Abstract
Purpose
The disease activity score including 28 joints (DAS28), the simplified disease activity index and the clinical disease activity index (CDAI) were developed in order to provide a quantifiable measure of rheumatoid arthritis (RA) activity. Although inflamed hip joints greatly impact activities of daily living (ADL) and walking ability, the hip joint was not included in the DAS28, SDAI or CDAI assessments. Although excellent clinical results have been reported for total hip arthroplasty (THA) in RA patients, correlations between disease activity and hip function in RA patients after THA remain unknown.
Methods
We analysed the effect of RA disease activity on a hip function score in an observational cohort of RA patients after THA. Twenty-five registered RA patients who had undergone THA (33 joints) were included. Hip function was recorded and RA disease activity was measured on the same day. The mean age of the patients was 65.17 years. They were followed up for a mean of 5.24 years after surgery. The mean duration of disease following RA diagnosis for this patient group was 19.47 years. The Japanese Orthopaedic Association (JOA) hip score was used as a clinical outcome measure for hip dysfunction. RA disease activity and health-related quality of life were measured using the DAS28, SDAI, CDAI and the modified health assessment questionnaire (MHAQ).
Results
The mean JOA score for hip function was 80.48 at the final follow-up. The mean DAS28-ESR, DAS28-CRP, SDAI, CDAI and MHAQ measuring RA disease activity levels were 3.38, 2.65, 9.59, 8.63 and 0.44, respectively, at the final follow-up. There was a significant negative correlation between the JOA hip score and all disease activity assessments observed after THA (DAS-ESR [P = 0.0067], DAS-CRP [P = 0.0008]), SDAI [P = 0.0034], CDAI [P = 0.0003]) and MHAQ [P = 0.0002]).
Conclusion
We found significant negative correlations between JOA hip scores and all disease activity assessments in RA patients treated with THA.
Introduction
Rheumatoid arthritis (RA) is characterised by inflammation of the synovial membrane, leading to invasion of synovial tissue into the adjacent cartilage matrix with degradation of articular cartilage and bone as a consequence. This results in bone erosion, which is often observed as marginal joint erosions radiographically and is predictive of a poor prognosis [1]. The course of RA varies greatly, from a mild disease to a severe destructive variant that progress rapidly over a few years. Orthopaedic procedures can substantially improve the overall function and quality of life for RA patients [2]. Though excellent clinical results have been reported for total hip arthroplasty (THA) in RA patients, the effects of RA disease activity on hip function after THA remain unknown. The disease activity score including 28 joints (DAS28) [3], the simplified disease activity index (SDAI) [4] and the clinical disease activity index (CDAI) [5] were developed in order to provide a quantifiable measure of rheumatoid arthritis (RA) activity. Inflamed hip joints greatly impact activities of daily living (ADL) and walking ability, however the hip joint was not included in the DAS28, SDAI and CDAI assessments.
This analysis aimed to assess correlations in RA disease activity and the JOA hip score after THA in patients with established RA. We analysed the JOA hip score as a measure of hip function to determine whether improved hip function contributed to a decrease in RA disease activity score after THA.
Patients and methods
We retrospectively reviewed 33 THA procedures from 25 RA patients who were followed up for more than one year in the Department of Orthopaedic Surgery at Mie University Hospital between 1997 and 2010. Each had a hip function assessment and a RA disease activity assessment on the same day.
The mean patient age was 65.17 years (range, 38–84 years) (Table 1). There were three male (five hips) and 22 female patients (28 hips) included in the study. Patients were followed up for a mean of 5.24 years (range, 1.5–19). All patients were Japanese and fulfilled the 1987 revised American College of Rheumatology criteria for RA [6].
Table 1.
