Abstract
Purpose
Persistent displacement of ankle fractures increases the stresses on the articular cartilage and leads to degenerative arthritis. Correction of the ankle mortise restores the normal ankle biomechanics and should prevent the development of degenerative joint disease.
Methods
Seventeen patients were treated for symptomatic ankle joint due to malunited distal fibular fracture. There were eleven male and six female patients. Their ages ranged from 23 to 54 years (median 34 years). The procedure included transverse fibular osteotomy for restoration of the lateral malleolar alignment, acute distraction of the osteotomy to restore the fibular length with interpositional graft and reduction of subluxation of the distal tibio-fibular articulation. Internal fixation of the osteotomy was performed with plate and screws and trans-syndesmotic screws.
Results
Fibular lengthening was performed in all cases and ranged from six to 12 mm (median eight millimetres). The American Orthopaedic Foot and Ankle Society score preoperatively ranged from 40 to 74 (median 60) and at follow up ranged from 50 to 95 (median 79). Progression of ankles arthrosis occurred in one patient leading to ankle arthrodesis as a secondary procedure. Results were satisfactory in 12 cases (70.6 %), and unsatisfactory in five cases (29.4 %) due to stiffness and pain in the ankle joint. The follow-up ranged from 24 to 45 months (median 31 months).
Conclusion
Corrective osteotomy of fibular malunion produces considerable improvement provided that the patient does not have significant degenerative changes before surgery. The use of athrodiastasis of the ankle as a secondary procedure may be of value to improve the outcome.
Introduction
The primary goal of treatment for displaced ankle fractures is to restore anatomical alignment, joint congruence and full function. The most frequent malunion of the fibula is shortening and malrotation resulting in widening of the ankle mortise and talar instability [1].
Patients with persistent displacement of ankle fractures may develop degenerative arthritis due to reduction in the tibio-talar contact area, increasing the stresses on the articular cartilage. Several biomechanical studies have revealed the importance of fibular shortening and rotation on stability of the ankle joint. A malunited fracture of the distal fibula results in sublaxation of the anterior aspect of the tibiofibular joint, due to shortening and external rotation deformity of the lateral malleolus, and talar tilt [1].
A lateral talar displacement, by even one millimetre, would result in a decreased contact surface area by approximately 40 % which markedly increases the pressure of the area of the talus in contact with the tibia leading to degenerative arthritis. It has been recommended that any visible lateral displacement of the lateral malleolus should be reduced and that up to two millimetres of fibular shortening is acceptable [2–4].
Restoration of the ankle mortise, by adequate lengthening and correction of the angular and rotational deformities of the fibula, should restore the normal ankle biomechanics and prevent the development of degenerative joint disease [5–7].
In this study we present the results of treating malunited distal fibular fractures using a standard treatment approach.
Materials and methods
The material of this prospective study included the cases of 17 patients who were treated in the period between 2005 and 2009. There were eleven male and six female patients. Their ages ranged from 23 to 54 years (median 34 years). The inclusion criteria were, having a symptomatic ankle joint due to malunited distal fibular fracture, ankle range of motion more than 5° in either direction and osteoarthritis (OA) of the ankle joint radiologically diagnosed as grades 0, 1, 2 and 3 according to Kellgren–Lawrence Grading for osteoarthrosis (KL-OA grading); where Grade 0 indicates a definite absence of X-ray changes of osteo-arthrosis, Grade 1 doubtful, Grade 2 osteoarthrosis of minimal severity, and Grade 3 moderately severe osteoarthrosis [8]. Excluded from the study were patients having diabetic neuropathy or peripheral vascular insufficiency, stiff ankle joint, KL-OA Grade 4 (severe osteoarthrosis) and history of postoperative infection. The primary treatment was non-operative in four cases and operative in thirteen. The interval between the original injury and our treatment ranged from six to 18 months (median ten months). Table 1 summarises the demographic data of the study patients.
Table 1.
