Abstract
Objective
To examine the secondhand smoke (SHS) exposure level in Chinese office buildings and to evaluate the effectiveness of a smoke-free policy in reducing SHS exposure.
Methods
Survey of smoking policies and measurement of SHS level in 14 office buildings from 10 provinces in China.
Results
Smoking in the building significantly elevated the SHS concentrations both in offices with at least one smoker and in offices with no smokers. In one building that recently adopted a smoke-free policy, the nicotine concentrations decreased significantly after the policy was enacted. Enactment of a smoking policy was effective in reducing SHS exposure in the buildings.
Conclusions
Nonsmoking office workers in China were exposed to significant levels of SHS at work; both the central and local governments should realize the need to legislate against workplace smoking.
“The Tobacco Monopoly Act of the People’s Republic of China” passed in 1991 requires that smoking should be banned or restricted in public places and on public transportation. “The Act for Protection of Minors” (1991) stipulates that no smoking is allowed in classrooms or dorms of middle schools, elementary schools, and kindergartens. In 1997, the central government drafted its first legislation that banned smoking in public transportation and its waiting areas.1 Many provinces and cities also passed their own regulations. In 1993, Suzhou of Jiangsu Province became the first city in the country to ban smoking in all public places. By October 2006, 46% of all cities in China had passed regulations banning smoking in public places. The coverage of these local regulations went beyond public transportation and associated waiting areas, which are stipulated by the national law, to encompass most of the public places, including cinemas, museums, shopping malls, pubs, hospitals, kindergartens, and schools.1
Compared with smoking in public places, workplace smoking has scarcely been mentioned in the law in China. There are cases of voluntary adoption of smoke-free policies at work, typically in certain professions, such as among health care institutions, but to date, there has been no regulation at any government level restricting workplace smoking in China. A typical worker spends 8 hours a day at work, and studies have shown that the work-place is one of the most important sources of secondhand smoke (SHS) exposure for nonsmokers.2,3 In 2005, China Center for Disease Control and Prevention (China CDC) proposed that all CDC offices, hospitals, and university hospitals around the country ban smoking in their premises. Some institutes already had a smoke-free policy in place before the proposal, and some others signed the proposal to adopt the policy. Nevertheless, China CDC has no administrative control over most of the institutes mentioned above. In the end, only a minority of the institutes signed the proposal, and most were left without a smoking policy. To investigate the degree to which such a smoke-free policy has achieved its desired goal of protecting the health of non-smokers at work, we compared the SHS level across fourteen health-related government buildings with different types of smoking policy. In one building where a smoke-free policy was recently enacted, we were also able to evaluate the policy by sampling the SHS concentration both before and after the policy implementation.
Materials and Methods
We conducted a survey of smoking policies among 38 attendees from two tobacco advertising workshops in China during December 2005. Each attendee represented either a central or a local government health institute. On the basis of the results of the policy survey, we recruited attendees from 14 institutes during the workshop for SHS sampling. The 14 institutes included nine local Centers for Disease Control and Prevention (CDCs) and five Health Education Institutes from 10 provinces. Seven of the institutes were in northern China and seven were in southern China. The attendee from each institute was trained in SHS sampling during the workshop. Samplers were distributed to attendees at the workshop and returned by mail after sampling was completed. All samples were exposed to the air for approximately 7 consecutive days between December 2005 and February 2006.
The average weekly concentration of SHS was measured with a passive monitor that samples nicotine; a filter treated with sodium bisulfate is held in a modified 4-cm-diameter polystyrene cassette, a membrane filter serves as a windscreen, and nicotine passively diffuses to the treated filter, where it is trapped; details are presented by Hammond et al4 and Hammond and Leaderer.5 The effective sampling rate is 24 mL/min. Samplers were attached to the ceiling or lamp by duct tape and were kept at a minimum distance of 50 cm from the nearest door or window, 15 cm below the ceiling, and 30 cm away from the wall. The collected nicotine was analyzed by gas chromatography with nitrogen selective detection.4,5 The laboratory analysis method had the sensitivity to detect 0.087 μg/m3 of nicotine in the air; nevertheless, the detection limit used in the current study was based on the mean ± 2 SD of the field blanks, which was 0.15 μg/m3. Only 27 of 395 samples were below the detection limit. Because nicotine level quickly drops to near zero after smoking stops, we used 40 hours instead of 168 hours as the sampling time to calculate the nicotine concentration to better reflect the true exposure level of a nonsmoking worker. Between 12 and 63 samples (median = 25) were collected per building. Approximately two thirds of all the samples were collected in offices, and the remainder was collected in hallways, lounges, stairways, men’s restrooms, lobbies, conference rooms, elevators, and one dining hall. None of the buildings in this study had a central HVAC (heating, ventilating, and air conditioning) system; they relied on windows for ventilation.
