive transplant, and transplanting older patients: an international survey. Exp Clin Transplant. 2011;9:223–229. [PMC free article] [PubMed] [Google Scholar]
- 32.Rodrigue JR, Cornell DL, Kaplan B, et al. Patients' willingness to talk to others about living kidney donation. Prog Transplant. 2008;18:25–31. doi: 10.1177/152692480801800107. [DOI] [PubMed] [Google Scholar]
- 33.Isotani S, Fujisawa M, Ichikawa Y, et al. Quality of life of living kidney donors: the short-form 36-item health questionnaire survey. Urology. 2002;60:588–592. doi: 10.1016/s0090-4295(02)01865-4. discussion 92 doi:10.1016/S0090-4295(02)01865-4. [DOI] [PubMed] [Google Scholar]
- 34.Clarke KS, Klarenbach S, Vlaicu S, et al. The direct and indirect economic costs incurred by living kidney donors-a systematic review. Nephrol Dial Transplant. 2006;21:1952–1960. doi: 10.1093/ndt/gfl069. doi:10.1093/ndt/gfl069. [DOI] [PubMed] [Google Scholar]
- 35.Dew MA, Jacobs CL. Psychosocial and socioeconomic issues facing the living kidney donor. Adv Chronic Kidney Dis. 2012;19:237–243. doi: 10.1053/j.ackd.2012.04.006. doi:10.1053/j.ackd.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Johnson EM, Anderson JK, Jacobs C, et al. Long-term follow-up of living kidney donors: quality of life after donation. Transplantation. 1999;67:717–721. doi: 10.1097/00007890-199903150-00013. doi:10.1097/00007890-199903150-00013. [DOI] [PubMed] [Google Scholar]
- 37.Giessing M, Reuter S, Schonberger B, et al. Quality of life of living kidney donors in Germany: a survey with the validated short form-36 and Giessen Subjective Complaints List-24 questionnaires. Transplantation. 2004;78:864–872. doi: 10.1097/01.tp.0000133307.00604.86. doi:10.1097/01.TP.0000133307.00604.86. [DOI] [PubMed] [Google Scholar]
- 38.Yang RC, Thiessen-Philbrook H, Klarenbach S, et al. Insurability of living organ donors: a systematic review. Am J Transplant. 2007;7:1542–1551. doi: 10.1111/j.1600-6143.2007.01793.x. doi:10.1111/j.1600-6143.2007.01793.x. [DOI] [PubMed] [Google Scholar]
- 39.Gibney EM, Doshi MD, Hartmann EL, et al. Health insurance status of US living kidney donors. Clin J Am Soc Nephrol. 2010;5:912–916. doi: 10.2215/CJN.07121009. doi:10.2215/CJN.07121009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rodrigue JR, Pavlakis M, Danovitch GM, et al. Evaluating living kidney donors: relationship types, psychosocial criteria, and consent processes at US transplant programs. Am J Transplant. 2007;7:2326–2332. doi: 10.1111/j.1600-6143.2007.01921.x. doi:10.1111/j.1600-6143.2007.01921.x. [DOI] [PubMed] [Google Scholar]
- 41.Ibrahim HN, Foley R, Tan L, et al. Long-term consequences of kidney donation. N Engl J Med. 2009;360:459–469. doi: 10.1056/NEJMoa0804883. doi:10.1056/NEJMoa0804883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Leichtman A, Abecassis M, Barr M, et al. Living kidney donor follow-up: state-of-the-art and future directions, conference summary and recommendations. Am J Transplant. 2011;11:2561–2568. doi: 10.1111/j.1600-6143.2011.03816.x. doi:10.1111/j.1600-6143.2011.03816.x. [DOI] [PubMed] [Google Scholar]
- 43.Davis CL. Living kidney donor follow-up: state-of-the-art and future directions. Adv Chronic Kidney Dis. 2012;19:207–211. doi: 10.1053/j.ackd.2012.03.002. doi:10.1053/j.ackd.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 44.Onwujekwe OE, Ogbonna C, Uguru N, et al. Increasing access to modern contraceptives: the potential role of community solidarity through altruistic contributions. Int J Equity Health. 2012;11:34. doi: 10.1186/1475-9276-11-34. doi:10.1186/1475-9276-11-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pradel FG, Jain R, Mullins CD, et al. A survey of nephrologists' views on preemptive transplantation. Clin J Am Soc Nephrol. 2008;3:1837–1845. doi: 10.2215/CJN.00150108. doi:10.2215/CJN.00150108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shimazono Y. The state of the international organ trade: a provisional picture based on integration of available information. Bull World Health Organ. 2007;85:955–962. doi: 10.2471/BLT.06.039370. doi:10.2471/BLT.06.039370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Raza M, Skordis-Worrall J. Pakistan's kidney trade: an overview of the 2007 ‘Transplantation of Human Organs and Human Tissue Ordinance.’ To what extent will it curb the trade? J Pak Med Assoc. 2012;62:85–89. [PubMed] [Google Scholar]
- 48.Ghahramani N, Rizvi SA, Padilla B. Paid donation: a global view. Adv Chronic Kidney Dis. 2012;19:262–268. doi: 10.1053/j.ackd.2012.05.002. doi:10.1053/j.ackd.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Matas A, Ambagtsheer JA, Gaston R, et al. A realistic proposal – incentives may increase donation – we need trials now! Am J Transplant. 2012;12:1957–1958. doi: 10.1111/j.1600-6143.2012.04117.x. doi:10.1111/j.1600-6143.2012.04117.x. [DOI] [PubMed] [Google Scholar]