Demographic data of the study patients
| No. | Age | Sex | Side | Initial Tx. | Time to reconstruction | TCA | MCS | Fibular shortening | KL-OA Grade |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 54 | M | R | N-O | 8 months | 85° | 4 mm. | 6 mm. | 0 |
| 2 | 48 | M | R | N-O | 10 months | 86° | 4 mm. | 8 mm. | 0 |
| 3 | 23 | M | R | ORIF | 8 months | 86° | 6 mm. | 9 mm. | 0 |
| 4 | 27 | F | R | ORIF | 11 months | 85° | 4 mm. | 10 mm. | 1 |
| 5 | 34 | M | R | ORIF | 16 months | 88° | 6 mm. | 12 mm. | 3 |
| 6 | 30 | M | R | ORIF | 12 months | 85° | 5 mm. | 7 mm. | 0 |
| 7 | 39 | F | L | ORIF | 15 months | 86° | 6 mm. | 10 mm. | 0 |
| 8 | 30 | F | L | N-O | 9 months | 84° | 4 mm. | 6 mm. | 0 |
| 9 | 33 | F | L | ORIF | 6 months | 85° | 4 mm. | 6 mm. | 0 |
| 10 | 50 | M | L | ORIF | 11 months | 83° | 5 mm. | 7 mm. | 0 |
| 11 | 41 | M | R | ORIF | 13 months | 87° | 5 mm. | 9 mm. | 2 |
| 12 | 28 | M | R | ORIF | 9 months | 85° | 6 mm. | 10 mm. | 1 |
| 13 | 25 | M | L | ORIF | 10 months | 86° | 6 mm. | 10 mm. | 0 |
| 14 | 23 | M | L | ORIF | 6 months | 83° | 4 mm. | 7 mm. | 0 |
| 15 | 42 | F | L | ORIF | 7 months | 85° | 5 mm. | 6 mm. | 0 |
| 16 | 38 | F | R | ORIF | 18 months | 89° | 6 mm. | 10 mm. | 3 |
| 17 | 36 | M | R | N-O | 6 months | 86° | 5 mm. | 8 mm. | 0 |
| Median | 34 | 10 months | 85° | 5 mm. | 8 mm |
M male, F female, R right, L left, Initial Tx. initial treatment, N-O non-operative; ORIF open reduction and internal fixation, TCA talocrural angle (N. = 83 +/− 4°), MCS medial clear space (N. = <5 mm.), KL-OA score Kellgren–Lawrence osteoarthritis grade (0–4)
Preoperative evaluation
Clinical evaluation
The clinical examination involved assessment of the neurovascular status of the lower limb, local skin condition and previous operative scars, ankle and foot alignment while standing, and the range of movement and stability of the ankle with the patient sitting and standing. The American Orthopaedic Foot and Ankle Society (AOFAS) hind foot score was recorded [9].
Radiological evaluation
Included anteroposterior view of the ankle with 20° internal rotation and lateral view of the ankle and foot for both the affected and normal sides. Three radiological lines were examined as follows: 1, the joint space of which the line of the tibial plafond and the line of the surface of the talar dome should be strictly parallel; 2, a broken ‘Shenton’s line of the ankle’; 3, a broken curve between the lateral part of the talar articular surface and the fibular recess; indicative of fibular shortening . The talar tilt, the talocrural angle (TCA) (the angle formed by intersection of a line connecting the malleolar tips and the mid-diaphyseal line of the tibia). A difference of 2.5° or greater between both sides suggests fibular shortening; the medial clear space (MCS). The amount of fibular shortening was estimated on the radiographs by comparing the relationship between the medial and lateral malleolus on the affected side to those on the normal side. The degree of degenerative changes in the ankle joint were also assessed [1, 10–14]. CT scan examination was not routinely performed in this series of patients.
