Abstract
Purpose
Studies have shown that up to 25 % of TKA patients are dissatisfied with the implanted knee, even if registry data shows ten-year revision rates below 5 %. It has been the question of our study, if it would be possible to identify those patients at risk for dissatisfaction pre-operatively.
Methods
The data of 1,121 consecutive TKA patients with a follow-up between one and six years have been analysed retrospectively. Demographic, radiologic and perioperative variables have been recorded and all patients were asked by questionnaire for satisfaction with the implanted knee. Logistic regression models have been used to identify significant risk factors.
Results
The data of 996 patients (89 %) were complete, 849 (85.2 %) reported satisfaction and 147 (14.8 %) dissatisfaction. Patients’ satisfaction was independent of the time after operation (p = 0.285). The only factor which influenced patients’ satisfaction was the osteoarthritic severity. In comparison to severe arthritis Kellgren Lawrence IV°, the risk for dissatisfaction was 2.556-fold elevated for arthritis grade III° (p < 0.001) and 2.956-fold higher for grade II° (p = 0.001).
Conclusions
Patients suffering from mild or moderate osteoarthritis are at risk for dissatisfaction after TKA. The TKA indication in those patients should therefore be critically proven. Furthermore, to adjust patients’ expectations, the elevated dissatisfaction risk in case of mild or moderate osteoarthritis should be included into patients’ pre-operative information.
Introduction
Total knee arthroplasty (TKA) has revolutionized the care of severe arthritis of the knee joint [1]. Registry data show excellent implant survival with ten-year revision rates around 5 %. However, there is a well-known difference between patients’ satisfaction and measured clinical outcome in TKA [2–6]. Recent studies have demonstrated that, contrary to hip arthroplasty patients, up to 25 % of the TKA patients are dissatisfied with the implanted total knee [1, 7–9]. A pre-operative identification of patients at risk would be very helpful to critically prove the indications for TKA and to inform patients about a potential inferior outcome. So far only a few studies have been undertaken to investigate if pre-operative risk factors for postoperative dissatisfaction exist [3, 7, 8, 10–15]. Studies in the United States indicated that in one of six TKA patients, prostheses have been implanted before development of severe arthritis [16, 17]. It was our hypothesis that those patients suffering from mild or moderate osteoarthritis, as well as young patients, might be at risk of dissatisfaction with the implanted TKA. Therefore, it was the question of our study, if it would be possible to identify patients at risk for dissatisfaction after TKA by pre-operative, patient-specific factors.
Material and methods
In the authors’ clinic, the data of all primary total knee arthroplasties between January 2006 and December 2010 were analysed retrospectively. Exclusion criteria were the implantation of primary hinged prostheses and those with an antiallergic ceramic coating. The remaining 1,121 prostheses have been included in our study. To allow for a minimum follow up of one year, data collection was performed in December 2011.
Operative procedure
During 2006 and 2010 two different implants (PFC sigma, DePuy, UK and Nexgen Highflex, Zimmer, USA) were implanted by use of conventional jigs as provided by the manufacturers (n = 342) or by use of an imageless computer navigation device (BrainLab, Germany; n = 779). All TKAs were implanted by use of a standard medial parapatellar approach; the postoperative regime did not differ between different implants or alignment techniques.
Patients’ documents as well as operation protocols were analysed and the following criteria were recorded:
Sociodemographic data: Age and gender of the patient, patient’s body mass index (BMI), American Society of Anesthesiologists (ASA) physical status score, living status (living alone yes/no), diagnosis (primary arthritis, post traumatic arthritis, rheumatoid arthritis), use of opioids before operation, diagnosed depression, pre-operative range of motion (good ROM: extension lag <5° and flexion > 120°, moderate ROM: extension lag <10° and flexion 100–120°, limited ROM: extension lag >10° or flexion <100°), Charnley score.
Perioperative data: type of anaesthesia (general anaesthesia, spinal anaesthesia, additional epidural catheter), type of implant (PFC, Nexgen), type of alignment technique (navigation, conventional).
