Abstract
Purpose
The place of arthroscopic treatment in osteoarthritis of the knee has generated much controversy. A survey was initiated to collect the opinion of experienced surgeons.
Methods
Of the 211 surgeons interviewed, 170 (80.6 %) replied to the electronic questionnaire. Respondents had at least ten years of experience in arthroscopy and currently perform more than 100 arthroscopies per year. Various indications and treatment modalities for arthroscopy in osteoarthritis of the knee had to be evaluated on a scale from “excellent” to “no indication”.
Results
The respondents generally believe that an improvement is more likely in low-grade osteoarthritis (p < 0.001) and in neutral leg axis (p < 0.001). The outcome was rated better if symptoms had persisted for less than six months (p < 0.001) and for patients that were younger than 60 years (p < 0.001). Partial meniscectomy and notchplasty in cases of extension deficit were considered as successful treatment options. Debridement was an accepted indication, with an outcome mainly rated as fair. A majority saw no indication for joint lavage, arthroscopic treatment of arthrofibrosis and removal of osteophytes. The outcome appears to be poor if a bone edema is diagnosed on magnetic resonance imaging prior to arthroscopy. Only 55.9 % of respondents were comfortable with the current definition of osteoarthritis.
Conclusions
Experienced arthroscopic surgeons all over Europe believe arthroscopy in osteoarthritis is appropriate, under certain conditions. The major task for surgeons is to select the right patients who are likely to benefit from this intervention.
Introduction
Arthroscopic treatment in osteoarthritis of the knee is routinely performed in clinical practice. In 2002 Moseley et al. initiated the debate on its usefulness, after conducting a widely respected placebo-controlled trial [1]. They reported that the outcome after arthroscopic lavage or debridement did not show better results than placebo procedures. Potts et al. [2] in 2012 analysed practice patterns for arthroscopy in osteoarthritis in the USA and reported that the number of knee arthroscopies significantly decreased after publication of the study by Moseley et al. The total number of knee arthroscopies decreased and the percentage of knee arthroscopies in osteoarthritis cases fell from 19.8 % (2003) to 13.4 % (2007).
During the last decade, various randomised controlled trials have questioned this issue and concluded that arthroscopic surgery for osteoarthritis is not effective [3–5]. The American Academy of Orthopaedic Surgeons (AAOS) advises against performing arthroscopic debridement or lavage in patients with a primary diagnosis of symptomatic osteoarthritis of the knee [6].
In contrast, several studies, mainly case series, showed that subgroups of patients sustained benefit from arthroscopic intervention [7–9]. Dervin et al. showed in a trial including 126 patients with osteoarthritis of the knee that it is difficult to predict the outcome of arthroscopic interventions [10].
The aim of our survey was to highlight the results of treatment by experienced European arthroscopic surgeons and to analyse whether the AAOS recommendations should be incorporated into clinical practice.
Materials and methods
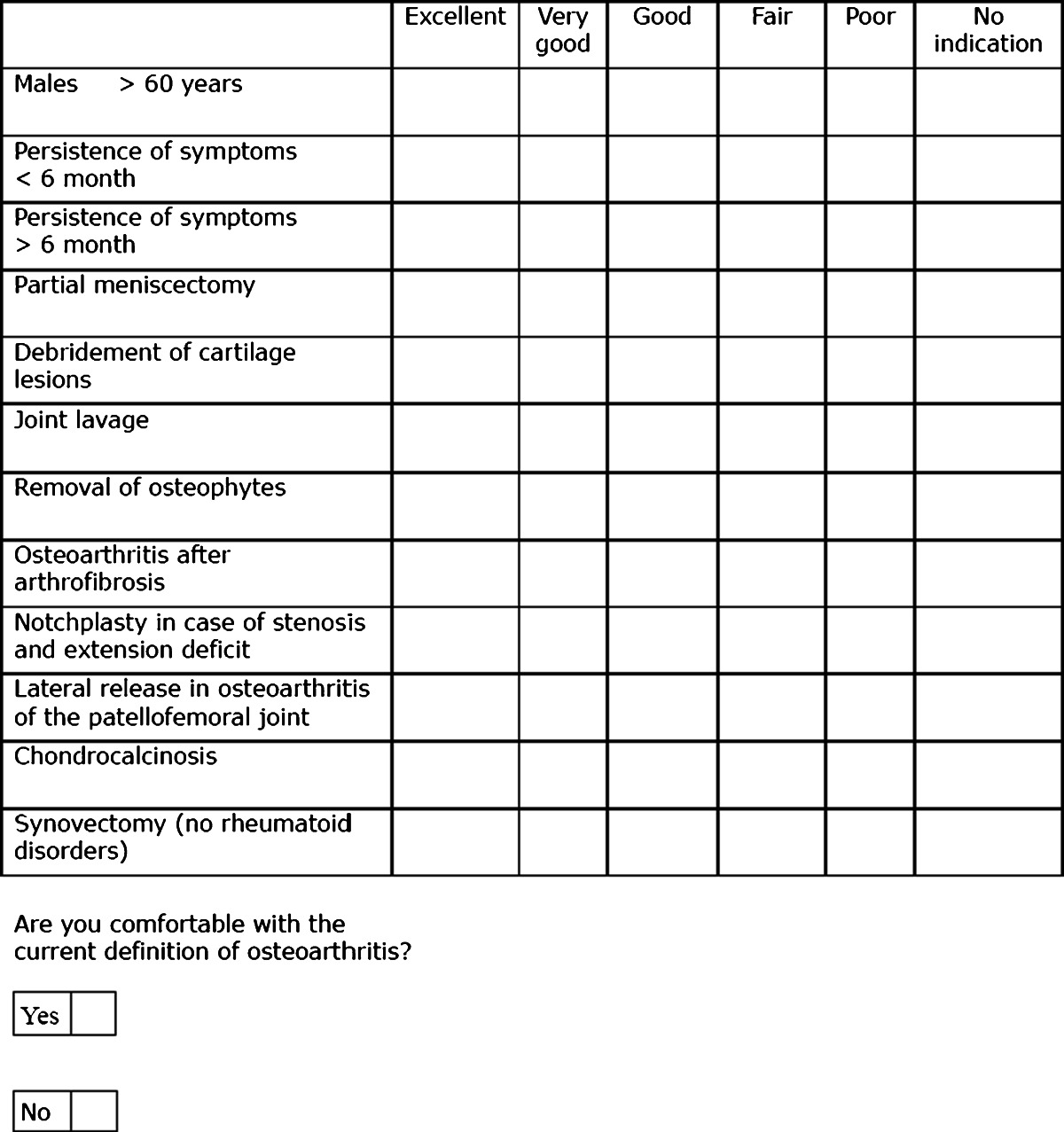