Surgical technique
The procedure was performed with the patient in the supine position, under image intensifier control and a tourniquet applied on the thigh to be deflated before wound closure for haemostasis. Through a lateral approach to the distal fibula, debridement of the syndesmotic scar tissue was performed to enable lengthening of the fibula and allow anatomical positioning of the lateral malleolus in the fibular notch of the tibia. A 2.5 mm Kirschner wire was then introduced from an anterolateral direction into the distal fibula and another wire was placed parallel to it in the proximal fibula to be used as guides for fibular derotation. Then, a transverse fibular osteotomy at the level of the malunion, was done, for lengthening and derotation of the lower end of the fibula. A lamina spreader was used for distraction of the osteotomy. Appropriate lengthening and rotation, as checked fluoroscopically, were defined by the following criteria: 1) appropriate closure of the medial clear space with restoration of the relationship of the medial malleolus and the medial surface of the talus, 2) an anatomical position of talus within the mortise with parallel articular surfaces of tibiotalar joint, and 3) restoration of the normal relationship of the medial and lateral malleoli. The resultant osteotomy gap was filled with autogenous bone graft taken from the lower metaphysis of the ipsilateral tibia. A 3.5 mm. reconstruction plate of suitable length was carefully contoured to the lower fibula and provisionally fixed by two plate holding forceps. The reduction was double checked under image intensifier before final fixation. The syndesmosis was fixed using two fully-threaded screws holding four cortices with the foot in the plantigrade position (Figs. 1 and 2). After wound closure, a posterior leg splint was applied. Leg elevation was ensured to avoid postoperative oedema and active non-weight bearing exercises were started when postoperative pain subsided. The postoperative management included partial weight bearing until complete healing of the osteotomy site, when the syndesmotic screw was removed through a stab wound under local anaesthesia. Hardware removal was performed only if local irritation of the skin occurred due to a prominent implant.
Fig. 1.
(a to d) a Radiographs of an ankle fracture treated by open reduction and internal fixation. The lateral malleolus was fixed in shortening and under-reduced. b Radiographs after implant removal show the lateral malleolus is united in external rotation and shortening, the medial clear space is widened and radiological evidence of osteoarthritis K-L grade 2. c Post-operative radiographs after reconstructive surgery. The fibular length and alignment are restored, the medial clear space is reduced to normal, and the resultant osteotomy gap is filled with a graft harvested from the ipsilateral distal tibial metaphysis. d Follow up radiographs after complete healing and implant removal
