Abstract
Purpose
Along with the increase in primary total knee arthroplasty, there has been an increase in the number of revisions. The aim of this study was to propose a selection algorithm for the knee revision constraint according to the state of ligaments and to the bone defects Anderson Orthopaedic Research Institute Classification [AORI] classification. The hypothesis was that this algorithm would facilitate the appropriate choice of prosthesis constraint, thus providing stable components and a good long-term survivorship of the knee revisions.
Methods
Sixty consecutive revision knee arthroplasties in 57 patients were prospectively evaluated. Prostheses implanted at revision included postero-stabilised, condylar constrained and rotating hinged, relative to the state of the ligaments and of the bone loss around the knee. The median follow-up was nine years (range, 4–12).
Results
The median IKS knee and function scores and HSS score were 41 (15–62), 21.5 (12–43) and 34 (23–65) points, respectively, before the operation, and 81 (48–97), 79 (56–92) and 83.5 (62–98) points (p < 0.001) at the latest follow-up evaluation. The median ROM increased from 74° (29–110°) preoperatively to 121° (98–132°) (p < 0.01) at the final follow-up. Re-revision was necessary in five (8.3 %) patients.
Conclusions
A selection algorithm for the revision implant constraint based on the state of ligaments and the bone loss AORI classification could provide stable knee reconstructions and long-term success of knee revisions.
Introduction
The increasing number of total knee arthroplasties implanted each year worldwide has led to a concomitant increase in revision surgeries. More than 350,000 primary knee arthroplasties were performed in the United States in 2002, and about 29,000 knee revisions [1], with 46,000 during 2005 alone [2]. It has been estimated that by 2030, every year, 500,000 Americans aged 65 or over will undergo total knee arthroplasty (TKA) [3].
Revision TKAs are certainly more complex than primary procedures, with poorer outcomes and a higher rate of complications [4]. The poorer results of revisions have been attributed to several factors including the deficiency of host bone stock both in quantity and quality, extensor mechanism problems, ligamentous instability [5] and a greater incidence of periprosthetic infection [6]. Numerous studies have reported rates of reoperation after revision TKA of eight to 19 % [6–8].
Apart from infections, the principal causes of revision TKA failure are wear, aseptic loosening [9] and instability due to the inappropriate choice of revision implant constraint [6, 10]. In fact, one of the greatest challenges during revision TKA is the management of the ligamentous instability affecting both the function and final survival of the knee joint reconstruction [5, 11].
Constraint choice depends on the state of collateral ligaments and other peripheral stabilisers of the knee, and on the severity of bone loss [12–14]. Primary postero-stabilised (PS) designs may be used if the ligaments are intact and bone defects are minimal [12], whereas hinged prostheses are necessary in cases of ligament absence/disruption with moderate or severe bone loss [5, 15]. Condylar constrained knee (CCK) prostheses are semi-constrained nonhinged implants, which represent an excellent alternative to the hinged prostheses. CCK systems have been introduced more recently, being more suitable in cases of intermediate severity with insufficiency (but not absence) of the ligaments and moderate bone loss [16–18].
The aim of this study was to present a modern algorithm for selection of the implant constraint according to the state of peripheral ligaments and to the bone defects AORI classification [19]. The hypothesis was that this algorithm would facilitate the constraint choice of the revision prosthesis thus providing stable components and a long-term success of knee revisions.
Materials and methods
From 2001 to 2009, 60 consecutive revision TKAs in 57 patients were carried out at our institution. The indications for the revision procedure included second-stage revision for the treatment of deep infection (22 knees), aseptic loosening (19), severe osteolysis (7), pain (4), severe knee instability (3), extensor mechanism problems (3) and wear (2). The median time from the primary knee replacement to revision was 29 months (range, four to 75). The study group included 36 women and 21 men. At the time of revision surgery, the median patient age was 72 years (range, 61–84), and the median body mass index (BMI) was 26.4 kg/m2 (range, 23.2–32.9).