Characteristics of the study population (n = 25 patients, 33 joints) at final follow-up
| Variables | Mean ± SD | Range |
|---|---|---|
| Age, years | 65.17 ± 8.91 | 38–84 |
| RA disease duration, years | 19.47 ± 12.48 | 2–47 |
| Patient global assessment (0–10 cm) | 2.66 ± 2.07 | 0.3–6.2 |
| Physician global assessment (0–10 cm) | 2.31 ± 1.81 | 0.0–6.7 |
| ESR, mm/h | 31.36 ± 25.27 | 0–90 |
| CRP, mg/dL | 0.96 ± 1.35 | 0.02–4.51 |
| Tender joints count (0–28) | 1.85 ± 2.03 | 0–9 |
| Swollen joints count (0–28) | 1.82 ± 1.47 | 0–6 |
| DAS28-ESR | 3.38 ± 1.43 | 0.81–6.04 |
| DAS28-CRP | 2.65 ± 1.13 | 1.29–5.21 |
| SDAI (0–86) | 9.59 ± 6.91 | 1.72–27.33 |
| CDAI (0–76) | 8.63 ± 6.22 | 1.60–23.90 |
| MHAQ (0–3) | 0.44 ± 0.63 | 0–2.25 |
| Post THA duration, years | 5.24 ± 3.83 | 1.5–19 |
| JOA total (0–100) | 80.48 ± 12.39 | 39–99 |
| Pain (0–40) | 36.52 ± 5.93 | 10–40 |
| Range of motion (0–20) | 17.42 ± 1.92 | 12–20 |
| Ability to walk (0–20) | 13.45 ± 4.50 | 5–20 |
| Activities of daily living (0–20) | 13.09 ± 5.00 | 2–20 |
DAS28 disease activity score including 28 joints, SDAI simplified disease activity index, CDAI clinical disease activity index, MHAQ modified health assessment questionnaire, JOA Japanese Orthopaedic Association
Clinical hip function outcomes were evaluated using the Japanese Orthopaedic Association (JOA) hip score [7]. The JOA hip score consists of four subcategories: pain (Pain) (up to 40 points), range of motion (ROM), ability to walk (Walk), and activities of daily living (ADL) (each up to 20 points). A perfect JOA hip score is 100 and the worst score is 0. To focus on functional ability, we also evaluated the sum scores (Walk and ADL) where a perfect score was 40, and the worst score was 0.
The mean duration of disease after RA diagnosis was 19.47 years (range two–47 years) (Table 1). Predonisolone was used to treat RA in 16 patients, methotrexate was used in 15 patients, other oral DMARDs (disease modifying antirheumatic drugs) were used in 11 patients, and bioagents were used in 12 patients (nine etanercept and three tocilizumab). The RA disease progression was assessed with Steinbrocker radiographic stages. Four patients (four THA) were in stage II, four patients (six THA) were in stage III, and 17 patients (23 THA) were in stage IV. More than half of the patients had advanced to Steinbrocker radiographic stage IV. Fifteen patients (21 joints) were treated with additional or exchange pharmacological agents due to poor control during the follow-up period after THA. Though the patients with additional or exchange pharmacological agents were treated more, the disease activity tended to be high, but not significant compared with those of the same pharmacological agents (Table 2).
Table 2.
RA disease activity of additional or exchange pharmacological agents compared with those of the same pharmacological agents during the follow-up period after THA
| Variable | Same pharmacologic agents (10 patients, 12 joints) | Additional or exchange pharmacologic agents (15patients, 21 joints) | P value |
|---|---|---|---|
| Mean ± SD | |||
| DAS28-ESR | 2.93 ± 1.37 | 3.63 ± 1.43 | 0.1807 |
| DAS28-CRP | 2.15 ± 0.97 | 2.94 ± 1.13 | 0.0516 |
| SDAI | 6.77 ± 5.54 | 11.20 ± 7.21 | 0.0757 |
| CDAI | 6.26 ± 5.36 | 9.99 ± 6.39 | 0.0985 |
| MHAQ | 0.60 ± 0.81 | 0.35 ± 0.50 | 0.2743 |
DAS28 disease activity score including 28 joints, SDAI simplified disease activity index, CDAI clinical disease activity index, MHAQ modified health assessment questionnaire
There was no significant RA disease activity between the patients treated with additional or exchange pharmacological agents and the patients with the same pharmacological agents
RA disease activity was assessed by DAS28, SDAI, CDAI and the modified health assessment questionnaire (MHAQ) [8]. The health assessment questionnaire (HAQ) and its modified version, the MHAQ, quantify disability in activities of daily living (ADL) in patients with rheumatoid arthritis. The following were recorded for each patient: tender joints count (TJC), swollen joints count (SJC), patient global assessment (PGA), physician global assessment (PhGA), ESR and CRP. The following formulae were used to calculate the DAS28, SDAI and CDAI, respectively: (1)  ; (2)
; (2)  ; (3)
; (3)  ; (4)
; (4)  , where SJC and TJC are the respective counts for 28 joints.