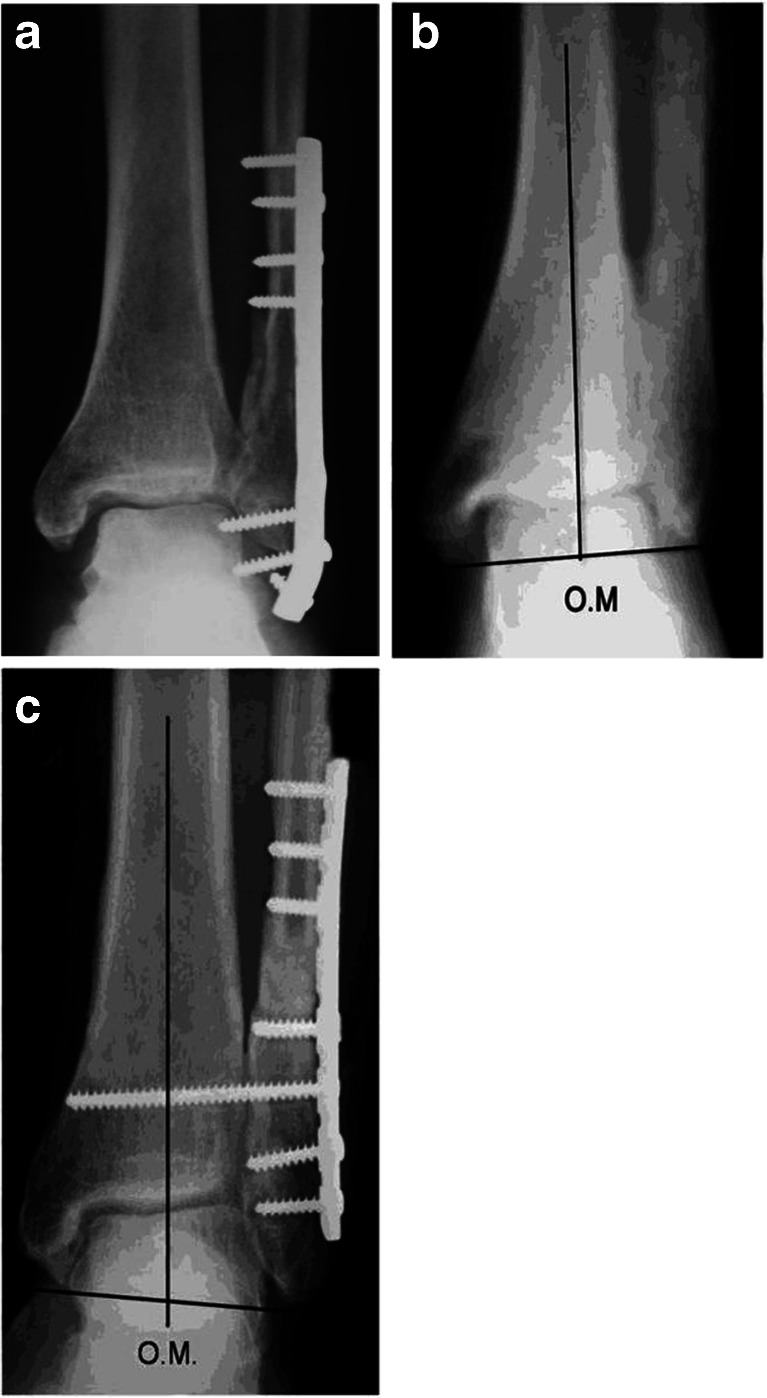
Fig. 2.
(a to c) a Radiographs of an ankle fracture treated by open reduction and internal fixation. The lateral malleolus was fixed in shortening. b Radiographs after implant removal show fibular shortening, increased talocrural angle (TCA) and widened medial clear space. c Follow-up radiograph shows complete healing of the osteotomy site and restoration fibular length and alignment
Evaluation of treatment results
Radiographs were obtained every month until bone healing and at the time of last follow up. The radiographs were examined for the radiographic criteria of anatomical reduction of the ankle and syndesmosis and the presence of osteoarthritis of the ankle joint and its grading (according to the K-L OA grading).
The clinical outcome was evaluated using the AOFAS clinical rating system, which incorporates both subjective and objective factors into numerical scales to describe function, alignment and pain. No radiological factors are included in this rating scale. In this system 50 points are assigned to function, 40 to pain and 10 to alignment. A score of 100 points is possible in a patient with no pain, full range of sagittal and hindfoot motion, no ankle or hindfoot instability, good alignment, ability to walk more than six blocks, ability to ambulate on any walking surface, no discernible limp, no limitation of daily or recreational activities and no assistive devices needed for ambulation. A score between 90 and 100 is excellent, 75–89 good, 60–74 fair and <60 indicates a poor outcome [9].
Results
The cases of 17 patients were available for review at the time of last follow up. Their ages ranged from 23 to 54 years (median 34 years). There were eleven males and six female patients. The right side was affected in ten patients and the left side in seven. The initial treatment was operative in 13 patients and non-operative in four. The time elapsed between the initial injury and our treatment ranged from six to 18 months (median ten months). Preoperative radiographs showed the talocrural angle (TCA) ranged from 83 to 89° (median 85°) and the medial clear space (MCS) four to six millimetres (median five millimetres). The preoperative fibular shortening ranged from six to 12 mm (median eight millimetres). Preoperative radiological evidence of osteoarthritis of the ankle was present in five cases [two grade 1, one grade 2, and two grade 3 (according to Kellgren–Lawrence OA grading)] (Table 1).