Removed knee arthroplasties were: postero-stabilised (34 implants), cruciate-retaining (11), semiconstrained (6), medial unicompartmental (5) and hinged (4). The state of the ligaments found during the revision was classified as intact, insufficient and absent; while bone loss was categorised according to the AORI bone defect classification system [19].
All data were prospectively collected. Clinical evaluation was performed preoperatively and at post-revision intervals of three months, six months, one year, and yearly thereafter. Patients were assessed using the International Knee Society (IKS) knee and function scores, and the Hospital for Special Surgery (HSS) knee score; median range of motion (ROM) was reported.
Radiographic assessment, including weight-bearing anteroposterior, lateral and Merchant views, was completed for all 57 patients to evaluate the presence of radiolucencies and osteolysis. Presence and location of radiolucent lines were assessed according to a modification of the Knee Society TKA radiographic evaluation system for long-stemmed revision prostheses [20]. An osteolytic lesion was recorded according to size as none, minimal (0.5 × 0.5 cm), or greater than two centimetres. The median follow-up of the revisions was nine years (range, four to 12).
Statistical analysis
Patient demographics were described using medians and ranges. Improvements relative to the median IKS knee and function scores, HSS knee score, and median ROM were analysed using a Student t test. The degree of statistical significance was defined as p < 0.05.
Results
Constraint choice for the revision prosthesis depended on the state of the ligaments and on the severity of bone loss according to AORI classification. A primary PS implant (Nexgen LPS, Zimmer, Warsaw, IN, USA) was sufficient in seven knees that presented with intact ligaments and type 1 bone loss. A semiconstrained CCK implant (Nexgen LCCK, Zimmer, Warsaw, IN, USA) was used in 35 knees with ligament insufficiency and type 2 bone defects. A rotating hinged prosthesis (Nexgen RHK, Zimmer, Warsaw, IN, USA) was necessary in 18 knees characterised by ligament absence/disruption and type 2 or 3 bone loss. All the prosthetic components were cemented in their condylar and metaphyseal portion.
Type 1 defects were managed with cement and morcellised autografts. Type 2 and 3 defects were treated with metal augmentations, tantalum cones, and modular cementless stems. In particular, tantalum cones were used only for management of type 3 defects. No allograft was used.
The median IKS knee and function scores and HSS score were 41 (range, 15–62), 21.5 (12–43) and 34 (23–65) points, respectively, before the operation, and 81 (48–97), 79 (56–92) and 83.5 (62–98) points (p < 0.001) at the latest follow-up evaluation. The median ROM increased from 74° (range, 29–110°) preoperatively to 121° (98–132°) (p < 0.01) at the final follow-up.
No significant differences were found between the three groups of prostheses (PS, CCK and RHK) in terms of IKS and HSS scores. PS prostheses only presented significantly higher ROM values compared to CCK and RHK ones (127° vs. 111.5° and 107.5°, respectively) (p < 0.01).
Re-revision was necessary in five (8.3 %) patients. One patient with a CCK prosthesis developed knee instability, probably caused by an underestimated complete lesion of the medial stabilisers, and was revised using a one-stage reimplantation with a RHK. Two patients, both with a CCK, developed recurrence of infection. One of these two patients required a knee arthrodesis because of a multidrug-resistant Pseudomonas aeruginosa infection. The other patient with methicillin-resistant Staphylococcus aureus re-infection was revised through a two-stage reimplantation with a RHK. One patient with a RHK was revised for persistent pain and an arthrodesis was necessary. Finally, one patient with an RHK was re-revised with a tumour prosthesis for wear and aseptic loosening.
Radiographic results
In four (6.7 %) cases, 12 months after surgery, anteroposterior radiographs revealed radiolucent lines (incomplete and less than one millimetre) around the tibial component, at the bone–cement interface. These radiolucent lines were not progressive at further follow-ups, nor associated with tibial subsidence. In three cases, the radiolucency was observed next to the medial tibial block of a CCK, while in one case the radiolucency was observed beneath the tibial platform of an RHK. Three (5 %) femora had minimal osteolysis without clinical or scintigraphic evidence of aseptic loosening.
