Video abstract
Video
Keywords: femtosecond laser precision, bladeless LASIK, corneal flap diameter, flap thickness, Alcon/WaveLight FS200, clear cone, patient interface, applanation cone, myopic laser correction, hyperopic laser correction
Abstract
Purpose
To evaluate the safety and efficacy of a novel LASIK flap patient interface (PI) cone with our reported digital analysis and compare for potential differences with the standard metal and glass PI in flap parameters when used with the Alcon/WaveLight FS200 femtosecond laser.
Patients and methods
Thirty-six consecutive LASIK patients (72 eyes) subjected to a bilateral femtosecond assisted LASIK procedure with the novel clear cone PI FS200 1505 were examined for flap diameter and flap thickness over the entire flap area via digital analysis performed on intraoperation image (flap diameter) and anterior-segment optical coherence tomography image (flap thickness). This group was compared with an age- and procedure-matched group B from our practice, in which the standard metal and glass PI was employed.
Results
Horizontal flap diameter for group A (clear cone) was 7.87 mm ± 0.02 mm (range 7.89–7.84 mm) for 8.00 mm programmed, whereas for group B (metal and glass cone) was 7.85 mm ± 0.04 mm (range 7.93–7.80 mm). Likewise, along the vertical line, flap diameter for group A was 7.84 mm ± 0.02 mm (range 7.85–7.80 mm) and for group B was 7.83 mm ± 0.03 mm (range 7.87–7.80 mm). Central flap thickness for group A was 113.29 μm (±1.19 μm) for 110 μm planned, 122.1 μm (±2.10 μm) for 120 μm planned, and 133.50 μm (±0.71 μm) for 130 μm planned. Group B central flap thickness was, accordingly, 112.8 μm (±1.25 μm), 122.4 μm (±2.15 μm), and 132.50 μm (±0.90 μm). The data evaluated (paired group comparisons) between group A and group B did not show statistically significant differences.
Conclusion
This study indicates that two PIs in use with the FS200 femtosecond laser are safe and have highly reproducible and accurate flap parameter results, such as achieved diameter and flap thickness. The paired group comparisons between the two PIs’ respective data do not show statistically significant differences.
Introduction
A very precise optical path control system is a prerequisite in all femtosecond ophthalmic surgical platforms, in order to precisely and accurately focus the successive laser pulses to their programmed positions within the cornea.1,2 For that purpose, the cornea is maintained to a defined shape via suction pressure facilitated by a patient interface (PI) or applanation cone. The patient interface for most femtosecond lasers is a flat clear surface that applanates the patient’s cornea surface in order to achieve a reliable separation plane for LASIK flap creation. Some systems use a concave interface with less applanation required.3 With the exception of intraocular pressure increase during flap creation,4 very little has been published in the peer review literature regarding these critical elements in femtosecond refractive surgery.
The Alcon/WaveLight® FS200 1505 PI (Alcon Surgical, Fort Worth, TX, USA) is a clear cone interface that has recently been introduced by the manufacturer. It carries the advantages of having a lower cost and high reproducibility, it is recyclable, and it offers a wider intraoperative field of view for the surgeon.
It is sterile and patient contact disposable (ie, intended for single use), consisting of a tubing system with integrated suction ring and an applanation cone. The flat bottom of the cone is used as an applanation plate for the patient’s cornea. The interface is indicated to be used with the FS200 femtosecond laser, consistent with the cleared indications for use for this refractive surgical laser.
