Abstract
Objective:
Prospective evaluation of the efficacy and safety of the extracorporeal shock wave lithotripsy (SWL) and ureteroscopy with Holmium: YAG laser lithotripsy (URSL) as a primary treatment for impacted stone in the proximal ureter.
Patients and Methods:
A total of 82 patients with a single impacted stone in the proximal ureter were included in the study. Patients were allocated into two groups according to patient preference for either procedure. The first group included 37 patients who were treated by SWL and the second group included 45 patients treated by URSL. The preoperative data and treatment outcomes of both procedures were compared and analyzed.
Results:
There was no difference as regards to patient and stone characters between the two groups. There was significantly higher mean session number and re-treatment rate in the SWL group in comparison to URSL group (1.5 ± 0.8 vs. 1.02 ± 0.15 session, and 43.2% vs. 2.2%, respectively). At one month, the stone-free rate of the URSL group was statistically significantly higher than that of the SWL group (80% vs. 67.6%, respectively). The stone-free rate at three months was still higher in the URSL group, but without statistically significant difference (80.2% vs. 78.4%, respectively). There was no statistically significant difference in the rate of complications between the SWL and URSL (24.3% vs. 15.6%, respectively).
Conclusion:
Both procedures can be used effectively and safely as a primary treatment for impacted stone in the proximal ureter; however, the URSL has a significantly higher initial stone-free rate and lower re-treatment rate.
Keywords: Shock wave lithotripsy, laser lithotripsy, impacted stone
INTRODUCTION
With the advances in the technology of the extracorporeal shock wave lithotripsy (SWL) and different intracorporeal endoscopic procedures, about 95% of ureteral stones can be successfully treated by minimally invasive techniques.[1] Both SWL and ureteroscopy with Holmium: YAG laser lithotripsy (URSL) are the most effective treatment options in the management of proximal ureteral stones; however, both procedures are facing difficulties when the stone becomes impacted.[2,3] Impacted ureteral stone is one that remained unchanged in the same position for at least two months,[4,5] and the optimal treatment option in this situation is still controversial.[6] The impacted stones are more resistant to shock wave disintegration because of insufficient water-stone interface and lack of the natural expansion space around such stones.[7,8] These stones are frequently associated with distal lesions such as stricture or polyps that produce difficulty in ureteroscopic approach and decrease its working space.[2,9]
Many studies compared the outcome of SWL and URSL in management of proximal ureteral stone with respect to stone size; however, less number of studies compared both procedures when impaction is the main problem. In the current study, comparison between the two procedures in the management of this situation will be discussed.
PATIENTS AND METHODS
Between October 2007 and July 2011, a total of 82 patients were included in the study; they were selected from patients with ureteral stones who attended the urology outpatient clinic or the emergency department at Mubarak Al-Kabeer hospital in Kuwait. The inclusion criteria were the presence of impacted radio-opaque solitary stone <2 cm in the proximal ureter (the ureter distal to ureteropelvic junction up to the superior aspect of the sacroiliac joint). Patients with multiple stones, previous surgery or endoscopic maneuver of the ureter, previous SWL of a stone in the same ureter, congenital anomalies, coagulopathy, or renal insufficiency were excluded from the study.
The details of each procedure, and possible re-treatment, shift to other treatment, or complications had been explained to all patients before they decided on the preferred procedure. Written informed consents were taken from all patients. The patients were allocated into two groups. The first group included 37 patients who were treated by SWL and the second group included 45 patients who were treated by ureteroscopy with Ho: YAG laser lithotripsy (URSL).
All patients were assessed by a full clinical history, serum creatinine, blood urea nitrogen, bleeding profile, urine culture, and radiological investigations in the form of intravenous urography (IVU) or computed tomography (CT) urography, and ultrasonography. All patients with positive urine culture were treated by proper antibiotics before the procedures.