Two types of smoking policy were observed in the buildings we surveyed: smoke-free policies and restrictive smoking policies. A smoke-free policy is the one that bans smoking in all locations inside the building, whereas a restrictive policy allows smoking only in designated areas such as the smoking lounge. On January 1, 2006, one of the buildings in the survey that did not have a smoking policy before implemented a smoke-free policy. To evaluate the effectiveness of the policy, nicotine samples were collected both 1 week before and 2 months after the policy implementation. Sampling before and after implementation took place during the same season, so that the influence of outside temperature on air exchange rate (eg, open windows) was minimized.
Results
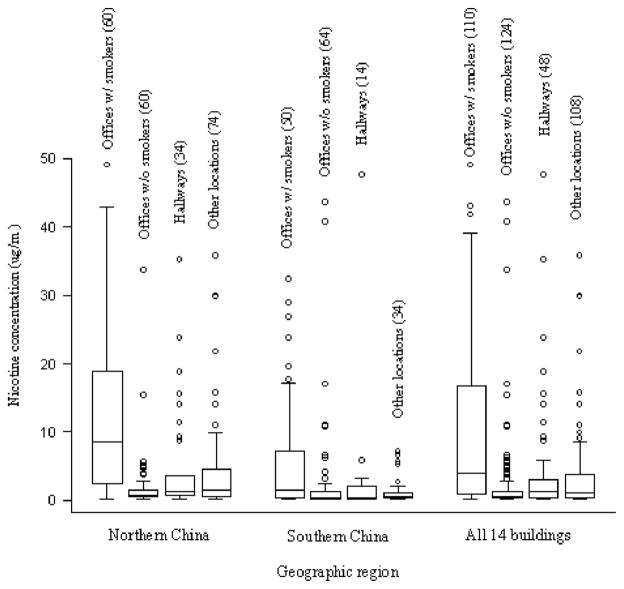
The nicotine concentrations in the 14 buildings ranged from below detection limit (<0.15 μg/m3) to 80.2 μg/m3 (one outlier 845.0 μg/m3 was excluded from the analysis). The median level for all 394 samples was 1.2 μg/m3. Significant nicotine concentrations were found in major locations inside the buildings (Fig. 1 and Table 1). For instance, 74% of the offices with at least one smoker had a concentration above 1.0 μg/m3 and 47% above 5.0 μg/m3. About 35% of the offices with only non-smokers and more than half of the hallway samples had concentrations above 1.0 μg/m3. Overall SHS exposure was found to be higher in buildings in northern China (Fig. 1). As all the samples were collected during winter, when windows are usually closed in northern China, and are often open in the south, the difference in air circulation from window status may have contributed to the higher nicotine concentrations observed in northern China.
Fig. 1.
Box plots of nicotine concentrations by location and geography (5 samples over 50 μg/m3 from offices with at least one smoker were not shown in the graph: 50.2, 56.4, 60.5, 80.2, and 84.5 μg/m3; the number of samples in each group is shown inside parentheses).
TABLE 1.