Radiologic data: Long-leg X-rays before and after operation were analysed and the pre- and postoperative mechanical leg axis were measured. Furthermore, the pre-operative radiographic severities according to the Kellgren-Lawrence (K/L) criteria [18] were recorded. The radiologic data were available in 938 cases (84 %).
All patients were asked by questionnaire for general satisfaction with the implanted knee prosthesis as described in the literature [1, 2, 15]. The possible answers included five graduate answers: (1) completely satisfied, (2) partially satisfied, (3) neutral, (4) partially unsatisfied, (5) completely unsatisfied. Those data were complete in 996 patients (89 %). For statistical analysis, answers (1)–(3) have been grouped as “satisfied/neutral”, answers (4)–(5) as “unsatisfied”.
Statistics
Variables were compared using the Student’s t-test or chi-squared test with a significance level of α < 0.1. Those factors showing significant differences have been included into logistic regression models for further analysis. The forward stepwise algorithm as well as the Wald statistic was used with a significance level of α < 0.05. For statistical calculations the SPSS 21 for Mac software (IBM, NY) was used.
Results
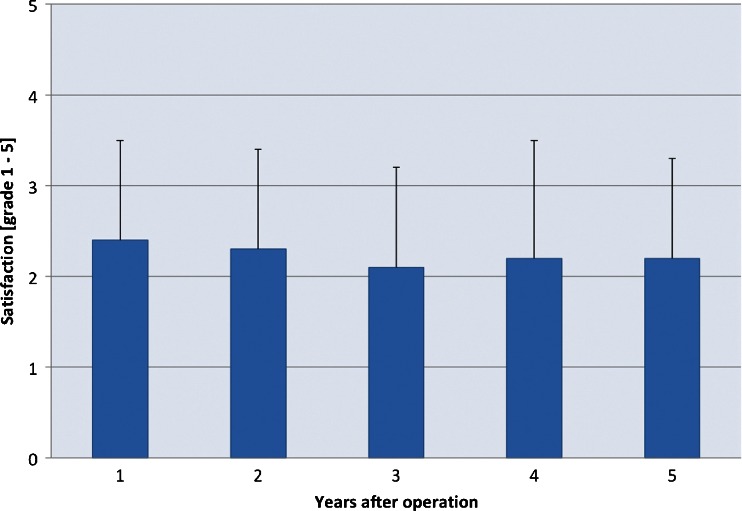
The mean follow up was 2.8 years, ranging from one to six years. Cumulative revision rate averaged 3 % (n = 32). As published before, Cox proportional hazard models identified “younger age” (p < 0.001) and “conventional jig technique” (p = 0.012) as risk factors for revision [19]. Analysis showed that 85.2 % (n = 849) of the patients reported “satisfied or neutral” with the implanted knee joint, whereas 14.8 % (n = 147) were dissatisfied with the implanted knee joint. No significant correlation between time period after operation and satisfaction was detected (Fig. 1, p = 0.285). Table 1 shows univariate analysis of patients’ satisfaction and pre-operative variables, radiologic variables and perioperative variables. The criteria “age of the patient” and “pre-operative arthritis level” were identified as those which influenced patients’ satisfaction significantly. Therefore these two were included in logistic regression models. These statistic calculations showed that the criterion “age” lost it’s significant influence (p = 0.526, odds ratio 0.993, 95%CI 0.974–1.014). By contrast, the factor “severity of arthritis” kept its significant influence, i.e. in comparison to severe osteoarthritis Kellgren-Lawrence grade IV, the risk for dissatisfaction was 2.556-fold elevated for arthritis grade III° and 2.956-fold higher for grade II° (p < 0.001, p = 0.001; Table 2).
Fig. 1.
Levels of satisfaction are shown for different time periods after operation. No significant correlation between time after operation and satisfaction was found
Table 1.
