Abstract
Most synthetic polymer hydrogel tissue adhesives and sealants swell considerably in physiologic conditions, which can result in mechanical weakening and adverse medical complications. Herein, we describe the synthesis and characterization of mechanically tough zero- or negative-swelling mussel-inspired surgical adhesives based on catechol-modified amphiphilic poly(propylene oxide)-poly(ethylene oxide) block copolymers. The formation, swelling, bulk mechanical, and tissue adhesive properties of the resulting thermosensitive gels were characterized. Catechol oxidation at or below room temperature rapidly resulted in a chemically cross-linked network, with subsequent warming to physiological temperature inducing a thermal hydrophobic transition in the PPO domains and providing a mechanism for volumetric reduction and mechanical toughening. The described approach can be easily adapted for other thermally sensitive block copolymers and cross-linking strategies, representing a general approach that can be employed to control swelling and enhance mechanical properties of polymer hydrogels used in a medical context.
Keywords: adhesives, hydrogels, mechanical properties, polymeric materials, structure-property relationship
1. Introduction
There is a growing need for new concepts in surgical wound closure due to limitations associated with invasive surgical closure techniques such as sutures and staples.[1–3] Medical adhesives and sealants that form in situ, many of which are approved for human clinical use, offer less invasive alternatives to conventional surgical closure techniques.[4–6] Several medical sealants are based on native proteins, for example fibrin glue and chemically cross-linked albumin.[4–7] While protein-based gels currently enjoy widespread use, their limitations include the possibility for disease transmission, allergic reactions, and poor mechanical properties.[6,8,9] As a result of these shortcomings, several synthetic surgical adhesives have been developed, including cyanoacrylates and hydrogels based on polymers such as poly(ethylene oxide) (PEO).[10–20] Cyanoacrylates exhibit excellent mechanical performance but their widespread use for internal procedures is limited by toxicity concerns.[10–12] PEO-based hydrogels, such as FocalSeal®, CoSeal®, and DuraSeal®, have satisfactory mechanical performance, are non-immunogenic, and have been used in cardiovascular,[13,14] pulmonary,[15,16] and dural[17,18] surgical procedures, among others.[19,20]
Swelling due to water absorption is a general feature of chemically cross-linked hydrophilic polymer networks.[21] The equilibrium swelling behavior of a polymer hydrogel is a reflection of the polymer-solvent interaction parameter, polymer architecture, extent of cross-linking, and polymer volume fraction.[22] In the context of in-situ forming medical adhesives, rapid covalent cross-linking of an aqueous polymer solution generally yields polymer hydrogels that are prone to significant swelling upon immersion into excess water.[23,24] For PEO-based medical adhesives, observed swelling values range from 30 % to >700 %.[23,25,26] The consequences of swelling on the mechanical performance of tissue adhesives are underappreciated in the literature, as standard adhesion test methods often probe adhesion strength under non-equilibrium swelling conditions.[27] Swelling of medical adhesives and sealants in the minutes and hours following deployment in vivo can lead to severe medical complications such as local nerve compression.[28–30]
One possible approach to preventing swelling of polymer hydrogel tissue adhesives is to employ thermosensitive polymers.[31–35] Block copolymers of PPO and PEO, including commercially available multi-arm block copolymers composed of central PPO blocks and peripheral PEO blocks (Tetronic®), exhibit interesting thermosensitive behavior due to the hydrophilic-to-hydrophobic transition of the PPO block that occurs by mild warming.[31–34] Previous reports of chemically cross-linked Tetronic® hydrogels for cell encapsulation and tissue adhesion have appeared in the literature,[31,36–44] though systematic studies of the relationship between chemical cross-linking, thermal transition, and mechanical properties in the context of medical adhesion have not been undertaken.
Herein, we describe the synthesis and characterization of in-situ forming polymer hydrogels with controllable swelling, good adhesion to soft tissue, and high mechanical robustness. Polymer gels were based on a branched amphiphilic PPO-PEO block copolymer terminated with catechols. The terminal catechol groups serve both an adhesive (interfacial) and cohesive (cross-linking) function, as they do in mussel adhesive proteins. This strategy has been employed in other mussel-mimetic adhesive hydrogels based on catechol-modified PEO, which have been evaluated in numerous in vitro, in vivo, and ex vivo studies.[25,26,45–48] Covalently cross-linked hydrogels were characterized by swelling, rheological, bulk compressive, and adhesive studies. These hydrogels exhibited controlled swelling and improved mechanical properties compared to similar PEO-based systems. Negative swelling systems with high mechanical toughness resulted from rapid chemical cross-linking followed by thermal equilibration, and a conceptual model is proposed for understanding the role of network structure in the observed mechanical properties.
2. Results
2.1. Oscillatory Rheometry
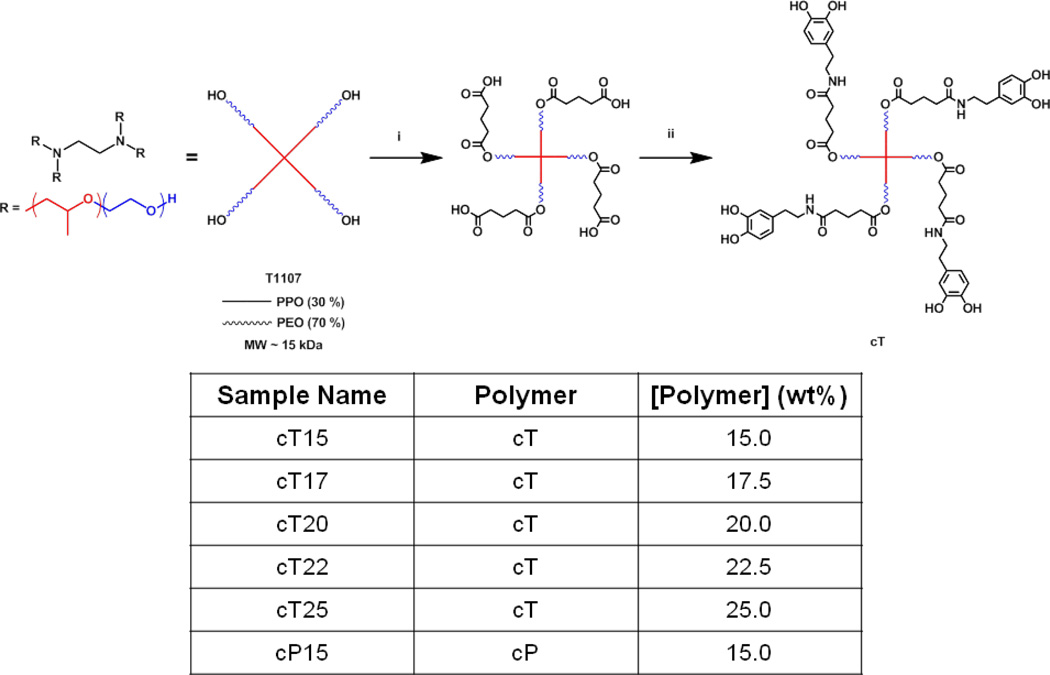
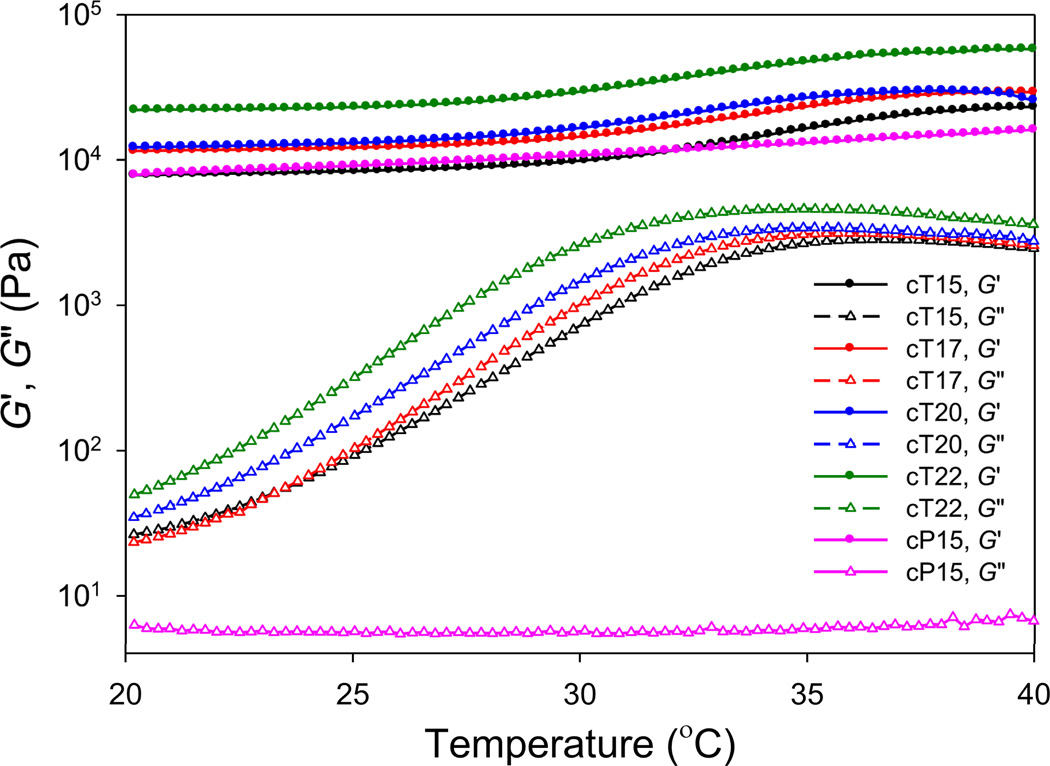
Solutions of catechol-modified Tetronic® (cT) in 2x phosphate-buffered saline (PBS) and NaIO4 in water (7/1 v/v) were mixed to induce cross-linking (catechol:IO4− of 2:1) and added to the rheometer. Gels with final cT concentrations of 150, 175, 200, or 225 mg/mL are designated cT15, cT17, cT20, and cT22, respectively (Figure 1). Covalent cT gels were then studied by rheology as a function of polymer content and temperature. Periodate-induced gelation occurred quickly (< 30 s) at 20 °C C in all cases, as evidenced by the fact that we were unable to record the cross-over point between the storage (G′) and loss (G″) moduli. The storage modulus increased rapidly in the first several minutes of reaction and approached a plateau within ten minutes, with the value of the plateau modulus increasing with cT concentration (Supporting Figure S1). The thermosensitive behavior of cT gels was analyzed by forming gels in situ within the rheometer at 20 °C, followed by monitoring G′ and G″ during a temperature sweep from 20–40 °C (Figure 2).G′ of cT gels increased approximately 2.5-fold between 30 and 37 °C, and G″ displayed a dramatic (~100-fold) increase over a wider temperature range (20–35 °C).
