Abstract
We compared service outcomes of dedicated language and cultural competency services in adequacy of care, ER, and inpatient care among Portuguese-speaking patients in ethnic- and non-ethnic-specific behavioral health clinics. We assessed adequacy of mental health care, and use of inpatient emergency department among Portuguese-speaking patients, comparing individuals receiving care from a culturally and linguistically competent mental health care setting (the Portuguese Mental Health Program [PMHP]) with usual mental health care in a community health care system in the USA. Propensity score matching was used to balance patients in treatment and control groups on gender, marital status, age, diagnosis of mental disorder, and insurance status. We used de-identified, longitudinal, administrative data of 854 Portuguese-speaking patients receiving care from the PMHP and 541 Portuguese-speaking patients receiving usual care from 2005–2008. Adequate treatment was defined as receipt of at least eight outpatient psychotherapy visits, or at least four outpatient visits of which one was a psychopharmacological visit. PMHP patients were more likely to receive adequate care. No differences were found in rates of ER use or inpatient mental health care. The present study suggests increased quality of care for patients that have contact with a clinic that dedicates resources specifically to a minority/immigrant group. Advantages of this setting include greater linguistic and cultural concordance among providers and patients. Further research is warranted to better understand the mechanisms by which culturally appropriate mental health care settings benefit minority/immigrant patients.
Keywords: adequate care, community mental health, mental health care, Portuguese-speaking patients, propensity scores, retention
In the USA, ethnic minority populations have lower levels of attendance and retention in mental health care in comparison with non-Latino Whites (Alegría et al., 2008). Many ethnic minority patients who suffer from mental health disorders prematurely drop out of treatment or discontinue care (Alegría, 2002, 2008; Hodgkin et al., 2007). These disparities in mental health care treatment are likely to result in higher than needed expenditures for these groups (Breen & Thornhill, 1998) and greater persistence and severity of mental illness for ethnic minorities (Breslau et al., 2005; Breslau et al., 2006).
Because of their specific focus on cultural competence, ethnic-specific mental health centers have great potential to improve the above mentioned shortfalls in ethnic minorities’ mental health care. According to Anderson et al. (2003), components of a culturally competent healthcare setting include: a culturally diverse staff that reflects the community served; providers or interpreters who speak the clients’ language(s); training for providers about the culture and language of the people they serve; and signage and instructional literature in the clients’ language(s) consistent with their cultural norms. Ethnic-specific mental health centers are likely to contain all of these components of culturally competent care.
Despite the widespread existence of ethnic-specific mental health care centers across the USA (Anderson et al. 2003), there has been a paucity of research assessing their effectiveness in treating ethnic minority populations. The few studies on this topic were conducted in the 1990s (Takeuchi et al., 1995; Yeh et al., 1994; Zane, Hatanaka, Park, & Akutsu, 1994). Ethnic-specific programs were found to increase return rates and length of treatment (Takeuchi et al., 1995), and ethnic minorities in ethnic-specific programs were more likely than ethnic minorities in mainstream programs to have been referred by natural help-giving or lay referral sources (for Asians and Hispanic Americans) and self-referred (for African Americans; Akutsu et al., 1996). These studies presented preliminary evidence of the effectiveness of ethnic-specific mental health programs, but further evaluation is needed to assess whether these programs continue to improve service, given the multiple changes since the 1990s in the policy, treatment, and financing of mental health care (Glied & Frank, 2009). According to a review by Bhui et al. (2007), evidence on the effectiveness of cultural competency training and service delivery in mental health care is still lacking. Alegría et al. (2008) discuss the potential of improved cultural competency programs to increase self-reported patient activation, retention and attendance in mental health care for minority populations through patient activation and empowerment.
The mental health of Portuguese-speaking populations in the USA
Portuguese-speaking minorities are a diverse group: their countries of origin are located in Europe, South America, Africa, and Asia. We are aware of no previous studies focused on mental health care in the Portuguese-speaking U.S. population, reflecting an overall lack of information on this population in the USA and world-wide (exceptions are Gonçalves, 2009, 2010; Han et al., 2009; James et al., 2005; Rubinstein-Avila, 2005). In the same vein, the importance of interpreters and reducing language barriers in mental health care has received substantial attention for Spanish-speaking patients (Ngo-Metzger et al., 2007), but not for Portuguese speakers.
We found only two small studies (N ≤ 50) that assessed mental health issues for Portuguese-speaking populations in the USA and Canada (James et al., 2002, 2005, 2009). The authors studied two culture-specific phenomena, agonias and problemas de nervos, demonstrating a link between somatic symptoms and psychological processes, social context, and religious beliefs, and highlighting that psychiatric categories can be limited when classifying these multidimensional experiences. The complexity that this presents for diagnosis and treatment suggests that culturally competent providers may be more readily able to understand this kind of culturally specific phenomena and therefore contribute to the improved treatment and retention of the patients.
