Abstract
Aim of the study
Platelet-derived growth factor B (PDGF-B), a vital growth factor which can induce angiogenesis and epithelial-mesenchymal transition (EMT), is important in the metastasis of many tumors. However, the roles of PDGF-B in gastric carcinoma are largely unknown. We investigated the correlation between PDGF-B, PDGFR-β and E-cadherin expression with the clinical features of gastric carcinoma patients to evaluate the relationship between PDGF-B signaling, E-cadherin and metastasis of gastric carcinoma, the correlation between PDGF-B and E-cadherin expression to assess the roles of PDGF-B signaling in metastasis of gastric carcinoma..
Material and methods
We detected expressions of PDGF-B, PDGFR-β and E-cadherin in gastric carcinoma tissues and normal gastric mucosa tissues of 64 patients with gastric carcinoma who had undergone surgical resection, and investigated their relationships with clinical features and the relationships between PDGF-B and E-cadherin expression in gastric carcinoma.
Results
In surgical specimens, tumor cells expressed PDGF-B, and PDGFR-β was expressed by tumor stromal cells. E-cadherin was expressed by both tumor cells and normal gastric mucosa cells. Expressions of PDGF-B and PDGFR-β were increased in gastric carcinoma tissues (p < 0.05) and were positively correlated with the depth of cancer invasion, lymph node metastasis and TNM stage (p < 0.05). The expression of E-cadherin was reduced in gastric carcinoma tissues (p < 0.05) and was negatively correlated with the depth of cancer invasion, lymph node metastasis and TNM stage (p < 0.05). The correlation between PDGF-B and E-cadherin expression was negative (p < 0.05).
Conclusion
Our data indicate that either the overexpression of PDGF-B and PDGFR-β or the underexpression of E-cadherin is correlated with cancer progression and lymphogenous metastasis of gastric carcinoma. The PDGF-B signal pathway might induce EMT by down-regulating expression of E-cadherin to promote metastasis of gastric carcinoma.
Keywords: platelet-derived growth factor B (PDGF-B), platelet-derived growth factor receptor-β (PDGFR-β), E-cadherin, gastric carcinoma
Introduction
In past decades, mortality caused by gastric cancer decreased notably [1], but gastric cancer is still a major leading cause of cancer mortality in the world [2]. Surgical resection and adjuvant chemotherapy are the main treatments for gastric cancer, but the overall 5-year survival rate of patients with resectable gastric cancer is still lower than 30% [3, 4]. Metastasis is the most important cause of death and emerging evidence suggests that platelet-derived growth factor B (PDGF-B) signaling was highly expressed in some kinds of tumors and was associated with metastasis of tumors [5–7]. But the roles of PDGF-B signaling in metastasis of gastric carcinoma are largely unknown.
Epithelial-mesenchymal transition (EMT) is a quite important process in the metastasis of various kinds of solid tumors [8, 9], including gastric carcinomas [10]. This process involves disassembly of cell–cell junctions, including downregulation and relocation of E-cadherin [11], so E-cadherin was an important molecular marker of EMT and was widely detected in many tumors [12, 13]. Also, the processes of EMT can be triggered by various growth factors, such as PDGF-B [14–16]. So, we ask whether PDGF-B signaling could induce EMT so as to promote metastasis of gastric carcinoma.
In this study, we examined the expression of PDGF-B, PDGFR-β and E-cadherin in human gastric carcinoma. Then, we investigated the correlation between PDGF-B, PDGFR-β and E-cadherin expression with the clinical features of gastric carcinoma patients to evaluate the relationship between PDGF-B signaling, E-cadherin and metastasis of gastric carcinoma. We also investigated the correlation between PDGF-B and E-cadherin expression to assess the roles of PDGF-B signaling in metastasis of gastric carcinoma.