Figure 1.
Synthesis of catechol-modified Tetronic® (cT) and composition of hydrogels investigated in this study. (i) glutaric anhydride, pyridine; (ii) dopamine, HBTU, TEA. In all gels, the catechol:IO4− ratio was 2:1.
Figure 2.
Temperature dependence of the storage (G′, closed symbols) and loss (G″, open symbols) moduli of cT gels.
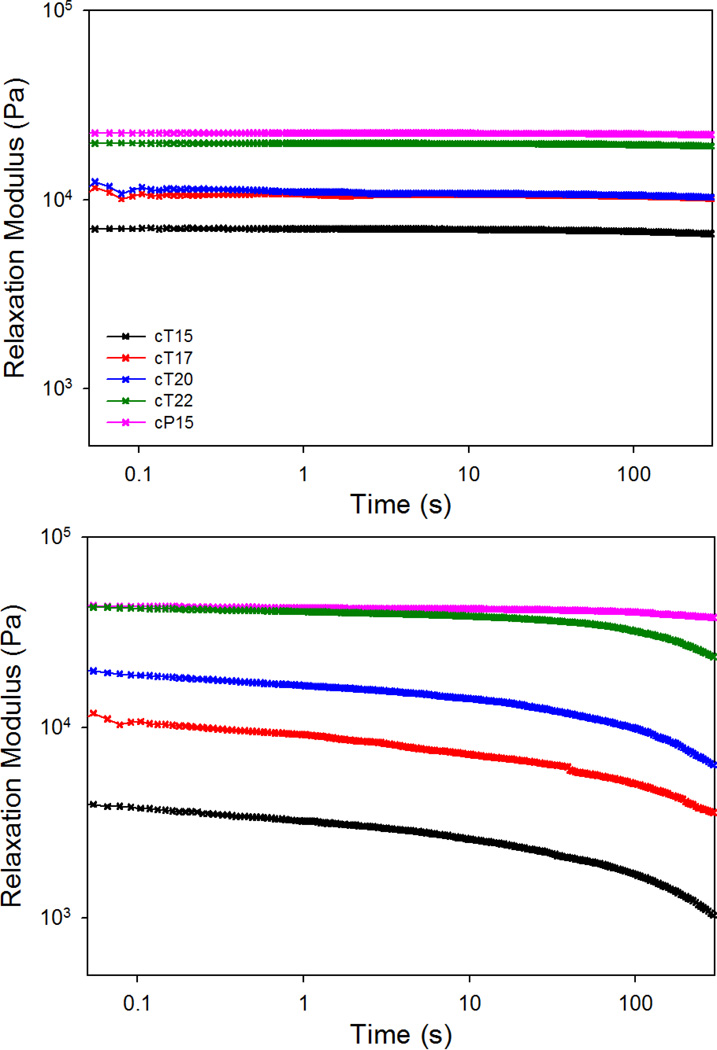
Considering the increase in G″ as evidence of viscous effects at high temperature, we next probed the frequency-dependent behavior using frequency sweep and step-strain (relaxation) experiments. As seen in Supporting Figure S2, cT gels probed at 20 °C appear to behave as elastic solids as judged by their frequency-independent behavior with G′ ≫G″. Step-strain experiments, in which the decay of modulus was monitored at constant strain (10 %), revealed little stress relaxation in cT hydrogels at 20 °C (Figure 3). This property was shared by a control gel composed of PEG (cP15) and is consistent with covalently cross-linked elastic networks.
Figure 3.
Step-strain relaxation experiments showing the decay of modulus with time for cT and cP gels at 20 °C (top) and 40 °C (bottom). The legend applies to both the top and bottom panels.
Frequency sweeps of cT gels conducted at 40 °C revealed only slight frequency-dependent behavior at high angular frequency (> 1 rads/s). However, a viscous response became increasingly apparent at very low angular frequencies (< 0.3 rads/s) (Supporting Figure S2), though G′ was greater than G″ at all angular frequencies tested. The relaxation behavior of cT gels was more evident in step-strain experiments conducted at 40 °C (Figure 3), in which the storage moduli (here, called relaxation moduli) of cT15, cT17, cT20, and cT22 gels decayed to 26, 30, 32, and 55 % of initial value within 5 min, respectively. This behavior was in stark contrast to cP15 cross-linked in an identical manner, which displayed minimal decrease in relaxation modulus at 40 °C (~13 %) over the same amount of time.
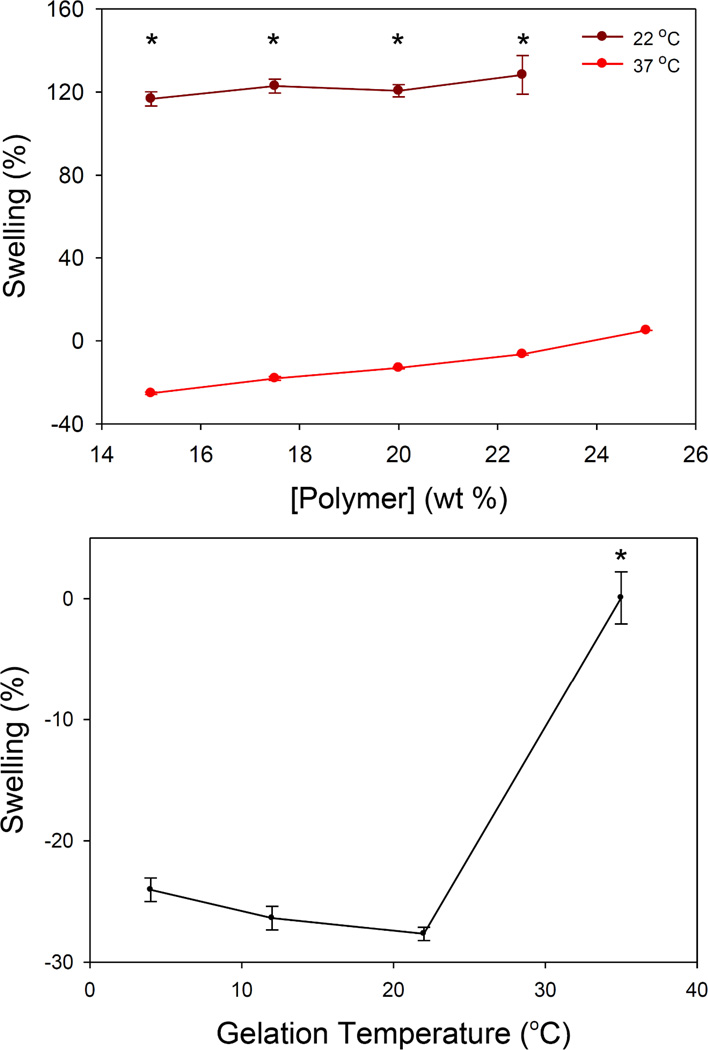
2.2. Gel Swelling
Swelling of cT samples was studied in 1x PBS at 22 °C and 37 °C (Figure 4, Supporting Table S1-S2) for up to 7 days. In almost all cases, equilibrium was reached after 1 day. At 22 °C, cT gels swelled between 110 % and 140 % over a 7-d study, which is considerably greater than the swelling of cP15 (50–60 %). At 37 °C, cT hydrogels exhibited concentration-dependent negative swelling (contraction) (Figure 4). After 7 d at 37 °C, cT15, cT17, cT20, cT22, and CT25 showed swelling values of approximately −25, −18, −13, −7, and +4 %, respectively. A fit of the plot of cT concentration as a function of swelling at 37 °C was highly linear (r2 ≈ 0.98), providing a guideline for tailoring gel swelling/contraction behavior through cT concentration. In contrast, gels based on catechol-modified PEG (cP) swelled 30–50 % at physiological temperature. Equilibrium swelling of cP gels was lower at 37 °C than at room temperature, which we attribute to the proximity of our experimental conditions (37 °C, high ionic strength) to the lower critical solution temperature (LCST) of PEO.[49,50]
Figure 4.