Description of the Portuguese Mental Health Program
The Portuguese Mental Health Program (PMHP) is a culturally and linguistically competent clinic housed within an urban safety-net hospital system in the Northeast region of the USA. It consists of 69 clinics and three hospitals, serving patients from a diverse range of ethnicities and socioeconomic backgrounds. Other than English, the language most commonly spoken by patients in this community health system is Portuguese. In 2009, 14% of all outpatient visits were by Portuguese-speaking patients compared to 9% that were Spanish speaking. Portuguese is the third most frequently spoken language in the state of the study, after English and Spanish. The health care system established the PMHP in 1985 with bilingual and bicultural staff to serve children and adults from Brazil, Portugal, and Cape Verde. The services cover the fields of psychiatry, psychology, social work, and family therapy. Services range from outpatient therapy to psychiatric emergency and acute hospital care. The community health system serves a higher proportion of uninsured and Free Care patients than most other regional health systems in the area and the nation. The main difference between PMHP and the other non-ethnic-specific settings of the community health system (usual care) is that 95% of the providers in the PMHP speak Portuguese, compared with only 5% of the providers in usual care. Most of the care in non-PMHP settings is provided with the assistance of an interpreter.
Hypotheses
The present study aimed to improve upon prior studies by measuring the association of dedicated language and cultural competency services on adequacy of care, ER use and inpatient care, and by focusing on Portuguese-speaking patients, a population that, to our knowledge, has never been considered in the ethnic-specific literature, despite representing a significant percentage of immigrants in a number of major cities in the USA. Based on prior studies identifying greater effectiveness in mental health treatment for patients receiving care in ethnic-specific clinics, we hypothesized that Portuguese-speaking patients receiving care in the PMHP would be more likely to receive adequate care, and less likely to receive acute care (inpatient and emergency room visits) than Portuguese-speaking patients receiving care in non-ethnic-specific clinics.
Methods
Sample
We used de-identified longitudinal administrative data of all Portuguese-speaking patients receiving services in an urban health care system between 2005 and 2008. Patients in the sample were enrolled in a public health insurance system (Commonwealth Care [the state-subsidized insurance program in Massachusetts], Free Care, Medicaid, or Medicaid-affiliated HMOs) at some point during the time period 2005–2008. The study sample subjects were comprised of three main groups of Portuguese speakers: Brazilians (majority White, but a small fraction of Blacks); Portuguese from Portugal or the Azorean Islands (primarily White); and immigrants from Cape Verde Islands off the coast of Africa (all Black).
Our sample included 828 Portuguese-speaking patients receiving care from the PMHP (ethnic-specific clinic) and 500 Portuguese-speaking patients receiving usual care from other non-ethnic-specific clinics within the same health services system from 2005–2008. The Institutional Review Board of the Cambridge Health Alliance approved the study protocol. The treatment group was defined as any patient with Portuguese as primary language of care and with any mental health visit to the PMHP. In sensitivity analyses, we restricted our criteria for inclusion in the treatment group further by requiring individuals in the treatment group to have four or more mental health visits at the PMHP and individuals in the control group to have four or more mental health visits at the non-PMHP clinics.
Measures
We used three dependent variables. The first was receiving adequate treatment, defined as receipt of at least eight outpatient psychotherapy visits, or at least four outpatient visits of which one was a psychopharmacological visit. This definition reflects evidence-based treatment guidelines for depressive disorder (Wang et al., 2002), which recommend receipt of appropriate medication plus four mental health visits, or at least eight visits of relevant psychotherapy with a mental health practitioner (Lehman et al., 1998). This definition has also been used to operationalize adequate mental health care in previous studies (Alegría et al., 2008; Carson et al., 2010; Harman et al., 2004; Kessler et al., 2003; Wang et al., 2002). Outpatient mental health visits were identified as psychotherapy or psychopharmacology using current procedural terminology (CPT) codes assigned by clinicians for each visit (Beebe et al., 2008).
The second dependent variable analyzed was any emergency room (ER) use among those with a visit for a psychiatric diagnosis, considering ER use to be a preventable and thus negative outcome. The third dependent variable was receipt of any inpatient care for a psychiatric diagnosis; this outcome was considered negative because inpatient care is nearly always preventable with proper outpatient and psychopharmacological treatment (Padgett et al., 1994).
Independent variables used in the multivariate regression to allow for propensity score matching (described below) were: insurance status (Medicaid, Medicare, Commonwealth Care, another state-run non-Medicaid public health insurance plan, private insurance); age (18–24, 25–34, 35–44, 45–54, 55–64, 65+); marital status (married, single, separated/divorced, widowed/unknown); race/ethnicity (White, Black, Hispanic, other); sex; and diagnosis of mental disorder (depression, anxiety, substance abuse, schizophrenia).
Data analysis
First, we presented descriptive characteristics of the administrative data, including age, gender, marital status, and type of psychiatric disorder. Differences in rates of categorical variables between treatment and control group patients were tested using chi-square tests.
To adjust for differences in insurance status, sociodemographics, and mental disorder between the two groups of Portuguese-speaking patients, we assessed differences between treatment and control groups before and after balancing on observed covariates at initial intake using propensity score matching. The propensity score is the probability of assignment to treatment, conditional on a vector of observed covariates, P(D=1|X=x), where D is treatment status (receiving care at the PMHP) and X is a vector of observed covariates measured at initial intake. Conditional on the propensity score, the distributions of observed covariates are the same for the treatment and the control group, approximating the randomization of individuals to these groups (Rosenbaum & Rubin, 1983; Rubin, 1997). The estimated propensity score êi(H) is the predicted probability of being in the treatment group under a logit model for this probability.
