Abstract
Purpose
We present our experience of using a newly modified Stoppa approach combined with a lateral approach to the iliac crest in patients with acetabular fractures in reference to fracture reduction and fixation, technical aspects, and the incidence of complications.
Methods
We used a consecutive group of 29 adult patients with acetabular fractures treated operatively with a newly modified Stoppa approach between 2009 and 2011. The newly modified Stoppa approach was performed to fix the acetabular fractures with main anterior displacement and the anterior and lateral parts of the pelvis. This approach was combined with a lateral approach on the iliac crest for fractures of the iliac wing.
Results
All the patients were followed up for at least 1.5 years. Of the 29 patients, ten anterior column, two associated both column, seven anterior column with posterior hemi-transverse, four transverse, and six T-type fractures. The average blood loss was 950 mL, and average operative time was 155 minutes. Anatomic or satisfactory reduction was achieved in 96 % of the acetabular fractures. Two patients had mild symptoms of the lateral femoral cutaneous nerve and improved within three months.
Conclusions
The newly modified Stoppa approach provides excellent visualization to the anterior column, quadrilateral surface and permits good postoperative results for treatment of acetabular fractures. We considered this technique as a viable alternative for the ilioinguinal approach when exposure of the anterior acetabulum is needed.
Introduction
Surgical management of displaced acetabular fractures has become the gold standard after the early work of Letournel [1–4]. The surgical decision making entails the fracture classification and operative approach. The choice of operative approach is dependent on the fracture type, direction of displacement, skin situation at the surgical incision site, and duration from initial injury [5–7]. Generally, the operative approaches to the acetabulum fractures can be classified into anterior, posterior, extensile and combined approaches. Those fractures with the main anterior displacement are approached anteriorly, while those with the main posterior displacement are approached posteriorly. A combined or extended approach is used if the displacement involves both the anterior and posterior parts of the acetabulum. Although the extended and combined approaches provide excellent access to visualize, reduce, and apply instrumentation to fix the fragments, they are thought to have higher complication rates and more morbidity compared with other limited approaches [8–11]. On the other hand, too limited an exposure might not provide adequate visualization for reduction and fixation of complex fracture types.
The ilioinguinal approach to the acetabulum, first described in 1961 by Letournel [1, 3], is often indicated in anterior wall and column fractures, anterior column with posterior hemi-transverse fractures, and selected both column fractures, transverse and T-type fractures with mainly anterior displacement. Its main limitations include difficulty in reducing and employing instrumentation to the quadrilateral surface and posterior column. And the main complications comprise high rates of postoperative wound infections and iatrogenic injury to the femoral nerve and the iliofemoral blood vessels [12, 13].
Stoppa described a midline approach for the treatment of complicated groin and incisional hernias with the support of a Dacron tulle prosthesis in 1989 [14]. Cole and Bolhofner reported this Stoppa approach could provide direct exposure to the medial wall, quadrilateral surface, and even extend to the sacroiliac joint, which could safely and effectively be used for reducing acetabular fractures [6]. However, this midline approach does not provide enough close visualization for the fracture patterns with main anterior displacement and treating the fractures for anatomical reduction of the iliac wing.
This study presents our experience of internal fixation of the acetabular fractures and pelvic fractures using a newly modified Stoppa approach, which provides closer visualization to the entire anterior column, quadrilateral surface and the pelvic brim portion of the posterior column, and permits stable internal fixation for the acetabular fracture patterns with main anterior displacement and the anterior and lateral parts of the pelvis.
Patients and methods
Patients
From February 2009 to April 2011, 29 cases of acetabular fractures were treated at our institution. The study group (n = 29) included 22 male and seven female patients with an average age of 42.3 years (range, 21–62 years), and the average injury severity score (ISS) was 18.7 (range, seven–42). There were five elementary fractures, ten anterior column, two associated both column, seven anterior column with posterior hemitransverse, four transverse, and six T-type fractures according to the classification of Judet and Letournel [3]. The mechanism of the initial injury was motor vehicle collision in 17 cases, fall from a height in nine cases, and industrial accidents in three cases (Table 1).
Table 1.