This study was initiated to explore indication modalities and outcome after arthroscopy in osteoarthritic knees. Therefore, a survey of highly experienced surgeons of the European Society of Sports Traumatology Knee Surgery and Arthroscopy (ESSKA) was started. The survey addressed ESSKA members with a minimum of ten years practical experience in the field of arthroscopy who currently perform at least 100 knee arthroscopies per year. To select suitable participants, ESSKA requested all members to indicate their experience via email. Members had to choose between working in the field of arthroscopy for less than two, less than five, under ten or more than ten years. A second question was the number of knee arthroscopies performed per year. Of 377 responding members, 227 matched the inclusion criteria and received an invitation to fill out the 25-item electronic questionnaire (Table 1). The questionnaire was designed to collect data on selection criteria, clinical, radiological and arthroscopic findings as well as results after arthroscopic treatment in the osteoarthritic knee. For each question, there was only one possible answer, which could be marked using common check boxes. The questionnaire could only be returned after complete response to the survey. The respondents were asked to repeat a description of their personal status and field of expertise. Subsequently they had to evaluate the outcome of arthroscopy in osteoarthritis with regard to different indications and modalities. A 6-point scale was used for evaluation containing grades from “excellent” to “poor” and “no indication”. At the end, participants were asked to decide whether or not they felt comfortable with the current definition of osteoarthritis. For classification of osteoarthritis grades, the generally accepted radiological classification of Kellgren and Lawrence was applied [11]. The time frame for electronically completing and submitting the survey ranged from 7 December 2011 to 21 March 2012. Respondents were identified by their email address to exclude repetitive completions, but were processed anonymously for further data analysis. To reach a representative return rate of 80 %, four reminders had to be sent.
Table 1.
25-item ESSKA survey. One answer per item was possible. Respondents had to evaluate different indications and treatment modalities (2.1–2.21) on a scale from “excellent” to “good”
Statistical analysis was performed using SPSS (Version 19, SPSS Inc., Chicago, IL, USA). The data were compared using the Wilcoxon test for compound samples. A p value less than 0.05 (p < 0.05) was considered statistically significant.
Results
Of the 227 surgeons interviewed, 186 (81.9 %) completed the survey. Sixteen respondents initially declaring that they performed more than 100 knee arthroscopies per year had indicated less than 100 when returning the survey. After excluding those respondents from data analysis, 170 answers of 211 ESSKA members were left. The result was a representative return rate of 80.6 %. There were 157 (92.4 %) respondents who indicated that they specialised in orthopaedic surgery and eleven (6.5 %) who marked traumatology. Of the surgeons surveyed, 64.7 % perform over 200 knee arthroscopies per year, while 35.3 % perform between 100 and 200. The majority of respondents work in private practices (44.7 %), followed by university (22.9 %) and public (22.4 %) hospitals.