Swelling of cT gels as a function of polymer concentration (top) and gel formation temperature (bottom). cT15 was studied in the temperature-based experiments (bottom panel). * indicates statistical significance (p < 0.001) between 22 and 37 °C (top) and between samples cross-linked at 37 °C and all other temperatures (bottom).
A second swelling test probed the influence of gelation temperature on 37 °C swelling of cT15 gels. Precursor solutions were equilibrated to 4, 12, 22, or 35 °C before mixing, and were cured at the same temperature for 18 h. After being removed from molds, cT15 samples were swelled for 24 h in PBS at 37 °C. Samples that were cross-linked at 4, 12, or 22 °C swelled approximately −25 % (Figure 4). However, gels that were equilibrated and cured at 35 °C displayed no swelling or contraction.
2.3. Compression Testing
The bulk mechanical properties of cT gels were studied by loading hydrogel cylinders in compression up to 90 % strain (the compression limit of our equipment), followed by unloading. Both loading and unloading data were recorded, and elastic moduli were estimated from the initial portion of the loading curves (<5 % strain). At room temperature and in the unswollen state, cP15 gel had a compression modulus of 99 kPa, whereas cT gels had moduli in the range of 28–83 kPa (Table 1). All unswollen cT gels were superior to cP gels in terms of extensibility and strength; cT gels survived compressive stresses of 3.4–4.3 MPa and 90 % strain without damage, whereas cP15 gels failed at 76 % strain and 1.0 MPa UCS.
Table 1.
Bulk Mechanical Properties of Adhesive cT Hydrogels
| Sample Notes | Sample | Compressive Modulus (kPa) |
Maximum Stress (MPa) |
Strain at Failure (%) | Relative Energy Dissipated (%) |
|---|---|---|---|---|---|
| As-made and tested at 22 °C |
cT15 | 28.2±8.4 | 3.4±0.9 | >90a | NCb |
| cT17 | 55.7±3.6 | 4.3±0.2 | >90a | NCb | |
| cT20 | 63.6±17.6 | 4.3±0.2 | >90a | NCb | |
| cT22 | 83.4±10.0 | 4.2±0.4 | >90a | NCb | |
| cP15 | 99.0±9.7 | 1.0±0.6 | 76.1±2.8 | NCb | |
| Equilibrated for 24 h and tested in 37 °C PBS |
cT15 | 92.2±13.2 | 1.0±0.02 | >90a | 38.2±0.6 |
| cT17 | 116.9±10.9 | 1.0±0.04 | >90a | 34.0±4.2 | |
| cT20 | 165.1±41.3 | 1.3±0.05 | >90a | 29.3±4.0 | |
| cT22 | 195.4±32.6 | 1.3±0.1 | >90a | 37.2±4.9 | |
| cP15 | 114.7±10.8 | 0.8±0.1 | 82.5±3.1 | NAc |
cT samples did not fail when compressed to 90 % strain;
not calculated;
Energy dissipation calculations could not be performed for cP samples because failure occurred before unloading curve was observed.
At physiological temperature in the swollen state (24 h in PBS), the compression moduli of cT gels increased with cT concentration, ranging from 92, 117, 165, and 195 kPa for cT15, cT17, cT20, and cT22, respectively. These values were substantially higher than the same samples at 22 °C in the unswollen state (Table 1). cT hydrogels were able to withstand 90 % compression at 37 °C in the equilibrium swollen state (Supporting Figure S3), though the maximum stresses at 90 % strain (~1 MPa) were significantly less than at room temperature (~3–4 MPa). In contrast, the mechanical behavior of cP15 at 37 °C in the swollen state (modulus of 115 kPa, 0.8 MPa UCS, 83 % strain at failure) was not significantly different compared to the unswollen state at 22 °C.
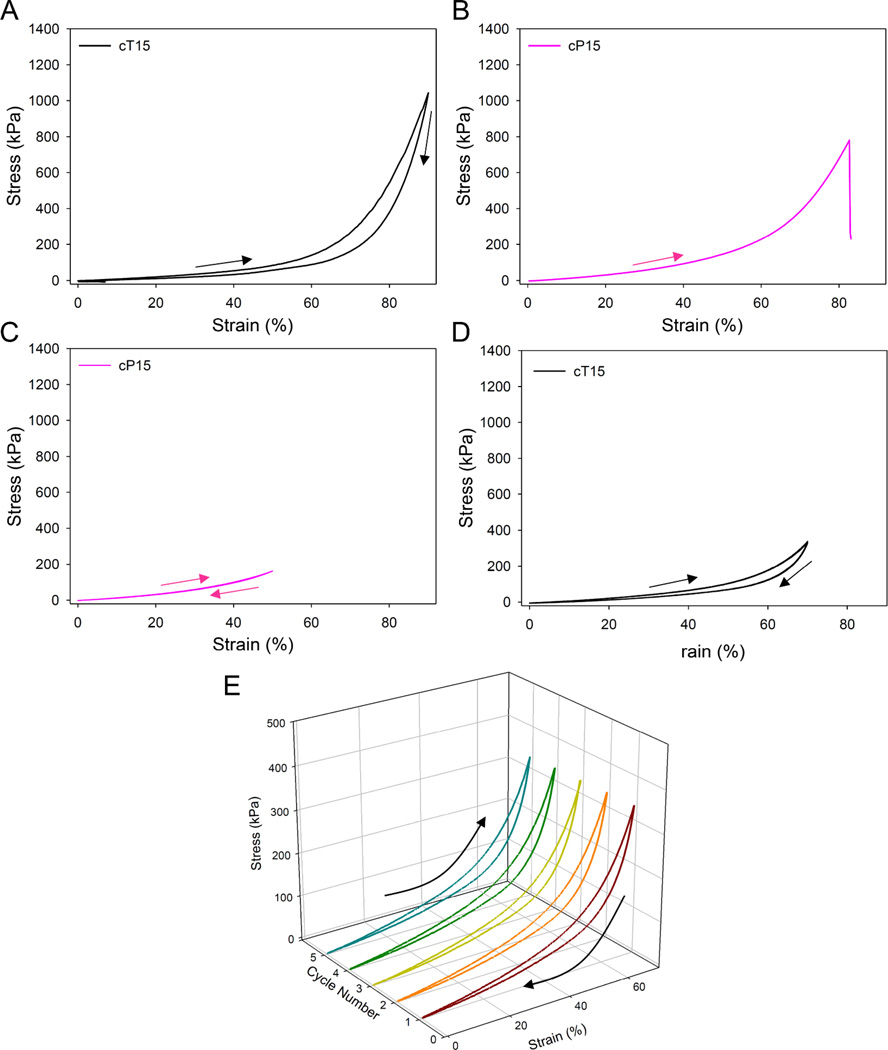
For cT gels in particular, a notable feature of the bulk mechanical behavior was the presence of significant hysteresis between the loading and unloading portions of the stress-strain curves (Figure 5, Supporting Figure S4). Hysteresis was particularly evident in the highly nonlinear region from 50–90 % strain. Differences between the area under the curve (AUC) for the loading and unloading curves provided a measure of energy dissipation during deformation,[51] which was found to be in the range 23–29 %. Stress-strain curves of cT gel samples subjected to multiple loading/unloading cycles in succession nearly perfectly overlapped (Figure 5 and Supporting Figure S5), providing further evidence of the lack of damage induced by severe compression loading of cT gels.
Figure 5.
Bulk compression of 15 % gels at 37 °C. Gels were equilibrated at physiological temperature for 24 h and then loaded in compression up to 90 % strain at constant temperature. The loading and unloading portion of the curves are identified with arrows. (A) cT15 gels survived 90 % strain without rupture, while (B) cP15 gels ruptured at ~80 % strain. (C) Compression loading of cP15 to 50 % followed by unloading revealed no hysteresis between loading and unloading portions of the curve. (D, E) Gels were repeatedly loaded in compression up to 70 % strain at constant temperature. Successive compression cycles are shown superimposed (D) and separated (E).