Demographic characteristics of the patients (N = 29)
| Variable | Value | Percent |
|---|---|---|
| Mean age (years) | 42.3 | |
| Male:female ratio | 22/7 | |
| Injury Severity Score (median) | 18.7 | |
| Acetabular fracture type (Letournel) | ||
| Anterior column | 10 | 34.5 |
| Both column | 2 | 6.9 |
| Anterior column with posterior hemitransverse | 7 | 24.1 |
| Transverse | 4 | 13.8 |
| T-type | 6 | 20.7 |
| Mechanism of injury | ||
| Motor vehicle collision | 17 | 58.6 |
| Fall from a height | 9 | 31.0 |
| Industrial accidents | 3 | 10.4 |
All the patients were regularly followed outpatients at two weeks, six weeks, three months, six months, and one year postoperatively. AP pelvic and Judet radiographs were taken and reviewed by an independent orthopaedic trauma surgeon, then the results of all fractures were classified by one of the authors. Postoperative fracture reduction of the acetabular fractures was evaluated on all three views with the scoring system published by Matta in 1996 [15], and a displacement of 1 mm or less was considered an anatomic reduction for iliac wing fractures according to Pohlemann [16]. The Harris hip score was used in the functional outcome of the acetabular fractures [17]. The perioperative data and incidence of complications were retrospectively reviewed for all patients treated with the newly modified Stoppa approach that had a minimum 18-months follow up.
The inclusion criteria for this study consisted of all simple and combined acetabular fracture types with main anterior displacement. And the patients with history of cesarean section, hysterectomy, bladder injury, prostatectomy, or bladder surgery were excluded. The indications for surgical treatment included any fracture with an obvious instability of the weight bearing area of the acetabulum, and displacement exceeding 2 mm of the non weight bearing area of the hip joint with or without dislocation of the joint (37 patients were excluded).
Surgical technique
All patients were treated with a similar surgical process. The patient was placed supine on the operating table to allow adequate visualization on AP and Judet radiographs. The injured limb was draped freely and the ipsilateral hip and knee were slightly flexed in order to relax the iliopsoas muscle and the external iliac neurovascular bundle. A Foley catheter was placed for bladder protection, improved visualization, and monitoring fluid balance. The surgical field was prepped from the nipple line down to the pubic symphysis; meanwhile, the entire ipsilateral limb was prepped. Prophylactic antibiotics were routinely administered. The surgeon stood on the side contralateral to the fractured acetabulum.
The newly modified Stoppa approach was performed through the inner two-thirds of the line 2 cm above the inguinal ligament and parallel to it (Fig. 1). Dissection was performed through the skin and subcutaneous tissue to the anterior rectus fascia, and the inferior epigastric artery was ligated after the rectus fascia was split. The transversalis fascia was incised just superior to the symphysis pubis and blunt dissection of the preperitoneal space was performed. Subsequently, the peritoneal sac was freed from its surroundings and it was manipulated upwards by a intestinal spatula and away from the surgeon. A subperiosteal dissection was performed along the posterior surface of the pelvic brim into the quadrilateral surface and posterior column, so that visualization of the quadrilateral surface and the medial aspect of the posterior column was obtained. The external iliac vessels and femoral nerve were protected by a Deaver retractor placed under the iliopsoas, and the rectus muscle was retracted to the inner side. As the dissection was performed posterior to the sacroiliac joint, the obturator vessels and nerve were protected by a narrow malleable retractor placed in the sciatic notch, and the connecting vessels between the external iliac and obturator vessels were addressed when present.
Fig. 1.