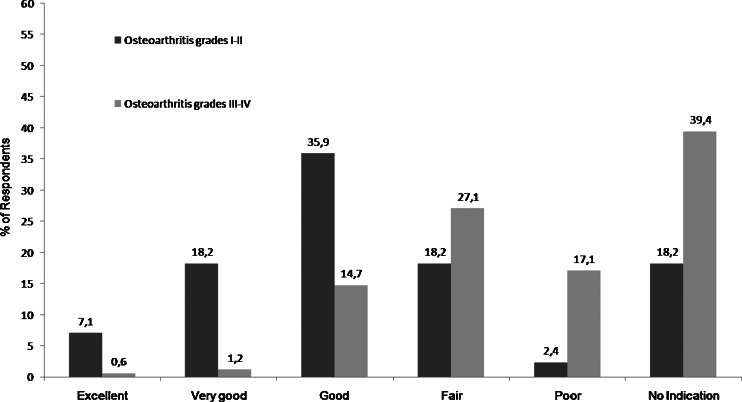
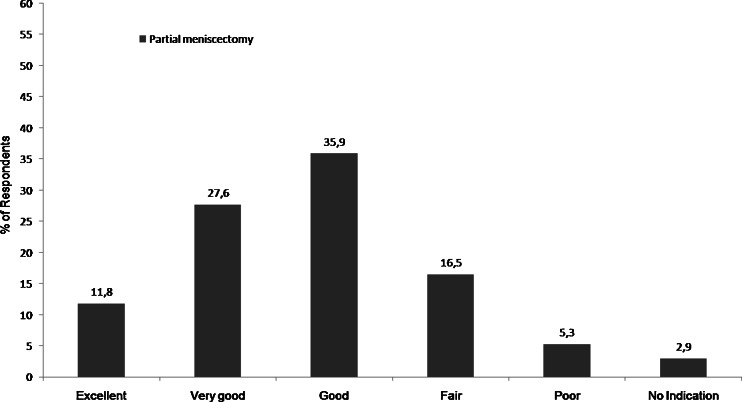
One of the central questions of this survey was to evaluate the differences in the outcome of arthroscopy in mild and severe osteoarthritis. Results show significantly (p < 0.001) better rates for grades 1 and 2 according to the Kellgren and Lawrence classification in comparison to grades 3 and 4 (Fig. 1). Of the surgeons surveyed, 39.4 % do not recommend arthroscopy in severe osteoarthritis compared to 18.2 % in mild forms. In grades 1 and 2, 7.1 % report excellent, 18.2 % very good and 35.9 % good results. In contrast, in higher grades of osteoarthritis 0.6 % obtained excellent, 1.2 % very good and 14.7 % good results.
Fig. 1.
Osteoarthritis grades 1 and 2 according to the radiological classification of Kellgren and Lawrence were evaluated significantly better than grades 3 and 4 (p < 0.001)
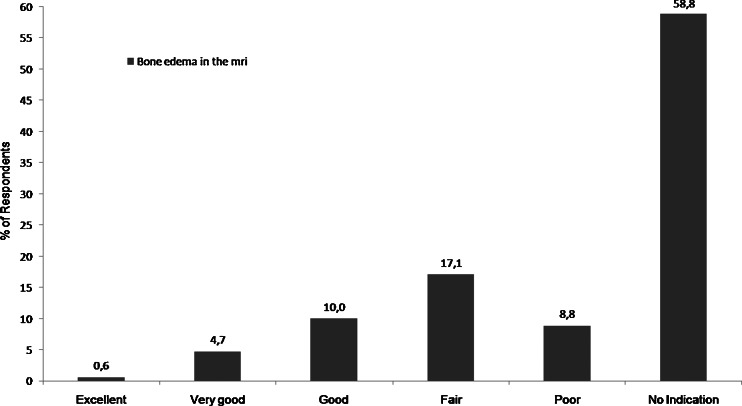
A finding of bone edema on magnetic resonance imaging (MRI) was connected with a poor outcome. It was evaluated worst of all indication modalities including 17.1 % fair and 8.8 % poor results. A total of 58.8 % replied that they saw no indication for arthroscopic intervention in these cases (Fig. 2).
Fig. 2.
Most respondents saw no indication for arthroscopy in knee osteoarthritis combined with bone edema diagnosed by MRI
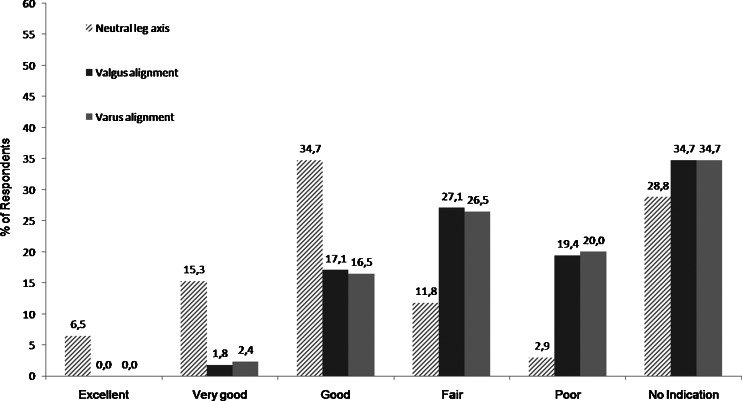
The outcome of patients with an axis deviation was described as significantly inferior in comparison to patients with a neutral leg axis (p < 0.001). Only a marginal difference was seen comparing valgus or varus malalignment. Of the interviewees, 34.7 % marked no indication in these cases compared to 28.8 % in neutral leg axis (Fig. 3).
Fig. 3.