Nearest neighbor-matching with replacement was used as the matching algorithm (Rosenbaum & Rubin, 1983). Each individual in the treatment group was matched to a control group individual with the nearest propensity score. The control group individual was then placed back into the pool for possible matching with the next treatment individual. Diagnostic tests of balance between treatment and control groups after propensity score matching were implemented following Ho et al. (2009), and included identifying pre- and postmatching differences in covariate means, quantile–quantile plots of covariate distributions to identify that empirical distributions of each covariate were similar in both treatment and control groups, and pre- and postmatching jitter plots and histograms as visual representations of the balance achieved by the propensity score method.
Once the balance of the two groups was properly satisfied, the difference in adequate care between the treatment and control groups was ascertained by subtracting the mean probability of the outcome of interest within the treatment group from the mean probability of the outcome of interest within the matched control group. The difference in adequate care between the treatment and control groups in this case represents a difference between the two groups after adjustment for observed covariates and is not meant to signify a causal effect. Standard errors were estimated assuming independent observations and homoskedasticity on the dependent variables within both the PMHP and usual care groups, and that the variance of the dependent variables did not depend on the propensity score. Propensity score analyses were conducted using the psmatch2 module (Leuven & Sianesi, 2003) in Stata 10. Propensity score diagnostics were implemented using the R software package MatchIt module (Ho et al., 2007).
Results
The results are based on 828 patients in the treatment group and 500 patients in the control group. Table 1 identifies several significant differences in rates of independent variables between the treatment and control groups. We found PMHP patients to be more likely to be enrolled in Medicare, age 55–64, married, to report White race, and to have a diagnosis of schizophrenia, and less likely to be in the 25–34 age group and single.
Table 1.
Sociodemographic characteristics of Portuguese-speaking patients in Portuguese Mental Health Program (PMHP) and usual care
| non-PMHP | PMHP | Total | |
|---|---|---|---|
| n = 500 | n = 828 | n = 1328 | |
| Insurance | |||
| Medicaid | 41.9 | 43.1 | 42.4 |
| Medicare | 0.5 | 2.4** | 1.2 |
| Commonwealth | 9.3 | 11.5 | 10.1 |
| Private | 16.2 | 13.5 | 15.1 |
| Network Neighborhood | 6.9 | 5.6 | 6.4 |
| Age | |||
| 18–24 | 6.1 | 4.8 | 5.6 |
| 25–34 | 10.7 | 5.0** | 8.5 |
| 35–44 | 28.3 | 28.3 | 28.3 |
| 45–54 | 29.3 | 26.8 | 28.3 |
| 55–64 | 23.2 | 30.9** | 26.2 |
| 65+ | 2.5 | 4.3 | 3.2 |
| Marital status | |||
| Married | 36.5 | 46.8*** | 40.5 |
| Single | 51.2 | 43.4** | 48.2 |
| Separated/divorced | 8.6 | 7.4 | 8.1 |
| Race/ethnicity | |||
| White | 53.3 | 58.8* | 55.4 |
| Black | 1.8 | 2.6 | 2.1 |
| Hispanic | 2.8 | 1.7 | 2.4 |
| Other | 41.9 | 37.0 | 40.0 |
| Sex | |||
| Female | 73.3 | 73.4 | 73.3 |
| Male | 26.7 | 26.6 | 26.7 |
| Mental health | |||
| Depression | 68.9 | 71.4 | 69.8 |
| Anxiety | 65.1 | 61.7 | 63.8 |
| Substance abuse | 7.5 | 7.0 | 7.3 |
| Schizophrenia | 4.8 | 7.4* | 5.8 |
Note. PMHP = Portuguese Mental Health Program; non-PMHP group = usual care: Other clinics within same community health care system.
significant at the p <.10 level;
significant at the p <.05 level.
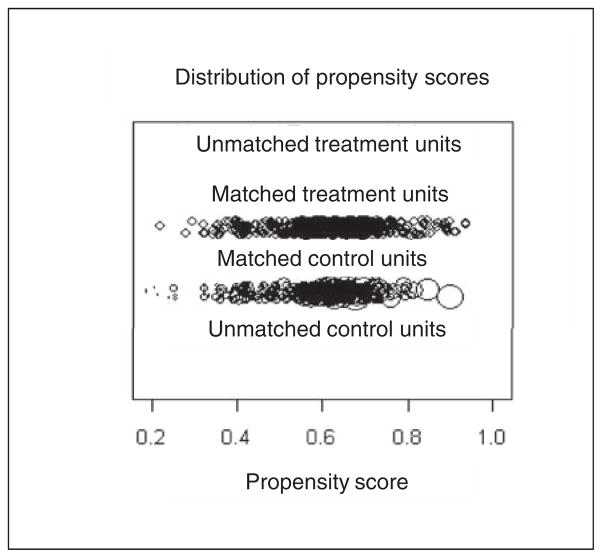
According to diagnostics comparing differences in means of covariates and visual plots, the propensity score method was able to balance the PMHP and usual care groups with no significant differences on any covariates after propensity score balancing (Table 2), good overlap and distribution of matched units (Figure 1), and propensity scores after matching (Figure 2).