Incision of the newly modified Stoppa approach and the lateral approach on the iliac crest used for reduction and fixation of high fractures in the anterior column exiting the iliac crest
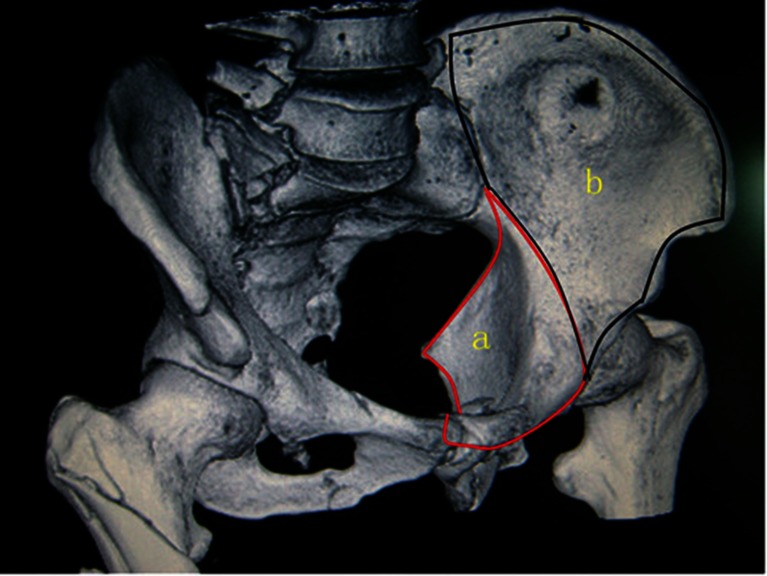
The lateral approach on the iliac crest can be performed simultaneously if adequate surgeons are present. This lateral window permits reduction and fixation fractures with a high anterior column component and the entire iliac wing, which also allows placement of posterior column lag screws. The skin bridge is maintained between the new Stoppa approach and the lateral approach on the iliac crest. In this way, full exposure and access of the quadrilateral surface and the iliac fossa is possible (Fig. 2).
Fig. 2.
Exposure region of the newly modified Stoppa approach (area a) and the lateral approach on the iliac crest (area b)
After adequate exposure of the fracture sites, the first step in reduction was to manage the high anterior column fractures exiting the iliac crest. Next the anterior column was reduced through the new Stoppa approach and/or the lateral window, and provisional fixation with a pelvic clamp or K-wires. Last the fracture of the quadrilateral surface (and posterior column if present) was reduced through the new Stoppa approach window and provisional reduction can be maintained with K-wires or a short plate.
Next, a pelvic reconstruction plate (Synthes, Paoli, PA) was contoured to fit the infrapectineal region inside the true pelvis through the newly modified Stoppa approach. The plate should be close to the sacroiliac joint. Posteriorly it was secured at the superior aspect of the sciatic notch in the sciatic buttress region with one to two screws, and then anteriorly with one to two screws in the superior pubic ramus (Fig. 3). For fractures with a high anterior column, a long supra-pectineal reconstruction plate was fixed on the superior surface of the pelvic brim and ramus through the two windows of the combined apporach (Figs. 3 and 4).
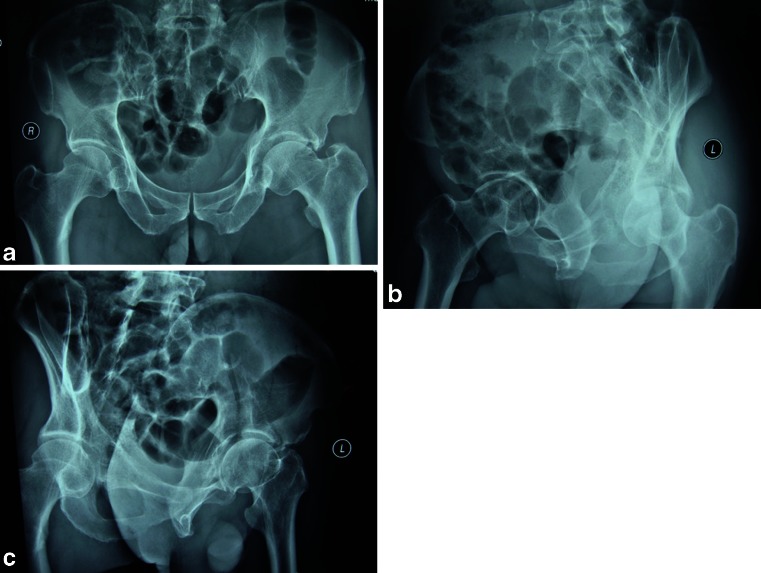
Fig. 3.