Nearly one third of respondents generally saw no indication, whereas one third of respondents saw no indication in valgus or varus malalignment. Of those who were performing arthroscopy in osteoarthritis the best results were seen in patients with neutral leg axis (p < 0.001)
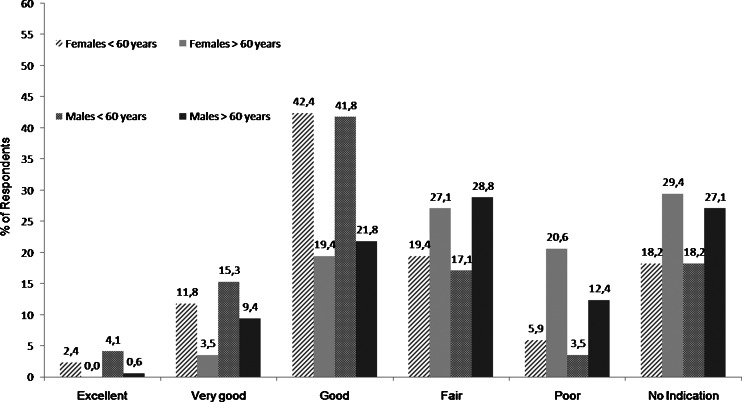
In women and men aged less than 60 years results seem to be significantly better compared to older patients (p < 0.001). Concerning men younger than 60, 3.5 % of the interviewees considered the outcome of an arthroscopic intervention as poor compared to 12.4 % in men over 60 years. Results in women generally seem to be less satisfying than in men. In women aged over 60 years, 29.4 % of respondents do not recommend performing arthroscopy, whereas only 18.2 % see no indication for women under 60 years of age (Fig. 4).
Fig. 4.
For patients less than 60 years results are significantly better (p < 0.001). Outcome in women generally seems to be less satisfying
The persistence of symptoms appears to be an important factor influencing success of the arthroscopic treatment. A presence of symptoms shorter than six months (p < 0.001) is favoured. Of the physicians questioned, 16.5 % experienced very good results when symptoms had been present less than six months in contrast to 5.3 % if symptoms prevailed longer.
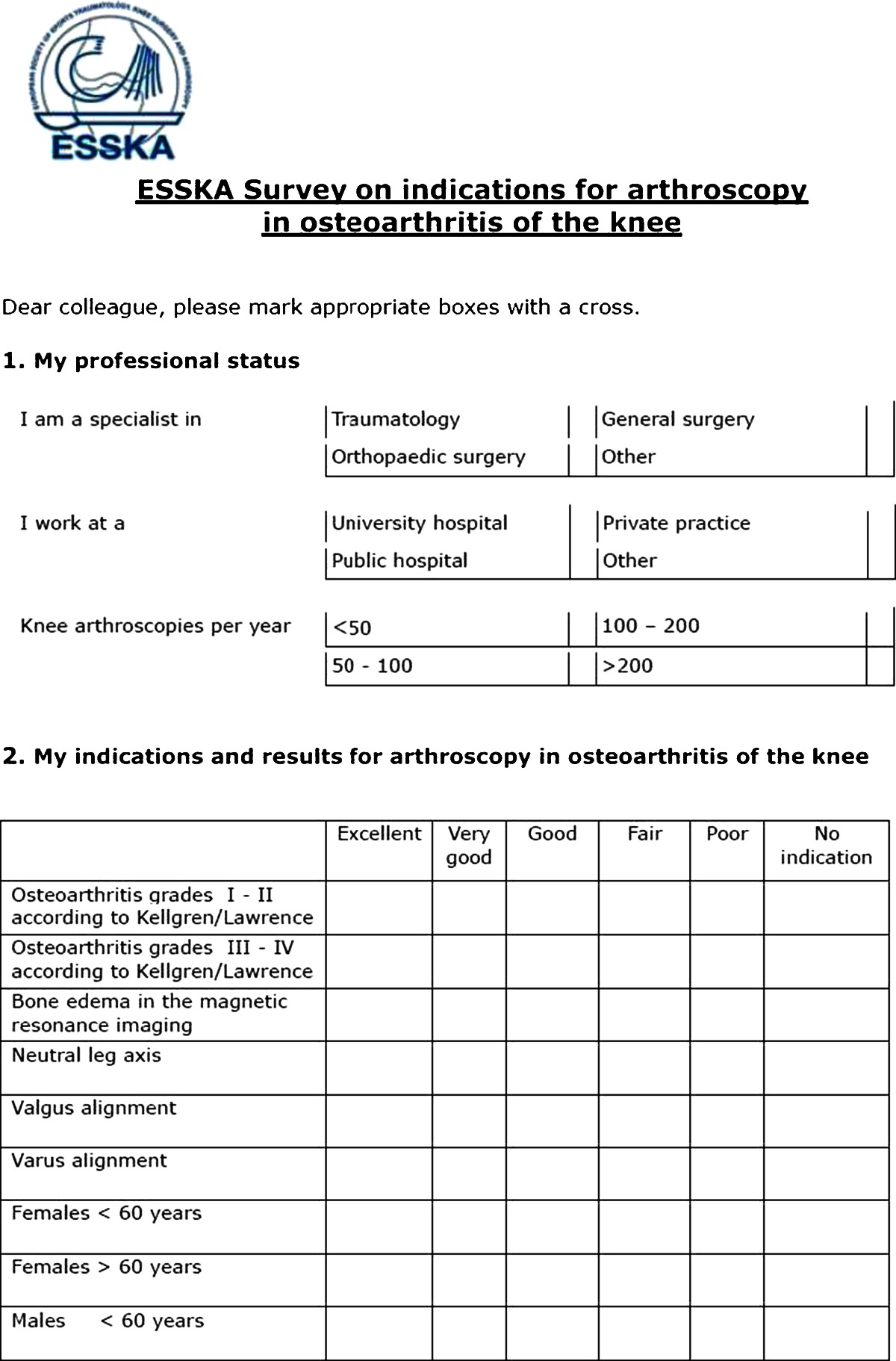
In evaluating partial meniscectomy consensus is shown amongst the respondents on indication in osteoarthritic knees; 11.8 % of the surgeons reported an excellent outcome. This item achieved the best assessment in the survey (Fig. 5).