All metal augmentations used (apart from three medial tibial blocks as previously mentioned) and all tantalum cones appeared well fixed radiographically at the final follow-up. In particular, no radiolucencies were observed between the cones and adjacent bone at the final follow-up, and this finding was considered to be evidence of osseointegration.
Discussion
The most important finding of our study was that 60 knee revisions were satisfactorily managed through three implants with different constraint degrees, relative to the state of peripheral ligaments and to the bone defects AORI classification: primary PS, semiconstrained CCK and rotating hinged (RHK) prostheses. Only two (out of five) failures of this series were due to mechanical factors; instability in one patient, and aseptic loosening in another patient. The median follow-up was nine years, therefore supporting the hypothesis that this protocol should provide stable and durable revision TKAs.
At the latest follow-up, IKS and HSS scores and ROM were significantly improved. No significant differences were found between the three different groups (PS, CCK and RHK) in terms of IKS and HSS scores, whereas PS designs only presented significantly higher ROM values, thus supporting the report of Fuchs et al. [21] who found a statistically significant difference in ROM between hinged and nonhinged designs (96.5° vs. 107.5°) but not in HSS, KSS, VAS, Tegner Activity Score, or Patella Score.
Constraint choice in revision TKA depends on the state of ligaments and on the severity of bone loss around the knee [12–14]. A simple algorithm of selection of the revision implant constraint is proposed (Table 1). A primary PS system can be used if the ligaments are intact and the bone stock is preserved (type 1 defects according to AORI classification). In these circumstances, it is possible to perform standard tibial bone resections, possibly