Univariate analysis between preoperative, radiologic, perioperative criteria and patients’ satisfaction
| Variables | Total (%) | Satisfied (n = 849) | Dissatisfied (n = 147) | Level of significance (p) |
|---|---|---|---|---|
| Pre-operative criteria | ||||
| Female | 658 (66 %) | 66 % | 68 % | 0.638b |
| Age [years] | – | 69 | 67 | 0.069a |
| BMI | – | 31 | 31 | 0.535a |
| Comorbidity (ASA 3–4) | 192 (23 %) | 24 % | 21 % | 0.870b |
| Living alone | 246 (33 %) | 32 % | 35 % | 0.571b |
| Opioid use | 39 (6 %) | 5 % | 9 % | 0.156b |
| Depression | 75 (9 %) | 9 % | 8 % | 1.0b |
| Post traumatic arthritis | 64 (7 %) | 6 % | 7 % | 0.855b |
| Rheumatoid arthritis | 82 (8 %) | 8 % | 8 % | 1.0b |
| Limited ROM | 270 (34 %) | 34 % | 31 % | 0.862b |
| Charnley score 1 | 662 (77 %) | 77 % | 78 % | 0.799b |
| Radiologic criteria | ||||
| Level of arthritis (K/L) grade 4 | 481 (54 %) | 57 % | 34 % | <0.001b |
| Mechanical leg axis [°] | – | 3 | 2 | 0.101a |
| Perioperative criteria | ||||
| Implant PFC | 845 (85 %) | 85 % | 84 % | 0.619b |
| Use of computer navigation | 699 (70 %) | 71 % | 67 % | 0.329b |
| Use of epidural catheter | 453 (56 %) | 57 % | 52 % | 0.411b |
| Postoperative leg axis [°] | 0 | 0 | 0.163a | |
ROM range of motion, BMI body mass index
Bold values indicate statistical significance
a Two-tailed Students t-test
b Chi-squared test
Table 2.
Logistic regression models are shown for arthritic severity
| Arthritis grade (K/L) | Number (n) | Logistic regression: forward Wald | ||
|---|---|---|---|---|
| p-value | Odds ratio | 95 % CI | ||
| I | 11 | 0.336 | 2.153 | 0.451–10.273 |
| II | 77 | 0.001 | 2.956 | 1.605–5.443 |
| III | 321 | <0.001 | 2.556 | 1.699–3.844 |
| IV | 481 | <0.001 | 0.103 | – |
CI confidence interval
Discussion
There are two different approaches to evaluate the success of total knee prostheses. The first approach is with physician-derived measurements, such as revision rates or function scores. The second way is questioning patient’s subjective satisfaction with the implanted total knee. Numerous studies focused on function scores and revision rates after TKA, indicating that TKA is a highly effective and cost-efficient treatment of knee arthritis. However, different studies indicate a substantial discrepancy between measured scores such as revision rates or function on the one hand and patient’s satisfaction with the operation on the other [2–5]. In our study population we detected a mean cumulative revision rate of 3 % after 2.8 years [19]. Those data are comparable to the well-known arthroplasty registers, e.g. the Swedish knee register showed an average revision rate of 2.5–3 % after three years and the Australian register circa 2.8 % after three years. However, our survey of patients’ satisfaction with the implanted TKA resulted in an alarming rate of 14.8 % unsatisfied or very unsatisfied patients. Some other studies focused on patients’ satisfaction after TKA. Robertsson et al. [20] reported dissatisfaction rates of 8 %, Hamilton et al., Bourne et al. and Scott et al. found dissatisfaction rates of 19 % after TKA [1, 7, 8], Baker found 18 % [21], Nilsdotter 7 % [15], Noble et al. 14 % [9] and Gandhi found 25 % dissatisfied [22]. Different authors compared satisfaction rates after TKA and total hip arthroplasty, whereby all studies found significantly higher satisfaction rates for patients with hip prostheses between 88 % and 91 %, indicating the specific high number of unsatisfied patients after TKA [1, 7, 23]. To summarize, the number of unsatisfied patients in our study as well as the published literature lies between 7 % and 25 % and contrasts the low revision rates after TKA. It has been the question of our study, if there are specific patients at risk for dissatisfaction, which could be identified by demographic, radiologic or perioperative factors. It would be essential to identify those patients before operation [1, 7]—the patient could be informed about the higher probability of dissatisfaction and the indication for operation could be critically proven. We hypothesized that “young age” and “mild osteoarthritis” might be risk factors for dissatisfaction. Indeed, our statistical analyses showed a highly significant influence of the radiologic arthritis severity on patients’ satisfaction; in comparison to those patients with a K/L grade IV, the