Table 2.
Matching results for 828 Portuguese-speaking patients with mental health care use seen in New England Health Care System between 2005 and 2008
| Variable name | Mean for PMHP patients | Mean for control group | Mean control after matching | Mean difference between matched pairs1 |
|---|---|---|---|---|
| Propensity score* | 0.6390 | 0.5978 | 0.6391 | 30.0001 |
| Insurance | ||||
| Medicaid | 43.6% | 46.0% | 39.5% | 4.1% |
| Medicare | 1.8% | 0.4% | 2.4% | 30.6% |
| Commonwealth | 11.8% | 8.6% | 12.0% | 30.2% |
| Network Neighborhood | 6.3% | 7.4% | 5.6% | 0.7% |
| Age | ||||
| 25–34 | 5.7% | 11.8% | 4.9% | 0.8% |
| 35–44 | 27.4% | 28.4% | 30.0% | 32.6% |
| 45–54 | 28.3% | 28.6% | 25.9% | 2.3% |
| 55–64 | 29.6% | 21.8% | 31.9% | 32.3% |
| 65+ | 3.4% | 3.2% | 2.8% | 0.6% |
| Marital status | ||||
| Single | 46.0% | 51.2% | 43.1% | 2.9% |
| Separate/divorced | 8.2% | 8.0% | 10.1% | 31.9% |
| Race/ethnicity | ||||
| Black | 1.9% | 2.4% | 3.5% | 31.6% |
| Hispanic | 1.6% | 4.0% | 1.7% | 30.1% |
| Sex | ||||
| Female | 74.2% | 74.4% | 73.3% | 0.9% |
| Mental Health | ||||
| Anxiety | 64.7% | 64.2% | 62.9% | 1.9% |
| Substance abuse | 6.9% | 7.2% | 5.8% | 1.1% |
| Schizophrenia | 8.1% | 2.6% | 7.4% | 0.7% |
Note.
The propensity score is a scalar summary of the predicted probability of being in the treatment group based on the probit equation estimating the probability of being in treatment regressed on the above described covariates.
There were no significant differences between PMHP patients and matched control patients on any of the above covariates.
Figure 1.
Distribution of propensity scores across matched treatment and control units. No units were unmatched.
Figure 2.
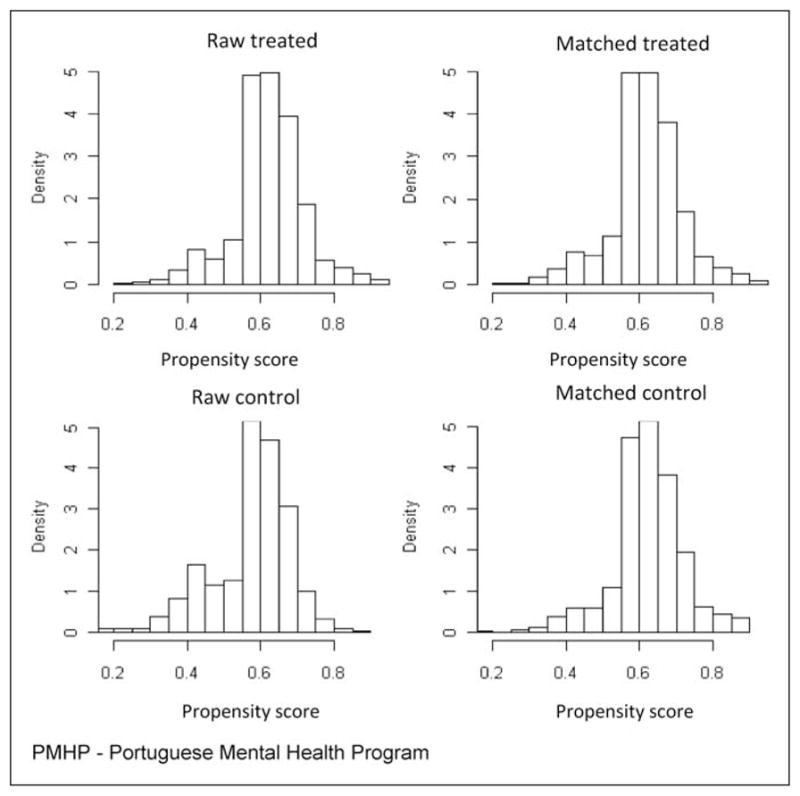
Histogram showing distributions of propensity score before and after matching for treated (>=1 PMHP visits) and control groups (other community health care system clinics).
Using eight mental health visits as a criterion of adequate care in unadjusted analyses, 58.5% of Portuguese-speaking patients with any contact with the PMHP received adequate care compared to 26.3% of those in usual care (see Table 3). After balancing using the propensity score methodology described above, we found similar results with 58.5% of PMHP patients and 30.4% of usual care patients receiving adequate care, for a difference in adequate care between the treatment and control groups of 28.1%. We also found significant differences in adequate care using the criteria of four visits with psychopharmacology, finding a 29% difference in adequate care between the treatment and control groups in the propensity score-matched analysis. For ER use and inpatient care, there were no significant differences identified between the two groups in either unadjusted or propensity score analyses.