with a thicker polyethylene insert (Fig. 1), or resections increased by up to five millimetres. In the latter case, the use of a tibial metal block may be indicated to avoid excessive tibial resection (Fig. 2). CCK are semiconstrained implants, which represent an excellent alternative to the hinged prostheses in cases of intermediate severity. CCK prostheses are characterised by a large and long tibial post which engages in the large, deep intercondylar cam of the femoral component, thus ensuring medio-lateral and rotational stability (Fig. 3). CCK systems can be used in case of insufficiency (but not absence) of the collateral ligaments, and moderate (type 2) bone loss. Hinged (total constraint) prostheses have been widely used in the past in revision TKA before the introduction of CCK implants in clinical practice. Modern hinged implants can provide a fixed or mobile insert and are generally used in the presence of complete disruption/absence of the ligaments with moderate (type 2) or severe (type 3) bone loss (Fig. 4).
Table 1.
Algorithm of choice of the knee revision constraint
| Implant | Indication | Notes |
|---|---|---|
| Primary PS | Intact peripheral ligaments | Consider the possibility to use a thicker polyethylene insert, or metal augments with or without short stems |
| Type 1 AORI bone defects | ||
| Semiconstrained CCK | Ligaments insufficiency | Large and long tibial post which engages in the large and deep intercondylar femoral cam, thus ensuring greater stability than PS implants |
| Type 2 AORI bone defects | ||
| Hinged | Ligaments disruption/absence | Total constraint, fixed or mobile insert |
| Type 2–3 AORI bone defects | ||
| Tumoral prostheses | Ligaments disruption/absence | Modular, custom-made implants |
| Massive not-reconstructable bone loss | ||
| Loss of periprosthetic soft tissues |
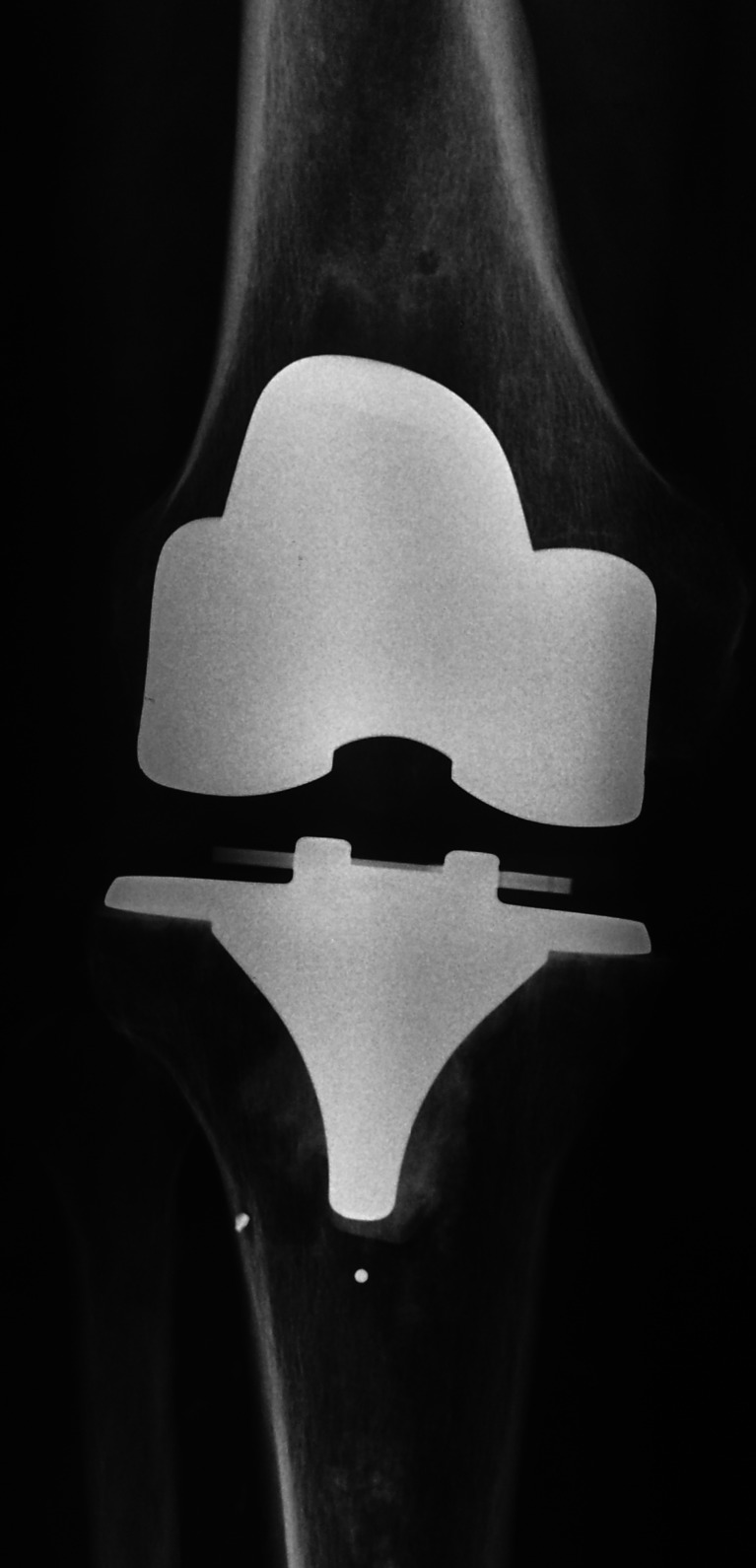
Fig. 1.