risk for dissatisfaction was three-fold higher for those with a K/L grade II and 2.6-fold higher for patients with a K/L grade III. It is common sense that the classic indication to implant a TKA is the end stage arthritis K/L grade IV. However, the individual indication is a complex one that includes not only radiologic criteria, but involves multiple factors [16], e.g. a high symptom intensity and duration, severe functional loss, distorted ligamentous integrity and bad response to previous therapies may indicate a TKA even if the radiologic osteoarthritis severity is below K/L grade IV. In our study, only 54 % of the patients suffered from arthritis K/L grade IV, while 36 % had K/L grade III and the remaining 10 % grades I and II. In other words, in 10 % of the patients a total knee was implanted in spite of low arthritis severity. In those patients below K/L grade IV, other reasons besides the radiologic aspect of the knee influenced the indication to implant a TKA. Riddle et al. [16] analysed the extent of tibiofemoral arthritis in US patients and reported similar findings such that in 19 % of the patients a TKA was implanted with a K/L grade I or II. Similarly, Wise et al. reported 17 % of the TKA patients with a K/L grade below III [17]. Those authors suggest that for approximately one in six patients in the United States, TKA is being performed before the development of moderate or severe knee osteoarthritis. Our study shows similar data for Europe. This finding is especially remarkable as our study indicates those patients without severe osteoarthritis being at risk for postoperative dissatisfaction.
Besides radiologic criteria, multiple demographic and perioperative factors have been included in our statistical analysis. It has been our hypothesis that low osteoarthritis severity and young age predicted dissatisfaction after TKA. However, besides osteoarthritis severity none of those demographic or operative factors influenced patients’ satisfaction in our study in a significant way.
The question, if dissatisfaction could be predicted before operation, has been addressed in some other studies [3, 7, 8, 10–15]. However, to the best of our knowledge, only few included radiologic criteria. Merle-Vincent et al. [11] analyzed a two-year follow up of 264 patients and found a significantly lower satisfaction rate for those with mild or moderate osteoarthritis, obesity, depression and age below 70 years. Valdes et al. analyzed 860 TKAs with a mean follow up of three years [12]. Similarly, they identified lower osteoarthritis severity as a risk factor for postoperative dissatisfaction. Besides radiologic criteria, depression, higher BMI, younger age and female gender were associated with higher postoperative dissatisfaction rates. A recently published study compared the pre-operative osteoarthritis severity in four cohorts with and without persisting pain after TKA [24]. In the cohort with persisting pain, the rate of patients with pre-operative early grade osteoarthritis averaged 49 %, while only 5–10 % of the patients without persistent pain suffered from low-grade osteoarthritis before operation. Two other studies analyzed TKA patients’ functional outcome and pre-operative osteoarthritis severity. Cushnaghan et al. [14] performed a matched pair analysis of 325 patients and analyzed the six-year postoperative functional status. They found greater improvement in physical function for patients with severe osteoarthritis and those without pain in other joints. Contrary to the above cited studies, they found no influence of patients’ BMI or age. However, patients’ satisfaction has not been asked for. Similarly, Meding et al. analyzed the relationship of osteoarthritis severity and postoperative pain and function in 1,888 patients with a mean follow up of 2.5 years [25]. Their results contrast ours and the above-cited studies in that pain and function were independent of the pre-operative osteoarthritis severity. However, they found better functional improvement in those patients suffering from severe osteoarthritis. To summarize, the factor “low osteoarthritis severity” has been identified in our analysis and in four of five studies as an independent risk factor for dissatisfaction. The analysis of demographic factors such as BMI, age and gender revealed conflicting results.