Preoperative anteroposterior (a), obturator oblique (b), and iliac oblique (c) view radiographs show anterior column with posterior hemitransverse
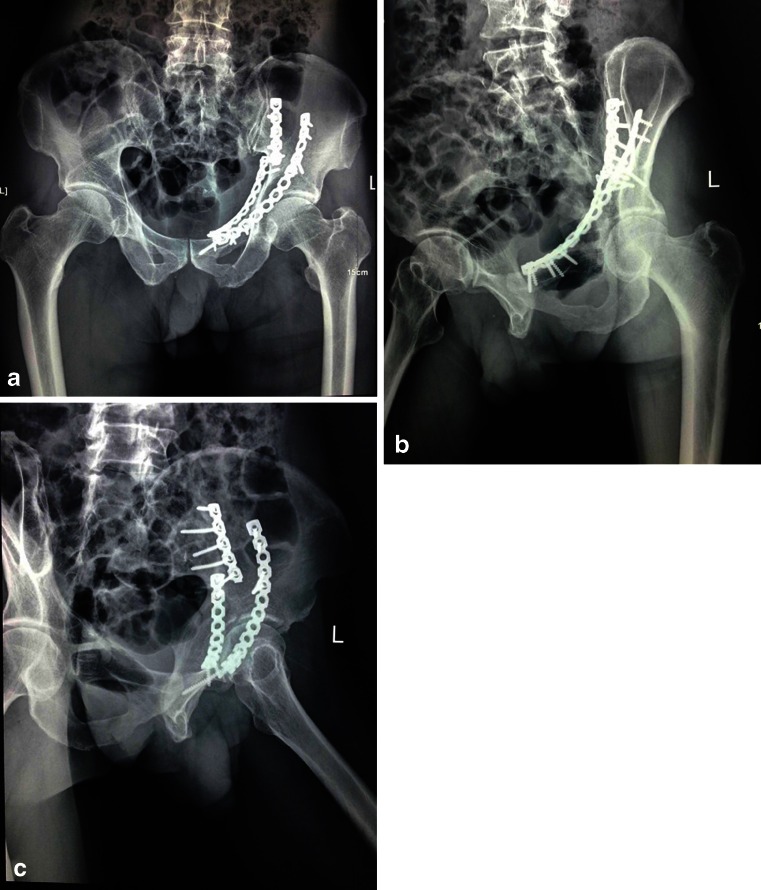
Fig. 4.
Postoperative anteroposterior (a), obturator oblique (b), and iliac oblique (c) view radiographs of the same patient shown in Fig. 3
Reduction and placement of fixation were evaluated with intraoperative fluoroscopic AP and Judet radiographs. After irrigation and hemostasis was performed, a drain was left in the preperitoneal cavity, and a second was left in the internal iliac fossa if the lateral approach on the iliac crest was used. The rectus sheath was closed with a monofilament resorbable suture in a running fashion. The skin was closed with interrupted monofilament sutures.
The drains were removed 24 to 48 hours postoperatively. Cephalosporin was routinely given for 48 hours, and administration of 10 mg Xarelto (Bayer, Leverkusen, Germany) was taken once a day for the prevention of venous thromboembolism starting the first day postoperative and continued for three weeks. Depending on associated injuries and patient condition, the patients were encouraged to walk with crutches after six to eight weeks, with full weight bearing at 12 weeks postoperatively.
Results
Twenty-nine patients in this study were followed up regularly for an average of two years (range, 1.5–three years). The average time from injury to surgery was 6.8 days (range, five–13 days), this interval was mostly determined by the patients’ general condition. In this study, four transverse fractures were treated with plates only using the newly modified Stoppa approach, and 25 patients were treated using the newly modified Stoppa approach combined with a lateral iliac surgical window.
Operative parameters included an average operative time from skin incision to skin closure of 155 minutes (range, 90–270 minutes), average estimated blood loss of 950 mL (range, 600–1800 mL) for all patients, and an average amount of two units (range, one to five units) of packed red blood cells (PRBC) were infused for 23 patients during or after the operation (Table 2).
Table 2.