Material and methods
Patients and tumor specimens
Surgical resection specimens (tumor and corresponding normal mucosa) of gastric tissue from 64 patients with gastric carcinoma at the First Affiliated Hospital of Chongqing Medical University between February 2011 and October 2011 were partly snap-frozen in liquid nitrogen and stored at –80°C until protein extraction for western blotting, and partly fixed by paraformaldehyde for immunohistochemical staining. The patients included 38 males and 26 females, with a mean age of 55.6 years (range, 32–76 years). The condition of the patients was assessed according to the system for staging primary tumor/regional lymph nodes/distant metastasis (TNM) described in the AJCC Cancer Staging Manual [17]. Pathology reports and clinical histories were reviewed for accurate staging at the time of surgery (Table 1). 47 patients (73.4%) had lymph node metastases. D2 or more extended lymph node dissection was conducted in 56 patients (87.5%). All cancers were resected (no residual tumor, R category 0) in 64 patients (100%). None of the patients had received any preoperative treatments, including neoadjuvant therapy. The Research Ethics and Scientific Committee of the Medical Faculty, Chongqin Medical University, approved the study protocol and all subjects gave informed consent.
Table 1.
Clinicopathological features of patients with gastric carcinoma
| Parameter | n | % |
|---|---|---|
| Total number of patients | 64 | |
| Gender | ||
| male | 38 | 59.4 |
| female | 26 | 40.6 |
| Age | ||
| mean (range) | 55.6 (32–76) | |
| Tumor differentiation | ||
| well differentiated | 12 | 18.6 |
| moderately differentiated | 18 | 28.2 |
| Poorly differentiated | 34 | 53.2 |
| T stage | ||
| Tis | 0 | 0 |
| T1 | 6 | 9.4 |
| T2 | 8 | 12.5 |
| T3 | 20 | 31.5 |
| T4 | 30 | 46.9 |
| N stage | ||
| N0 | 17 | 26.5 |
| N1 | 9 | 14.1 |
| N2 | 16 | 25.0 |
| N3 | 22 | 34.4 |
| Extent of lymphadenectomy | ||
| D0 | 2 | 3.1 |
| D1 | 6 | 9.4 |
| D2 | 46 | 71.9 |
| D3 | 10 | 15.6 |
| Residual tumor status (R category) | ||
| R0 | 64 | 100 |
| R1 | 0 | 0 |
Immunohistochemical staining
Paraformaldehyde-fixed and paraffin-embedded blocks of specimens were cut 3-µm thick and mounted onto poly-L-lysine coated glass slides. The tissue sections were stained immunohistochemically with antigen retrieval methods [18]. Briefly, sections were heated in a microwave oven to maintain the temperature at 92–98°C for 10–15 min, then were incubated with 10% normal goat serum for 30 min. After washing with PBS 3 times, sections were incubated with mouse anti-PDGF-B (Santa Cruz Biotechnology, Inc, USA), mouse anti-PDGFR-β (Santa Cruz Biotechnology, Inc, USA) and mouse anti-E-cadherin (Santa Cruz biotechnology, Inc, USA) primary antibody (1 : 100 dilution) at 4°C overnight, then were incubated with anti-mouse secondary antibody (1 : 100 dilution) at room temperature for 30 min. After adding 100 µl (1 : 200 dilution) streptavidin-coupled horseradish peroxidase (streptavidin-HRP), sections were incubated at room temperature for 20 min followed by adding freshly prepared 0.02% diaminobenzidine (DAB) for 3–5 min. The reaction was terminated by washing with distilled water. Tissues were counterstained with hematoxylin and returned to blue with ammonia water. After drying with gradient alcohol and xylene, tissues were mounted with 50% glycerine.
Evaluation of immunostaining
The immunoreactivity for PDGF-B, PDGFR-β and E-cadherin was localized in the cytoplasm. According to one of the established methods, staining intensity was scored as 0 (none), 1+ (weak), 2+ (moderate), or 3+ (strong). The proportion of positively stained tumor cells in lesions was scored as 0 (0%), 1 (1–25%), 2 (26–50%), 3 (51–75%), or 4 (76–100%) [19, 20]. When the sum of the two scores was less than 4, the section was considered negative, whereas 4 or more was considered positive for overexpression of PDGF-B and PDGFR-β.