Fibular lengthening was performed in all cases and ranged from six to 12 mm. (median eight millimetres). The ankle range of motion (ROM) preoperatively ranged from 5/15° to 15/40° dorsiflexion/plantarflexion (median 10/25°). Follow up evaluation showed ankle ROM ranged from 5/10 to 15/45° (median 10/35°). The American Orthopaedic Foot and Ankle Society score (AOFAS) preoperatively ranged from 40 to 74 (median 60) and at follow up ranged from 50 to 95 (median 79). The follow-up ranged from 24 to 45 months (median 31 months) (Table 2).
Table 2.
Results of treatment
| No. | Fibular lengthening | Ankle ROM | AOFAS score | Follow up | ||
|---|---|---|---|---|---|---|
| DF/PF° | ||||||
| Preop. | Postop. | Preop. | Postop. | |||
| 1 | 6 mm. | 15/30 | 15/40 | 72 | 90 | 24 months |
| 2 | 8 mm. | 10/25 | 15/30 | 65 | 79 | 33 months |
| 3 | 8 mm. | 10/20 | 10/25 | 60 | 75 | 38 months |
| 4 | 9 mm. | 15/25 | 15/25 | 58 | 65 | 26 months |
| 5 | 12 mm. | 5/15 | 5/15 | 40 | 50 | 27 months |
| 6 | 6 mm. | 10/30 | 10/35 | 60 | 80 | 30 months |
| 7 | 11 mm. | 5/20 | 10/35 | 64 | 79 | 40 months |
| 8 | 6 mm. | 15/30 | 15/35 | 68 | 79 | 31 months |
| 9 | 7 mm. | 15/35 | 15/35 | 70 | 85 | 25 months |
| 10 | 7 mm. | 10/35 | 10/35 | 65 | 76 | 29 months |
| 11 | 8 mm. | 5/20 | 10/25 | 45 | 60 | 26 months |
| 12 | 10 mm. | 10/25 | 10/30 | 58 | 66 | 34 months |
| 13 | 9 mm. | 10/20 | 10/25 | 55 | 76 | 36 months |
| 14 | 7 mm. | 15/40 | 15/40 | 70 | 85 | 25 months |
| 15 | 7 mm. | 15/35 | 15/40 | 74 | 91 | 45 months |
| 16 | 10 mm. | 5/10 | 5/10 | 40 | 46 | 41 months |
| 17 | 7 mm. | 10/40 | 15/45 | 70 | 95 | 27 months |
| Median | 8 mm. | 10/25 | 10/35 | 60 | 79 | 31 months |
Ankle ROM ankle range of motion, DF/PF dorsiflexion/plantarflexion, Preop. preoperative, Postop. postoperative, AOFAS score American Orthopaedic Foot and Ankle Society score
The ankle ROM improved in all except five patients (29.4 %), who were diagnosed as having preoperative osteoarthritis of the ankle joint and limitation of the ROM.
All osteotomies healed in good alignment and no implant failure occurred in this series.
Progression of arthritic changes of the ankles was noted in one patient (case number 16), who had preoperative K-L osteoarthritis Grade 3; for this patient ankle arthrodesis was needed as a secondary procedure due to persistent pain and stiffness. Complications included skin irritation due to a prominent implant especially in skinny patients. Superficial wound infection occurred in one case, and a tender scar was observed in two cases which subsided by the time of last follow up.
The AOFAS score was excellent in three cases (17.6 %), good in nine cases (53 %), fair in three cases (17.6 %) and fair in two cases (11.8 %). Results were satisfactory (excellent and good) in 12 cases (70.6 %), and unsatisfactory (fair and poor) in five cases (29.4 %) due to stiffness of the ankle joint and pain secondary to the arthritic changes of the ankle joint.