A revision total knee arthroplasty (TKA) performed for an allergy to the cobalt caused by the previous implant. A PS design was sufficient for the revision, but a thicker polyethylene insert was necessary for correct ligament balancing
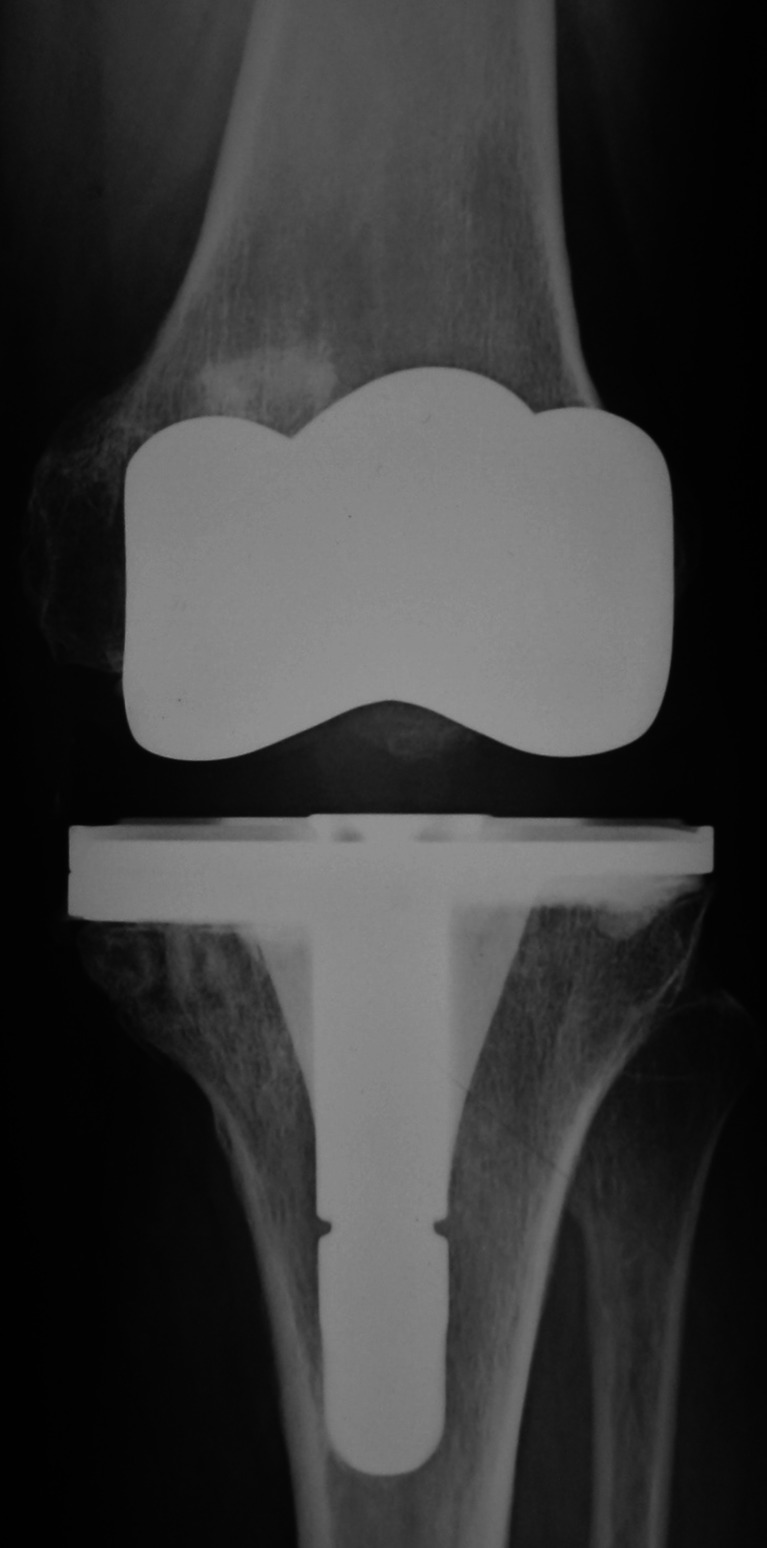
Fig. 2.
The use of tibial metal half-block (with or without a short tibial stem) may be indicated to avoid an excessive tibial resection, as during the revision of a unicompartmental knee arthroplasty
Fig. 3.

Due to their large and long tibial post which engages in the large and deep intercondylar femoral cam, CCK implants ensure medio-lateral and rotational stability (more than PS primary implants), thus representing a viable alternative to the hinged prostheses in knees that are not too compromised
Fig. 4.