Our study has some limitations. At first we used a retrospective study design. However, we included a consecutive series of 1,121 patients with an adequate follow-up rate of 89 %. Next, patients’ satisfaction was measured at different time points between one and six years after operation. To evaluate the influence of time after operation on the satisfaction rate, we performed a correlation analysis. Statistical analysis showed no influence of “time after operation” on satisfaction rates. Different studies focused on that topic, for example, Robertsson et al. [20] reported on 27,372 TKAs with two–17 year follow up from the Swedish Knee register. They found patient satisfaction was remarkably constant in patients not requiring revision procedures for all follow-up periods. Similarly, Nilsdotter et al. [15] showed comparable satisfaction rates one and five years after operation. Finally, we did not use a functional score such as the Knee Society score or the Oxford knee score. On the one hand, this could be interpreted as a limitation of our study; on the other hand the aim of our study was the identification of patients dissatisfied with the implanted knee. The proven difference between functional scores and subjective satisfaction has already been mentioned above. So far, there is no gold standard to evaluate patients’ satisfaction [3]. We therefore used a well-established questionnaire with five graduate answers as described in the literature [1, 2, 15].
In conclusion, our study showed an elevated risk for dissatisfaction after TKA in cases of mild or moderate osteoarthritis severity. Our results confirm the few existing studies, which included radiologic criteria and patients’ satisfaction. Those higher dissatisfaction rates are especially remarkable, as a substantial number of TKAs were implanted before development of severe osteoarthritis. The TKA indication in patients with mild or moderate osteoarthritis should therefore be critically proven. Furthermore, to adjust patients’ expectations, the elevated dissatisfaction risk in cases of mild or moderate osteoarthritis should be included into patients’ pre-operative information.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Bourne RB, Chesworth B, Davis A, Mahomed N, Charron K. Comparing patient outcomes after THA and TKA: is there a difference? Clin Orthop Relat Res. 2010;468(2):542–546. doi: 10.1007/s11999-009-1046-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sharkey PF, Miller AJ. Noise, numbness, and kneeling difficulties after total knee arthroplasty: is the outcome affected? J Arthroplasty. 2011;26(8):1427–1431. doi: 10.1016/j.arth.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 3.Matsuda S, Kawahara S, Okazaki K, Tashiro Y, Iwamoto Y (2012) Postoperative alignment and ROM affect patient satisfaction after TKA. Clin Orthop Relat Res 471(1):127–133. doi:10.1007/s11999-012-2533-y [DOI] [PMC free article] [PubMed]
- 4.Bullens PH, van Loon CJ, de Waal Malefijt MC, Laan RF, Veth RP. Patient satisfaction after total knee arthroplasty: a comparison between subjective and objective outcome assessments. J Arthroplasty. 2001;16(6):740–747. doi: 10.1054/arth.2001.23922. [DOI] [PubMed] [Google Scholar]
- 5.Brokelman RB, van Loon CJ, Rijnberg WJ. Patient versus surgeon satisfaction after total hip arthroplasty. J Bone Joint Surg Br. 2003;85(4):495–498. [PubMed] [Google Scholar]
- 6.Becker R, Doring C, Denecke A, Brosz M. Expectation, satisfaction and clinical outcome of patients after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19(9):1433–1441. doi: 10.1007/s00167-011-1621-y. [DOI] [PubMed] [Google Scholar]
- 7.Hamilton D, Henderson GR, Gaston P, Macdonald D, Howie C, Simpson AH. Comparative outcomes of total hip and knee arthroplasty: a prospective cohort study. Postgrad Med J. 2012;88(1045):627–631. doi: 10.1136/postgradmedj-2011-130715. [DOI] [PubMed] [Google Scholar]