Western blot analysis
After comminution, tissues were lysed in RIPA buffer containing 50 mM Tris–HCl, 150 mM NaCl, 1% NP-40, 0.1% SDS, 0.5% sodium deoxycholate, 2 mM sodium fluoride, 2 mM Na3VO42, 1 mM EDTA, and 1 mM EGTA, then were analyzed by western blotting [21]. Samples (20 µg of total protein or from 1 mg of total cell proteins) were loaded onto SDS-PAGE gels (Invitrogen) and separated by size using electrophoresis. Proteins were then transferred to PVDF membranes for 1 hour. The membranes were then blotted for 1 hour with 5% milk. Membranes were incubated with primary antibodies (1 : 500 dilution) against PDGF-B (Santa Cruz Biotechnology, Inc, USA) and E-cadherin (Santa Cruz Biotechnology, Inc, USA) at 4°C overnight. After incubation with horseradish peroxidase-conjugated secondary antibody (1 : 1000 dilution) for 3 hours at 37°C, proteins were detected by ECL chemiluminescence HRP substrate for 5 minutes. The films were analyzed by densitometry with image software.
Statistical analysis
Statistical Package for the Social Science software (version 15.0; SPSS Concepts) was used for the data analysis. Clinicopathological variables, as well as expression of PDGF-B, PDGFR-β and E-cadherin, were analyzed. Immunohistochemical data of PDGF-B, PDGFR-β and E-cadherin expression between gastric carcinoma and normal gastric mucosa tissues were analyzed with the χ2 test. The correlations between PDGF-B, PDGFR-β and E-cadherin expressions, and the other variables, were assessed with the χ2 and Fisher's exact tests. The association between PDGF-B and E-cadherin was evaluated using Spearman's correlation test. P < 0.05 was considered to indicate a statistically significant difference.
Results
Expression of platelet-derived growth factor B, platelet-derived growth factor receptor-β and E-cadherin
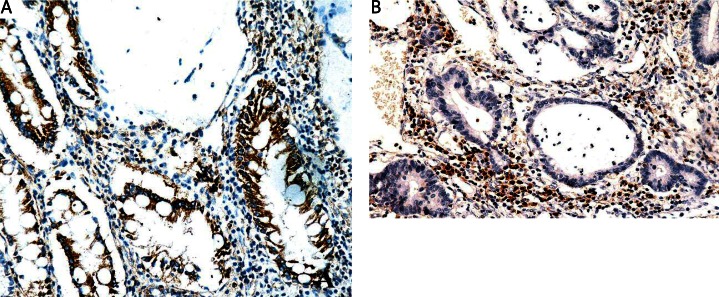
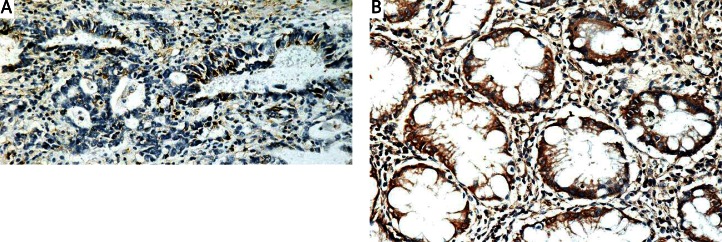
Immunoreactivity for PDGF-B was present predominantly in the cytoplasm of the carcinoma cells (Fig. 1A). Immunoreactivity for PDGFR-β was present predominantly in the cytoplasm of tumor stromal cells and of some inflammatory cells (Fig. 1B). Immunoreactivity for E-cadherin was lower in the cytoplasm of carcinoma cells and tumor stromal cells in gastric carcinoma tissues (Fig. 2A), and was higher in the cytoplasm of normal gastric mucosa cells and stromal cells in normal gastric mucosa tissues (Fig. 2B). Positive rate of PDGF-B expression was significantly higher in gastric carcinoma tissues (45/64, 70.3%) than in normal gastric mucosa tissues (3/64, 4.7%) (p < 0.05) (Table 2). Positive rate of PDGFR-β expression was significantly higher in gastric carcinoma tissues (39/64, 60.9%) than in normal gastric mucosa tissues (2/64, 3.1%) (p < 0.05) (Table 2). Positive rate of E-cadherin expression was significantly lower in gastric carcinoma tissues (17/64, 26.6%) than in normal gastric mucosa tissues (61/64, 95.3%) (p < 0.05) (Table 2).