A ligament disruption causing severe total knee arthroplasty (TKA) instability (a) was managed with an RHK prosthesis (b), a modern total constraint implant with a mobile bearing
To our knowledge, this is the first study to provide precise indications for the use of the three different constraint knee prostheses on the basis of the state of peripheral ligaments and the severity of bone loss according to AORI classification, with a long follow-up.
Hwang et al. [5] reviewed the outcomes of 36 revision TKAs performed with a cemented PS, CCK and RHK prosthesis in eight, 25 and 13 cases, respectively. The mean follow-up was 30 months. Good or excellent outcomes were obtained in 82 % of knees. In general, a cemented PS prosthesis was used if both collateral ligaments were felt to be competent, while cemented CCK or RHK prostheses were used if one or both collateral ligaments were incompetent. RHK was used in cases of extensor mechanism failure. However, the authors did not clearly indicate the precise indications for the use of a CCK instead of a RHK. They only asserted that RHK was used for extensor mechanism failure, which is not at all a criterion for the constraint choice [22]. Hossain et al. [23] retrospectively reviewed 349 revision TKAs in 343 patients. Three implant types were used: PS, CCK and RHK. The minimum follow-up was 12 months. The PS implant was used in cases of intact collateral ligaments, providing valgus-varus stability, and minimal bone loss. In cases of partially intact or functioning ligaments, cases with valgus-varus deformities of greater than 15° or with flexion-extension gap mismatches that may predispose to cam dissociation of a standard PS design, a CCK was considered. In these cases larger metaphyseal bone defects were encountered. A RHK prosthesis was used in cases with complete absence of ligaments, in cases of severe valgus-varus deformity and flexion contracture, which would necessitate the complete release of the collateral ligaments, and in cases of severe bone defects. Overall ten-year survivorship was 90.6 %. However, bone defects AORI classification was not used by the authors, thus failing to provide a very reproducible study. Fuchs et al. [21] reported good outcomes of 26 revision TKAs performed with hinged or semiconstrained implants. The indication for a hinged implant was based on whether or not the medial collateral ligament was completely absent. The ten patients with an infected TKA met these criteria and received a hinged implant. All 16 non-infected knees received a semiconstrained implant. Thus, no indication was given relative to the use of CCK implants, nor information about the influence of bone loss on the constraint design.
Although most reports of revision TKA include several types of prostheses, many studies have focused on a single prosthetic design [5]. Jones [24] reported excellent midterm results with no mechanical failures in 65 patients receiving a RHK prosthesis. Jones stressed that the primary indications for a RHK implant include medial and/or lateral collateral loss, massive bone loss, and metaphysis and cortical shell, which includes collateral origins or insertion, as well as a severe gap imbalance requiring a link system for stability. Utting and Newman [25] reported on 30 revision TKAs performed with hinged implants (21 rotating, nine fixed). No prostheses failed from an aseptic cause and most of the knees of this challenging group provided both stability and flexion. The authors concluded that hinged prostheses could be used to salvage of limb threatening situations in elderly patients at risk of arthrodesis or amputation. Gudnason et al. [10], more recently, reported similar results. Kim et al. [11] reported a ten-year 96 % components survivorship on 114 revision TKAs using a CCK prosthesis. The indication to use a CCK was deficient soft-tissue constraints around the knee. No mention was made about the influence of bone loss on the use of a CCK prosthesis. Moreover, most of the recent studies on CCK results have been performed in (difficult) primary knee replacements [16–18], whereas bone loss is rarely encountered.
The main limitation of this study is that a non-randomised case series is presented, although the final outcomes of the PS, CCK and RHK groups were individually analysed. Moreover, patients and respective outcomes were not matched based on their age, BMI or cause of revision. The paper was primarily focused on overall results of the knee revisions and on the possible validity of a selection algorithm for constraint choice rather than on assessment of the different factors potentially influencing the revision. However, predisposing factors which are relevant for the clinical outcome after revision TKA have been recently reported [26, 27].