Summary Statistics of the Nicotine Sampling in 14 Office Buildings in China, Separated by Types of Smoking Policy and Sampling Locations
| Nicotine Concentration (3g/m3) | Buildings With a Smoke-Free or Restrictive Policy
|
Buildings With No Smoke-Free or Restrictive Policy
|
All 14 Buildings
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Offices With at Least One Smoker | Offices With No Smoker | All Offices | Entire Building | Offices With at Least One Smoker | Offices With No Smoker | All Offices | Entire Building | Offices With at Least One Smoker | Offices With No Smoker | All Offices | Entire Building | |
| Minimum | 0.24 | 0.08 | 0.08 | 0.08 | 0.08 | 0.08 | 0.08 | 0.08 | 0.08 | 0.08 | 0.08 | 0.08 |
| 10th percentile | 0.68 | 0.18 | 0.21 | 0.24 | 0.26 | 0.08 | 0.15 | 0.17 | 0.26 | 0.08 | 0.17 | 0.20 |
| 25th percentile | 1.19 | 0.29 | 0.35 | 0.38 | 0.75 | 0.25 | 0.38 | 0.37 | 0.85 | 0.27 | 0.35 | 0.37 |
| Median | 2.21 | 0.47 | 0.67 | 0.78 | 6.66 | 0.67 | 1.61 | 1.39 | 4.39 | 0.58 | 1.21 | 1.15 |
| Mean | 4.74 | 1.90 | 2.71 | 2.80 | 12.80 | 2.72 | 8.43 | 6.83 | 11.31 | 2.37 | 6.65 | 5.51 |
| 75th percentile | 4.98 | 1.16 | 1.88 | 1.96 | 18.82 | 1.93 | 10.99 | 6.84 | 17.25 | 1.36 | 6.48 | 4.75 |
| 90th percentile | 12.77 | 2.49 | 6.10 | 6.10 | 34.03 | 4.75 | 27.42 | 20.6 | 30.21 | 4.68 | 20.60 | 17.25 |
| Maximum | 29.91 | 43.66 | 43.66 | 47.63 | 80.16 | 40.80 | 80.16 | 80.16 | 80.16 | 43.66 | 80.16 | 80.16 |
| N | 21 | 53 | 74 | 129 | 93 | 71 | 164 | 265 | 114 | 124 | 238 | 394 |
| % of samples >1 μg/m3 | 81% (17) | 26% (14) | 42% (31) | 46% (59) | 73% (67) | 42% (30) | 59% (97) | 57% (152) | 74% (84) | 35% (44) | 54% (128) | 54% (211) |
| % of samples >5 μg/m3 | 24% (5) | 8% (4) | 12% (9) | 12% (15) | 54% (49) | 8% (6) | 34% (55) | 30% (79) | 47% (54) | 8% (10) | 27% (64) | 24% (94) |
Compared with the 10 buildings with no smoking policy, the four buildings with a smoke-free or a restrictive policy had lower concentrations of nicotine. Of the 14 buildings we sampled, two in northern China had a smoke-free policy, and two in southern China had a restrictive policy. The presence of a smoke-free policy or a restrictive policy was associated with considerably lower SHS concentration in offices (including both offices with at least one smoker and offices with no smoker) as well as in the entire building (Table 1). In buildings with a smoking policy, the median SHS level was 67% lower in offices with at least one smoker and 30% lower in offices with no smoker. When all the samples in the building were considered, the median level was 44% lower where there was a smoking policy. A similar effect of policy was also reflected in the percentages of samples with high concentrations (Table 1). When separately analyzed by geographic region, a smoking policy was found to be associated with lower SHS concentration inside the building in both northern and southern China. For all 14 buildings, offices in buildings with smoking policies had less than half SHS as offices without smoking policies.