Surgical data of the patients
| Characteristic | Value | Percent |
|---|---|---|
| Operation time, minutes (median; range) | 155 (90–270) | |
| Blood loss, ml (median; range) | 950 (600–1800) | |
| Blood transfusions (median; range) | 2 (1–5) | |
| Postoperative reduction (acetabular fractures) | ||
| Anatomic (≤1 mm) | 24 | 82.8 |
| Imperfect (>1 to <3 mm) | 4 | 13.8 |
| Poor (≥ 3 mm) | 1 | 3.4 |
| Postoperative reduction (iliac wing fractures) | ||
| Anatomic (≤1 mm) | 29 | 100 |
| Functional result (Harris hip score) | ||
| Excellent (≥ 90 points) | 11 | 37.9 |
| Good (80–89) | 16 | 55.2 |
| Fair (70–79) | 2 | 6.9 |
| Poor (≤ 70) | 0 | 0 |
For acetabular fractures, an anatomic reduction was obtained in 24 patients (82.8 %), a satisfactory reduction in four patients (13.8 %) and poor reduction in one patient (3.4 %). All iliac wing fractures were anatomically reduced (n = 29). The Harris hip score was more than 90 points in 11 patients (37.9 %), 80–89 in 16 (55.2 %) and less than 79 in two patients (9 %) (Table 2).
Complications included two patients who had mild symptoms of the lateral femoral cutaneous nerve which improved within three months. There were no deep venous thrombosis and infectious encountered, nor iatrogenic lesions of the obturator vessels and the spermatic cord.
Discussion
Although intrapelvic techniques for the treatment of acetabular fractures has developed over the last 40 years, treatment of the acetabular fractures is still demanding. The ilioinguinal approach, which is widely used within intrapelvic approaches, has the advantages of allowing a wide view of anterior and transverse fracture patterns, a low risk of vascular injury, as well as a low rate of heterotopic ossification [1, 6, 18]. However, because of complicated anatomic structures in the surgical area, the learning curve is quite sharp, and the combined view through the four windows still only allows a limited assessment of the fracture patterns, and other indirect reduction skills are often used. Therefore, this approach has been modified in order to provide easy access to the medial wall of the acetabulum [19, 20].
The application of an extraperitoneal approach for fixation of pelvic fractures was first described by Hirvensalo. Cole and Bolhofner described a modified Stoppa approach through the rectus abdominus muscle for the treatment of fractures of the pelvic ring or acetabulum [6]. The primary modification of the primitive Stoppa approach was the dissection performed laterally and posteriorly into the internal iliac fossa and the quadrilateral surface. And publications using this approach for infrapectineal plating and management of acetabular fractures involving the quadrilateral surface was reported [8, 9]. However, we find that the exposure of the acetabulum was restricted due to obstruction of the retus abdominis and the subcutaneous fatty layer through the vertical midline incision, especially in obese patients. Therefore, we further modified this approach mentioned above which maintains the advantages of the Stoppa approach, and even closer to the acetabulum.
The intent of this study was to present our experience of internal fixation of the acetabular fractures and pelvic fracture using a newly modified Stoppa approach. This approach is indicated in all simple and combined acetabular fracture types, associated anterior column with posterior hemitransverse, selected both column, transverse and Ttype fractures. The isolated, totally posterior-located acetabular fracture patterns (posterior wall, posterior column) and posterior pelvic ring injuries treated by sacroiliac screw fixation were excluded. At the same time, the patients with history of cesarean section, hysterectomy, bladder injury, or bladder surgery were excluded in this study, which may increase the risk of cystotomy, contamination or infection. And the patients with a history of prostatectomy were also excluded which may increase the risk of perioperative bleeding for excessive scarring of the structures in the Retzius space.
The technique described in this study has not been reported previously, which is based on an anterolateral approach directed to the inside of the acetabulum. Compared to the modified Stoppa approach with a vertical midline incision, the newly modified Stoppa approach is performed on the injured side and the procedure window is between the rectus muscle and the iliopsoas, which is closer to the acetabulum and quadrilateral surface, and easier for reduction and fixation of the fracture fragments after proper exposure. Meanwhile, to obtain maximum exposure and allow easier manipulation for both the associated column fracture and fractures involving the iliac wing, a lateral approach on the iliac crest was considered [8].