Fig. 1.
Expression of PDGF-B and PDGFR-β protein in human gastric adenocarcinoma tissues by immunohistochemistry. Original magnification 200×. A) Strong expression of PDGF-B in tumor cells of gastric carcinoma cells. B) Strong expression of PDGFR-β in tumor stromal cells of gastric carcinoma tissues
Fig. 2.
Expression of E-cadherin protein in human gastric adenocarcinoma tissues and in normal gastric mucosa tissues by immunohistochemistry. Original magnification 200×. A) Weak expression of E-cadherin in gastric carcinoma tissues. B) Strong expression of E-cadherin in normal gastric mucosa tissues
Table 2.
Positive rate of PDGF-B and PDGFR-β expression in gastric carcinoma tissues and normal gastric mucosa tissues
| Gastric carcinoma tissues | Gastric mucosa tissues | P | |
|---|---|---|---|
| PDGF-B expression | 45/64 (70.3%) | 3/64 (4.7%) | < 0.05 |
| PDGFR-β expression | 39/64 (60.9%) | 2/64 (3.1%) | < 0.05 |
| E-cadherin expression | 17/64 (26.6%) | 61/64 (95.3%) | < 0.05 |
Gastric adenocarcinoma tissues compared with normal gastric mucosa tissues p < 0.05
Relation between overexpression of platelet-derived growth factor B, platelet-derived growth factor receptor-β and E-cadherin and clinicopathological features of gastric carcinoma
Expression of PDGF-B and PDGFR-β was positively correlated with the depth of cancer invasion (p < 0.0001 and p < 0.0001, respectively), lymph node metastasis (p < 0.0001 and p < 0.0001, respectively) and tumor-node-metastasis (TNM) stage (p = 0.0004 and p = 0.0005, respectively), but there was no difference between different grades of tumor differentiation (p = 0.1289 and p = 0.2013, respectively) (Table 3). The expression of E-cadherin was negatively correlated with the depth of cancer invasion (p < 0.0001), lymph node metastasis (p < 0.0001) and TNM stage (p = 0.0004), but no difference was found between different grades of tumor differentiation (p = 0.2243) (Table 4).
Table 3.
Correlation between expression of PDGF-B, PDGFR-β and clinicopathological features of gastric carcinoma
| Variable | n | PDGF-B | χ2 | P | PDGFR-β | χ2 | P | ||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| (+) | (–) | (+) | (–) | ||||||
| Tumor differentiation | 0.392 | > 0.05 | 0.371 | > 0.05 | |||||
| well differentiated | 12 | 8 | 4 | 7 | 5 | ||||
| moderately differentiated | 18 | 13 | 5 | 11 | 7 | ||||
| poorly differentiated | 34 | 24 | 10 | 21 | 13 | ||||
| T stage | 9.192 | < 0.01 | 8.937 | < 0.01 | |||||
| Tis | 0 | 0 | 0 | 0 | 0 | ||||
| T1 | 6 | 1 | 5 | 0 | 6 | ||||
| T2 | 8 | 3 | 5 | 3 | 5 | ||||
| T3 | 20 | 13 | 7 | 12 | 8 | ||||
| T4 | 30 | 28 | 2 | 24 | 6 | ||||
| N stage | 11.679 | < 0.01 | 12.059 | < 0.01 | |||||
| N0 | 17 | 4 | 13 | 4 | 13 | ||||
| N1 | 9 | 6 | 3 | 5 | 4 | ||||
| N2 | 16 | 14 | 2 | 11 | 5 | ||||
| N3 | 22 | 21 | 1 | 19 | 3 | ||||
| TNM stage | 7.398 | < 0.01 | 7.051 | < 0.01 | |||||
| I | 8 | 3 | 5 | 1 | 7 | ||||
| II | 18 | 11 | 7 | 10 | 8 | ||||
| III | 36 | 29 | 7 | 26 | 10 | ||||
| IV | 2 | 2 | 0 | 2 | 0 | ||||
Different variable interclass date compared p < 0.05
Table 4.