Fig. 5.
Partial meniscectomy was seen as an indication with the best evaluated outcome. Only five respondents recommended no indication
Although the majority described results as fair (33.5 %), followed by good (30 %), debridement is an accepted procedure amongst the respondents. Only 11.2 % replied there was no indication in osteoarthritic knees. Arthroscopic joint lavage in knee osteoarthritis seems to be less successful. Of the interviewees, 30 % did not see an indication, while 17.1 % had experienced a poor outcome. Of the respondents, 33.5 % marked no indication for removal of osteophytes, whereas 25.3 % shared the opinion of a fair outcome. Nevertheless, a small group (7.1 %) appeared to be convinced of the procedure’s benefit while rating their results as very good.
Concerning the indication of arthroscopy in osteoarthritis after arthrofibrosis, the collected data show a limited benefit for the patient. One third of the respondents saw no indication for arthroscopy in these cases, 28.2 % reported a fair outcome and 21.2 % poor results. In contrast, arthroscopic intervention seems to be beneficial in the therapy of extension deficits due to intercondylar notch stenosis. In these cases 21.2 % of the interviewees marked a good indication for notchplasty, while 14.7 % reported very good results. Disagreement is predominant in the respondents’ opinion regarding lateral release in cases of osteoarthritis of the patellofemoral joint; 12.4 % of the surgeons indicated very good results, while 12.9 % estimated results to be poor, 20.6 % replied fair and 21.2 % good. Every third surgeon (31.2 %) would not perform a lateral release in these cases. In therapy of chondrocalcinosis, arthroscopy appears to be established; 31.2 % of the respondents reported a fair outcome, whereas a minority of 15.9 % saw no indication for arthroscopy (Table 2).
Table 2.
Evaluation of chondrocalcinosis, lateral release, notchplasty and arthrofibrosis. The majority of the respondents saw no indication for arthroscopic treatment in osteoarthritis after arthrofibrosis or for a lateral release in osteoarthritis of the patellofemoral joint. The outcome in chondrocalcinotic cases was rated as fair, while the results of a notchplasty in cases of extension deficits were evaluated better
| Answer options | Excellent | Very good | Good | Fair | Poor | No indication |
|---|---|---|---|---|---|---|
| Osteoarthritis after arthrofibrosis | 1.8 | 6.5 | 12.4 | 28.2 | 21.2 | 30.0 |
| Notchplasty in cases of stenosis and extension deficit | 5.3 | 14.7 | 21.2 | 24.1 | 12.9 | 21.8 |
| Lateral release in osteoarthritis of the patellofemoral joint | 1.8 | 12.4 | 21.2 | 20.6 | 12.9 | 31.9 |
| Chondrocalcinosis | 0.0 | 12.4 | 26.5 | 31.2 | 14.1 | 15.9 |
In contrast, the outcome of synovectomy in osteoarthritic knees seems to be more positive with 14.1 % very good and 29.4 % good answers. Finally, the majority of the surgeons interviewed confirmed their comfort with the current definition of osteoarthritis. However, 44.1 % respondents of the survey were not satisfied.
Discussion
The survey has revealed that almost two thirds of respondents see an indication for arthroscopy in osteoarthritis, under certain conditions. Osteoarthritis should not be very advanced. Bone edema on MRI should not exist. In cases of short duration symptoms better results are achieved, just as in people who are younger than 60 years. Even in joint lavage, where the usefulness was challenged by various level 1 studies [1, 3–5] and criticism prevails in the survey, 7.1 % see a very good up to an excellent outcome.
Almost 40 % of the experts surveyed do not recommend performing arthroscopy in grades 3 and 4 according to the Kellgren and Lawrence classification. The results of Aaron et al. [7] support this recommendation. In a prognostic level 2 study, they reported in 84 % of knees substantial pain relief post-operatively in grade 2, while in grade 4 the outcome was significantly worse. Several other studies demonstrated good results in low-grade osteoarthritis and described worse outcomes in advanced stages and in multicompartmental disease [8, 12, 13]. Moseley et al. used a grading system that rated each compartment and summarised the results to a score for the whole knee joint [1]. On this scale, low-grade osteoarthritis in all compartments and severe osteoarthritis in one compartment cannot be differentiated, which makes interpretation and comparison difficult. Kirkley et al. [4] found in a randomised, controlled trial in patients with moderate to severe osteoarthritis of the knee no additional benefit of arthroscopic surgery compared to physical and medical therapy. In our survey presence of a bone edema on MRI was the item which received the worst evaluated outcome, and it was mostly accepted among the informants that the results do not justify arthroscopic treatment (58.8 % no indication). Xu et al. [14] noted as the result of a review of recent papers about MRI of subchondral bone marrow lesions in association with osteoarthritis that subchondral bone marrow lesions are associated with the progression of articular cartilage loss and fluctuation of pain in knee osteoarthritis. This may be the cause of poor results in the arthroscopic therapies when bone edema is present.