Discussion
The fibula and interosseous membrane provide lateral stability for the ankle during late stance and push-off phases of the walking cycle. The downward movement of the fibula deepens the mortise and tightens the interosseous membrane, pulling the fibula medially and provides additional firm lateral support for the ankle during stress [15, 16].
The goal of any reconstructive intervention for malunion is to restore the anatomical alignment, joint congruency and ankle joint stability. Reconstruction may reduce the progression of degenerative changes and can decrease the symptoms of arthritis by decreasing instability and load on the arthritic locations of the joint [1, 17, 18].
Several procedures have been described for correction of malunited malleolar fractures and their benefit in terms of function and pain relief have been described. A transverse fibular osteotomy allows an easier derotation and significant amount of lengthening can be achieved. A successful reconstruction requires anatomical positioning of the lateral malleolus in the fibular notch of the tibia. Moreover, debridement of the syndesmotic scar tissue is mandatory to be able to lengthen the fibula, otherwise the fibula cannot be pushed downwards to the tibiofibular joint [1, 11–14, 17, 18].
In this study, a transverse fibular osteotomy was performed in all cases and autogenous bone graft, harvested from the ipsilateral distal tibial metaphysis, was used to fill the resultant defect. A satisfactory outcome (excellent and good) was obtained in 12 cases (70.6 %). The most important determinants of the clinical outcome were the presence of degenerative arthritis at the time of the osteotomy and the preoperative range of ankle motion (Table 2). An unsatisfactory (fair and poor) outcome occurred in the patients who were diagnosed, preoperatively, as having osteoarthritis and those who had a limited range of ankle motion. Despite this unsatisfactory outcome in those cases (n. 5; 29.4 %), they benefitted from the procedure in terms of reduction of pain and improved function at work.
Weber and Simpson in their evaluation of 23 patients with fibular malunion, treated by corrective lengthening osteotomy, (74 %) were graded good to excellent and (26 %) were fair to poor [11]. Offierski reported the results of treatment of 11 patients with fibular malunion treated by lengthening osteotomy and reported (91 %) fair to good [18]. Clinical factors affecting outcome were mostly thought to be the quality of reduction and the presence of osteoarthritis at the time of revision. On the other hand, Marti and colleagues suggested that the clinical outcome was mainly related to the preoperative mobility of the ankle joint. Only a severely disturbed ankle function was considered a contraindication for reconstructive surgery [17].
Realignment-lengthening osteotomy of the fibula is expected to improve the biomechanics of the ankle and slow the degenerative process, however, the procedure does not address the pre-existing arthritic changes.
In their study, Intema et al. demonstrated that treatment of advanced post-traumatic ankle osteoarthritis with joint distraction produced an overall decrease of subchondral bone density, which persisted for at least two years, and resolution of subchondral bone cysts which was correlated to the clinical improvement in their patients [19].
In the light of our results we believe that lengthening-realignment osteotomy of the fibular malunion leads to reasonable improvement of ankle function and pain relief. Progression of arthritic changes in some patients is an unavoidable sequel to the original trauma. Further investigations are needed to examine the possible benefits of articulated distraction arthrodiastasis of the ankle joint as a secondary procedure to improve the clinical outcome in the patients who have arthritic and stiff ankle joint.