- 50.Hippen B, Matas A. Incentives for organ donation in the United States: feasible alternative or forthcoming apocalypse? Curr Opin Organ Transplant. 2009;14:140–146. doi: 10.1097/MOT.0b013e3283295e0d. doi:10.1097/MOT.0b013e3283295e0d. [DOI] [PubMed] [Google Scholar]
- 51.Hippen B, Ross LF, Sade RM. Saving lives is more important than abstract moral concerns: financial incentives should be used to increase organ donation. Ann Thorac Surg. 2009;88:1053–1061. doi: 10.1016/j.athoracsur.2009.06.087. doi:10.1016/j.athoracsur.2009.06.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Danovitch G, Veale J, Hippen B. Living donor kidney donation in the United States: quo vadis? Am J Transplant. 2010;10:1345–1346. doi: 10.1111/j.1600-6143.2010.03097.x. doi:10.1111/j.1600-6143.2010.03097.x. [DOI] [PubMed] [Google Scholar]
- 53.Danovitch GM, Delmonico FL. The prohibition of kidney sales and organ markets should remain. Curr Opin Organ Transplant. 2008;13:386–394. doi: 10.1097/MOT.0b013e3283097476. doi:10.1097/MOT.0b013e3283097476. [DOI] [PubMed] [Google Scholar]
- 54.Kubler A, Adamik B, Lipinska-Gediga M, et al. End-of-life attitudes of intensive care physicians in Poland: results of a national survey. Intensive Care Med. 2011;37:1290–1296. doi: 10.1007/s00134-011-2269-2. doi:10.1007/s00134-011-2269-2. [DOI] [PubMed] [Google Scholar]
- 55.Wandrowski J, Schuster T, Strube W, et al. Medical ethical knowledge and moral attitudes among physicians in Bavaria. Dtsch Arztebl Int. 2012;109:141–147. doi: 10.3238/arztebl.2012.0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.De Zordo S, Mishtal J. Physicians and abortion: provision, political participation and conflicts on the ground – the cases of Brazil and Poland. Womens Health Issues. 2011;21(Suppl 3):S32–S36. doi: 10.1016/j.whi.2011.01.006. doi:10.1016/j.whi.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 57.Gielen J, van den Branden S, Broeckaert B. Religion and nurses' attitudes to euthanasia and physician assisted suicide. Nurs Ethics. 2009;16:303–318. doi: 10.1177/0969733009102692. doi:10.1177/0969733009102692. [DOI] [PubMed] [Google Scholar]
- 58.Lawrence RE, Curlin FA. Physicians' beliefs about conscience in medicine: a national survey. Acad Med. 2009;84:1276–1282. doi: 10.1097/ACM.0b013e3181b18dc5. doi:10.1097/ACM.0b013e3181b18dc5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Combs MP, Antiel RM, Tilburt JC, et al. Conscientious refusals to refer: findings from a national physician survey. J Med Ethics. 2011;37:397–401. doi: 10.1136/jme.2010.041194. doi:10.1136/jme.2010.041194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rios A, Lopez-Navas A, Ayala-Garcia MA, et al. Attitudes toward living kidney donation in transplant hospitals: a Spanish, Mexican, and Cuban multicenter study. Transplant Proc. 2010;42:228–232. doi: 10.1016/j.transproceed.2009.11.006. doi:10.1016/j.transproceed.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 61.Bruzzone P. Religious aspects of organ transplantation. Transplant Proc. 2008;40:1064–1067. doi: 10.1016/j.transproceed.2008.03.049. doi:10.1016/j.transproceed.2008.03.049. [DOI] [PubMed] [Google Scholar]
- 62.Abouna GM. Negative impact of trading in human organs on the development of transplantation in the Middle East. Transplant Proc. 1993;25:2310–2313. [PubMed] [Google Scholar]
- 63.O'Donnell O, van Doorslaer E, Rannan-Eliya RP, et al. Who pays for health care in Asia? J Health Econ. 2008;27:460–475. doi: 10.1016/j.jhealeco.2007.08.005. doi:10.1016/j.jhealeco.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 64.Barsoum RS. A mission in evolution: the International Society of Nephrology in the past 10 years – 2001–2010. Kidney Int. 2011;79:935–943. doi: 10.1038/ki.2011.7. doi:10.1038/ki.2011.7. [DOI] [PubMed] [Google Scholar]
- 65.Callegaro M, Disogra C. Computing response metrics for online panels. Public Opin Quart. 2008;72:1008–1032. doi:10.1093/poq/nfn065. [Google Scholar]
- 66.Braithwaite D, Emery J, De Lusignan S, et al. Using the Internet to conduct surveys of health professionals: a valid alternative? Fam Pract. 2003;20:545–551. doi: 10.1093/fampra/cmg509. doi:10.1093/fampra/cmg509. [DOI] [PubMed] [Google Scholar]
- 67.Leece P, Bhandari M, Sprague S, et al. Internet versus mailed questionnaires: a controlled comparison (2) J Med Internet Res. 2004;6:e39. doi: 10.2196/jmir.6.4.e39. doi:10.2196/jmir.6.4.e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Malloy DC, Sevigny P, Hadjistavropoulos T, et al. Perceptions of the effectiveness of ethical guidelines: an international study of physicians. Med Health Care Philos. 2009;12:373–383. doi: 10.1007/s11019-009-9212-0. doi:10.1007/s11019-009-9212-0. [DOI] [PubMed] [Google Scholar]