Most of the surgeons interviewed described better outcome in patients without deviation of the leg axis. This is consistent with the findings of Aaron et al. [7] who reported significantly worse results in the presence of malalignment. In their study, treatment of knees with valgus deviation was more disappointing than with varus deviation. A difference of results between both types of malalignment could not be found in our survey. Harwin [15] divided 204 knees into three groups based on alignment and concluded that patients with less deviated axis do better than those with pronounced axis deviation. Ogilvie-Harris and Fitsialos had similar results [16], whereas Steadman et al. [17] reported success in cases of moderate to severe osteoarthritis and functional improvement in knees with significant angular deformity, but they defined failure as knees requiring arthroplasty.
The outcome of patients older than 60 was evaluated to be significantly worse in our survey, regarding both male and female patients. This observation was confirmed by Wai et al. [18], who found that the rate of early total knee arthroplasty following arthroscopic debridement rises with age. In their analysis, patients of 70 years of age or more were 4.7 times more likely to have total knee arthroplasty within one year after debridement compared to patients less than 60 years of age. Gender was not a determinant for the need for revision in that study, but Dervin et al. [10] recognised a tendency for female patients to suffer from a higher degree of pain. Further, they reported a trend towards greater improvement in pain after the intervention, which contradicts the prevalent opinion in this survey. When analysing the influence of gender, it should be remembered that the incidence of osteoarthritis among women seems to be higher [19].
The polled experienced better results in patients with a persistence of symptoms less than six months. That a short duration of symptoms improves the chances of a satisfying outcome is supported by current literature [20–22]. Fond et al. have shown that a persistence of symptoms for longer than five years is connected with significantly worse results [8].
Partial meniscectomy was evaluated by respondents as most recommendable; 75.3 % of informants described results as excellent, very good or good, while only 2.9 % recommended not performing it. It is the only indication for arthroscopy in symptomatic osteoarthritis of the knee that is given in the treatment recommendations of the AAOS [6], and different authors have demonstrated its value [23, 24]. Dervin et al. [10] found a significant connection between improvement after debridement to remove an unstable meniscus fragment at arthroscopy. The study by Moseley et al. [1] included partial meniscectomy even in the lavage group, as leaving an unstable meniscus tear untreated was considered unethical. The randomised controlled study by Kirkley et al. [4], which doubted the use of arthroscopy in osteoarthritis, excluded patients with large meniscus tears from their trial. However, Herrlin et al. [3] doubt the use of partial meniscectomy in degenerative medial meniscus tears. They showed that followed by physiotherapy it does not lead to greater improvement than physiotherapy alone. Katz et al. [25] reported that meniscectomy in the presence of cartilage damage in the medial compartment can reduce the functional status after surgery. Of the respondents in our survey, 44.2 % believed debridement of cartilage lesions is a reasonable option in osteoarthritis, whereas joint lavage was evaluated by 30 % as having “no indication”, and 17.1 % of surgeons believed its results were poor. In the literature success of debridement was disputed [1, 4, 5]; nevertheless, some authors see evidence that under certain conditions it provides satisfactory results [7, 9, 13]. Lavage as a sole intervention came under criticism and most authors assessed it sceptically or negatively [1, 4]. Removal of osteophytes was rated even worse than lavage in our survey, although it has been shown in the literature that resection of osteophytes, which contribute to locking of the knee in extension, can provide improvement in function and decrease pain [8, 17, 26]. In osteoarthritis after arthrofibrosis, 30 % did not see an indication for arthroscopy; the results were evaluated as poor or fair by 49.4 % of respondents. Arthroscopic treatment of arthrofibrosis is a very difficult intervention due to the prevalence of thickened capsule, loss of joint space, adhesions and scar tissue [27]. Mayr et al. [28] showed a significant relation between persistence of an extension deficit and development of osteoarthritis. In limited range of motion, improvement of range of motion might help to prevent this effect. The majority of surgeons interviewed for this survey were convinced that in cases of extension deficit a notchplasty can provide improvement. This is consistent with the findings of León et al. [29]. They reported 90 % good to excellent pain relief, 81 % significant decrease of flexion contracture and 74 % excellent relief of subjective instability in a case series of 69 knees with degenerative arthritis. A survey by Fithian et al. [30] reflects the disagreement concerning lateral release in osteoarthritis of the patellofemoral joint that has been revealed in our survey. Among experienced knee surgeons, with a special interest in diseases of the patellofemoral joint, agreement was poor concerning which clinical evidence provides the most appropriate indication for this procedure. Fithian et al. concluded that isolated lateral release is believed to be indicated only under rare circumstances.