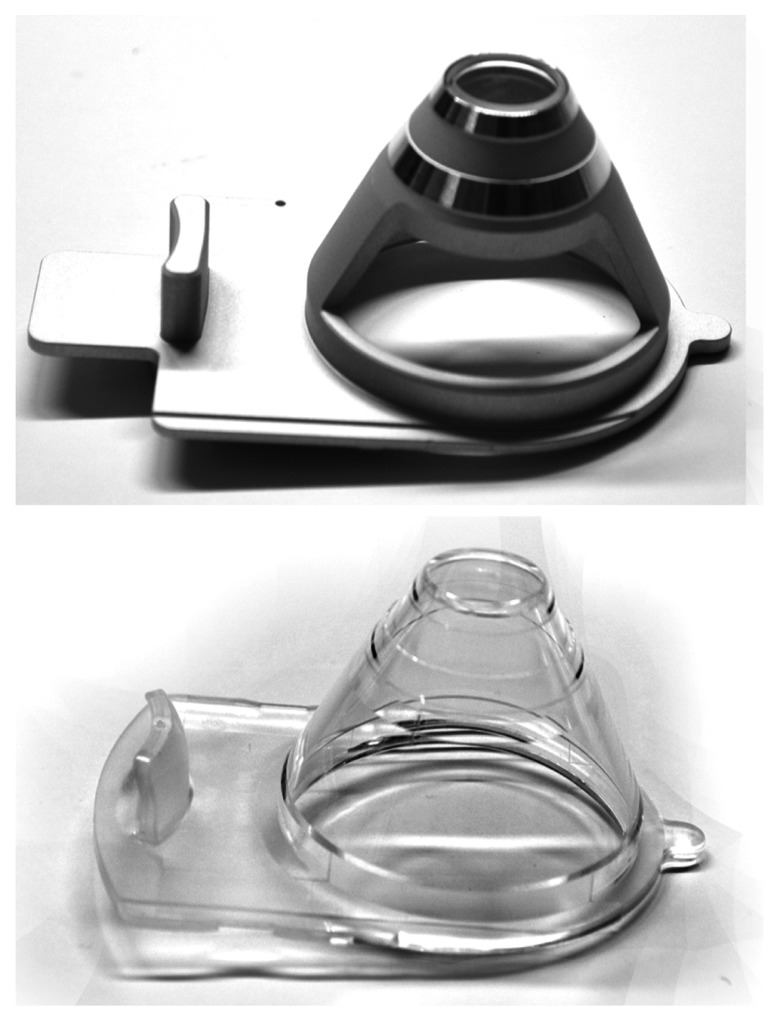
The standard metal device was the interface 1504, the main differences being in the applanation cone. The applanation cone of the predicate device 1504 consists of a metal and glass cone with a bonded glass plate, whereas the applanation cone in interface 1505 is a one-piece molded plastic cone (Figure 1). We have recently implemented the use of clear cone interface 1505 in our practice.
Figure 1.
The Alcon/WaveLight® FS200 patient interfaces 1504 (metal and glass, top) and 1505 (clear cone, bottom).
In an effort to validate flap precision and accuracy, our team has introduced a digital analysis flap diameter technique during the LASIK operation and prior to flap lifting,5 as well as a flap thickness study,6 examining the FS200 flap thickness characterization achieved with the interface 1504.
The purpose of this paper is to compare the differences in achieved flap diameter and thickness precision and accuracy created via the FS200 femtosecond laser with the recently introduced clear cone interface 1505 versus the metal and glass cone interface 1504 in the FS200 femtosecond laser.
Materials and methods
This case series study received approval by the ethics committee of our institution, adherent to the tenets of the Declaration of Helsinki. Informed consent was obtained from each subject at the time of the LASIK intervention or the first clinical visit. The study was conducted in our clinical practice on patients during the refractive operation and scheduled postoperative visits.
Patient inclusion criteria
The study group consisted of 36 consecutive patients (72 eyes) treated for bilateral primary myopic or hyperopic femtosecond assisted LASIK between October 2012 and January 2013 in our center using the interface 1505, forming the clear cone group A. Mean preoperative spherical equivalent for this group A was −4.23 D ± 1.22 D. Of the 72 flaps in the group, as shown in Table 1, the majority subgroup (48 flaps) were programmed to 8.00 mm diameter, whereas 22 flaps were programmed to 8.50 mm diameter, and two flaps were programmed to 9.50 mm diameter.
Table 1.