, where SJC and TJC are the respective counts for 28 joints.
Informed consent was obtained from each patient, and the study received approval from the local ethics committee.
Statistical analysis
Data were presented as the percentage of the mean ± standard deviation (SD). Data analyses were performed using Stat View 5.0 for Windows. Correlations between JOA score and RA disease activity assessment were analysed using Spearman’s test. P values ≤ 0.05 were considered statistically significant.
Results
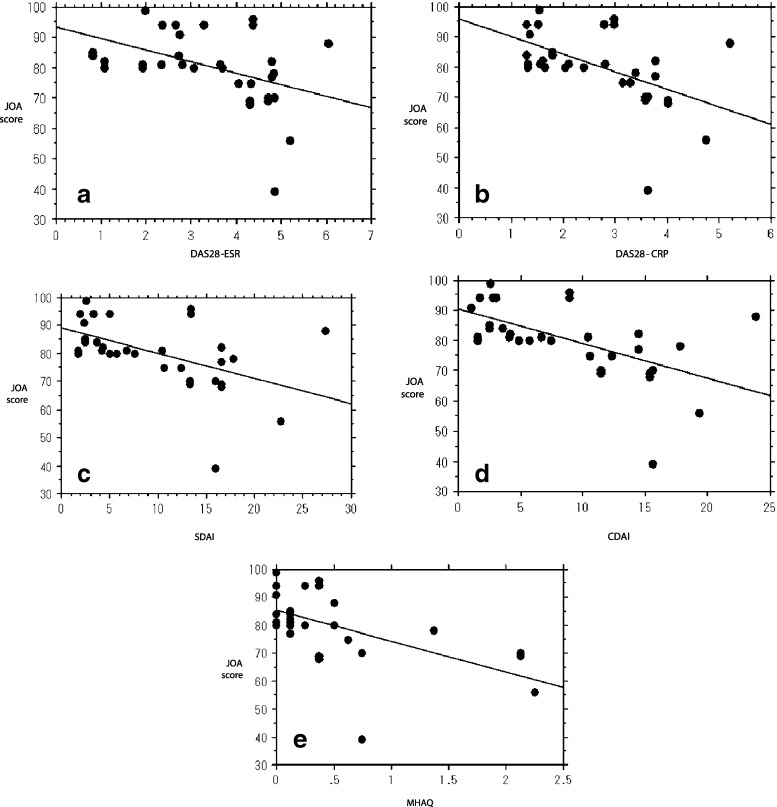
RA disease activity and hip function scores at final follow-up are shown in Table 1. The mean preoperative JOA hip score of 46.00 ± 14.80 improved significantly to 80.48 ± 12.39 postoperatively at final follow-up. A significant correlation in JOA hip score and all disease activity assessments was observed after THA (DAS-ESR [P = 0.0067], DAS-CRP [P = 0.0008]), SDAI [P = 0.0034], CDAI [P = 0.0003] and MHAQ [P = 0.0002]; Table 3). We found significant negative correlations between JOA hip score and all disease activity assessments in RA patients treated with THA (Table 3, Fig. 1a–e).
Table 3.
Correlation p values between JOA score and RA disease activity assessment
| Variable | JOA score | Pain | ROM | Walk | ADL | Sum score Walk+ADL |
|---|---|---|---|---|---|---|
| DAS28-ESR | 0.0067 | 0.2101 | 0.4538 | 0.0746 | 0.0052 | 0.0080 |
| DAS28-CRP | 0.0008 | 0.3792 | 0.6408 | 0.0006 | 0.0017 | 0.0002 |
| SDAI | 0.0034 | 0.3483 | 0.8307 | 0.0079 | 0.0019 | 0.0015 |
| CDAI | 0.0003 | 0.2159 | 0.4884 | 0.0015 | 0.0003 | 0.0002 |
| MHAQ | 0.0002 | 0.6885 | 0.3518 | 0.0015 | <0.0001 | <0.0001 |
DAS28 disease activity score including 28 joints, SDAI simplified disease activity index, CDAI clinical disease activity index, MHAQ modified health assessment questionnaire, JOA Japanese Orthopaedic Association
Correlation p values between the JOA hip score and RA disease activity score was calculated. The JOA hip score was correlated with DAS28, SDAI, CDAI and MHAQ in RA patients after total hip arthroplasty. The activities of daily living (ADL) and ability to walk (Walk) parameters were strong contributors to the decrease in DAS28, SDAI, CDAI and MHAQ scores after THA
Fig. 1.