Table 3.
Average treatment effect estimated using propensity score matching
| non-PMHP | PMHP | Difference | SE | t statistic | ||
|---|---|---|---|---|---|---|
| PMHP treatment group: >= 1 visit to PMHP | ||||||
| Adequate care (>= 8 visits) | Unmatched | 58.5% | 26.3% | 32.1% | 2.6% | 12.43 |
| PS matched | 58.5% | 30.4% | 28.1% | 4.6% | 6.07 | |
| Adequate care (>= 4 visits with Rx) | Unmatched | 67.5% | 32.4% | 35.1% | 2.6% | 13.68 |
| PS matched | 67.5% | 38.8% | 28.7% | 4.9% | 5.82 | |
| ER use | Unmatched | 72.0% | 73.2% | −1.1% | 2.4% | −0.46 |
| PS matched | 72.0% | 75.8% | −3.8% | 4.6% | −0.84 | |
| Inpatient care | Unmatched | 2.4% | 3.0% | −0.6% | 0.9% | −0.6 |
| PS matched | 2.4% | 1.4% | 1.0% | 2.3% | 0.4 | |
| PMHP treatment group: >= 4 visits to PMHP; control group: >= 4 visits outside of PMHP | ||||||
| Adequate care (>= 8 visits) | Unmatched | 81.4% | 48.0% | 33.4% | 3.0% | 11.31 |
| PS matched | 81.4% | 54.7% | 26.7% | 6.0% | 4.47 | |
| Adequate care (>= 4 visits with Rx) | Unmatched | 90.5% | 64.5% | 26.0% | 2.5% | 10.23 |
| PS matched | 90.5% | 72.2% | 18.3% | 5.2% | 3.53 | |
| ER use | Unmatched | 73.6% | 75.0% | −1.4% | 3.0% | −0.46 |
| PS matched | 73.6% | 80.3% | −6.7% | 5.1% | −1.33 | |
| Inpatient care | Unmatched | 2.2% | 3.0% | −0.8% | 0.9% | −0.9 |
| PS matched | 2.2% | 3.2% | −1.0% | 2.3% | −0.4 | |
Note. PMHP = Portuguese Mental Health Program; PS = propensity score.
As a sensitivity analysis, we reconducted these analyses, switching the criteria for membership in the treatment group to require four or more visits to the PMHP. Because these patients were required to have four visits to be in the treatment group, we compared them to those patients that had four or more mental health care visits in non-PHMP settings. Differences in adequate care in this sensitivity analyses were smaller in magnitude than the previous analysis, but similar in terms of direction (higher rates of adequate care in the PMHP group). As in the previous analysis, all differences between patients in the PMHP and non-PMHP settings were significant for the variables indicating adequate care and insignificant in the variables reporting any ER or inpatient use.
Discussion
Higher rates of adequate care in the PHMP group compared to usual care suggest that a culturally and linguistically competent setting may be better able to provide quality of care to patients in need of mental health care. A number of mechanisms potentially explain the findings of improved adequacy of care in the ethnic-specific clinic. First, the major difference between this clinic and usual care is its large group of culturally competent therapists and an emphasis on close follow-up contact using Portuguese-language providers and ancillary staff. Although capacity is not great enough to provide all PMHP patients with a Portuguese-speaking psychiatrist, there is enough capacity to match every patient with a culturally competent clinical therapist (i.e., social worker, psychologist) that is fluent in their language. Recent qualitative work on cultural differences in preferences for relational style suggests that subtle communication cues may encourage retention in care but preferences for these relational styles may vary across race and ethnicity (Mulvaney-Day et al., 2010). It is possible that implicit communication patterns understood by culturally and linguistically competent providers may facilitate care provided by ethnic-specific clinics. A second mechanism mentioned in discussion with PMHP staff is that the success of the PMHP is not only because of customized or individualized care in one’s native language, but also because the PMHP has become a trusted and stable institution within a community that is in transition and struggling to find its bearings in a new culture and society.
We found no differences between patients in PMHP and non-PMHP settings in ER use or inpatient use even after matching on mental health diagnoses, age, and other covariates. This suggests that culturally appropriate care may not have an added advantage over usual care in preventing these health care outcomes in this population. It is possible that among those with acute or severe mental illness who require inpatient care, a culturally targeted response is not as strong an influence on patterns of care. Illness severity may drive decision-making about inpatient care and ER use, whereas cultural competence may primarily facilitate engagement, hence encouraging retention in outpatient care.