PROCEDURES OR PATIENTS AND METHODS
Shock wave lithotripsy
All patients were treated in the supine position by the same lithotripter (SIEMENS Lithostar Multiline). Treatment was started by a voltage of 11-12 kV, which then increased gradually till reaching to a maximum that could be tolerated by the patients. The session terminated if the stone fragmented on the screen or reached about 3,000 shocks. Patients were followed up after two weeks by KUB film and ultrasonography, if needed. If there was no or inadequate fragmentation observed, re-treatment was carried out in the same day of follow-up with a maximum of total three sessions. Patients were followed up by KUB films and ultrasonography, if needed, until they completed three months of follow-up.
Ureteroscopy with Ho: YAG laser lithotripsy (URSL)
All patients were treated under general anesthesia in lithotomy position under C-arm fluoroscopy. Ureteroscopy was carried out by an 8.6/9.8F semi-rigid ureteroscope (Olympus). After identification of the ureteric orifice, retrograde ureterography was performed to visualize the ureter distal to the stone. Retrograde placement of a floppy tip guidewire was tried to pass the stone, if possible, and then the ureteroscope was introduced into the ureteric orifice, and continuous irrigation was used to maintain clear vision. Stone disintegration was performed using Ho: YAG laser (LUMENIS, Versa Pulse Power Suite.100 watt) via a 550-nm Slim Line laser fiber (LUMENIS). The setting of the laser machine was adjusted to produce 0.2-0.8 Joules/pulse with a repetition rate (frequency) of 3-16 Hz.
At the end of procedure, a 6F ureteric catheter was placed for 24 hours or 6F double-J stent was placed if there was post-operative significant ureteral wall edema, minimal perforation, large residuals, or incomplete procedure. The double-J stent was removed after 4-6 weeks under local anesthesia if there were no residual fragments. Patients were followed up by KUB film on the first post-operative day, and then every month by KUB film and ultrasonography, if needed, up to three months.
Treatment outcome of both procedures was considered stone-free if no residual fragments were detected by imaging study after three months of follow-up. The data of each procedure were collected, tabulated, analyzed, and compared by statistical software (SPSS for Microsoft Windows, Version 17.0). P values were estimated and considered statistically significant if <0.05.
RESULTS
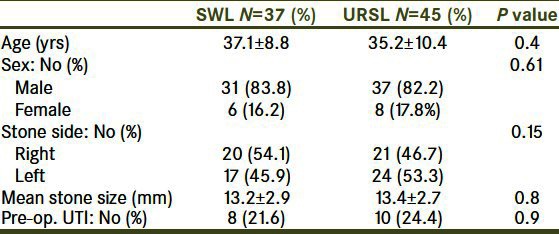
Patients and stone characters are presented in Table 1. There was no statistically significant difference between the SWL and URSL groups as regards to patients’ age and sex, mean stone size, stone side, and pre-operative urinary tract infection (UTI). In the SWL groups, the mean age was 37.1 ± 8.8 years versus 35.2 ± 10.4 years in the URSL group. In the SWL group, 83.8% were male and 16.2% were female, and in the URSL group, 82.2 % were male and 17.8% were female. Mean stone size was 13.2 ± 2.9 mm in the SWL group and 13.4 ± 2.7 mm in the URSL group.
Table 1.
Patients and stones characters
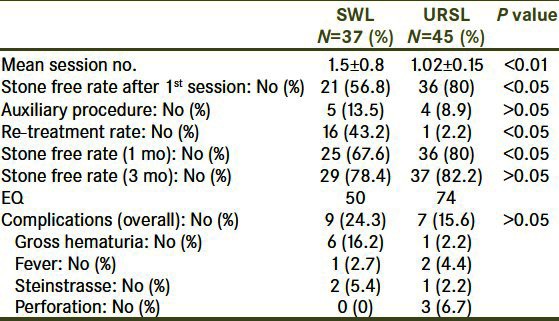
SWL was the primary procedure in 37 patients. The mean number of sessions and shock waves applied for the patients were 1.5 ± 0.8 session and 4281.1 ± 2411.6 shock waves, respectively. Twenty-one patients (56.8%) became stone-free after the first session. Five and three patients became stone-free after the second and third session, respectively. The re-treatment rate was 43.2%. The stone-free rate was 67.6% at one month, and it increased to 78.4% at three months of follow-up. Stone failed to be fragmented in eight patients (21.6%); five of them were managed later by URSL, and the remaining three patients managed by laparoscopic ureterolithotomy. Six (16.2%) patients developed hematuria that was managed conservatively; two patients (5.4%) were complicated by steinstrasse and managed by URSL, and one patient (2.7%) had febrile UTI that necessitated hospitalization and intravenous antibiotic. The calculated efficacy quotient (EQ) for the procedure was 50.