There were negative correlations between JOA hip score and disease activity in RA patients. a DAS28-ESR (R2 = 0.193). b DAS28-CRP (R2 = 0.282). c SDAI (R2 = 0.252). d CDAI (R2 = 0.330). e MHAQ (R2 = 0.320)
Next, we evaluated correlations between RA disease activity assessment and four subcategories of the JOA hip score (Table 3). There were significant correlations among JOA hip score parameters of ADL (DAS-ESR [P = 0.0052], DAS-CRP [P = 0.0017]), SDAI [P = 0.0019], CDAI [P = 0.0003], MHAQ [P < 0.0001]) and ability to walk (DAS-CRP [P = 0.0006], SDAI [P = 0.0079], CDAI [P = 0.0015], MHAQ [P = 0.0015]). However, the pain score and the ROM score were also not correlated with RA disease activity.
We investigated RA disease activity between high (more than average) and low (below average) JOA hip score patients at final follow-up. The mean RA disease activity score was significantly lower in the more than average JOA hip score group than in the below average group (Table 4).
Table 4.
RA disease activity between JOA high and low hip score patients
| Variables | High hip score (≥81) (18 joints) | Low hip score (≤80) (15 joints) | P value |
|---|---|---|---|
| Mean ± SD | |||
| DAS28-ESR | 2.82 ± 1.41 | 4.05 ± 1.18 | 0.0113 |
| DAS28-CRP | 2.18 ± 1.06 | 3.22 ± 0.96 | 0.0064 |
| SDAI | 6.93 ± 6.84 | 12.79 ± 5.67 | 0.0128 |
| CDAI | 5.86 ± 5.80 | 11.95 ± 5.10 | 0.0034 |
| MHAQ | 0.13 ± 0.16 | 0.83 ± 0.77 | 0.0007 |
DAS28 disease activity score including 28 joints, SDAI simplified disease activity index, CDAI clinical disease activity index, MHAQ modified health assessment questionnaire, JOA Japanese Orthopaedic Association
The mean RA disease activity score was significantly lower in the more than average than in the below average JOA score group
In addition, we evaluated correlations between RA disease activity assessment and the JOA hip score. There were significant correlations among RA disease activity of tender joints [P = 0.0009], swollen joints [P = 0.0023], PGA [P = 0.0063] and PhGA [P = 0.0008]. However, ESR [P = 0.2507] and CRP [P = 0.7120] score were also not correlated with JOA hip score.
Discussion
The course of RA varies greatly from a mild, even self-limiting, disease to a severe destructive variant that progresses rapidly [9]. The efficacy of TNF-α blockers is now well established in patients with rheumatoid arthritis (RA) [10–12], and these types of drugs are being prescribed more and more frequently. Their use in patients with rheumatic disorders has led to less joint destruction and has greatly improved functional patient prognosis [13, 14].
The requirement for TJA tended to decrease in rheumatoid patients before the use of TNF-α blockers in rheumatology, thanks to strategies of earlier and more intensive management of recent rheumatic disorders [15, 16]. However, the need for TJA remains frequent, particularly due to joint destruction occurring before the introduction of TNF-α blockers or due to failure of medical therapy. In patients with chronic RA, one, or more often, both, hips are involved, and THA has become the gold standard for the treatment of hips destroyed by RA [17, 18]. The hip and knee joints are among the largest joints in the body, and it is possible that inflammation of these joints greatly affects RA disease activity. The inflamed synovium in RA produces many cytokines and chemokines that promote joint cartilage destruction. It might be postulated that synovectomy decreases the amount of inflamed synovium, and the replacement of the degenerative and pathological articular cartilage with other components during THA and TKA may reduce disease activity and restore drug efficacy. However, subsequent pharmacological management still remains necessary in these RA patients for improved control of their RA activity. THA and TKA may possibly have additional effects on RA disease activity.