In a retrospective study by Ogilvie-Harris and Fitsialos [16], 441 arthroscopic procedures in degenerative and arthritic knees, including 51 patients with chondrocalcinosis, showed relatively poor results. In our survey, 51.2 % of respondents did not see an indication for arthroscopy in chondrocalcinosis or observed fair and poor results. Our survey results were not much better for synovectomy, although Kuzmanova et al. reported good therapeutic results maintained for five years after this procedure [31].
The majority of surgeons interviewed confirmed they were comfortable with the current definition of osteoarthritis, although 44.1 % replied they were not. These findings express a certain discontent and could be a sign of the wish for a more precise definition and clearer methods for assessment of the disease.
The strengths of the study are to be found in the representative return rate, which was above 80 %, and in the fact that every respondent answered every question of the survey. A weakness of the study might be the complex structure of the survey, by including grading options with the additional possibility to select “no indication”. Thus, evaluation of outcome and the question about indication are combined, which might have led to conflicting decisions between conveying poor outcome and indicating that one does not see an indication.
Conclusion
It has been shown that arthroscopy is not universally helpful in the therapy of osteoarthritis [1, 3–5]; nonetheless, the results show that experienced surgeons in Europe believe it is appropriate and that in certain cases patients can profit from arthroscopic treatment. Selecting patients who are likely to benefit from this therapy is the major task for surgeons. The findings of this survey show that specialists believe there is improvement in cases of low-grade osteoarthritis, neutral leg axis, persistence of symptoms less than six months and in patients with an age of less than 60 years. Partial meniscectomy and notchplasty in cases of extension deficit were considered as successful treatment options. Debridement was an accepted indication, with an outcome mainly rated as fair. In joint lavage, arthroscopic treatment of arthrofibrosis and resection of osteophytes a majority saw no indication for arthroscopy. The outcome appears to be unsatisfactory if a bone edema can be found on MRI prior to arthroscopy.
References
- 1.Moseley JB, O’Malley K, Petersen NJ, Menke TJ, Brody BA, Kuykendall DH, Hollingsworth JC, Ashton CM, Wray NP. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347(2):81–88. doi: 10.1056/NEJMoa013259. [DOI] [PubMed] [Google Scholar]
- 2.Potts A, Harrast JJ, Harner CD, Miniaci A, Jones MH. Practice patterns for arthroscopy of osteoarthritis of the knee in the United States. Am J Sports Med. 2012;40(6):1247–1251. doi: 10.1177/0363546512443946. [DOI] [PubMed] [Google Scholar]
- 3.Herrlin S, Hållander M, Wange P, Weidenhielm L, Werner S. Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2007;15(4):393–401. doi: 10.1007/s00167-006-0243-2. [DOI] [PubMed] [Google Scholar]
- 4.Kirkley A, Birmingham TB, Litchfield RB, Giffin JR, Willits KR, Wong CJ, Feagan BG, Donner A, Griffin SH, D’Ascanio LM, Pope JE, Fowler PJ. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359(11):1097–1107. doi: 10.1056/NEJMoa0708333. [DOI] [PubMed] [Google Scholar]
- 5.Risberg MA. Arthroscopic surgery provides no additional benefit over physiotherapy and medication for the treatment of knee osteoarthritis. Aust J Physiother. 2009;55(2):137. doi: 10.1016/S0004-9514(09)70045-5. [DOI] [PubMed] [Google Scholar]
- 6.Richmond J, Hunter D, Irrgang J, Jones MH, Levy B, Marx R, Snyder-Mackler L, Watters WC, 3rd, Haralson RH, 3rd, Turkelson CM, Wies JL, Boyer KM, Anderson S, St Andre J, Sluka P, McGowan R, et al. Treatment of osteoarthritis of the knee (nonarthroplasty) J Am Acad Orthop Surg. 2009;17(9):591–600. doi: 10.5435/00124635-200909000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aaron RK, Skolnick AH, Reinert SE, Ciombor DM. Arthroscopic débridement for osteoarthritis of the knee. J Bone Joint Surg Am. 2006;88(5):936–943. doi: 10.2106/JBJS.D.02671. [DOI] [PubMed] [Google Scholar]
- 8.Fond J, Rodin D, Ahmad S, Nirschl RP. Arthroscopic debridement for the treatment of osteoarthritis of the knee: 2- and 5-year results. Arthroscopy. 2002;18(8):829–834. doi: 10.1053/jars.2002.36225. [DOI] [PubMed] [Google Scholar]
- 9.Spahn G, Hofmann GO, Klinger HM. The effects of arthroscopic joint debridement in the knee osteoarthritis: results of a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2012 doi: 10.1007/s00167-012-2169-1. [DOI] [PubMed] [Google Scholar]