Intended diameters of the flaps studied comparing the two groups
| Clear cone group | Metal and glass cone group | |||
|---|---|---|---|---|
|
|
|
|||
| N-T | S-I | N-T | S-I | |
| Programmed 8.00 mm | ||||
| No of eyes: 48 | ||||
| Average | 7.87 | 7.84 | 7.85 | 7.83 |
| SD | 0.02 | 0.02 | 0.04 | 0.03 |
| Maximum | 7.89 | 7.85 | 7.93 | 7.87 |
| Minimum | 7.84 | 7.80 | 7.80 | 7.80 |
| Programmed 8.50 mm | ||||
| No of eyes: 22 | ||||
| Average | 8.43 | 8.42 | 8.38 | 8.39 |
| SD | 0.03 | 0.02 | 0.03 | 0.02 |
| Maximum | 8.48 | 8.46 | 8.43 | 8.41 |
| Minimum | 8.39 | 8.41 | 8.34 | 8.34 |
| Programmed 9.50 mm | ||||
| No of eyes: 2 | ||||
| Average | 9.58 | 9.56 | 9.56 | 9.56 |
| SD | 0.03 | 0.03 | 0 | 0 |
| Maximum | 9.60 | 9.58 | 9.56 | 9.56 |
| Minimum | 9.56 | 9.54 | 9.56 | 9.56 |
Notes: N-T, horizontal plane along the nasal-temporal line; S-I, coronal plane along the superior-inferior line. All units in mm.
A second group of 36 patients (72 eyes) was randomly selected from a pool of patients previously treated (between March 2012 and October 2012) for bilateral primary myopic or hyperopic femtosecond assisted LASIK in our center using the interface 1504, with the intent to match the programmed flap diameter population of the study group A. This group formed the metal and glass cone reference group B. Mean preoperative spherical equivalent for this group B was −4.15 D ± 1.34 D.
In all procedures (performed by the same surgeon [AJK]), the LASIK flap was created with the Alcon/Wave- Light FS200 femtosecond laser, and subsequent excimer ablation was provided by the Alcon/WaveLight EX500 excimer laser.7,8
The femtosecond laser settings were as follows: stromal bed cut spot separation 8 μm, line separation 8 μm, side cut bed separation 5 μm, line separation 3 μm, bed cut pulse energy 0.80 μJ, and side cut pulse energy 0.80 μJ.
Imaging and measurement
Intraoperative images were collected from the applanated corneas using the documentation software, a feature of the Alcon/WaveLight Refractive Suite WaveNet system. These images are created by default during the refractive procedure, stored in the system software, and are available for documentation. Digital analysis of such images provided the methodology of flap diameter, as presented in detail in our previous work.5 Flap diameter was thus measured for the horizontal plane (X) along the nasal-temporal line (N-T), as well as for the vertical line of the coronal plane (Y) along the superior-inferior line (S-I).
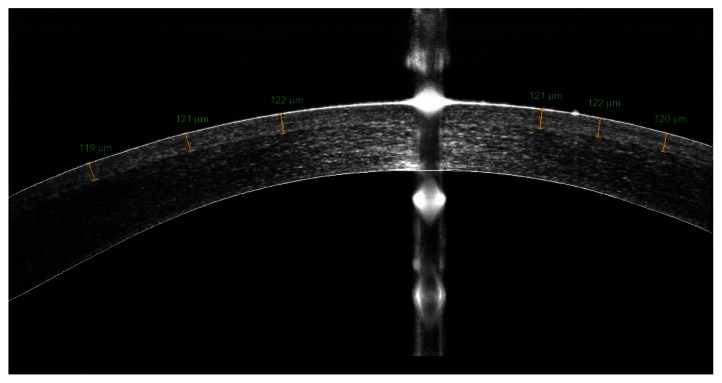
Flap central thickness was evaluated 1 week postoperatively by means of anterior-segment optical coherence tomography (AS-OCT), specifically the OptoVue RTVue (OptoVue Inc, Fremont, CA, USA) system, using the L-Cam lens, a 6 mm-long high-resolution cross-line scan, centered at the pupil center. The meridional cross-sectional images were processed via the RTVue software Version A6 (9,0,27). Flap thickness was measured (via the caliper tool) as the average of four thickness measurements in the 0–3 mm central corneal zone (example shown in Figure 2).
Figure 2.
Measurement of flap thickness from the high-resolution meridional scan provided by the anterior-segment optical coherence tomography system.
Note: The specific flap was programmed to 120 μm of thickness.
Linear regression analysis was performed to seek possible correlations of intended versus achieved flap dimensions. Descriptive statistics (average, minimum, maximum, standard deviation, and range), comparative statistics, and linear regression were performed in Microsoft Excel 2010 (Microsoft Corp, Redmond, WA, USA) and Origin Lab Version 9.0 Build b45 (OriginLab Corp, Northampton, MA, USA). Analysis of variance between groups was performed via the Origin Lab statistics tool.