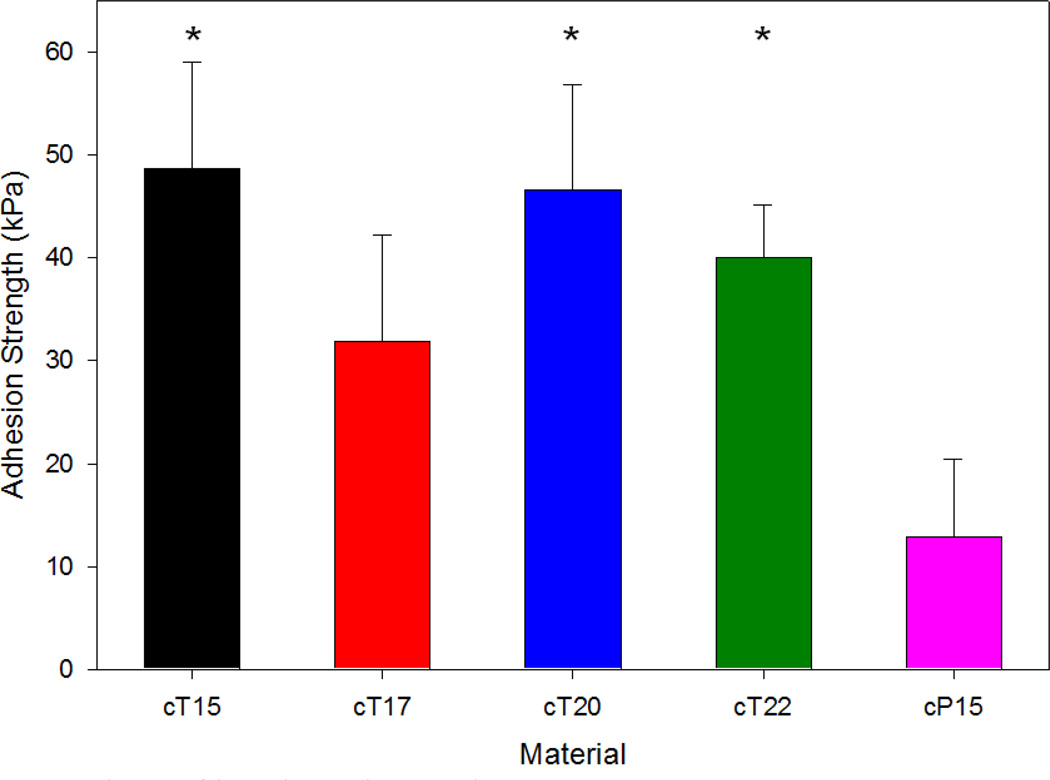
2.4. Tissue Adhesion
The ability of cT hydrogel to mechanically adhere hydrated tissue surfaces together was studied via lap shear testing with decellularized porcine dermis. Samples of cT15, cT17, cT20, and cT22, cured for 1 h in PBS at 37 °C, demonstrated lap shear adhesive strengths of 48.7, 31.9, 46.6, and 40.0 kPa, respectively (Figure 6). Adhesives of cP15 were also tested, yielding a lap shear adhesion strength of ~13 kPa, which is significantly less than previously studied formulation based on catechol-modified PEO.[25,52]
Figure 6.
Comparison of lap shear tissue adhesion performance. Samples were immersed in 1x PBS for 1 h at 37 °C and then tested wet. * represents statistical significance (p < 0.05) relative to cP15.
3. Discussion
Our lab, as well as others, have recently investigated mussel-mimetic hydrogels based on catechol modified polymers,[25,45,46,53–55] with in vitro, in vivo, and ex vivo studies demonstrating significant potential for use as medical adhesives and sealants.[26,46–48] The choice to use catechol-based chemistry is motivated by the discovery that marine mussels, which can attach to virtually any surface (organic or inorganic), use protein-based glues that contain 3,4-dihydroxy-L-phenylalanine (DOPA), a catechol-containing amino acid.[56,57] The most impressive aspect of these biological adhesives is that they are able to successfully function in aqueous environments that often cause the failure of other glues.[58,59] DOPA is particularly abundant at the interface between the adhesive foot pad and the substrate,[60–62] an observation that has resulted in significant speculation about the role of DOPA in the adhesive bonding of mussels. Additionally, oxidized DOPA residues and DOPA-DOPA oligomers are thought to play important cohesive roles in the cross-linking reactions that lead to solidification of secreted adhesive precursors.[63,64] Our approach to designing medical adhesives, though significantly more simplistic than the natural mussel adhesive proteins, takes advantage of both the cohesive and adhesive capabilities of catechols. Oxidative cross-linking by IO4− has been used in the past to form gels from catechol polymers by oxidizing catechols to reactive o-quinones that are capable of covalent coupling with catechols, amines, thiols, imidazoles, etc.
PEO has been employed as a polymer building block for approved medical sealants and a number of experimental formulations due to its long history of use in approved medical sealants, other medical devices, and pharmaceutical formulations.[5,46,65,66] However, most experimental and commercially available PEO-based hydrogels experience extensive swelling and suffer from mechanical weakness in the swollen state.[23,24,26] As these characteristics can lead to significant medical complications,[28–30] we aimed to circumvent these shortcomings by designing a zero- or negative-swelling, mechanically robust medical adhesive. More specifically, we sought to exploit the thermal transition associated with hydrophobic PPO blocks in PPO-PEO copolymers to induce gel contraction as a means to modulate the mechanical and swelling behavior. PPO is known to undergo a thermally induced transition from hydrophilic to hydrophobic in aqueous systems,[67,68] leading to a collapse of PPO into hydrophobic domains at modest temperatures (Supporting Figure S6). In the case of linear PPO-PEO block copolymers (Pluronic®), thermally induced micelle formation occurs in water-based solutions in order to minimize exposure of hydrophobic segments to water.[69–71] In highly concentrated solutions, the thermal transition induces physical gelation.[70,71] Tetronic® polymers, on the other hand, have four linear PPO-PEO arms emanating from a tetrafunctional ethylenediamine core (Figure 1). Concentrated aqueous solutions of Tetronic® also undergo physical gelation at temperatures in the 20–35 °C range due to the hydrophobic transition associated with the PPO segments.[31–34] A number of studies have previously reported chemically cross-linked Tetronic® gels prepared by polymerization of terminal reactive functional groups.[31,36–44]
In their ground-breaking work, Tirelli and coworkers have reported a ‘tandem’ method of gelling thermosensitive polymers that combines both thermal and chemical gelation.[42,43] The tandem method, first described for Pluronic® polymers[42] and later for Tetronic® [43] as a mild means of cell encapsulation, relies on rapid thermal gelation of highly concentrated polymer solutions followed by chemical polymerization. Tandem cross-linked Pluronic® gels exhibited thermosensitive (LCST) properties and swelled >200 % in pure water, though less in PBS.[42] Highly concentrated solutions of Tetronic® (30 wt%) thermally gel at ~20–21 °C, allowing tandem formation of Tetronic® gels by rapid thermal gelation followed by slower chemical cross-linking.[43] Tandemly processed Tetronic® gels have been recently explored as tissue sealants, exhibiting decreased swelling and modest increases in tissue adhesion compared to PEO-based counterparts.[44] However, negative swelling gels were not reported. Catechol-modified linear PPO-PEO copolymers have also been explored by our lab in the past, but not in the context of negative swelling adhesives.[72]
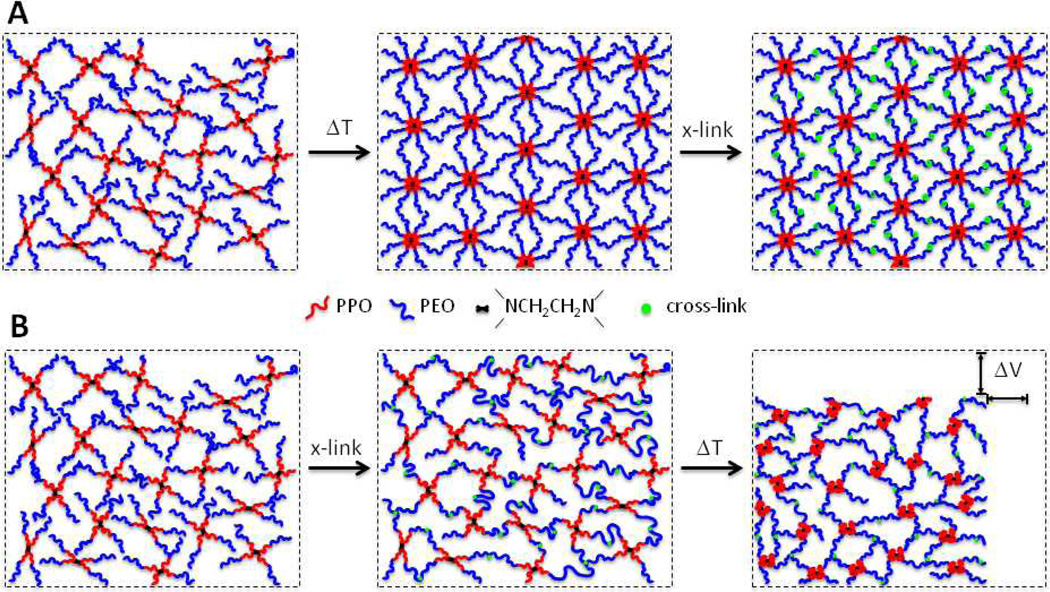
We hypothesized that a negative-swelling thermosensitive polymer adhesive could be realized by avoiding widespread thermal gelation before chemical cross-linking through careful management of polymer composition and concentration, chemical cross-linking rate, and temperature. Thus, borrowing the terminology of Tirelli and coworkers, we employed an inverse ‘tandem’ method (Figure 7). Our method acknowledges a few key practical aspects associated with medical adhesive/sealant deployment in the clinic. First, we recognized that most medical sealants and adhesives are deployed at room temperature and are desired to solidify rapidly – instantaneously, a few seconds, or, at most, tens of seconds – upon contact with tissue. Secondly, the temperature of tissue surfaces during many clinical procedures is variable and can be significantly less than core body temperature, introducing an element of uncertainty with respect to methods requiring an increase in temperature for solidification of the adhesive.
Figure 7.