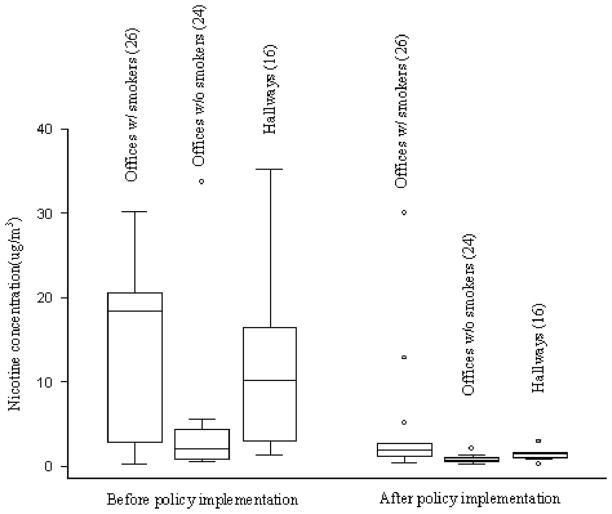
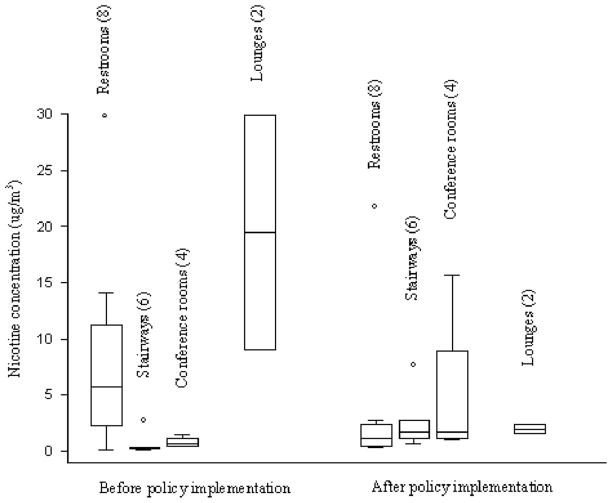
In one building where we sampled the air before and after a smoke-free policy was implemented on January 1, 2006, the SHS concentrations decreased significantly after the policy was enacted (for policy details, please refer to Appendix). Figures 2 and 3 compare the nicotine concentrations measured at the same locations before and after policy implementation. The average nicotine concentration in all offices decreased 80%, from 14.2 μg/m3 to 2.9 μg/m3 (the median declined from 4.8 μg/m3 to 1.2 μg/m3). An 86% decrease was also observed in hallway samples after the policy was enacted (Fig. 2 and Table 2). Figure 3 compares the nicotine concentrations measured before and after policy implementation from locations other than offices and hallways. The nicotine concentrations decreased in restrooms and lounges, but increased in lobby, stairways, conference rooms, and dining hall. One possible explanation for this nonuniform reduction of SHS concentration is that the smoke-free policy may have driven smokers to smoke in less noticeable locations, such as stairways.
Fig. 2.
Comparison of nicotine concentrations in offices and hallways before and after the implementation of smoke-free policy in an office building (2 samples above 40 μg/m3 from offices with at least one smoker before the implementation of the policy were not shown in the graph: 56.4 and 80.16 μg/m3; the number of samples in each location is shown inside parentheses).
Fig. 3.
Comparison of nicotine concentrations at locations other than offices and hallways in one building before and after the implementation of a smoke-free policy.
TABLE 2.
Comparison of the Mean and Median Nicotine Concentrations in an Office Building Before and After the Implementation of a Smoke-Free Policy
| Nicotine Concentration (μg/m3) | Locations With Decreased Nicotine Levels After the Policy
|
Locations With Increased Nicotine Levels After the Policy
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Offices With at Least One Smoker | Offices With No Smoker | Restrooms | Hallways | Lounges | Lobby | Stairways | Conference Rooms | Dining Hall | |
| Mean (prepolicy) | 22.30 | 4.89 | 8.50 | 11.97 | 19.47 | <0.15 | 0.62 | 0.78 | <0.15 |
| Mean (postpolicy) | 4.90 | 0.80 | 3.73 | 1.39 | 1.92 | 1.06 | 2.58 | 5.04 | 4.19 |
| Median (prepolicy) | 18.82 | 2.06 | 5.69 | 10.24 | 19.47 | <0.15 | 0.29 | 0.67 | <0.15 |
| Median (postpolicy) | 1.88 | 0.69 | 1.16 | 1.40 | 1.92 | 1.06 | 1.68 | 1.73 | 4.19 |
| Sample size | 13 | 12 | 8 | 8 | 2 | 1 | 6 | 4 | 1 |
We also surveyed the smoking behavior of the employees in each institute. Considering that the rate of smoking in women in the general public was only 4% and the rate among female health professionals would be even lower, we surveyed the smoking behavior among only male employees. Although the rate of smoking in men in most of the institutes was between 10% and 30%, much lower than the general public (>60%); five institutes had a smoking rate higher than 30%, including one institute where more than half of all the male employees were smokers.
Discussion
The two buildings with a smoke-free policy had a “Smoke-Free Workplace” sign posted at the entrance of the building as well as smoke-free signs posted inside the building. Incentives were offered to employees who quit smoking, and fines were issued to those who smoked inside the building. No ashtray was allowed anywhere in the building and the smoke-free policy also applied to visitors. There were no smoking rooms or smoking areas inside the building.