URSL was the primary procedure in 45 patients. Failure to reach the stone occurred in four (8.9%) patients due to tortuous ureter and impassable stricture distal to the stone; three of them were managed later by laparoscopic ureterolithotomy and the fourth one by open ureterolithotomy. Stone was pushed back during the procedures in two (5.4%) cases that were managed successfully after that by SWL. Large residual fragments remained in four (8.9%) patients. One of them passed the residual stone after five weeks from the URSL with the aid of conservative treatment; two patients were managed by SWL and the last one developed steinstrasse that was managed successfully again by URSL. The re-treatment rate and EQ of the URSL was 2.2% and 74, respectively. The stone-free rate at one month was 80%, which slightly increased to 82.2% in three months. Minimal ureteral perforation was seen in three (6.7%) patients and managed by placement of ureteric double-J stents, prolonged postoperative hematuria for five days in one (2.2%) case, and postoperative fever in two (4.4%) cases. Comparison of the outcome of the two procedures is presented in Table 2.
Table 2.
Features and outcome of treatment
DISCUSSION
The optimal management of impacted stone in the proximal ureter is still controversial with no established guidelines for the treatment of choice.[9–11] The dilemma is to choose between the two most commonly used procedures in treating ureteral stone—SWL and ureteroscopy.[12]
Impacted stone is defined as the stone that has remained in the same position for at least two months with failure in visualization of the contrast material in the ureter distal to the stone. Failure of retrograde passage of a guidewire beyond the stone is sometimes present with impaction; however, this is due to the transient lie of the stone.[2,4,5]
In the current study, the criteria of impaction were failure of visualization of the ureter distal to a proximal ureteral stone in IVU or CT urography, with a radiological investigation confirmed the presence of the stone in the same position since two months, if possible, or presence of symptoms for two months. In all patients who underwent URSL, there was failure to pass the stone by the guidewire.
In the current study, the patient and stone characters were homogenous. There was no statistically significant difference between the two groups with regard to age and sex of patients, mean stone size, stone side, and pre-operative UTI; this minimized the effect of any of them on the outcomes of the procedures.
The mean number of sessions in the SWL group was statistically significantly higher than that of the URSL group, (1.5 ± 0.8 vs. 1.02 ± 0.15, respectively, P < 0.01) and stone-free rate after one session was significantly higher in the URSL group in relation to the SWL group (80% vs. 56.8%, respectively, P < 0.05). In the study by Wu et al.,[13] the stone-free rate of large proximal ureteral stone after one session of URSL was 92.3% in comparison to 61% after one session of SWL, which is comparable to results of the current study.
The initial stone-free rate of SWL in management of proximal ureteral stone is decreased when the stone is either larger or impacted with a concomitant increase in the number of treatment sessions. In the study by Karlsen et al.,[14]82% of patients who had 5-10 mm proximal ureteral stone became stone-free after one session of SWL, while in the study by Ziaee et al.,[15] the stone size was in the range of 10-15 mm and the stone-free rate of SWL after one session was in the range of 73.3-80.2%, with a 1.2 mean number of session; this rate decreased sharply when the stone was impacted as in the study of Ghoneim et al.[16] to be 28.3%, with a mean session number in the range of 1.97-2.0 sessions. Although the impacted stone usually needs more than one session of SWL to be fragmented, it is believed that the obstruction is relieved after the first session due to partial disintegration of the stone.[16]
With increasing size of the stone in the proximal ureter and presence of impaction, the re-treatment rate became significantly higher in SWL in comparison with URSL. The study by Karlsen et al.[14] compared both procedures for the management of small-sized stones in the proximal ureter (5-10 mm), and re-treatment rate was found to be 18% for both. In the study by Fong et al.,[17] the stone size was larger and measured 5-35 mm, and the re-treatment rate was significantly higher in SWL group than in the URSL group of patients (14% vs. 2%, respectively). In case of impacted stone, the re-treatment rate of SWL is sharply increased to be more than 60%.[16] The previous results matched to a large degree with results in the current study, as the re-treatment rate was statistically significantly higher in the SWL group in comparison to URSL group (43.2% vs. 2.2%, respectively).