Previously, it was reported that disease activity after THA and TKA, as evaluated by the DAS28, had decreased in patients with RA [19]. Inflamed knee joints greatly affect RA disease activity, and are readily identified because the knee joint is included in the DAS28, SDAI and CDAI assessments. Although inflamed hip joints greatly affect ADL and walking ability, the hip joint was not included in the DAS28, SDAI and CDAI assessments. The clinical results of our study demonstrated a negative correlation between RA disease activity and the hip function score.
The JOA hip score has been widely used in Japan as a method to assess hip joint diseases. The JOA consists of four items (pain, range of motion in the operated hip, walking ability, and ADL). It has been reported to verify the reliability and validity of the JOA hip score [7]. We found clearly that all decreases in disease activity assessment scores were correlated with increases in ADL and walking ability, as identified by JOA hip score parameters. On the other hand, factors that appear to reflect more directly the effect of total joint replacement such as pain and ROM did not show correlation with RA activity scores. And, we found significant correlation between JOA hip score and scores of tender joints, swollen joints, PGA and PhGA in disease activity scores. In addition, we found a negative correlation of MHAQ score as function score of polyarthritic diseases with JOA hip score. In rheumatology, the most widely used self report questionnaires are the health assessment questionnaire (HAQ), and its modified version the MHAQ, which were developed to measure disability in daily activities in patients with rheumatoid arthritis. Furthermore, the HAQ has been shown to predict severe outcomes of rheumatoid arthritis such as hip replacement surgery [9]. Therefore, these results suggest that tight control of RA disease activity using pharmacological agents, including biologics, is still required in patients with RA after THA to decrease disease activity and improve function.
Limitations of this study are that this was a small retrospective design, and a control group was not included. We were also unable to evaluate RA disease activity before and after THA treatment, and were unable to evaluate JOA hip score before and after RA treatment. In future studies, we propose investigating RA disease activity and JOA hip scores prospectively in patients undergoing THA or RA treatment.
In conclusion, we found significant negative correlations between JOA hip scores and all disease activity assessments in RA patients treated with THA. The mean RA disease activity score was significantly lower in the more than average JOA hip score group. Our results suggest the level of RA disease control may have an effect on increasing hip function in RA patients after THA.
Acknowledgments
No benefits or funds were received in support of the study.
Conflict of interest
The authors have declared no conflicts of interest.
References
- 1.Van Zeben D, Hazes JM, Zwinderman AH, Vandenbroucke JP, Breedveld FC. Factors predicting outcome of rheumatoid arthritis: results of a followup study. J Rheumatol. 1993;20:1288–1296. [PubMed] [Google Scholar]
- 2.Anderson RJ. The orthopedic management of rheumatoid arthritis. Arthritis Care Res. 1996;9:223–228. doi: 10.1002/1529-0131(199606)9:3<223::AID-ANR1790090311>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 3.Prevoo ML, van’t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL. Modified disease activity scores that include twenty–eight–joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995;48:3844–3848. doi: 10.1002/art.1780380107. [DOI] [PubMed] [Google Scholar]
- 4.Smolen JS, Breedveld FC, Schiff MH, Kalden JR, Emery P, Eberl G, van Riel PL, Tugwell P. A simplified disease activity index for rheumatoid arthritis for use in clinical practice. Rheumatology (Oxford) 2003;42:244–257. doi: 10.1093/rheumatology/keg072. [DOI] [PubMed] [Google Scholar]
- 5.Aletaha D, Nell VP, Stamm T, Uffmann M, Pflugbeil S, Machold K, Smolen JS. Acute phase reactants add little to disease activity indices for rheumatoid arthritis- validation of a clinical activity score. Arthritis Res Ther. 2005;7:796–806. doi: 10.1186/ar1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–324. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- 7.Kuribayashi M, Takahashi KA, Fujioka M, Ueshima K, Inoue S, Kubo T. Reliability and validity of the Japanese Orthopaedic Association hip score. J Orthop Sci. 2010;15:452–458. doi: 10.1007/s00776-010-1490-0. [DOI] [PubMed] [Google Scholar]