The two buildings with a partial smoking policy instead of a complete ban also had a “Smoke-free Work-place” sign posted at the entrance of the building as well as smoke-free signs posted inside the building. But, the policy was less strict in that there were no incentives for quitting or fines for smoking inside the building. The most notable difference is that both of these two buildings had ventilated smoking rooms or smoking areas inside the building.
Phillips et al6 sampled 145 office workers in Beijing using personal monitors and found that the median 24-hour average nicotine level was 0.8 μg/m3 for those who worked at office buildings that allowed smoking and 0.3 μg/m3 for those who worked at office buildings that did not. Because both groups of subjects lived in nonsmoking homes at the time of sampling, if one assumes the home nicotine concentration to be close to zero, the expected 8-hour average nicotine concentration at work would be 2.4 μg/m3 for those who worked at smoking office buildings and 0.9 μg/m3 for those who worked at nonsmoking office buildings. A similar study conducted in Hong Kong by the same group of authors7 found that the median concentration of nicotine was 0.5 μg/m3 for those who worked at office buildings where smoking was allowed and 0.1 μg/m3 for those who worked at office buildings where smoking was restricted. Similar levels of nicotine concentration were observed in our study; the median level was 1.2 μg/m3 for all 14 buildings combined and 1.4 μg/m3 for buildings without a smoking policy. That smoke-free policy reduces SHS concentration at the workplace was also observed by Hammond et al2 in US office buildings. After reviewing 22 previous studies that measured nicotine concentration in office settings, Hammond et al2 found that the presence of a restrictive smoking policy led to an 85% reduction and a smoke-free policy led to a 97% decrease in nicotine concentration.
Only four of the 14 buildings in our survey had a smoking policy. Because all 14 buildings in the current study were health-related government office buildings, where the smoking rate was much lower and the awareness of the health effects of smoking and passive smoking was much higher compared with the general public, we expect that fewer workplaces outside the health profession would have a smoking policy and the concentration of SHS exposure in the workplace would be higher. To illustrate the level of SHS one can be exposed to at work in the general public, we selected worksites in our survey that did not have a smoking policy and evaluated the situation of SHS exposure in various locations inside these building. We found that 59% of these offices had a nicotine concentration above 1.0 μg/m3 and 25% above 10.0 μg/m3. The average concentration was 8.4 μg/m3 in offices and 6.8 μg/m3 in the entire building; nevertheless, the smoking rate among men was lower among these health workers (~30%) than among the population at large (>60%), so SHS concentrations would be expected to be higher in most other office buildings. Repace et al8 estimated that 70% of non-smoking office workers in the United States were exposed to SHS at work in 1990, and that this occupational exposure caused 4800 deaths annually from heart disease (4400) and lung cancer (400). Assuming the same concentrations of SHS as in the United States and that virtually all office workers in China are exposed to SHS because smoking policies at work are rare in China, and also considering the fact that the size of non-farming employment population in China is three times larger than in the United States, SHS exposure in offices is associated with approximately 21,000 deaths each year in China.
Conclusion
Our study found that both smoke-free policies and restrictive smoking policies substantially reduced the SHS concentration in office buildings. Both types of policies were associated with reduced SHS level in offices as well as in the entire building. In the building where a smoke-free policy became effective recently, the SHS level decreased significantly as a result of the policy, especially in locations where non-smokers spent most of their time at work, eg, offices (75% decrease) and hallways (86% decrease).
Several countries in Europe have passed laws prohibiting workplace smoking and more countries are expected to follow.9–11 Many states in the United States have also banned smoking at work.12 To date, there are still no such laws or regulations at the governmental level in China and smoke-free policies at individual workplaces are rare. Despite the fact that China CDC proposed that all CDC offices, hospitals, and university hospitals around the country ban smoking in their premises, only 4 of 14 CDC buildings in the current survey had a smoking policy and none of the cities we surveyed had a city-wide policy regulating work-place smoking. A similar situation is expected in other cities that were not part of our survey. With clear evidence that workplace SHS is one of the most significant sources of tobacco smoke exposure and non-smoking workers are facing significant health risks from being exposed to SHS at work,13,14 both the central and local governments should pass legislation requiring smoke-free environments in all workplaces.