Schematic illustration of chemically cross-linked PPO-PEO block copolymer thermoresponsive gels (not drawn to scale), demonstrating the significance of controlling the sequence of thermal transition and chemical cross-linking. (A) In the ‘tandem’ method of Cellesi et al.,[42,43] chemical cross-linking occurs after thermal equilibration. (B) In the present method, chemical cross-linking of cT is intended to occur prior to thermal equilibration, producing a PPO-PEO block copolymer network. Subsequent warming induces thermal transition of the PPO segments from hydrophilic to hydrophobic, producing volumetric shrinkage and toughening of the network.
Taking these practical aspects of medical adhesion into consideration, we sought to develop a system wherein rapid cross-linking chemistry coupled with subsequent thermal transition would give rise to negative swelling and enhanced mechanical properties. The oxidative mussel-mimetic catechol cross-linking chemistry met the desired cross-linking requirement due to the rapid rate of cross-linking upon mixing catechol polymers with a chemical oxidant.[45] The PPO block in Tetronic® provides the thermosensitivity due to a hydrophilic-to-hydrophobic transition with increasing temperature, as evidenced by a decrease of more than four orders of magnitude in critical micellization concentration (CMC) in the temperature range of 15–40 °C.[73] Xu et al. has shown that a PPO core block of 33 repeat units undergoes self-association into micelles at 25 °C.[74] In our case, the PPO block length is shorter (~19 repeat units), giving rise to a moderately higher thermal transition. This facilitates the progression of chemical cross-linking prior to thermal equilibration to body temperature. Once chemical cross-linking gives rise to integration of hydrophilic PPO segments into the network, thermal self-association of PPO into hydrophobic domains is expected to result in negative swelling due to hydrophobic collapse (Figure 7). Additionally, we surmised that collapsed hydrophobic PPO domains present in the network at elevated temperatures could act as energy dissipating domains that deform under applied load, leading to enhanced toughness (Supporting Figure S7).[75–78]
Synthesis of catechol-modified PPO-PEO block copolymer (cT) proceeded in a facile manner from commercial Tetronic® 1107 using a glutarate linker, HBTU activation, and dopamine (Figure 1). Gelation of a cT solution by IO4− was rapid, as the cross-over point of G′ and G″ was not visible in the time sweeps of cT samples. Further rheological analysis of these hydrogels revealed unique, temperature-dependent behavior. For example, cT gels stiffened significantly upon heating from 20 to 40 °C (Figure 2), a result that is consistent with thermomechanical behavior of chemically cross-linked Tetronic® gels[39] and with the formation of hydrophobic PPO domains within the same temperature range.[73,74] It is notable that G″ increased dramatically over this temperature range, indicative of energy dissipation arising from hydrophobic PPO domains.
Frequency sweep and step-strain experiments conducted at 20 and 40 °C revealed additional thermoresponsive behavior (Figure 3 and Supporting Figure S2). At room temperature, cT gels exhibited frequency-independent behavior, consistent with a covalently cross-linked network and similar to an identically cross-linked cP gel composed of PEO. However, cT gels show frequency-dependent moduli and significant relaxation when heated to 40 °C. Such behavior was not observed in the PEO-based cP gels. This was most apparent in the step-strain relaxation experiments, in which the gel was exposed to a constant strain while changes in the relaxation modulus are monitored with time. cP gel modulus exhibited minimal relaxation (~13 %) in this experiment, whereas cT gel moduli relaxed up to 74 % in a concentration-dependent manner. We hypothesize that the temperature-dependent viscous behavior of cT hydrogels is based on the thermosensitive solubility of PPO in aqueous conditions.[67,68]
The thermosensitivity of cT gels, and the contrasting behavior in comparison with PEO-based gels, was also apparent in swelling tests. It was interesting to note that, at room temperature, cP15 swelled much less than all cT gels over a 7-d study (Figure 4, Supporting Table S1 and S2). We believe that this observation can be explained by the fact that each arm in the cT precursor is ~50 % larger by weight relative to cP and that PPO segments retained hydrophilic character at room temperature. Therefore, if we assume that the cross-linking reaction proceeds to an equivalent conversion in both cases, the cT gels would have a larger molecular weight between cross-links, explaining the higher swelling at room temperature. When swelling studies were conducted at 37 °C, both cT and cP gels displayed a reduction in the extent of swelling, presumably due to the LCST of PEO[49,50] and PPO-PEO.[69–71] At 37 °C, cP15 swelled ~50 %, whereas cT contracted 7–25 % in a concentration-dependent manner (Figure 4).
Previous reports of gels designed from covalently linked 4-arm PPO-PEO copolymers describe various levels of swelling and contraction at 37 °C.[36,43,44] We believe the origin of these disparities to be related to differences in the PPO aggregation state at the time of cross-linking, arising from differences in relative rates of chemical gelation versus thermal gelation/micellization. Supporting this hypothesis, a second set of swelling tests involved forming cT gels at 4, 12, 22, or 35 °C for 18 h and then measuring swelling at 37 °C after 24 h. Swelling was found to be greatly affected by the gelation temperature (Figure 4). For cT gels formed at or below room temperature, in which PPO domains remain hydrophilic, negative swelling was observed at 37 °C. This result is consistent with the notion that hydrophobic collapse of PPO domains induced by warming to 37 °C resulted in volumetric contraction by ~25 %. In contrast, using a method that is analogous to the ‘tandem’ gelation method (thermally induced gelation followed by chemical cross-linking), gels formed at 35 °C did not demonstrate negative swelling after 1 day at 37 °C. This result is consistent with previous reports,[43,44] and can be understood to be a consequence of the hydrophobic state of PPO prior to cross-linking (no further hydrophobic PPO collapse is possible to induce network contraction and negative swelling). In practice, the rate of chemical cross-linking and thermal equilibration on gelation cannot be easily isolated from one another in this system. Ultimately, swelling during in-vivo deployment will be greatly affected by the preparation temperature of the precursors, the tissue temperature at the site of adhesive deployment, the volume of adhesive applied, and the rate of ester hydrolysis as the network degrades.
Previous investigations of the mechanical behavior of chemically cross-linked Tetronic® gels have been limited to rheological or macroscopic measurements of stiffness.[36,39,43] As expected, our rheological and bulk mechanical compression experiments revealed increases in modulus of cT gels when heated above room temperature (Figure 2 and Table 1). This stiffening was realized without sacrificing extensibility, as all cT hydrogels survived 90 % compression and maximum stresses of ~1 MPa; in contrast, cP gels failed at lower maximum strain and stress.
However, the existence of significant relaxation of cT gels at 40 °C (Figure 3) has not been previously reported and suggested more complicated mechanical behavior, perhaps involving viscous energy dissipation mechanisms connected to the presence of hydrophobic PPO domains present within the gel network. Indeed, significant mechanical hysteresis was observed at 37 °C in the bulk compression curves of cT gels, but not in cP gels (Figure 5, Supporting Figure S4). We hypothesize that this behavior is at least partially caused by the presence of hydrophobic domains in cT gels, whose formation is driven by the thermally induced collapse of PPO segments. A possible explanation for the mechanical hysteresis involves disruption of the hydrophobic domains when the covalently linked cT network is strained, revealing hidden length[79] by force-induced elongation of polymer chains (Supporting Figure S7). Similar behavior is a key feature of several biological tissues, such as tendon and cartilage, where the viscoelastic response of these tissues is very important in energy dissipation and load transfer.[80–83] Stress-strain plots of cT gel samples subjected to several successive loading and unloading cycles perfectly overlapped (Figure 5, Supporting Figure S5), indicating a high level of robustness and resistance to damage under extreme loading conditions.
Finally, the performance of cT and cP gels as tissue adhesives was investigated (Figure 6). In order to probe adhesive performance shortly after application, tissue samples were bonded together using either cT or cP gels and allowed to cure at 37 °C for 1 h while fully submerged in PBS; this method is in contrast to protocols that call for longer (2–24 h) cross-linking periods and/or minimally hydrated environments.[25,44,52] Although we found no clear trends of lap shear strength with respect to cT concentration, all cT gel concentrations tested (15–22.5 wt%) outperformed cP samples. cT gels exhibited adhesion strengths of 31–49 kPa, 2.5–4 times greater than that of cP15 (12.7 kPa). Interestingly, one of the strongest adhesives (cT15) also exhibited the greatest degree of contraction (negative swelling), suggesting that negative swelling does not compromise adhesion strength.
Although our highest lap shear adhesive strength (49 kPa) is well above the mean value recently reported by Cho et al. for a chemically cross-linked Tetronic® adhesive formed by the tandem method,[44] comparisons must be approached with caution due to the use of different test methodologies, cross-linking chemistries and tissues. Our own experiences have led us to believe that key parameters affecting results include the method of incubation during the curing period and the swelling state of the adhesive (equilibrium or nonequilibrium). To illustrate this, we can make some comparisons with other catechol-modified PEO adhesive systems from our lab due to their structural similarity to cP and utilization of the same cross-linking chemistry involving catechol oxidation.[25,52] Previously, we achieved adhesion strengths of cP-like gels in the range of 30–35 kPa for gels incubated in a humid atmosphere;[25,52] in the present study, we incubated cP-bonded tissue samples in PBS at 37 °C during the 1-h curing period and achieved an adhesion strength of only ~13 kPa. Although the gels are unlikely to achieve equilibrium (negative) swelling within 1 h even with full immersion in PBS, the current results nevertheless suggest that the adhesion strength of PEO-based materials is significantly weakened by swelling in an aqueous environment. In contrast, the adhesion strength of cT gel remained high under full immersion conditions, implying that the mechanical strength of cT gels may be retained under equilibrium swelling conditions.