- 10.Dervin GF, Stiell IG, Rody K, Grabowski J. Effect of arthroscopic débridement for osteoarthritis of the knee on health-related quality of life. J Bone Joint Surg Am. 2003;85-A(1):10–19. doi: 10.2106/00004623-200301000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Livesley PJ, Doherty M, Needoff M, Moulton A. Arthroscopic lavage of osteoarthritic knees. J Bone Joint Surg Br. 1991;73(6):922–926. doi: 10.1302/0301-620X.73B6.1720118. [DOI] [PubMed] [Google Scholar]
- 13.Jackson RW, Dieterichs C. The results of arthroscopic lavage and debridement of osteoarthritic knees based on the severity of degeneration: a 4- to 6-year symptomatic follow-up. Arthroscopy. 2003;19(1):13–20. doi: 10.1053/jars.2003.50022. [DOI] [PubMed] [Google Scholar]
- 14.Xu L, Hayashi D, Roemer FW, Felson DT, Guermazi A (2012) Magnetic resonance imaging of subchondral bone marrow lesions in association with osteoarthritis. Semin Arthritis Rheum 42(2):105–118. doi:10.1016/j.semarthrit.2012.03.009. Epub 2012 Apr 26. doi:10.1016/j.arthro.2004.03.002 [DOI] [PMC free article] [PubMed]
- 15.Harwin SF. Arthroscopic debridement for osteoarthritis of the knee: predictors of patient satisfaction. Arthroscopy. 1999;15(2):142–146. doi: 10.1053/ar.1999.v15.015014. [DOI] [PubMed] [Google Scholar]
- 16.Ogilvie-Harris DJ, Fitsialos DP. Arthroscopic management of the degenerative knee. Arthroscopy. 1991;7(2):151–157. doi: 10.1016/0749-8063(91)90101-3. [DOI] [PubMed] [Google Scholar]
- 17.Steadman JR, Ramappa AJ, Maxwell RB, Briggs KK. An arthroscopic treatment regimen for osteoarthritis of the knee. Arthroscopy. 2007;23(9):948–955. doi: 10.1016/j.arthro.2007.03.097. [DOI] [PubMed] [Google Scholar]
- 18.Wai EK, Kreder HJ, Williams JI. Arthroscopic débridement of the knee for osteoarthritis in patients fifty years of age or older: utilization and outcomes in the Province of Ontario. J Bone Joint Surg Am. 2002;84-A(1):17–22. doi: 10.2106/00004623-200201000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Oliveria SA, Felson DT, Reed JI, Cirillo PA, Walker AM. Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis Rheum. 1995;38(8):1134–1141. doi: 10.1002/art.1780380817. [DOI] [PubMed] [Google Scholar]
- 20.Day B. The indications for arthroscopic debridement for osteoarthritis of the knee. Orthop Clin North Am. 2005;36(4):413–417. doi: 10.1016/j.ocl.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Baumgaertner MR, Cannon WD, Jr, Vittori JM, Schmidt ES, Maurer RC. Arthroscopic debridement of the arthritic knee. Clin Orthop Relat Res. 1990;253:197–202. [PubMed] [Google Scholar]
- 22.Merchan EC, Galindo E. Arthroscope-guided surgery versus nonoperative treatment for limited degenerative osteoarthritis of the femorotibial joint in patients over 50 years of age: a prospective comparative study. Arthroscopy. 1993;9(6):663–667. doi: 10.1016/S0749-8063(05)80503-1. [DOI] [PubMed] [Google Scholar]
- 23.Pearse EO, Craig DM. Partial meniscectomy in the presence of severe osteoarthritis does not hasten the symptomatic progression of osteoarthritis. Arthroscopy. 2003;19(9):963–968. doi: 10.1016/j.arthro.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 24.Rand JA. Role of arthroscopy in osteoarthritis of the knee. Arthroscopy. 1991;7(4):358–363. doi: 10.1016/0749-8063(91)90004-H. [DOI] [PubMed] [Google Scholar]
- 25.Katz JN, Meredith DS, Lang P, Creel AH, Yoshioka H, Neumann G, Fossel AH, de Pablo P, Losina E. Associations among preoperative MRI features and functional status following arthroscopic partial meniscectomy. Osteoarthritis Cartilage. 2006;14(5):418–422. doi: 10.1016/j.joca.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 26.Puddu G, Cipolla M, Cerullo G, Scala A. Arthroscopic treatment of the flexed arthritic knee in active middle-aged patients. Knee Surg Sports Traumatol Arthrosc. 1994;2(2):73–75. doi: 10.1007/BF01476475. [DOI] [PubMed] [Google Scholar]
- 27.Millett PJ, Steadman JR. The role of capsular distention in the arthroscopic management of arthrofibrosis of the knee: a technical consideration. Arthroscopy. 2001;17(7):E31. doi: 10.1053/jars.2001.25240. [DOI] [PubMed] [Google Scholar]
- 28.Mayr HO, Weig TG, Plitz W. Arthrofibrosis following ACL reconstruction—reasons and outcome. Arch Orthop Trauma Surg. 2004;124(8):518–522. doi: 10.1007/s00402-004-0718-x. [DOI] [PubMed] [Google Scholar]
- 29.León HO, Blanco CE, Guthrie TB, Martínez OJ. Intercondylar notch stenosis in degenerative arthritis of the knee. Arthroscopy. 2005;21(3):294–302. doi: 10.1016/j.arthro.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 30.Fithian DC, Paxton EW, Post WR, Panni AS, et al. Lateral retinacular release: a survey of the International Patellofemoral Study Group. Arthroscopy. 2004;20(5):463–468. doi: 10.1016/j.arthro.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 31.Kuzmanova SI. Treatment of knee osteoarthritis by arthroscopic synovectomy and debridement of cartilage lesions—late results. Folia Med (Plovdiv) 2003;45(3):66–72. [PubMed] [Google Scholar]