Correlation between expression of E-cadherin and clinicopathological features of gastric carcinoma
| Variable | n | E-cadherin | χ2 | P | |
|---|---|---|---|---|---|
|
|
|||||
| (+) | (–) | ||||
| Tumor differentiation | 0.715 | > 0.05 | |||
| well differentiated | 12 | 3 | 9 | ||
| moderately differentiated | 18 | 5 | 13 | ||
| poorly differentiated | 34 | 9 | 25 | ||
| T stage | 11.309 | < 0.01 | |||
| Tis | 0 | 0 | 0 | ||
| T1 | 6 | 5 | 1 | ||
| T2 | 8 | 4 | 4 | ||
| T3 | 20 | 5 | 15 | ||
| T4 | 30 | 3 | 27 | ||
| N stage | 12.097 | < 0.01 | |||
| N0 | 17 | 11 | 6 | ||
| N1 | 9 | 3 | 6 | ||
| N2 | 16 | 2 | 14 | ||
| N3 | 22 | 1 | 21 | ||
| TNM stage | 8.657 | < 0.01 | |||
| I | 8 | 6 | 2 | ||
| II | 18 | 8 | 10 | ||
| III | 36 | 3 | 33 | ||
| IV | 2 | 0 | 2 | ||
Different variable interclass date compared p < 0.05
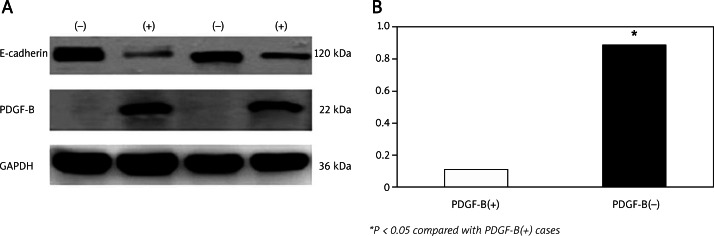
Relation between overexpression of platelet-derived growth factor B and underexpression of E-cadherin
To evaluate the relation between overexpression of PDGF-B and underexpression of E-cadherin in gastric carcinoma tissue samples, western blot was performed. Nine PDGF-B positive cases of gastric carcinoma tissue specimens and 9 PDGF-B negative cases of gastric carcinoma tissue specimens were chosen for western blotting analysis. We found that E-cadherin protein expression (0.116 ±0.02) in PDGF-B positive gastric carcinoma tissues was much lower than E-cadherin protein expression (0.887 ±0.060) in PDGF-B negative gastric carcinoma tissues (p < 0.05). The results showed that E-cadherin expression was negatively correlated with PDGF-B expression (rs = –0.489; p < 0.001) (Fig. 3).
Fig. 3.
Western blot analysis of E-cadherin in PDGF-B positive and PDGF-B negative gastric carcinoma tissues. A) E-cadherin protein expression in representative two couple cases of gastric carcinoma. GAPDH protein was used as protein loading control. (+): PDGF-B(+) cases; (–): PDGF-B(–) cases. B) E-cadherin protein expression in PDGF-B positive and PDGF-B negative gastric carcinoma tissues
Discussion
Metastasis is a common clinical finding in many human cancers and is the primary cause of death for most cancer patients [22]. Both angiogenesis and EMT are important in the process of tumor metastasis [11, 23, 24].
PDGF-B and PDGFR-β have been demonstrated to be expressed in many kinds of cancers [5, 7, 25]. PDGF-B through interaction with PDGFR-β expressed on tumor stromal cells was thought to be one of the direct angiogenesis factors to promote tumor metastasis, and it was once thought to be the only role of PDGF-B [26]. But, in an extensive study in which Patel et al. [16] implanted PDGF-B in mouse peritoneum, the factor was shown to induce EMT. Additionally, it was widely reported that EMT was a major cause of tumor metastasis [8, 9, 27, 28]. So, we asked whether PDGF-B could induce EMT to promote tumor metastasis in gastric carcinomas.