Policy makers, researchers, and health professionals are now more aware of the challenges in providing mental health care to a culturally and racially diverse population (Anderson et al., 2003; Griner & Smith, 2006) and resources are being allocated to improve cultural competency in health care settings nationwide. Different kinds of culturally competent care have been studied, including: (a) workforce training (Bhui et al., 2007); (b) service delivery/treatment adaptations (Grinner & Smith, 2006; Whaley & Davis, 2007); and (c) the addition of written informational materials (Han et al., 2009). Grinner and Smith (2006) found a moderately strong benefit of culturally adapted mental health interventions on mental health outcomes and retention in care, particularly when the interventions were targeted to a specific racial/ethnic group and conducted in the client’s preferred language. This study provides preliminary evidence that creation and continued funding of ethnic-specific mental health centers can lead to improved treatment for ethnic minorities. It also suggests that heightened interest in moving towards a medical home model as a source of improved efficiency and quality of care (e.g., the demonstration projects legislated in the Patient Protection and Affordable Care Act [PPACA]) should take into account the cultural and linguistic competency of the medical home. Just as the PMHP appears to have improved retention because of its wealth of culturally and linguistically competent providers, there may be additional benefits to medical homes for ethnic minorities when issues of language and culture are taken into account.
We were limited by the observational nature of the data and our sample, which was drawn from a major teaching health services network in New England and may not be generalizable to other areas of the USA. We have used propensity score matching in an attempt to identify associations between treatment in an ethnic-specific clinic and adequate care, recognizing that randomization of Portuguese-speaking patients into PMHP and usual care groups would be a superior method of identifying causal relationships. A further limitation is that our propensity score analyses balance the two groups on indicators of psychiatric diagnosis but not on measures of mental health severity or symptoms since they were unavailable from the administrative data. We were also unable to balance on provider variables such as psychotherapy training and experience. If the PMHP had providers with greater training and experience, then that may provide an alternative explanation to the greater rates of adequacy of care identified in the ethnic-specific clinic. Future study is needed that more accurately adjusts for baseline mental health status and experience of providers. A further limitation was that we were unable to test the association of ethnic-specific clinics on mental health outcomes given a lack of mental health status measures.
Other patient characteristics not present in the administrative data may confound the association between visits to an ethnic-specific clinic and adequate care. The inclusion of two such variables—language proficiency and immigration status—could strengthen our findings, given that limited English-proficient and immigrant groups have been identified to have poorer access to health care (Fiscella, 2002; Ku, 2001) and local practitioners report anecdotally that these groups are more likely to use the PMHP. However, we are unsure of the direction of influence of other unobserved characteristics (e.g., comorbid physical health conditions) and this represents a limitation of our study.
The present study reinforces the conclusions of studies in the 1990s that found that ethnic-specific mental health clinics improve service outcomes (Takeuchi et al., 1995). Clinically, we have identified that culturally competent intensive mental health care services can improve retention and quality of care. Further replication of this study’s findings in the other ethnic-specific clinics in community health systems would support policy recommendations to devote resources to expand availability of such clinics. A strength of this study is the use of administrative data to analyze differences between ethnic-specific and general outpatient mental health clinics. However, more intensive, qualitative investigation is needed to explicate further the factors that are contributing to these differences and provide concrete information to inform clinical policies. Data collection might include patients’ self-assessment of the clinic characteristics, satisfaction with care, perception of the “therapeutic” factors embedded in the environment, and perspectives of staff members working in the clinics. Qualitative interviews with patients and staff in the PMHP setting are necessary to collect this information and provide context to interpret these findings.
Acknowledgments
Funding
This study was supported by the Portuguese Foundation for Science and Technology through the Postdoctoral Fellowship SFRH/BPD/48528/2008 granted to the first author (MG) at Harvard University. Additional support was provided by NIMH grant R01 MH091042 (PI Benjamin Cook).
Biographies
Marta Gonçalves, PhD, is currently a researcher at the Centre for Social Research and Intervention at the Lisbon University Institute ISCTE-IUL and at the Center for Multicultural Mental Health Research at Harvard Medical School and a visiting professor at the Department of Social and Organizational Psychology at ISCTE-IUL and at the Doctoral Program in Mental Health and Clinical Neurosciences at the University of Porto. Dr. Gonçalves completed her PhD at the University of Zurich within the 52nd Swiss National Program – Childhood, Youth and Intergenerational Relationships in a Changing Society. Dr. Goncalves was also an Invited Researcher at the University of Freiburg in Germany and a psychologist for expatriate and diplomatic families in Brussels (Belgium) and Warsaw (Poland). Her basic training was at the German School of Porto and at the Faculty of Psychology of the University of Porto.
Benjamin Cook, PhD, MPH, is a senior scientist at the CMMHR and an Assistant Professor at Harvard Medical School. His research interests are in improving methods for measuring disparities, and applying these methods to understanding the mechanisms underlying mental health and substance abuse treatment disparities, the association between acculturation and mental health, and geographic differences in mental health service use disparities. He received a PhD in Health Policy at Harvard University concentrating in Evaluative Science and Statistics, an MPH from UNC-Chapel Hill in the Department of Health Behavior and Health Education, and a BA in Psychology from Swarthmore College.
Norah Mulvaney-Day, PhD, is an associate/scientist in the Behavioral Health Section at Abt Associates with expertise in disparities research among those with behavioral health disorders. She is currently the Task Leader on a project for the Substance Abuse and Mental Health Services Administration investigating smoking prevention and cessation models for individuals with mental health disorder, particularly those from vulnerable populations. She is also a collaborating scientist on the National Vietnam Veterans Longitudinal Study. Dr. Mulvaney-Day received her PhD from Brandeis University, where she was an NIMH trainee in mental health services research. Dr. Mulvaney-Day has been an advisor and consultant for numerous disparities research groups, including the Advisory Board of the Public Mental Health Research group at Boston City Hospital, and the Healthcare Disparities Reduction and Elimination Committee for the Massachusetts Department of Mental Health. Prior to working at Abt, Dr. Mulvaney-Day was a Senior Scientist at the Center for Multicultural Mental Health Research at the Cambridge Health Alliance, and an Instructor in Psychiatry at Harvard Medical School.