4. Conclusion
We have described the synthesis and characterization of mussel-inspired hydrogel adhesives that combine biologically inspired covalent adhesive chemistry with a thermally sensitive block copolymer. The resulting polymer gels possess covalent catechol-catechol cross-links between branched PPO-PEO block copolymers. This network is augmented by thermosensitive transitions of PPO blocks, which exhibit a hydrophobic collapse upon heating to physiological temperature. Chemical cross-linking using rapid catechol oxidation chemistry at or below room temperature followed by warming to body temperature, resulted in hydrophobic collapse of PPO domains and contraction of the gel. Through variation of polymer concentration and gel formation temperature, swelling could be systematically controlled in the range of zero to −25 %. Rheological experiments showed that the gel stiffened above the PPO thermal transition. Strength and toughness of the gels was greater than those of analogous PEO-based gels, with PPO-PEO block copolymer gels surviving 90 % compression and exhibiting significant mechanical hysteresis between loading and unloading curves. Finally, the tissue adhesive potential was demonstrated through lap shear adhesion measurements of decellularized porcine dermis, producing bond strengths greater than PEO-based adhesives. This novel class of thermosensitive biomaterials represents a facile and versatile synthetic route to strong hydrogels, enhancing the adhesion strength of mussel-inspired polymer hydrogels.
5. Experimental Section
Materials
Tetronic® 1107 (T1107, MW ≈ 15 kDa; 30 wt% PPO, 70 wt% PEO) was a generous gift from BASF (Florham Park, NJ). PEO (4-arm, MW ≈ 10 kDa) was purchased from JenKem Technology USA, Inc. (Allen, TX). 2-(1H-benzotriazole-1-yl)-1,1,3,3-tetramethyluronium hexafluorophosphate (HBTU) was purchased from Chem-Impex International (Wood Dale, IL). Sodium meta-periodate (NaIO4) and glutaric anhydride (GA) were purchased from Sigma-Aldrich (Milwaukee, WI). Dopamine hydrochloride (DA), triethylamine (TEA), 4-nitrophenyl chloroformate (4NPC), dichloromethane (DCM), dimethylformamide (DMF), tetrahydrofuran (THF), and methanol (MeOH) were purchased from Fisher Scientific (Philadelphia, PA). All chemicals were used without further purification. Dehydrated and decellularized porcine dermis was a gift from Kensey Nash Corporation (Exton, Pa).
Synthesis of catechol-Tetronic® (cT)
T1107 (10 g) and glutaric anhydride (5x mol. equiv. relative to –OH) were added to a two-neck round-bottom flask, which was then purged with Ar. Anhydrous chloroform (70 mL) and THF (20 mL) were added. The solids were stirred until fully dissolved. Pyridine (5x mol. equiv. relative to –OH) was added, and the reaction was refluxed under Ar for ~18 h. The reaction solution was then washed with brine and water, dried with MgSO4, filtered, and concentrated under reduced pressure. The glutarate-modified T1107 intermediate was precipitated in ether and dried under vacuum overnight.
Purified glutarate-modified T1107 was dissolved in DCM (50 mL) and DMF (50 mL). DA (1.2x mol. equiv. relative to –COOH) was added and completely dissolved. HBTU (1.2x mol. equiv. relative to –COOH) was added and completely dissolved. TEA (2.5x mol. equiv. relative to –COOH) was added, and the reaction was stirred for 1.5 h before being concentrated under reduced pressure. The polymer was precipitated in acidified ether, dried under vacuum overnight, and dissolved in ~100 mL of 12.1 mM HCl. The solution was filtered, dialyzed (3500 MWCO) against water at pH 4 for 24 h, dialyzed against MilliQ water for 4 h, frozen at −80 °C, and lyophilized. The final cT polymer was obtained as a white solid and stored under Ar at −20 °C until needed. The percent conversion was ~90 %, as determined by 1H NMR (Supporting Figure S8).
Synthesis of catechol-PEO (cP)
cP was synthesized by adding 10 g PEO to a two-neck round-bottom flask, which was purged with Ar. Anhydrous DCM (80 mL) was added to dissolve the PEO. TEA (2.5x mol. equiv. relative to –OH) was added, and the solution was stirred for 15 min. Separately, 4NPC (2.5x mol. equiv. relative to –OH) was dissolved in anhydrous DCM (20 mL) and slowly added to the PEO solution. The reaction was allowed to proceed for ~18 h at room temperature in an inert environment of Ar. The volume was reduced by rotary evaporation, and the activated PEO (4PEO-NPC) was collected by precipitation in cold ether and −20 °C MeOH (2x). The product was then dried under vacuum overnight.
Purified 4PEO-NPC was combined with 90 mL of a 2:1 (v/v) solution of DMF and DCM. Once dissolved, DA (2.5x mol. equiv. relative to –NPC) was added. When the solution was homogeneous, the reaction was activated by the addition of TEA (2.5x mol. equiv. relative to –NPC) and stirred for ~18 h. The volume was reduced by rotary evaporation, and the PEO was collected by precipitation in acidified cold ether and acidified MeOH at −20 °C. The product was then dried under vacuum overnight and dissolved in ~100 mL of 12.1 mM HCl. The solution was filtered, dialyzed (3500 MWCO) against water at pH 4 for 24 h, dialyzed against MilliQ water for 4 h, frozen at −80 °C, and lyophilized. The final purified cP was obtained as a white solid and stored under Ar at −20 °C until needed. The percent conversion was ~90 %, as determined by 1H NMR (Supporting Figure S9).
Hydrogel Formation
Solutions of cT in 2x PBS and NaIO4 in water (7/1 v/v) were mixed thoroughly (by vortex or in a syringe) at room temperature such that the final polymer concentration was 150, 175, 200, or 225 mg/mL and the catechol:IO4− was 2:1 (Figure 1). Hydrogels of cP were formed by combining equal volumes of 300 mg/mL cP in 2x PBS and 12 mg/mL NaIO4 in water at room temperature.
Rheometry
Rheological characterization was performed on an Anton Paar MCR 300 rheometer with a CP 25-2 fixture (25 mm diameter, 2° cone angle), peltier hood, and an evaporation shield. Solutions of IO4− and either cT or cP were mixed as above (except that cP was dissolved in 2x PBS at pH 7.0) and added as a liquid onto the rheometer baseplate. The fixture was brought down into contact with the liquid mixture as quickly as possible. For all samples, the following tests were performed in sequence: time test (20 Pa shear stress, 10 rads/s, 20 °C), frequency sweep (5 % strain, 100 rads/s to 0.1 rads/s, 20 °C), relaxation experiment (10 % strain, 20 °C, stress monitored for ~300 s), temperature sweep (5 % strain, 10 rads/s, 20 °C to 40 °C, 1 °C/min), frequency sweep (5 % strain, 100 rads/s to 0.1 rads/s, 40 °C), relaxation experiment (10 % strain, 40 °C, stress monitored for ~300 s).
Swelling of Hydrogels
Two sets of swelling experiments were conducted on pre-formed gels. In the first method, gels were formed as described above by introducing liquid precursor mixture into a polytetrafluoroethylene mold and allowing the gel to solidify for 15 minutes at room temperature. Gel samples were removed from the molds, weighed and immersed in 1x PBS at room temperature or 37 °C for 1, 2, 3, or 7 d. At specified time points, samples were removed from PBS, blotted to remove excess surface water, and weighed.
In the second set of swelling experiments, precursor solutions for cT15 samples were equilibrated for 30 min at either 4, 12, 22, or 35 °C. Gels were then formed as described above by introducing liquid precursor mixtures into a polytetrafluoroethylene mold. Gels were allowed to solidify for 18 h at the same temperatures used to equilibrate precursor solutions. Gel samples were then removed from the molds, weighed, and immersed in 1x PBS at 37 °C. After 1 d, samples were removed from PBS, blotted to remove excess surface water, and weighed.
Swelling (Q) was calculated by
| (1) |
where mf and mi represent the initial and final mass of the hydrogels, respectively. Three replicates were performed and the average value was reported.
Bulk Compression Testing of Adhesive Hydrogels
Compression tests were conducted on a Sintech 20/G mechanical tester equipped with a 1000-lb load cell. Cylindrical gels (~5 mm diameter, ~10 mm height) were formed as described above by introducing liquid precursors into a polytetrafluoroethylene mold and allowing the gel to solidify for 15 minutes at room temperature. Gel samples were removed from the molds and tested in the unswollen state or after swelling for 24 h at 37 °C. Samples were strained to 90 % at a crosshead speed of 10 mm/min at room temperature in air or 37 °C in 1x PBS. Compressive moduli were calculated by determining the slope of the first 5 % of the stress-strain curve. Ultimate compressive stress (UCS) and failure strain were defined as the largest stress and strain values recorded before samples failed. The AUC for both loading and unloading portions of the curve were estimated by the rectangle method in MATLAB. Energy dissipation was calculated by
| (2) |
where AUCL and AUCU represent the areas under the loading and unloading curves, respectively. Three trials were performed and the average value was reported.