In our study, E-cadherin as a molecular marker of EMT was detected to evaluate EMT. We found that expression of PDGF-B and PDGFR-β was much higher in gastric carcinoma tissues than normal gastric mucosa tissues, and expression of E-cadherin was much lower in gastric carcinoma tissues than normal gastric mucosa tissues (Table 2). The results of the present study are consistent with the previous studies [25, 29]. In a previous study, it was demonstrated that positive immunostaining rates of PDGF-B and PDGFR-β correlated with lymph node metastasis [25], the same as we reported. In addition, we also found that expression of PDGF-B and PDGFR-β was positively correlated with the depth of cancer invasion, and TNM stage, but not correlated with tumor differentiation (Table 3). The expression of E-cadherin was negatively correlated with the depth of cancer invasion, lymph node metastasis and TNM stage (Table 4), the same as Yuan et al. [29] reported. Those results suggested that PDGF-B, PDGFR-β and E-cadherin might be useful biomarkers of tumor metastasis. But further studies were needed to explain how PDGF-B signaling and E-cadherin affect metastasis of gastric carcinoma.
In our study, we also analyzed the correlation between PDGF-B and E-cadherin expressions. We found that the correlation between PDGF-B and E-cadherin expression was negative. High expression of PDGF-B may induce down-regulation of E-cadherin (Fig. 3). Also, many studies have shown that down-regulation and relocation of E-cadherin are hallmarks of EMT [11, 30, 31]. So, we might infer that PDGF-B could induce EMT to promote tumor metastasis by downregulation of E-cadherin in gastric carcinoma. However, the mechanism by which PDGF-B induced downregulation of E-cadherin is still unknown. Some interesting studies show that the PI3K/AKT pathway could induce EMT by downregulation of E-cadherin [32–34]. According to these findings, we might conjecture that PDGF-B may induce EMT by activation of the PI3K/AKT pathway so as to promote metastasis of gastric carcinoma, but further studies are needed. It might be another important role of PDGF-B signaling in promoting metastasis of gastric carcinoma.
In conclusion, we found that either the overexpression of PDGF-B and PDGFR-β or the underexpression of E-cadherin is correlated with cancer progression and lymphogenous metastasis of gastric carcinoma, suggesting that both of them may play an important role in tumor progression and metastasis of gastric carcinoma. PDGF-B signaling perhaps could not only induce angiogenesis but also induce EMT to promote metastasis of gastric carcinoma. Thus, blockage of the PDGF-B signaling pathway may be a reasonable approach for treatment of gastric carcinoma.
This work was partly funded by grants from the Department of Gastrointestinal Surgery, First Affiliated Hospital of Chongqing Medical University.
References
- 1.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Michael J. Cancer statistics, 2009. CA Cancer J Clin. 2009;59:225–49. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- 2.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 3.Alberts SR, Cervantes A, van de Velde CJH. Gastric cancer: epidemiology, pathology and treatment. Ann Oncol. 2003;14:ii31–6. doi: 10.1093/annonc/mdg726. [DOI] [PubMed] [Google Scholar]
- 4.Green D, Ponce DL, Leon-Rodriguez E, Sosa-Sanchez R. Adenocarcinoma of the stomach: univariate and multivariate analysis of factors associated with survival. Am J Clin Oncol. 2002;25:84–9. doi: 10.1097/00000421-200202000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Donnem T, Al-Saad S, Al-Shibli K, Busund LT, Bremnes RM. Co-expression of PDGF-B and VEGFR-3 strongly correlates with lymph node metastasis and poor survival in non-small-cell lung cancer. Ann Oncol. 2010;21:223–31. doi: 10.1093/annonc/mdp296. [DOI] [PubMed] [Google Scholar]