Margarita Alegría, PhD is the Director of the Center for Multicultural Mental Health Research and a professor of psychology in the Department of Psychiatry at Harvard Medical School. Dr. Alegría researches mental health services for Latinos and other ethnic populations. She is currently the Principal Investigator of the Advanced Center for Mental Health Disparities, and the Latino Arm of the National Latino and Asian American Study, as well as the Co-Principal Investigator of the CHA-UPR Excellence in Partnerships for Community Outreach, Research on Health Disparities and Training (EXPORT) Center. Her published works focus on mental health services research, conceptual and methodological issues with minority populations, risk behaviors, and disparities in service delivery. Dr. Alegría received her PhD from Temple University.
Gustavo Kinrys, MD, is a graduate from the Mayo Clinic Graduate School and the Massachusetts General Hospital. Dr. Kinrys was the Director of the Mood and Anxiety Disorders Research Program and the Psychopharmacology Research Program, and the Medical Director of the Portuguese Mental Health Clinic at the Cambridge Health Alliance, Harvard Medical School for 9 years. Following that, he returned to MGH to become the Associate Medical Director of MGH Clinical Trials Network and Institute (CTNI), Bipolar Clinic and Research Program (BCRP), Massachusetts General Hospital, Harvard Medical School.
Footnotes
Reprints and permissions: sagepub.co.uk/journalsPermissions.nav
Contributor Information
Marta Gonçalves, Instituto Universitário de Lisboa (ISCTE-IUL) and Harvard Medical School.
Benjamin Cook, Harvard Medical School.
Norah Mulvaney-Day, Abt Associates.
Margarita Alegría, Harvard Medical School.
Gustavo Kinrys, Harvard Medical School.
References
- Akutsu P, Snowden L, Organista K. Referral patterns in ethnic-specific and mainstream programs for ethnic minorities and Whites. Journal of Counseling Psychology. 1996;43:56–64. [Google Scholar]
- Alegría M, Canino G, Rios R, Vera M, Calderon J, Rusch D, Ortega AN. Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino Whites. Psychiatric Services. 2002;53:1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- Alegría M, Polo A, Gao S, Santana L, Rothstein D, Jimenez A, Normand S-L. Evaluation of a patient activation and empowerment intervention in mental health care. Medical Care. 2008;46(3):247–256. doi: 10.1097/MLR.0b013e318158af52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J Task Force on Community Preventive Services. Culturally competent healthcare systems. A systematic review. American Journal of Preventive Medicine. 2003;24(3S):68–79. doi: 10.1016/s0749-3797(02)00657-8. [DOI] [PubMed] [Google Scholar]
- Beebe M, Dalton JA, Espronceda M Professional, editor. Current procedural terminology. Chicago, IL: American Medical Association; 2008. [Google Scholar]
- Bhui K, Warfa N, Edonya P, McKenzie K, Bhugra D. Cultural competence in mental health care: A review of model evaluations. BMC Health Services Research. 2007;7(15) doi: 10.1186/1472-6963-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breen R, Thornhill JT. Noncompliance with medication for psychiatric disorders: Reasons and remedies. CNS Drugs. 1998;9(6):457–471. [Google Scholar]
- Breslau J, Aguilar-Gaxiola S, Kendler KS, Su M, Williams D, Kessler RC. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychological Medicine. 2006;36(1):57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Kendler K, Su M, Gaxiola-Aguilar S, Kessler R. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychological Medicine. 2005;35(3):317–327. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson N, Cook B, Alegría M. Social determinants of mental health treatment among Haitian, African American, and White youth in community health centres. Journal of Health Care for the Poor and Underserved. 2010;21(2):32–48. doi: 10.1353/hpu.0.0297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured: Findings from a national sample. Medical Care. 2002;40(1):52–59. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- Glied SA, Frank RG. Better but not best: Recent trends in the well-being of the mentally ill. Health Affairs. 2009;28(3):637–648. doi: 10.1377/hlthaff.28.3.637. [DOI] [PubMed] [Google Scholar]
- Gonçalves M. The access of migrant children to mental health care: A study with Portuguese-speaking families in the multicultural context of Switzerland. Hamburg, Germany: Verlag Dr. Kovac; 2009. Der Zugang von Migrantenkindern zur psychischen Gesundheitsversorgung. Eine Untersuchung mit portugiesisch-sprachigen Familien im multi-kulturellen Umfeld der Schweiz. [Google Scholar]
- Gonçalves M, De Oliveira Käppler C. The access to mental health care in children: Portuguese-speaking families living in a multicultural context in Europe. Interamerican Journal of Psychology. 2010;44(3):411–420. [Google Scholar]
- Griner D, Smith TB. Culturally adapted mental health interventions: A meta-analytic review. Psychotherapy: Theory, Research, Practice, Training. 2006;43(4):531–548. doi: 10.1037/0033-3204.43.4.531. [DOI] [PubMed] [Google Scholar]