Acknowledgments
The authors thank the following colleagues at each participating local health institute for their help with the SHS sampling: Li Zhu, Liu Yanbing, Zhang Shouting, Jiang Ge, Tang Yuhui, Wang Yuejuan, Lu Jie, Qiu Wuqi, Su Shenghua, Chen Qi, Chang Ailing, Wang Xia, Guo Lijuan, Zhao Baifan, Nie Shaoping, Liang Xiaodong, Xue Yufeng, and Li Mingzhu.
Appendix
The detailed smoke-free policy at a local CDC in China:
Smoking lounges will be removed from the CDC premises and no smoking will be allowed anywhere inside CDC buildings.
No ashtray or display of cigarettes will be permitted inside offices; CDC employees should dissuade visitors from smoking inside the building.
CDC managers should set the example by quitting first.
CDC employees should encourage and support each other to quit smoking.
Penalty will be issued upon violation of the policy.
Divisions that closely follow the policy and individuals who have successfully quit will be awarded at the end of the year.
References
- 1.Cheng Y, Su Z. The Effect of WHO FCTC on the Development of Chinese Tobacco Industry. Beijing: Tobacco Economic Research Institute of Chinese Tobacco Monopoly; 2003. [Google Scholar]
- 2.Hammond SK. Exposure of U.S. workers to environmental tobacco smoke. Environ Health Perspect. 1999;107(suppl 2):329–340. doi: 10.1289/ehp.99107s2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hammond SK, Sorensen G, Youngstrom R, Ockene JK. Occupational exposure to environmental tobacco smoke. JAMA. 1995;274:956–960. [PubMed] [Google Scholar]
- 4.Hammond SK, Leaderer BP, Roche AC, Schenker M. Collection and analysis of nicotine as a marker for environmental tobacco-smoke. Atmos Environ. 1987;21:457–462. [Google Scholar]
- 5.Hammond SK, Leaderer BP. A diffusion monitor to measure exposure to passive smoking. Environ Sci Technol. 1987;21:494–497. doi: 10.1021/es00159a012. [DOI] [PubMed] [Google Scholar]
- 6.Phillips K, Howard DA, Bentley MC, Alvan G. Environmental tobacco smoke and respirable suspended particle exposures for non-smokers in Beijing. Indoor Built Environ. 1998;7:254–269. doi: 10.1007/s004200050296. [DOI] [PubMed] [Google Scholar]
- 7.Phillips K, Howard DA, Bentley MC, Alvan G. Assessment of environmental tobacco smoke and respirable suspended particle exposures for nonsmokers in Hong Kong using personal monitoring. Environ Int. 1998;24:851–870. doi: 10.1007/s004200050296. [DOI] [PubMed] [Google Scholar]
- 8.Repace JL, Jinot J, Bayard S, Emmons K, Hammond SK. Air nicotine and saliva cotinine as indicators of workplace passive smoking exposure and risk. Risk Anal. 1998;18:71–83. doi: 10.1111/j.1539-6924.1998.tb00917.x. [DOI] [PubMed] [Google Scholar]
- 9.Gallus S, Zuccaro P, Colombo P, et al. Effects of new smoking regulations in Italy. Ann Oncol. 2006;17:346–347. doi: 10.1093/annonc/mdj070. [DOI] [PubMed] [Google Scholar]
- 10.McElvaney NG. Smoking ban—made in Ireland, for home use and for export. N Engl J Med. 2004;350:2231–2233. doi: 10.1056/NEJMp048097. [DOI] [PubMed] [Google Scholar]
- 11.Howell F. Ireland’s workplaces, going smoke free. BMJ. 2004;328:847–848. doi: 10.1136/bmj.328.7444.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rigotti NA, Pashos CL. No-smoking laws in the United-States—an analysis of state and city actions to limit smoking in public places and workplaces. JAMA. 1991;266:3162–3167. doi: 10.1001/jama.266.22.3162. [DOI] [PubMed] [Google Scholar]
- 13.USDHHS. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Washington, DC: US Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2006. [Google Scholar]
- 14.CalEPA. Proposed Identification of Environmental Tobacco Smoke as a Toxic Air Contaminant. Sacramento, CA: California Environmental Protection Agency Air Resources Board and Office of Environmental Health Hazard Assessment; 2005. [Google Scholar]