This higher re-treatment rate of SWL in managing large and impacted proximal ureteral stone is one of the factors that make it the least preferred primary treatment modality in such situations.[15,18] The cause of re-treatment in URSL is post-laser lithotripsy steinstrasse that developed in distal position.[19] In the current study, this was the cause of re-treatment in the URSL group; it was observed that the significant lower re-treatment rate of URSL in case of impacted stone was due to shift to another treatment rather than re-treatment. This was because most of the unsuccessful procedures were due to failure to reach the stone or pushback of the stone rather inadequate fragmentations as in SWL.
The initial stone-free rate of URSL in the management of proximal ureteral stone is generally higher than that of SWL; however, with a longer duration of follow-up, there is more increase in the stone-free rate of SWL and the difference between the two procedures became less.[15,20] In the current study, the initial stone-free rate after one month of the URSL group was statistically significantly higher than that of the SWL group (80% vs. 67.6%), after three months of follow-up, the stone-free rate increased in both groups to be 82.2% in the URSL group and 78.4% in the SWL group. Although the stone-free rate after three months was still higher in the URSL group, but it was without statistically significant difference. These results match to a large degree with the results of Fong et al.[17] who found the one-month stone-free rates of URSL and SWL were 80% and 50%, respectively, with significant difference; however, after three months of follow-up the stone-free rates were 90% for URSL and 78% for SWL and the difference was insignificant.
The EAU/AUA Nephrolithiasis Guideline Panel, 2007, for the management of ureteral calculi recommended both ureteroscopy and SWL as acceptable first-line treatment modalities for treating ureteral stone >1 cm. The guidelines also showed that the stone-free rate of a stone >1 cm in the proximal ureter was in the range of 55-79% with SWL and 71-87% with ureteroscopy.[21] Since this report, many studies were conducted to evaluate the two procedures in the management of proximal ureteral stones but with more precise characters, one of these characters is the presence of impaction.
In the study by Ghoneim et al.,[16] they reported a stone-free rate of SWL in the management of impacted proximal ureteral stone to be 90% and 86.7% in the stented and non-stented group of patients, with an overall stone-free rate of 88.3%. For the same situation, Sun et al.[9] reported the stone-free rate of URSL as 86.4%. In the study by Juan et al.,[10] they reported a stone-free rate of URSL to be 58%, and this relatively lower rate might be due to a larger stone size cutoff set in this study (>1.5 cm).
In the current study, the complication rate of the SWL and URSL groups was 24.3% and 15.6%, respectively, with no statistically significant difference between the two groups.
URSL is considered as a safe and effective technique with a very low incidence of major complications.[22] Although ureteral perforation is one of the most common and serious complications of ureteroscope, but with the use of laser lithotripsy, the risk of perforation becomes less because the depth of thermal effect is 0.5-1 mm.[11,12,23] The rate of perforation in proximal ureteral stone is in the range of 3-9%; however, this rate is steadily decreasing with the improvement in technology and technique.[12,21] Another less serious reported complications are gross hematuria (12-22.6%), fever (5-6.5%), steinstrasse (0-2%), and stricture (1-5%).[10,11,15,21,22] The reported complications in the URSL group in the current study were perforation (6.7%), gross hematuria (2.2%), fever (4.4%), and steinstrasse (2.2%), which were comparable to previously mentioned results.
SWL is the least invasive modality in treating proximal ureteral stones, but it is not free from complications.[24] The most common complications associated with SWL are gross hematuria (8-9%), fever (0.8-4%), and steinstrasse (2-10%).[12,14–16,21] In the current study, the reported complications in the SWL group were hematuria (16.2%), fever (2.7%), and steinstrasse (5.4%), which matched to a great extent to the previous results.
The limitation of the current study is the relatively small number of patients; however, it was due the strict inclusion criteria of the study for the selection of an actually impacted stone.