Results
Subjects’ ages for group A at the time of the operation were (average ± standard deviation) 28.7 years ± 6.6 years, range 41–18, whereas for group B they were 29.6 years ± 7.8 years, range 44–17.
Flap diameter predictability
As stated in the Materials and methods section, flap diameter was measured digitally along two meridian lines, the horizontal along the nasal-temporal line and the vertical along the superior-inferior line. The reading error for each measurement was ±1 pixel, which corresponds, based on the resolution of the original images and subsequent conversion, as described in our previous publication,5 to ±0.05 mm of accuracy.
As reported in Table 1, within group A (clear cone), the flap diameter along the N-T line was 7.87 mm ± 0.02 mm (range 7.89–7.84 mm) for 8.00 mm programmed, whereas within group B (metal and glass cone) was 7.85 mm ± 0.04 mm (range 7.93–7.80 mm). Likewise, along the vertical line, diameter was 7.84 mm ± 0.02 mm (range 7.85–7.80 mm) and 7.83 mm ± 0.03 mm (range 7.87–7.80 mm).
Similar results were obtained for the 8.50 mm programmed flap thickness. With a sample of 22 eyes for each group, the diameter along the N-T line was measured for group A as 8.43 mm ± 0.03 mm (range 8.48–8.39 mm) and for group B as 8.38 mm ± 0.03 mm (range 8.43–8.34 mm). Along the S-I line, the measured flap diameter for group A was 8.42 mm ± 0.02 mm (range 8.46–8.41 mm) and for group B was 8.39 mm ± 0.02 mm (range 8.41–8.34 mm).
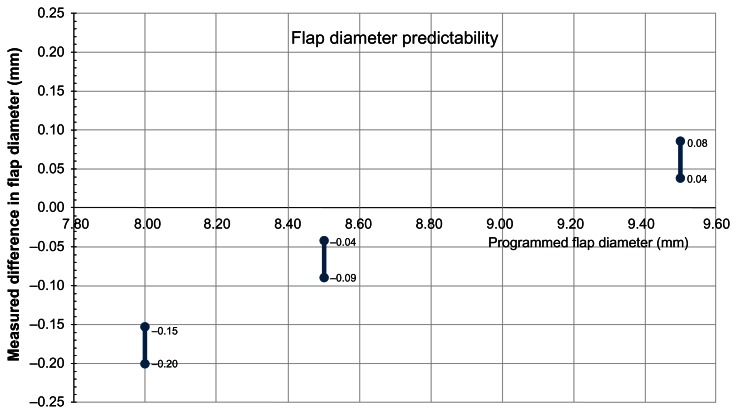
Figure 3 illustrates the flap diameter predictability for group A, specifically the measured differences in flap diameter (measured postoperatively – programmed preoperatively), based on the data reported in Table 1.
Figure 3.
Flap diameter predictability using the clear cone interface 1505.
Notes: Vertical axis, measured difference in flap diameter = achieved postoperatively – programmed preoperatively. Horizontal axis, programmed flap diameter. All units in mm.
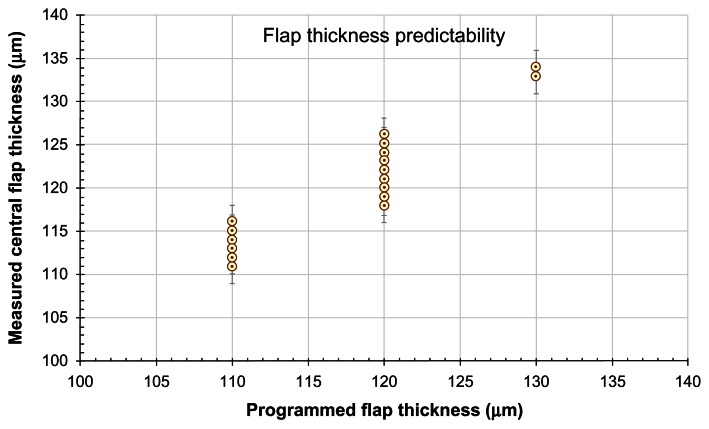
Flap thickness predictability
All flaps were subjected to high-resolution AS-OCT meridional imaging along the S-I line 1 week postoperatively, as shown in Figure 2. The measured flap thickness results for the programmed 110 μm (n = 49 eyes), 120 μm (n = 21 eyes), as well as the 130 μm flaps (n = 2), are shown in Table 2, and Figure 4 illustrates these results in the form of a scatter plot. The reading error in each measurement was estimated in the order of ±2 μm.