Another advantage is that this approach does not need to dissect the lateral femoral cutaneous nerve, the femoral nerve, the external iliac vessels, the lymphatic channels of the inguinal canal, the spermatic cord or round ligament like the ilioinguinal approach [1], which is associated with the incidence of thrombosis, lymphedema and nerve injury. These structures were enclosed in their fasciae and retracted as a group in this approach. Of 29 patients, no acute vascular injuries were noted and no deep venous thrombosis was encountered, which is comparable to the study of Andersen et al. [21]. Two cases had mild symptoms of the lateral femoral cutaneous nerve and improved within three months.
This series included 29 patients with acetabular fractures treated through this newly modified Stoppa approach by a single surgeon who were followed radiographically and clinically for an average of 1.5 years. We were able to obtain an acceptable result in 96.6 % of the acetabular fractures—82.8 % anatomic and 13.8 % satisfactory reduction—which is in keeping with previous studies [12, 21–24]. And the lateral approach on the iliac crest was used in 25 patients with high anterior column fractures exiting the iliac crest or requiring placement of posterior column lag screws.
It is important to note that the newly modified Stoppa approach combined with the lateral approach on the iliac crest could achieve the same visualization as the ilioinguinal approach (Fig. 2), which enlarges the indication of this approach, and some complex acetabulum fractures could be treated through this combined approach. On the one hand, the duration of the operative procedure will be curtailed, on the other hand, the amount of blood loss will be reduced.
It is our experience that the connecting vessels between the external iliac and obturator vessels, the corona mortis [25], should be looked after meticulously and ligation if detected before the dissection was performed into the quadrilateral surface. The bleeding can not be controlled easily if it were torn or cut, especially if fracture haematoma exists in the acetabulum area.
Postoperative ileus is a common sequela of abdominal surgery, and no postoperative ileus was observed in the patients in this study, perhaps because of the extraperitoneal and minimally invasive approach. And local infection is a crucial threat to the outcome of operative fracture treatment, but we had no deep infections in this study. Also the gluteal muscles did not disrupt in this study, and we had no instances of heterotopic ossification.
This study has several limitations. It was a retrospective review and lacked a comparative cohort. And just a relatively small number of patients was treated using this newly modified approach. It may need a larger number of cases to study and long-term follow-up.
Conclusion
Our experience using of the newly modified Stoppa approach for the treatment of acetabular fractures provides excellent access and visualization to the anterior column, quadrilateral surface and sciatic notch, while permitting good to excellent reduction and fixation. The rate of complications in this study associated with the newly modified Stoppa approach is comparable to that reported for the AIP (modified Rives-Stoppa) and ilioinguinal approaches. And as such, we considered this technique as a viable alternative for the ilioinguinal approach when exposure of the anterior acetabulum is needed.
Acknowledgments
Conflict of interest
None.
References
- 1.Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993;292:62–76. [PubMed] [Google Scholar]
- 2.Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary report. J Bone Joint Surg Am. 1964;46:1615–1646. [PubMed] [Google Scholar]
- 3.Letournel E. Fractures of the acetabulum. A study of a series of 75 cases. 1961. Clin Orthop Relat Res. 1994;305:5–9. doi: 10.1097/00003086-199408000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Letournel E. Acetabulum fractures: classification and management. Clin Orthop Relat Res. 1980;151:81–106. [PubMed] [Google Scholar]
- 5.Letournel E. Fractures of the acetabulum: a study of a series of 75 cases – Les fractures du cotyle, etude d'une serie de 75 cas. J de Chirurgie 82:47–87, 1961. (Translated and substantially abridged) J Orthop Trauma. 2006;20(1 Suppl):S15–19. [PubMed] [Google Scholar]