Lap-Shear Testing
The performance of cT hydrogels as tissue adhesives was analyzed in a lap shear test based on ASTM standard F2255-05.[27] Dehydrated and decellularized porcine dermis was reconstituted for >1 h in 1x PBS and cut to size (2.5 cm × 2.0 cm). Tissue substrates were glued onto aluminum fixtures using cyanoacrylate glue (Permabond 268, Permabond, Pottstown, PA) and cured for 1 h at 37 °C, keeping the fixture wrapped in PBS-soaked gauze to prevent dehydration of the tissue. The gel precursors were mixed as described above and 100 µL of the adhesive solution was applied to the tissue surface. A second tissue sample on an aluminum fixture was immediately brought into contact with the adhesive, achieving an overlapping (adhesive bonded) area of approximately 2.5 cm × 1.0 cm. A 100-g weight was placed on the fixture assembly for ~15 min, after which test samples were submerged for 1 h in 1x PBS at 37 °C. Immediately prior to tensile testing, samples were removed from the water bath, and the area of substrate overlap was measured using digital calipers. Samples were strained until failure in lap shear on a Sintech 20/G mechanical tester equipped with a 1000-lb load cell at 37 °C with a cross-head speed of 5 mm/min.
Statistical Analysis
Statistical significance was conducted with IBM SPSS Statistics software by a one-way analysis of variance (ANOVA) with a Bonferroni post-hoc test.
Supplementary Material
Acknowledgements
The authors thank Mark Seniw, Tadas Sileika, and Dr. Dominic Fullenkamp for insightful discussions. Compression experiments made use of Central Facilities supported by the MRSEC program of the National Science Foundation (DMR-0520513) at the Northwestern University Materials Research Science and Engineering Center. This work was supported by grants from the NIH. DGB was partially supported by the IBNAM-Baxter Early Career Development Award in Bioengineering. GGB is grateful for a McCormick Summer Research Award from Northwestern University.
Footnotes
Supporting Information
Supporting Information is available online from the Wiley Online Library or from the author.
Contributor Information
Dr Devin G. Barrett, Biomedical Engineering Department Chemistry of Life Processes Institute Institute for Bionanotechnology in Medicine Northwestern University Evanston, IL 60208, USAd-barrett@northwestern.edu.
Grace G. Bushnell, Biomedical Engineering Department Chemistry of Life Processes Institute Northwestern University Evanston, IL 60208, USA
Phillip B. Messersmith, Biomedical Engineering Department Materials Science and Engineering Department Chemical and Biological Engineering Department Chemistry of Life Processes Institute Institute for Bionanotechnology in Medicine Robert H. Lurie Comprehensive Cancer Center Northwestern University Evanston, IL 60208, USAphilm@northwestern.edu.
References
- 1.Kjaergard HK. The American Journal of Surgery. 2001;182:S15. doi: 10.1016/s0002-9610(01)00772-3. [DOI] [PubMed] [Google Scholar]
- 2.Lau H. Ann. Surg. 2005;242:670. doi: 10.1097/01.sla.0000186440.02977.de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwab R, Willms A, Kröger A, Becker H. Hernia. 2006;10:272. doi: 10.1007/s10029-006-0080-8. [DOI] [PubMed] [Google Scholar]
- 4.Ryou M, Thompson CC. Techniques in Gastrointestinal Endoscopy. 2006;8:33. [Google Scholar]
- 5.Peng HT, Shek PN. Expert Rev. Med. Devices. 2010;7:639. doi: 10.1586/erd.10.40. [DOI] [PubMed] [Google Scholar]
- 6.Seyednejad H, Imani N, Jamieson T, Seifalian AM. Br. J. Surg. 2008;95:1197. doi: 10.1002/bjs.6357. [DOI] [PubMed] [Google Scholar]
- 7.Jackson MR. The American Journal of Surgery. 2001;182:S1. [Google Scholar]
- 8.Joch C. Cardiovasc. Surg. 2003;11:23. doi: 10.1016/S0967-2109(03)00068-1. [DOI] [PubMed] [Google Scholar]
- 9.Klimo PJ, Khalil A, Slotkin JR, Smith ER, Scott RM, Goumnerova LC. Neurosurgery. 2007;60:305. doi: 10.1227/01.NEU.0000255416.55560.D2. [DOI] [PubMed] [Google Scholar]
- 10.Leggat PA, Smith DR, Kedjarune U. ANZ J. Surg. 2007;77:209. doi: 10.1111/j.1445-2197.2007.04020.x. [DOI] [PubMed] [Google Scholar]
- 11.Mattamal GJ. Expert Rev. Med. Devices. 2008;5:41. doi: 10.1586/17434440.5.1.41. [DOI] [PubMed] [Google Scholar]
- 12.Achneck HE, Sileshi B, Jamiolkowski RM, Albala DM, Shapiro ML, Lawson JH. Ann. Surg. 2010;251:217. doi: 10.1097/SLA.0b013e3181c3bcca. [DOI] [PubMed] [Google Scholar]
- 13.Glickman M, Gheissari A, Money S, Martin J, Ballard JL. Arch Surg. 2002;137:326. doi: 10.1001/archsurg.137.3.326. [DOI] [PubMed] [Google Scholar]
- 14.Napoleone CP, Valori A, Crupi G, Ocello S, Santoro F, Vouhé P, Weerasena N, Gargiulo G. Interact. Cardiovasc. Thorac. Surg. 2009;9:978. doi: 10.1510/icvts.2009.212175. [DOI] [PubMed] [Google Scholar]
- 15.Ranger WR, Halpin D, Sawhney AS, Lyman M, Locicero J. The American surgeon. 1997;63:788. [PubMed] [Google Scholar]
- 16.Allen MS, Wood DE, Hawkinson RW, Harpole DH, McKenna RJ, Walsh GL, Vallieres E, Miller DL, Nichols Iii FC, Smythe WR, Davis RD. The Annals of Thoracic Surgery. 2004;77:1792. doi: 10.1016/j.athoracsur.2003.10.049. [DOI] [PubMed] [Google Scholar]
- 17.Cosgrove GR, Delashaw JB, Grotenhuis JA, Tew JM, van Loveren H, Spetzler RF, Payner T, Rosseau G, Shaffrey ME, Hopkins LN, Byrne R, Norbash A. J. Neurosurg. 2007;106:52. doi: 10.3171/jns.2007.106.1.52. [DOI] [PubMed] [Google Scholar]
- 18.Than KD, Baird CJ, Olivi A. Neurosurgery. 2008;63:182. doi: 10.1227/01.neu.0000335034.08274.d2. [DOI] [PubMed] [Google Scholar]
- 19.Park EL, Ulreich JB, Scott KM, Ullrich NPF, Linehan JA, French MH, Ho WY, White MJN, Talley JR, Fellah AM, Ramakumar S. The Journal of Urology. 2004;172:2446. doi: 10.1097/01.ju.0000138159.69642.d9. [DOI] [PubMed] [Google Scholar]
- 20.Ufret R, Yu S-Y, Christoforidis J, D'Amico DJ. Invest Ophthalmol Vis Sci. 2004;45:U767. doi: 10.1167/iovs.03-0414. [DOI] [PubMed] [Google Scholar]
- 21.Kim SW, Bae YH, Okano T. Pharm. Res. 1992;9:283. doi: 10.1023/a:1015887213431. [DOI] [PubMed] [Google Scholar]
- 22.Peppas NA, Hilt JZ, Khademhosseini A, Langer R. Adv. Mater. 2006;18:1345. [Google Scholar]
- 23.Bennett SL, Driscoll A, Sawhney AS, editors. In Vitro Testing. Mansfield, MA: Covidien Laboratories; 2007. P. K. Campbell Evaluation of Absorbable Surgical Sealants: In Vitro Testing. [Google Scholar]
- 24.Azadani AN, Matthews PB, Ge L, Shen Y, Jhun C-S, Guy TS, Tseng EE. The Annals of Thoracic Surgery. 2009;87:1154. doi: 10.1016/j.athoracsur.2008.12.072. [DOI] [PubMed] [Google Scholar]
- 25.Brubaker CE, Messersmith PB. Biomacromolecules. 2011;12:4326. doi: 10.1021/bm201261d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mehdizadeh M, Weng H, Gyawali D, Tang L, Yang J. Biomaterials. 2012;33:7972. doi: 10.1016/j.biomaterials.2012.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.ASTM F2255-05 (2010) Standard Test Method for Strength Properties of Tissue Adhesives in Lap-Shear by Tension Loading. ASTM International; West Conshohocken, PA: 2010. www.astm.org. [Google Scholar]
- 28.Blackburn Sl, Smyth MD. Journal of Neurosurgery: Pediatrics. 2007;106:302. [Google Scholar]
- 29.Mulder M, Crosier J, Dunn R. Spine. 2009;34:E144. doi: 10.1097/BRS.0b013e31818d5427. [DOI] [PubMed] [Google Scholar]