Table 2.
Measured (via anterior-segment optical coherence tomography imaging) versus programmed flap thickness, as obtained using the clear cone interface
| Programmed thickness 110 μm (n = 49) | |
| Average | 113.29 |
| SD | 1.19 |
| Maximum | 116 |
| Minimum | 111 |
| Programmed thickness 120 μm (n = 21) | |
| Average | 122.10 |
| SD | 2.10 |
| Maximum | 126 |
| Minimum | 118 |
| Programmed thickness 130 μm (n = 2) | |
| Average | 133.50 |
| SD | 0.71 |
| Maximum | 134 |
| Minimum | 133 |
Note: All units in μm.
Figure 4.
Flap thickness predictability using the clear cone interface 1505.
Notes: Measured central flap thickness (by anterior-segment optical coherence tomography imaging) versus programmed flap thickness. All units in μm.
Discussion
The PI applanation cone is unique in every system,9 and many of the improvements (such as closer-matched achieved vs programmed flap thickness and diameter) can be attributed to the PI.10 For example, one of the characteristics of the Alcon/WaveLight FS200 femtosecond laser11 is a balance control check to automatically calibrate each applanation cone, which adjusts for glass thickness and temperature shifts within the laser system’s components, enabling the calibration process to provide consistent and predictable flap thickness.
Both PIs in the study (1504 and 1505) have a cornea applanating cone glass surface with a diameter of 13.4 mm, corresponding to a surface area of 179.6 mm2, which is 30% larger than the corresponding area used in the FS60 IntraLase femtosecond laser, whereas the external diameter of the suction ring is 10% shorter for the FS200 laser compared with the IntraLase FS60 femtosecond laser.11 The larger applanation diameter helps centering flaps as big in diameter as 9.50 mm, which is what we clinically employ for the hyperopic treatments. Because of the shorter external diameter, it is easier to place the suction ring in eyes with smaller palpebral fissures or compact orbital anatomy.
Flap diameter accuracy and precision
Our results indicate a similar pattern with impressive accuracy, as compared with the findings in our previous study5 with the interface 1504 (metal and glass cone). Specifically, for the small flap size (diameter 8.00 mm), the mean achieved flap diameter was minimally smaller (ie, for the horizontal diameter there was a negative difference of −0.13 mm and for the vertical diameter −0.16 mm). This compares with −0.15 and −0.17 mm, respectively, for the horizontal and vertical diameters reported in our previous study,5 in which the metal and glass cone interface was studied. Precision was also similar (ranging from ±0.02 mm to ±0.04 mm).
As presented in Table 1, accuracy and precision were also very satisfactory for the 8.50 mm flap diameter.
Specifically, for group A, the difference was −0.07 mm to −0.08 mm, which compares with −0.12 mm to −0.11 mm for group B. Standard deviation was also very small, ranging from ±0.03 mm to ±0.02 mm. Again, for the larger flap diameters (9.50 mm in our study), we found a slight positive difference (ie, +0.08 mm to +0.06 mm), also in agreement with the findings in our previous study.
Overall, our study indicates an astounding flap diameter accuracy (less than −0.12 mm, up to +0.06 mm) on the LASIK flap creation with either PI on the FS200 femtosecond laser. Flap diameter precision was also outstanding in both groups, with the most precise flaps being those intended for 9.5 mm (±0.00 mm to ±0.04 mm for the horizontal and vertical meridian).
Flap thickness accuracy and precision
This study indicates that the flaps created with the novel FS200 1505 interface, as measured 1 week postoperatively via high-resolution AS-OCT imaging, are very consistent and with a very small positive difference of measured flap thickness – programmed thickness. Specifically, for the intended 110 flap, the achieved flap was just +3.29 μm thicker, also with very small standard deviation (±1.19 μm). Similarly, for the 120 μm programmed flap thickness, our data indicate slightly thicker measured flap thickness by +2.10 μm, also with very small standard deviation (±2.10 μm). This is in excellent agreement with our previously published study6 regarding topographic variability of the FS200-created flaps, in comparison with two other flap creation modalities. Specifically, in that study, the flap thickness with the FS200 femtosecond laser-created flaps (using the 1504 PI) produced flaps whose central thickness (within the 0–6 mm zone) was 120.00 μm ± 5.64 μm.