- 6.Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994;305:112–123. doi: 10.1097/00003086-199408000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Gupta RK, Singh H, Dev B, Kansay R, Gupta P, Garg S. Results of operative treatment of acetabular fractures from the Third World—how local factors affect the outcome. Int Orthop. 2009;33(2):347–352. doi: 10.1007/s00264-007-0461-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hirvensalo E, Lindahl J, Kiljunen V. Modified and new approaches for pelvic and acetabular surgery. Injury. 2007;38(4):431–441. doi: 10.1016/j.injury.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 9.Ponsen KJ, Joosse P, Schigt A, Goslings JC, Luitse JS. Internal fracture fixation using the Stoppa approach in pelvic ring and acetabular fractures: technical aspects and operative results. J Trauma. 2006;61(3):662–667. doi: 10.1097/01.ta.0000219693.95873.24. [DOI] [PubMed] [Google Scholar]
- 10.Jakob M, Droeser R, Zobrist R, Messmer P, Regazzoni P. A less invasive anterior intrapelvic approach for the treatment of acetabular fractures and pelvic ring injuries. J Trauma. 2006;60(6):1364–1370. doi: 10.1097/01.ta.0000208139.97474.f7. [DOI] [PubMed] [Google Scholar]
- 11.Qureshi AA, Archdeacon MT, Jenkins MA, Infante A, DiPasquale T, Bolhofner BR. Infrapectineal plating for acetabular fractures: a technical adjunct to internal fixation. J Orthop Trauma. 2004;18(3):175–178. doi: 10.1097/00005131-200403000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Matta JM. Operative treatment of acetabular fractures through the ilioinguinal approach: a 10-year perspective. J Orthop Trauma. 2006;20(1 Suppl):S20–29. [PubMed] [Google Scholar]
- 13.Helfet DL, Borrelli J, Jr, DiPasquale T, Sanders R. Stabilization of acetabular fractures in elderly patients. J Bone Joint Surg Am. 1992;74(5):753–765. [PubMed] [Google Scholar]
- 14.Stoppa RE. The treatment of complicated groin and incisional hernias. World J Surg. 1989;13(5):545–554. doi: 10.1007/BF01658869. [DOI] [PubMed] [Google Scholar]
- 15.Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78(11):1632–1645. [PubMed] [Google Scholar]
- 16.Pohlemann T, Gansslen A, Schellwald O, Culemann U, Tscherne H. Outcome after pelvic ring injuries. Injury. 1996;27(Suppl 2):B31–38. [PubMed] [Google Scholar]
- 17.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 18.Ghalambor N, Matta JM, Bernstein L. Heterotopic ossification following operative treatment of acetabular fracture. An analysis of risk factors. Clin Orthop Relat Res. 1994;305:96–105. doi: 10.1097/00003086-199408000-00013. [DOI] [PubMed] [Google Scholar]
- 19.Moed BR, Dickson KF, Kregor PJ, Reilly MC, Vrahas MS. The surgical treatment of acetabular fractures. Instr Course Lect. 2010;59:481–501. [PubMed] [Google Scholar]
- 20.Sagi HC, Afsari A, Dziadosz D. The anterior intra-pelvic (modified Rives-Stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010;24(5):263–270. doi: 10.1097/BOT.0b013e3181dd0b84. [DOI] [PubMed] [Google Scholar]
- 21.Andersen RC, O’Toole RV, Nascone JW, Sciadini MF, Frisch HM, Turen CW. Modified stoppa approach for acetabular fractures with anterior and posterior column displacement: quantification of radiographic reduction and analysis of interobserver variability. J Orthop Trauma. 2010;24(5):271–278. doi: 10.1097/BOT.0b013e3181b2b4ca. [DOI] [PubMed] [Google Scholar]
- 22.Ebraheim NA, Patil V, Liu J, Sanford CG, Jr, Haman SP. Reconstruction of comminuted posterior wall fractures using the buttress technique: a review of 32 fractures. Int Orthop. 2007;31(5):671–675. doi: 10.1007/s00264-006-0246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sen RK, Tripathy SK, Aggarwal S, Tamuk T. Posterior wall reconstruction using iliac crest strut graft in severely comminuted posterior acetabular wall fracture. Int Orthop. 2011;35(8):1223–1228. doi: 10.1007/s00264-010-1177-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stockle U, Hoffmann R, Nittinger M, Sudkamp NP, Haas NP. Screw fixation of acetabular fractures. Int Orthop. 2000;24(3):143–147. doi: 10.1007/s002640000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pungpapong SU, Thum-umnauysuk S. Incidence of corona mortis; preperitoneal anatomy for laparoscopic hernia repair. J Med Assoc Thai. 2005;88(Suppl 4):S51–53. [PubMed] [Google Scholar]