- 8.Scott CE, Howie CR, MacDonald D, Biant LC. Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br. 2010;92(9):1253–1258. doi: 10.1302/0301-620X.92B9.24394. [DOI] [PubMed] [Google Scholar]
- 9.Gandhi R, Davey JR, Mahomed NN. Predicting patient dissatisfaction following joint replacement surgery. J Rheumatol. 2008;35(12):2415–2418. doi: 10.3899/jrheum.080295. [DOI] [PubMed] [Google Scholar]
- 10.Kim TK, Chang CB, Kang YG, Kim SJ, Seong SC. Causes and predictors of patient’s dissatisfaction after uncomplicated total knee arthroplasty. J Arthroplasty. 2009;24(2):263–271. doi: 10.1016/j.arth.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Merle-Vincent F, Couris CM, Schott AM, Conrozier T, Piperno M, Mathieu P, Vignon E. Factors predicting patient satisfaction 2 years after total knee arthroplasty for osteoarthritis. Joint Bone Spine. 2011;78(4):383–386. doi: 10.1016/j.jbspin.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 12.Valdes AM, Doherty SA, Zhang W, Muir KR, Maciewicz RA, Doherty M. Inverse relationship between preoperative radiographic severity and postoperative pain in patients with osteoarthritis who have undergone total joint arthroplasty. Semin Arthritis Rheum. 2012;41(4):568–575. doi: 10.1016/j.semarthrit.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 13.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cushnaghan J, Bennett J, Reading I, Croft P, Byng P, Cox K, Dieppe P, Coggon D, Cooper C. Long-term outcome following total knee arthroplasty: a controlled longitudinal study. Ann Rheum Dis. 2009;68(5):642–647. doi: 10.1136/ard.2008.093229. [DOI] [PubMed] [Google Scholar]
- 15.Nilsdotter AK, Toksvig-Larsen S, Roos EM. Knee arthroplasty: are patients’ expectations fulfilled? A prospective study of pain and function in 102 patients with 5-year follow-up. Acta Orthop. 2009;80(1):55–61. doi: 10.1080/17453670902805007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Riddle DL, Jiranek WA, Neff RS, Whitaker D, Hull JR. Extent of tibiofemoral osteoarthritis before knee arthroplasty: multicenter data from the osteoarthritis initiative. Clin Orthop Relat Res. 2012;470(10):2836–2842. doi: 10.1007/s11999-012-2328-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wise BL, Felson DT, Clancy M, Niu J, Neogi T, Lane NE, Hietpas J, Curtis JR, Bradley LA, Torner JC, Zhang Y. Consistency of knee pain and risk of knee replacement: the Multicenter Osteoarthritis study. J Rheumatol. 2011;38(7):1390–1395. doi: 10.3899/jrheum.100743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schnurr C, Gudden I, Eysel P, Konig DP. Influence of computer navigation on TKA revision rates. Int Orthop. 2012;36(11):2255–2260. doi: 10.1007/s00264-012-1606-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop. 2000;71(3):262–267. doi: 10.1080/000164700317411852. [DOI] [PubMed] [Google Scholar]
- 21.Baker PN, van der Meulen JH, Lewsey J, Gregg PJ (2007) The role of pain and function in determining patient satisfaction after total knee replacement. Data from the National Joint Registry for England and Wales. J Bone Joint Surg Br 89(7):893–900 [DOI] [PubMed]
- 22.Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35–43. doi: 10.1097/01.blo.0000238825.63648.1e. [DOI] [PubMed] [Google Scholar]
- 23.Scott CE, Bugler KE, Clement ND, MacDonald D, Howie CR, Biant LC. Patient expectations of arthroplasty of the hip and knee. J Bone Joint Surg Br. 2012;94(7):974–981. doi: 10.1302/0301-620X.94B7.28219. [DOI] [PubMed] [Google Scholar]
- 24.Polkowski GG, 2nd, Ruh EL, Barrack TN, Nunley RM, Barrack RL. Is pain and dissatisfaction after TKA related to early-grade preoperative osteoarthritis? Clin Orthop Relat Res. 2013;471(1):162–168. doi: 10.1007/s11999-012-2465-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meding JB, Ritter MA, Faris PM, Keating EM, Harris W. Does the preoperative radiographic degree of osteoarthritis correlate to results in primary total knee arthroplasty? J Arthroplasty. 2001;16(1):13–16. doi: 10.1054/arth.2001.16501. [DOI] [PubMed] [Google Scholar]