- 6.Calzolari F, Appolloni I, Tutucci E, Caviglia S, Terrile M, Corte G, Malatesta P. Tumor progression and oncogene addiction in a PDGF-B-induced model of gliomagenesis. Neoplasia. 2008;10:1373–82. doi: 10.1593/neo.08814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yu J, Ustach C, Kim HR. Platelet-derived growth factor signaling and human cancer. J Biochem Mol Biol. 2003;36:49–59. doi: 10.5483/bmbrep.2003.36.1.049. [DOI] [PubMed] [Google Scholar]
- 8.Zavadil J, Haley J, Kalluri R, Muthuswamy SK, Thompson E. Epithelial-mesenchymal transition. Cancer Res. 2008;68:9574–7. doi: 10.1158/0008-5472.CAN-08-2316. [DOI] [PubMed] [Google Scholar]
- 9.Yang J, Weinberg RA. Epithelial-mesenchymal transition: at the crossroads of development and tumor metastasis. Developmental Cell. 2008;10:818–26. doi: 10.1016/j.devcel.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 10.Kim MA, Lee HS, Lee HE, Kim JH, Yong HK, Kim WH. Prognostic importance of epithelial–mesenchymal transition-related protein expression in gastric carcinoma. Histopathology. 2009;54:442–51. doi: 10.1111/j.1365-2559.2009.03247.x. [DOI] [PubMed] [Google Scholar]
- 11.Christiansen JJ, Rajasekaran AK. Reassessing epithelial to mesenchymal transition as a prerequisite for carcinoma invasion and metastasis. Cancer Res. 2006;66:8319–26. doi: 10.1158/0008-5472.CAN-06-0410. [DOI] [PubMed] [Google Scholar]
- 12.Özgüven BY, Karaçetin D, Kabukçuoğlu F, Takin T, Yener S. Immunohistochemical study of E-cadherin and β-catenin expression in colorectal carcinomas. Pol J Pathol. 2011;1:19–24. [PubMed] [Google Scholar]
- 13.Rakha EA, Patel A, Powe DG, Benhasouna A, Green AR, Lambros MB, Reis-Filho JS, Ellis IO. Clinical and biological significance of E-cadherin protein expression in invasive lobular carcinoma of the breast. Am J Surg Pathol. 2010;34:1472–9. doi: 10.1097/PAS.0b013e3181f01916. [DOI] [PubMed] [Google Scholar]
- 14.Fischer AN, Fuchs E, Mikula M, Huber H, Beug H, Mikulits W. PDGF essentially links TGF-beta signaling to nuclear beta-catenin accumulation in hepatocellular carcinom a progression. Oncogene. 2007;26:3395–405. doi: 10.1038/sj.onc.1210121. [DOI] [PubMed] [Google Scholar]
- 15.Gotzmann J, Fischer AN, Zojer M, et al. A crucial function of PDGF in TGF-beta-mediated cancer progression of hepatocytes. Oncogene. 2006;25:3170–85. doi: 10.1038/sj.onc.1209083. [DOI] [PubMed] [Google Scholar]
- 16.Patel P, West-Mays J, Kolb M, Rodrigues JR, Hoff CM, Margetts PJ. Platelet derived growth factor B and epithelial mesenchymal transition of peritoneal mesothelial cells. Matrix Biology. 2010;29:97–106. doi: 10.1016/j.matbio.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 17.Washington K. 7th edition of the AJCC cancer staging manual: stomach. Ann Surg Oncol. 2010;17:3077–9. doi: 10.1245/s10434-010-1362-z. [DOI] [PubMed] [Google Scholar]
- 18.Ciaparrone M, Yamamoto H, Yao Y, et al. Localization and expression of p27KIP1 in multistage colorectal carcinogenesis. Cancer Res. 1998;58:114–22. [PubMed] [Google Scholar]
- 19.Kolev Y, Uetake H, Iida S, Ishikawa T, Kawano T, Sugihara K. Prognostic significance of VEGF expression in correlation with COX-2, microvessel density, and clinicopathological characteristics in human gastric carcinoma. Ann Surg Oncol. 2007;14:2738–47. doi: 10.1245/s10434-007-9484-7. [DOI] [PubMed] [Google Scholar]