The clinical relevance of our study was to show how a simple but effective algorithm could favour the correct selection of the revision implant constraint, thus providing stable knee reconstructions and long-term success of the revision TKAs.
Conclusions
Management of the ligamentous instability represents one of the greatest challenges during revision TKA. An algorithm for choice of the revision implant constraint is presented, based on the state of the peripheral ligaments and on the bone defects AORI classification. This algorithm is proven to help the knee surgeon in selecting the appropriate constraint degree of the knee revision implant.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Mahomed NN, Barrett J, Katz JN, Baron JA, Wright J, Losina E. Epidemiology of total knee replacement in the United States medicare population. J Bone Joint Surg Am. 2005;87:1222–1228. doi: 10.2106/JBJS.D.02546. [DOI] [PubMed] [Google Scholar]
- 2.Johnson AJ, Sayeed SA, Naziri Q, Khanuja HS, Mont MA. Minimizing dynamic knee spacer complications in infected revision arthroplasty. Clin Orthop Relat Res. 2012;470:220–227. doi: 10.1007/s11999-011-2095-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whittaker JP, Dharmarajan R, Toms AD. The management of bone loss in revision total knee replacement. J Bone Joint Surg Br. 2008;90:981–987. doi: 10.1302/0301-620X.90B8.19948. [DOI] [PubMed] [Google Scholar]
- 4.Freeman MG, Fehring TK, Odum SM, Fehring K, Griffin WL, Mason JB. Functional advantage of articulating versus static spacers in 2-stage revision for total knee arthroplasty infection. J Arthroplasty. 2007;22:1116–1121. doi: 10.1016/j.arth.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 5.Hwang SC, Kong JY, Nam DC, Kim DH, Park HB, Jeong ST, Cho SH. Revision total knee arthroplasty with a cemented posterior stabilized, condylar constrained or fully constrained prosthesis: a minimum 2-year follow-up analysis. Clin Orthop Surg. 2010;2:112–120. doi: 10.4055/cios.2010.2.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mortazavi SM, Molligan J, Austin MS, Purtill JJ, Hozack WJ, Parvizi J. Failure following revision total knee arthroplasty: infection is the major cause. Int Orthop. 2011;35:1157–1164. doi: 10.1007/s00264-010-1134-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hanna SA, Aston WJ, de Roeck NJ, Gough-Palmer A, Powles DP. Cementless revision TKA with bone grafting of osseous defects restores bone stock with a low revision rate at 4 to 10 years. Clin Orthop Relat Res. 2011;469:3164–3171. doi: 10.1007/s11999-011-1938-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peters CL, Erickson JA, Gililland JM. Clinical and radiographic results of 184 consecutive revision total knee arthroplasties placed with modular cementless stems. J Arthroplasty. 2009;24(6 Suppl):48–53. doi: 10.1016/j.arth.2009.04.033. [DOI] [PubMed] [Google Scholar]
- 9.Sternheim A, Lochab J, Drexler M, Kuzyk P, Safir O, Gross A, Backstein D. The benefit of revision knee arthroplasty for component malrotation after primary total knee replacement. Int Orthop. 2012;36:2473–2478. doi: 10.1007/s00264-012-1675-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gudnason A, Milbrink J, Hailer NP. Implant survival and outcome after rotating-hinge total knee revision arthroplasty: a minimum 6-year follow-up. Arch Orthop Trauma Surg. 2011;131:1601–1607. doi: 10.1007/s00402-011-1330-5. [DOI] [PubMed] [Google Scholar]
- 11.Kim YH, Kim JS. Revision total knee arthroplasty with use of a constrained condylar knee prosthesis. J Bone Joint Surg Am. 2009;91:1440–1447. doi: 10.2106/JBJS.H.00425. [DOI] [PubMed] [Google Scholar]