- 8.Pincus T, Summey JA, Soraci SA, Wallston KA, Hummon NP. Assessment of patient satisfaction in activities of daily living using a modified Stanford health assessment questionnaire. Arthritis Rheum. 1983;26:1346–1353. doi: 10.1002/art.1780261107. [DOI] [PubMed] [Google Scholar]
- 9.Wolfe F, Zwillich SH. The long-term outcomes of rheumatoid arthritis: a 23-year prospective, longitudinal study of total joint replacement and its predictors in 1,600 patients with rheumatoid arthritis. Arthritis Rheum. 1998;41:1072–1082. doi: 10.1002/1529-0131(199806)41:6<1072::AID-ART14>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 10.Lee YH, Woo JH, Rho YH, Choi SJ, Ji JD, Song GG. Meta-analysis of the combination of TNF inhibitors plus MTX compared to MTX monotherapy, and the adjusted indirect comparison of TNF inhibitors in patients suffering from active rheumatoid arthritis. Rheumatol Int. 2008;28:553–559. doi: 10.1007/s00296-007-0475-6. [DOI] [PubMed] [Google Scholar]
- 11.Koike T, Harigai M, Inokuma S, Ishiguro N, Ryu J, Takeuchi T, Tanaka Y, Yamanaka H, Fujii K, Yoshinaga T, Freundlich B, Suzukawa M. Safety and effectiveness responses to etanercept for rheumatoid arthritis in Japan: a sub-analysis of a post-marketing surveillance study focusing on the duration of rheumatoid arthritis. Rheumatol Int. 2012;32:1511–1519. doi: 10.1007/s00296-010-1784-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wiens A, Correr CJ, Venson R, Otuki MF, Pontarolo R. A systematic review and meta-analysis of the efficacy and safety of adalimumab for treating rheumatoid arthritis. Rheumatol Int. 2010;30:1063–1070. doi: 10.1007/s00296-009-1111-4. [DOI] [PubMed] [Google Scholar]
- 13.Takeuchi T, Miyasaka N, Inoue K, Abe T, Koike T, RISING study Impact of trough serum level on radiographic and clinical response to infliximab plus methotrexate in patients with rheumatoid arthritis: results from the RISING study. Mod Rheumatol. 2009;19:478–487. doi: 10.1007/s10165-009-0195-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van der Heijde D, Klareskog L, Landewé R, Bruyn GA, Cantagrel A, Durez P, Herrero-Beaumont G, Molad Y, Codreanu C, Valentini G, Zahora R, Pedersen R, MacPeek D, Wajdula J, Fatenejad S. Disease remission and sustained halting of radiographic progression with combination etanercept and methotrexate in patients with rheumatoid arthritis. Arthritis Rheum. 2007;56:3928–3939. doi: 10.1002/art.23141. [DOI] [PubMed] [Google Scholar]
- 15.Louie GH, Ward MM. Changes in the rates of joint surgery among patients with rheumatoid arthritis in California, 1983–2007. Ann Rheum Dis. 2010;69:868–871. doi: 10.1136/ard.2009.112474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Momohara S, Inoue E, Ikari K, Kawamura K, Tsukahara S, Iwamoto T, Hara M, Taniguchi A, Yamanaka H. Decrease in orthopaedic operations, including total joint replacements, in patients with rheumatoid arthritis between 2001 and 2007: data from Japanese outpatients in a single institute-based large observational cohort (IORRA) Ann Rheum Dis. 2010;69:312–313. doi: 10.1136/ard.2009.107599. [DOI] [PubMed] [Google Scholar]
- 17.Rud-Sørensen C, Pedersen AB, Johnsen SP, Riis AH, Overgaard S. Survival of primary total hip arthroplasty in rheumatoid arthritis patients. Acta Orthop. 2010;81:60–65. doi: 10.3109/17453671003685418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zwartele R, Peters A, Brouwers J, Olsthoorn P, Brand R, Doets C. Long-term results of cementless primary total hip arthroplasty with a threaded cup and a tapered, rectangular titanium stem in rheumatoid arthritis and osteoarthritis. Int Orthop. 2008;32:581–587. doi: 10.1007/s00264-007-0383-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Momohara S, Inoue E, Ikari K, Yano K, Tokita A, Suzuki T, Sakuma Y, Hiroshima R, Kawakami K, Masuda I, Iwamoto T, Taniguchi A, Yamanaka H. Efficacy of total joint arthroplasty in patients with established rheumatoid arthritis: improved longitudinal effects on disease activity but not on health-related quality of life. Mod Rheumatol. 2011;21:476–481. doi: 10.1007/s10165-011-0432-9. [DOI] [PubMed] [Google Scholar]