- 20.Cabuk D, Basaran G, Celikel C, Dane F, Yumuk PF, Iyikesici MS, Ekenel M, Turhal NS. Vascular endothelial growth factor, hypoxia-inducible factor 1 alpha and CD34 expressions in early-stage gastric tumors: relationship with pathological factors and prognostic impact on survival. Oncology. 2007;72:111–7. doi: 10.1159/000111118. [DOI] [PubMed] [Google Scholar]
- 21.Kong D, Li Y, Wang Z, Banerjee S, Sarkar FH. Inhibition of angiogenesis and invasion by 3,3’-diindolylmethane is mediated by the nuclear factor-kappaB downstream target genes MMP-9 and uPA that regulated bioavailability of vascular endothelial growth factor in prostate cancer. Cancer Res. 2007;67:3310–19. doi: 10.1158/0008-5472.CAN-06-4277. [DOI] [PubMed] [Google Scholar]
- 22.Steeg PS. Tumor metastasis: mechanistic insights and clinical challenge. Nature Medince. 2006;12:895–904. doi: 10.1038/nm1469. [DOI] [PubMed] [Google Scholar]
- 23.Zetter BR. Angiogenesis and tumor metastasis. Annu Rev Med. 1998;49:407–24. doi: 10.1146/annurev.med.49.1.407. [DOI] [PubMed] [Google Scholar]
- 24.Folkman J. Role of angiogenesis in tumor growth and metastasis. Oncology. 2002;29:15–8. doi: 10.1053/sonc.2002.37263. [DOI] [PubMed] [Google Scholar]
- 25.Suzuki S, Dobashi Y, Hatakeyama Y, Tajiri R, Fujimura T, Heldin CH, Ooi1 A. Clinicopathological significance of platelet-derived growth factor (PDGF)-B and vascular endothelial growth factor-A expression, PDGF receptor-b phosphorylation, and microvessel density in gastric cancer. BMC Cancer. 2010;10:659–69. doi: 10.1186/1471-2407-10-659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sennino B, Falcon BL, McCauley D, et al. Sequential loss of tumor vessel pericytes and endothelial cells after inhibition of platelet-derived growth factor B by selective aptamer AX102. Cancer Res. 2007;67:7358–67. doi: 10.1158/0008-5472.CAN-07-0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thiery JP. Epithelial–mesenchymal transitions in tumour progression. Nat Rev. 2002;2:442–54. doi: 10.1038/nrc822. [DOI] [PubMed] [Google Scholar]
- 28.Kang Y, Massagué J. Epithelial-mesenchymal transitions: twist in development and metastasis. Cell. 2004;118:277–9. doi: 10.1016/j.cell.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 29.Yuan W, Chen Z, Wu S, Ge J, Chang S, Wang X, Chen J, Chen Z. Expression of EphA2 and E-cadherin in gastric cancer: correlated with tumor progression and lymphogenous metastasis. Pathol Oncol Res. 2009;15:473–8. doi: 10.1007/s12253-008-9132-y. [DOI] [PubMed] [Google Scholar]
- 30.Cano A, Pérez-Moreno MA, Rodrigo I, Locascio A, Blanco MJ, del Barrio MJ, Portillo F, Nieto MA. The transcription factor Snail controls epithelial–mesenchymal transitions by repressing E-cadherin expression. Nat Cell Biol. 2000;2:76–83. doi: 10.1038/35000025. [DOI] [PubMed] [Google Scholar]
- 31.Korpol M, Lee ES, Hu G, Kang Y. The miR-200 family inhibits epithelial-mesenchymal transition and cancer cell migration by direct targeting of E-cadherin transcriptional repressors ZEB1 and ZEB2. J Biol Chem. 2008;283:14910–4. doi: 10.1074/jbc.C800074200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bellacosa A, Larue L. PI3K/AKT Pathway and the Epithelial-Mesenchymal Transition. In: Thomas-Tikhonenko A, editor. Cancer Genome and Tumor Microenvironment. New York: Springer; 2010. pp. 11–32. [Google Scholar]
- 33.Larue L, Bellacosa A. Epithelial-mesenchymal transition in development and cancer: role of phosphatidylinositol 3’ kinase/AKT pathway. Oncogene. 2005;24:7443–54. doi: 10.1038/sj.onc.1209091. [DOI] [PubMed] [Google Scholar]
- 34.Grille SJ, Bellacosa A, Upson J, et al. The Protein Kinase Akt Induces Epithelial Mesenchymal Transition and Promotes Enhanced Motility and Invasiveness of Squamous Cell Carcinoma Lines. Cancer Res. 2003;62:2172–80. [PubMed] [Google Scholar]