Conclusion
Our study indicates that the achieved flap diameter as compared with the programmed diameter, as well as the achieved flap thickness as compared with the programmed thickness, have similar high precision and accuracy results in both novel and standard PIs examined in this study. Both PIs show interchangeable flap parameter results, which validates the safe clinical use of the newly introduced clear cone PI in LASIK flap creation.
Footnotes
Disclosure
AJK is a consultant to Alcon/WaveLight. GA has no conflicts of interest in this work.
References
- 1.Ratkay-Traub I, Ferincz IE, Juhasz T, Kurtz RM, Krueger RR. First clinical results with the femtosecond neodynium-glass laser in refractive surgery. J Refract Surg. 2003;19(2):94–103. doi: 10.3928/1081-597X-20030301-03. [DOI] [PubMed] [Google Scholar]
- 2.Nordan LT, Slade SG, Baker RN, Suarez C, Juhasz T, Kurtz R. Femtosecond laser flap creation for laser in situ keratomileusis: six-month follow-up of initial US clinical series. J Refract Surg. 2003;19(1):8–14. doi: 10.3928/1081-597X-20030101-03. [DOI] [PubMed] [Google Scholar]
- 3.Strohmaier C, Runge C, Seyeddain O, et al. Profiles of intraocular pressure in human donor eyes during femtosecond laser procedures: a comparative study. Invest Ophthalmol Vis Sci. 2013;17;54(1):522–528. doi: 10.1167/iovs.12-11155. [DOI] [PubMed] [Google Scholar]
- 4.Vetter JM, Holzer MP, Teping C, et al. Intraocular pressure during corneal flap preparation: comparison among four femtosecond lasers in porcine eyes. J Refract Surg. 2011;27(6):427–433. doi: 10.3928/1081597X-20101210-01. [DOI] [PubMed] [Google Scholar]
- 5.Kanellopoulos AJ, Asimellis G. Digital analysis in flap parameter accuracy and opaque bubble layer objective assessment in femtosecond laser assisted LASIK. A novel technique. Clin Ophthalmol. 2013;7:343–351. doi: 10.2147/OPTH.S39644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kanellopoulos AJ, Asimellis G. Three dimensional LASIK flap thickness variability: Topographic central, paracentral and peripheral assessment, in flaps created by a mechanical microkeratome (M2) and 2 different femtosecond lasers (FS60 and FS200) Clin Ophthalmol. 2013 doi: 10.2147/OPTH.S40762. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kanellopoulos AJ, Asimellis G. Long term bladeless LASIK outcomes with the FS200 femtosecond and EX500 excimer laser workstation: the Refractive Suite. Clin Ophthalmol. 2013;7:261–269. doi: 10.2147/OPTH.S40454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kanellopoulos AJ, Asimellis G. High myopia one-year refractive and keratometric stability in LASIK with high-frequency femtosecond and excimer lasers. J Refract Surg. 2013 doi: 10.3928/1081597X-20130924-02. In press. [DOI] [PubMed] [Google Scholar]
- 9.Holzer MP, Rabsilber TM, Auffarth GU. Femtosecond laser-assisted corneal flap cuts: morphology, accuracy, and histopathology invest. Ophth Vis Sci. 2006;47(7):2828–2831. doi: 10.1167/iovs.05-1123. [DOI] [PubMed] [Google Scholar]
- 10.Khoramnia R, Salgado JP, Lohmann CP, Kobuch KA, Winkler von Mohrenfels C. Precision, morphology, and histology of corneal flap cuts using a 200-kHz femtosecond laser. Eur J Ophthalmol. 2011;22(2):161–167. doi: 10.5301/EJO.2011.8376. [DOI] [PubMed] [Google Scholar]
- 11.Mrochen M, Wüllner C, Krause J, Klafke M, Donitzky C, Seiler T. Technical aspects of the WaveLight FS200 femtosecond laser. J Refract Surg. 2010;26(10):S833–S840. doi: 10.3928/1081597X-20100921-12. [DOI] [PubMed] [Google Scholar]