References
- 1.van Wensen RJ, van den Bekerom MP, Marti RK, van Heerwaarden RJ. Reconstructive osteotomy of fibular malunion: review of the literature. Strateg Trauma Limb Reconstr. 2011;6(2):51–57. doi: 10.1007/s11751-011-0107-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yablon IG, Heller FG, Shouse L. The key role of the lateral malleolus in displaced fractures of the ankle. J Bone Joint Surg Am. 1977;59(2):169–173. [PubMed] [Google Scholar]
- 3.Clarke HJ, Michelson JD, Cox QG, Jinnah RH. Tibio-talar stability in bimalleolar ankle fractures: a dynamic in vitro contact area study. Foot Ankle. 1991;11(4):222–227. doi: 10.1177/107110079101100407. [DOI] [PubMed] [Google Scholar]
- 4.Kimizuka M, Kurosawa H, Fukubayashi T. Load-bearing pattern of the ankle joint. Contact area and pressure distribution. Arch Orthop Trauma Surg. 1980;96(1):45–49. doi: 10.1007/BF01246141. [DOI] [PubMed] [Google Scholar]
- 5.Vrahas M, Fu F, Veenis B. Intraarticular contact stresses with simulated ankle malunions. J Orthop Trauma. 1994;8(2):159–166. doi: 10.1097/00005131-199404000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Curtis MJ, Michelson JD, Urquhart MW, Byank RP, Jinnah RH. Tibiotalar contact and fibular malunion in ankle fractures. A cadaver study. Acta Orthop Scand. 1992;63(3):326–329. doi: 10.3109/17453679209154793. [DOI] [PubMed] [Google Scholar]
- 7.Thordarson DB, Motamed S, Hedman T, Ebramzadeh E, Bakshian S. The effect of fibular malreduction on contact pressures in an ankle fracture malunion model. J Bone Joint Surg Am. 1997;79(12):1809–1815. doi: 10.2106/00004623-199712000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 10.Stufkens SA, Barg A, Bolliger L, Stucinskas J, Knupp M, Hintermann B. Measurement of the medial distal tibial angle. Foot Ankle Int. 2011;32(3):288–293. doi: 10.3113/FAI.2011.0288. [DOI] [PubMed] [Google Scholar]
- 11.Weber BG, Simpson LA. Corrective lengthening osteotomy of the fibula. Clin Orthop Relat Res. 1985;199:61–67. [PubMed] [Google Scholar]
- 12.Ward AJ, Ackroyd CE, Baker AS. Late lengthening of the fibula for malaligned ankle fractures. J Bone Joint Surg Br. 1990;72(4):714–717. doi: 10.1302/0301-620X.72B4.2116417. [DOI] [PubMed] [Google Scholar]
- 13.Weber D, Friederich NF, Müller W. Lengthening osteotomy of the fibula for post-traumatic malunion. Indications, technique and results. Int Orthop. 1998;22(3):149–152. doi: 10.1007/s002640050229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reidsma II, Nolte PA, Marti RK, Raaymakers EL. Treatment of malunited fractures of the ankle: a long-term follow-up of reconstructive surgery. J Bone Joint Surg Br. 2010;92(1):66–70. doi: 10.1302/0301-620X.92B1.22540. [DOI] [PubMed] [Google Scholar]
- 15.Wang Q, Whittle M, Cunningham J, Kenwright J. Fibula and its ligaments in load transmission and ankle joint stability. Clin Orthop Relat Res. 1996;330:261–270. doi: 10.1097/00003086-199609000-00034. [DOI] [PubMed] [Google Scholar]
- 16.Scranton PE, Jr, McMaster JG, Kelly E. Dynamic fibular function: a new concept. Clin Orthop Relat Res. 1976;118:76–81. [PubMed] [Google Scholar]
- 17.Marti RK, Raaymakers EL, Nolte PA. Malunited ankle fractures. The late results of reconstruction. J Bone Joint Surg Br. 1990;72(4):709–713. doi: 10.1302/0301-620X.72B4.2116416. [DOI] [PubMed] [Google Scholar]
- 18.Offierski CM, Graham JD, Hall JH, Harris WR, Schatzker JL. Late revision of fibular malunion in ankle fractures. Clin Orthop Relat Res. 1982;171:145–149. [PubMed] [Google Scholar]
- 19.Intema F, Thomas TP, Anderson DD, Elkins JM, Brown TD, Amendola A, Lafeber FP, Saltzman CL. Subchondral bone remodeling is related to clinical improvement after joint distraction in the treatment of ankle osteoarthritis. Osteoarthr Cartil. 2011;19(6):668–675. doi: 10.1016/j.joca.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]