- Han A, Laranjo H, Friedman SM. The design and pilot of a translation aid to help ED clinicians enhance communication with the Portuguese-speaking patient. International Journal of Emergency Medicine. 2009;2:41–46. doi: 10.1007/s12245-008-0081-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harman JS, Edlund MJ, Fortney JC. Disparities in the adequacy of depression treatment in the United States. Psychiatric Services. 2004;55(12):1379–1385. doi: 10.1176/appi.ps.55.12.1379. [DOI] [PubMed] [Google Scholar]
- Ho D, Imai K, King G, Stuart E. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Political Analysis. 2007;15:199–236. [Google Scholar]
- Ho DE, Imai K, King G, Stuart EA. MatchIt: Nonparametric preprocessing for parametric causal inference. Journal of Statistical Software. 2011;42(8):1–29. [Google Scholar]
- Hodgkin D, Volpe-Vartanian J, Alegría M. Discontinuation of antidepressant medication among Latinos in the U.S. Journal of Behavioral Health Services and Research. 2007;34(3):329–342. doi: 10.1007/s11414-007-9070-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James S, Navara GS, Clarke JN, Lomotey J. An inquiry into the agonies of Portuguese immigrants from the Azores. Hispanic Journal of Behavioral Sciences. 2005;27(4):547–564. [Google Scholar]
- James S, Fernandes M, Navara GS, Harris S, Foster D. Problemas de nervos: A multivocal symbol of distress for Portuguese immigrants. Transcultural Psychiatry. 2009;46(2):285–299. doi: 10.1177/1363461509105819. [DOI] [PubMed] [Google Scholar]
- James S, Prilleltensky I. Cultural diversity and mental health: Towards integrative practice. Clinical Psychology Review. 2002;22:1133–1154. doi: 10.1016/s0272-7358(02)00102-2. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Wang PS. National Comorbidity Survey Replication: The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCSR) Journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Ku L, Matani S. Left out: Immigrants’ access to health care and insurance. Health Affairs. 2001;20(1):247–256. doi: 10.1377/hlthaff.20.1.247. [DOI] [PubMed] [Google Scholar]
- Lehman AF, Steinwachs DM. Patterns of usual care for schizophrenia: Initial results from the Schizophrenia Patient Outcomes Research Team (PORT) client survey. Schizophrenia Bulletin. 1998;24:11–20. doi: 10.1093/oxfordjournals.schbul.a033303. [DOI] [PubMed] [Google Scholar]
- Leuven E, Sianesi B. PSMATCH2: Stata module to perform full Mahalanobis and propensity score matching, common support graphing, and covariate imbalance testing, [Computer software] Boston, MA: Boston College Department of Economics; 2003. [Google Scholar]
- Mulvaney-Day N, Earl T, Diaz-Linhart Y, Alegría M. Preferences for relational style with mental health clinicians: A qualitative comparison of African American, Latino and Non-Latino. Journal of Clinical Psychology. 2011;67(1):31–44. doi: 10.1002/jclp.20739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngo-Metzger Q, Sorkin DH, Phillips RS, Greenfield S, Massagli MP, Clarridge B, Kaplan SH. Providing high-quality care for limited English proficient patients: The importance of language concordance and interpreter use. Journal of General Internal Medicine. 2007;22(Suppl 2):324–330. doi: 10.1007/s11606-007-0340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padgett DK, Patrick C, Burns B, Schlesinger H. Ethnic differences in use of inpatient mental health services by Blacks, Whites, and Hispanics in a national insured population. Health Services Research. 1994;29(2):135–153. [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- Rubin DB. Estimating causal effects from large data sets using propensity scores. Annals of Internal Medicine. 1997;127(8, Pt. 2):757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- Rubinstein-Avila E. Brazilian Portuguese in Massachusetts’s linguistic landscape: A prevalent yet understudied phenomenon. Hispania. 2005;4(88):873–880. [Google Scholar]
- Takeuchi D, Sue S, Yeh M. Return rates and outcomes from ethnicity-specific mental health programs in Los Angeles. American Journal of Public Health. 1995;85:638–643. doi: 10.2105/ajph.85.5.638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang PS, Demler O, Kessler RC. Adequacy of treatment for serious mental illness in the United States. American Journal of Public Health. 2002;92:92–98. doi: 10.2105/ajph.92.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whaley AL, Davis KE. Cultural competence and evidence-based practice in mental health services. American Psychologist. 2007;62(6):563–574. doi: 10.1037/0003-066X.62.6.563. [DOI] [PubMed] [Google Scholar]
- Yeh M, Eastman K, Cheung MK. Children and adolescents in community health centers: Does the ethnicity or language of the therapist matter? Journal of Community Psychology. 1994;22:153–163. [Google Scholar]
- Zane N, Hatanaka H, Park S, Akutsu P. Ethnic-specific mental health services: Evaluation of the parallel approach for Asian-American clients. Journal of Community Psychology. 1994;22:68–81. [Google Scholar]