- 12.Meijer MF, Reininga IH, Boerboom AL, Stevens M, Bulstra SK. Poorer survival after a primary implant during revision total knee arthroplasty. Int Orthop. 2013;37:415–419. doi: 10.1007/s00264-012-1739-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nett M, Long WJ, Scuderi GR. Principles of revision total knee arthroplasty. Tech Knee Surg. 2009;8:144–153. doi: 10.1097/BTK.0b013e3181b57fbe. [DOI] [Google Scholar]
- 14.Radnay CS, Scuderi GR. Management of bone loss. Augments, cones, offset stems. Clin Orthop Relat Res. 2006;446:83–92. doi: 10.1097/01.blo.0000214437.57151.41. [DOI] [PubMed] [Google Scholar]
- 15.Yang JH, Yoon JR, Oh CH, Kim TS. Primary total knee arthroplasty using rotating-hinge prosthesis in severely affected knees. Knee Surg Sports Traumatol Arthrosc. 2012;20:517–523. doi: 10.1007/s00167-011-1590-1. [DOI] [PubMed] [Google Scholar]
- 16.Anderson JA, Baldini A, MacDonald JH, Tomek I, Pellicci PM, Sculco TP. Constrained condylar knee without stem extensions for difficult primary total knee arthroplasty. J Knee Surg. 2007;20:195–198. doi: 10.1055/s-0030-1248042. [DOI] [PubMed] [Google Scholar]
- 17.Girard J, Amzallag M, Pasquier G, Mulliez A, Brosset T, Gougeon F, Duhamel A, Migaud H. Total knee arthroplasty in valgus knees: predictive preoperative parameters influencing a constrained design selection. Orthop Traumatol Surg Res. 2009;95:260–266. doi: 10.1016/j.otsr.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 18.Lachiewicz PF, Soileau ES. Results of a second-generation constrained condylar prosthesis in primary total knee arthroplasty. J Arthroplasty. 2011;26:1228–1231. doi: 10.1016/j.arth.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 19.Engh GA. Bone loss classification. In: Engh GA, Rorabeck CH, editors. Revision total knee arthroplasty. Baltimore: Williams and Wilkins; 1997. pp. 63–120. [Google Scholar]
- 20.Murray PB, Rand JA, Hanssen AD. Cemented long-stem revision total knee arthroplasty. Clin Orthop Relat Res. 1994;309:116–123. [PubMed] [Google Scholar]
- 21.Fuchs S, Sandmann C, Gerdemann G, Skwara A, Tibesku CO, Bottner F. Quality of life and clinical outcome in salvage revision total knee replacement: hinged vs total condylar design. Knee Surg Sports Traumatol Arthrosc. 2004;12:140–143. doi: 10.1007/s00167-003-0401-8. [DOI] [PubMed] [Google Scholar]
- 22.Burnett RS, Butler RA, Barrack RL. Extensor mechanism allograft reconstruction in TKA al a mean of 56 months. Clin Orthop Relat Res. 2006;452:159–165. doi: 10.1097/01.blo.0000238818.25530.2b. [DOI] [PubMed] [Google Scholar]
- 23.Hossain F, Patel S, Haddad FS. Midterm assessment of causes and results of revision total knee arthroplasty. Clin Orthop Relat Res. 2010;468:1221–1228. doi: 10.1007/s11999-009-1204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jones RE. Total knee arthroplasty with modular rotating platform hinge. Orthopedics. 2006;29(9 Suppl):S80–S82. [PubMed] [Google Scholar]
- 25.Utting MR, Newman JH. Customised hinged knee replacements as a salvage procedure for failed total knee arthroplasty. Knee. 2004;11:475–479. doi: 10.1016/j.knee.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 26.Hardeman F, Londers J, Favril A, Witvrouw E, Bellemans J, Victor J. Predisposing factors which are relevant for the clinical outcome after revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;206:1049–1056. doi: 10.1007/s00167-011-1624-8. [DOI] [PubMed] [Google Scholar]
- 27.Panni AS, Vasso M, Cerciello S. Modular augmentation in revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012 doi: 10.1007/s00167-012-2258-1. [DOI] [PubMed] [Google Scholar]