- 30.Thavarajah D, De Lacy P, Hussain R, Redfern RM. Spine. 2010;35:E25. doi: 10.1097/BRS.0b013e3181b9fc45. [DOI] [PubMed] [Google Scholar]
- 31.Garty S, Kimelman-Bleich N, Hayouka Z, Cohn D, Friedler A, Pelled G, Gazit D. Biomacromolecules. 2010;11:1516. doi: 10.1021/bm100157s. [DOI] [PubMed] [Google Scholar]
- 32.Go DH, Joung YK, Lee SY, Lee MC, Park KD. Macromol Biosci. 2008;8:1152. doi: 10.1002/mabi.200800098. [DOI] [PubMed] [Google Scholar]
- 33.Alvarez-Lorenzo C, Gonzalez-Lopez J, Fernandez-Tarrio M, Sandez-Macho I, Concheiro A. Euro J Pharm Biopharm. 2007;66:244. doi: 10.1016/j.ejpb.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 34.Chiappetta DA, Facorro G, Rubin de Celis E, Sosnik A. Nanomedicine NBM. 2011;7:624. doi: 10.1016/j.nano.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 35.You Z, Cao H, Gao J, Shin PH, Day BW, Wang Y. Biomaterials. 2010;31:3129. doi: 10.1016/j.biomaterials.2010.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sosnik A, Sefton MV. Journal of Biomedical Materials Research Part A. 2005;75A:295. doi: 10.1002/jbm.a.30419. [DOI] [PubMed] [Google Scholar]
- 37.Sosnik A, Sodhi RNS, Brodersen PM, Sefton MV. Biomaterials. 2006;27:2340. doi: 10.1016/j.biomaterials.2005.11.028. [DOI] [PubMed] [Google Scholar]
- 38.Park KM, Joung YK, Park KD. Tissue Eng A. 2008;14:849. [Google Scholar]
- 39.Park KM, Shin YM, Joung YK, Shin H, Park KD. Biomacromolecules. 2010;11:706. doi: 10.1021/bm9012875. [DOI] [PubMed] [Google Scholar]
- 40.Park KM, Jun I, Joung YK, Shin H, Park KD. Soft Matter. 2011;7:986. [Google Scholar]
- 41.Park KM, Lee Y, Son JY, Oh DH, Lee JS, Park KD. Biomacromolecules. 2012;13:604. doi: 10.1021/bm201712z. [DOI] [PubMed] [Google Scholar]
- 42.Cellesi F, Tirelli N, Hubbell JA. Macromol. Chem. Phys. 2002;203:1466. [Google Scholar]
- 43.Cellesi F, Tirelli N, Hubbell JA. Biomaterials. 2004;25:5115. doi: 10.1016/j.biomaterials.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 44.Cho E, Lee JS, Webb K. Acta Biomater. 2012;8:2223. doi: 10.1016/j.actbio.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee BP, Dalsin JL, Messersmith PB. Biomacromolecules. 2002;3:1038. doi: 10.1021/bm025546n. [DOI] [PubMed] [Google Scholar]
- 46.Brubaker CE, Kissler H, Wang LJ, Kaufman DB, Messersmith PB. Biomaterials. 2010;31:420. doi: 10.1016/j.biomaterials.2009.09.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bilic G, Brubaker C, Messersmith PB, Mallik AS, Quinn TM, Haller C, Done E, Gucciardo L, Zeisberger SM, Zimmermann R, Deprest J, Zisch AH. Am J Obstet Gynecol. 2010;202:85.e1. doi: 10.1016/j.ajog.2009.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Haller CM, Buerzle W, Brubaker CE, Messersmith PB, Mazza E, Ochsenbein-Koelble N, Zimmermann R, Ehrbar M. Prenat. Diagn. 2011;31:654. doi: 10.1002/pd.2712. [DOI] [PubMed] [Google Scholar]
- 49.Saeki S, Kuwahara N, Nakata M, Kaneko M. Polymer. 1976;17:685. [Google Scholar]
- 50.Kjellander R, Florin E. Journal of the Chemical Society, Faraday Transactions 1: Physical Chemistry in Condensed Phases. 1981;77:2053. [Google Scholar]
- 51.Lv S, Dudek DM, Cao Y, Balamurali MM, Gosline J, Li H. Nature. 2010;465:69. doi: 10.1038/nature09024. [DOI] [PubMed] [Google Scholar]
- 52.Burke SA, Ritter-Jones M, Lee BP, Messersmith PB. Biomed Mater. 2007;2:203. doi: 10.1088/1748-6041/2/4/001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lee Y, Chung HJ, Yeo S, Ahn C-H, Lee H, Messersmith PB, Park TG. Soft Matter. 2010;6:977. [Google Scholar]
- 54.Ryu JH, Lee Y, Kong WH, Kim TG, Park TG, Lee H. Biomacromolecules. 2011;12:2653. doi: 10.1021/bm200464x. [DOI] [PubMed] [Google Scholar]
- 55.Holten-Andersen N, Harrington MJ, Birkedal H, Lee BP, Messersmith PB, Lee KYC, Waite JH. Proc Natl Acad Sci USA. 2011;108:2651. doi: 10.1073/pnas.1015862108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Waite JH. J. Biol. Chem. 1983;258:2911. [PubMed] [Google Scholar]
- 57.Lee BP, Messersmith PB, Israelachvili JN, Waite JH. Annu. Rev. Mater. Res. 2011;41:99. doi: 10.1146/annurev-matsci-062910-100429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Waite JH. Int. J. Adhes. Adhes. 1987;7:9. [Google Scholar]
- 59.Anderson TH, Yu J, Estrada A, Hammer MU, Waite JH, Israelachvili JN. Adv. Funct. Mater. 2010;20:4196. doi: 10.1002/adfm.201000932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Waite JH, Tanzer ML. Science. 1981;212:1038. doi: 10.1126/science.212.4498.1038. [DOI] [PubMed] [Google Scholar]
- 61.Papov VV, Diamond TV, Biemann K, Waite JH. J. Biol. Chem. 1995;270:20183. doi: 10.1074/jbc.270.34.20183. [DOI] [PubMed] [Google Scholar]
- 62.Waite JH, Qin XX. Biochemistry (Mosc.) 2001;40:2887. doi: 10.1021/bi002718x. [DOI] [PubMed] [Google Scholar]
- 63.Yu ME, Hwang JY, Deming TJ. J. Am. Chem. Soc. 1999;121:5825. [Google Scholar]
- 64.Burzio LA, Waite JH. Biochemistry (Mosc.) 2000;39:11147. doi: 10.1021/bi0002434. [DOI] [PubMed] [Google Scholar]
- 65.Artzi N, Shazly T, Crespo C, Ramos AB, Chenault HK, Edelman ER. Macromol. Biosci. 2009;9:754. doi: 10.1002/mabi.200800355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Strehin I, Nahas Z, Arora K, Nguyen T, Elisseeff J. Biomaterials. 2010;31:2788. doi: 10.1016/j.biomaterials.2009.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Malcolm GN, Rowlinson JS. Transactions of the Faraday Society. 1957;53:921. [Google Scholar]
- 68.Sandell LS, Goring DAI. Journal of Polymer Science Part A-2: Polymer Physics. 1971;9:115. [Google Scholar]
- 69.Schmolka I. J. Am. Oil Chem. Soc. 1977;54:110. [Google Scholar]
- 70.Alexandridis P, Holzwarth JF, Hatton TA. Macromolecules. 1994;27:2414. [Google Scholar]
- 71.Alexandridis P, Alan Hatton T. Colloids and Surfaces A: Physicochemical and Engineering Aspects. 1995;96:1. [Google Scholar]
- 72.Huang K, Lee BP, Ingram DR, Messersmith PB. Biomacromolecules. 2002;3:397. doi: 10.1021/bm015650p. [DOI] [PubMed] [Google Scholar]
- 73.Wanka G, Hoffmann H, Ulbricht W. Macromolecules. 1994;27:4145. [Google Scholar]
- 74.Xu J, Ge Z, Zhu Z, Luo S, Liu H, Liu S. Macromolecules. 2006;39:8178. [Google Scholar]
- 75.Abdurrahmanoglu S, Can V, Okay O. Polymer. 2009;50:5449. [Google Scholar]
- 76.Matsuda A, Kaneko T, Gong J, Osada Y. Macromolecules. 2000;33:2535. [Google Scholar]
- 77.Zhang C, Aung A, Liao L, Varghese S. Soft Matter. 2009;5:3831. [Google Scholar]
- 78.Tuncaboylu DC, Sari M, Oppermann W, Okay O. Macromolecules. 2011;44:4997. [Google Scholar]
- 79.Fantner GE, Oroudjev E, Schitter G, Golde LS, Thurner P, Finch MM, Turner P, Gutsmann T, Morse DE, Hansma H, Hansma PK. Biophys. J. 2006;90:1411. doi: 10.1529/biophysj.105.069344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Taylor DC, Dalton JD, Seaber AV, Garrett WE. The American Journal of Sports Medicine. 1990;18:300. doi: 10.1177/036354659001800314. [DOI] [PubMed] [Google Scholar]
- 81.Johnson GA, Tramaglini DM, Levine RE, Ohno K, Choi N-Y, Woo L-YS. J. Orthop. Res. 1994;12:796. doi: 10.1002/jor.1100120607. [DOI] [PubMed] [Google Scholar]
- 82.Hayes WC, Mockros LF. J. Appl. Physiol. 1971;31:562. doi: 10.1152/jappl.1971.31.4.562. [DOI] [PubMed] [Google Scholar]
- 83.Mak AF. J. Biomech. Eng. 1986;108:123. doi: 10.1115/1.3138591. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.