CONCLUSION
Both URSL and SWL enable an effective and safe primary treatment option for the impacted stone in the proximal ureter. The URSL has a significant higher initial stone-free rate; however, after three months of follow-up, the stone-free rate of SWL has been further increased and the difference between the two procedures becomes insignificant. Although SWL has a significantly higher re-treatment rate and lower initial stone-free rate, it has the advantage of being non-invasive and outpatient procedure with absence of anesthesia.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Tunc L, Kupeli B, Senocak C, Alkibay T, Sözen S, Karaoglan U, et al. Pneumatic lithotripsy for large ureteral stones: Is it the first line treatment? Int Urol Nephrol. 2007;39:759–64. doi: 10.1007/s11255-006-9084-7. [DOI] [PubMed] [Google Scholar]
- 2.Mugiya S, Ito T, Maruyama S, Hadano S, Nagae H. Endoscopic features of impacted ureteral stones. J Urol. 2004;171:89–91. doi: 10.1097/01.ju.0000100960.08768.81. [DOI] [PubMed] [Google Scholar]
- 3.Kanno T, Shichiri Y, Oida T, Yamamoto M, Kanamaru H, Takao N, et al. Extraperitoneal laparoscopic ureterolithotomy in the supine position for impacted ureteral stones. Urology. 2006;67:828–9. doi: 10.1016/j.urology.2005.10.032. [DOI] [PubMed] [Google Scholar]
- 4.Deliveliotis C, Chrisofos M, Albanis S, Serafetinides E, Varkarakis J, Protogerou V. Management and follow-up of impacted ureteral stones. Urol Int. 2003;70:269–72. doi: 10.1159/000070133. [DOI] [PubMed] [Google Scholar]
- 5.Morgentaler A, Bridge SS, Dretler SP. Management of the impacted ureteral calculus. J Urol. 1990;143:263–6. doi: 10.1016/s0022-5347(17)39928-7. [DOI] [PubMed] [Google Scholar]
- 6.Binbay M, Tepeler A, Singh A, Akman T, Tekinaslan E, Sarilar O, et al. Evaluation of pneumatic versus holmium: YAG laser lithotripsy for impacted ureteral stones. Int Urol Nephrol. 2011;43:989–95. doi: 10.1007/s11255-011-9951-8. [DOI] [PubMed] [Google Scholar]
- 7.Mugiya S, Nagata M, Un-No T, Takayama T, Suzuki K, Fujita K. Endoscopic management of impacted ureteral stones using a small caliber ureteroscope and a laser lithotriptor. J Urol. 2000;164:329–31. [PubMed] [Google Scholar]
- 8.Mugiya S, Ozono S, Nagata M, Takayama T, Nagae H. Retrograde endoscopic management of ureteral stones more than 2 cm in size. Urology. 2006;67:1164–8. doi: 10.1016/j.urology.2006.01.088. [DOI] [PubMed] [Google Scholar]
- 9.Sun X, Xia S, Lu J, Liu H, Han B, Li W. Treatment of large impacted proximal ureteral stones: Randomized comparison of percutaneous antegrade ureterolithotripsy versus retrograde ureterolithotripsy. J Endourol. 2008;22:913–7. doi: 10.1089/end.2007.0230. [DOI] [PubMed] [Google Scholar]
- 10.Juan YS, Shen JT, Li CC, Wang CJ, Chuang SM, Huang CH, et al. Comparison of percutaneous nephrolithotomy and ureteroscopic lithotripsy in the management of impacted, large, proximal ureteral stones. Kaohsiung J Med Sci. 2008;24:204–9. doi: 10.1016/S1607-551X(08)70118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manohar T, Ganpule A, Desai M. Comparative evaluation of Swiss Litho Clast 2 and holmium: YAG laser lithotripsy for impacted upper-ureteral stones. J Endourol. 2008;22:443–6. doi: 10.1089/end.2007.0288. [DOI] [PubMed] [Google Scholar]
- 12.Matlaga BR, Lingeman JE. Surgical management of upper urinary tract calculi. In: Wein AJ, Kavoussi LR, Partin AW, Novick AC, Peters CA, editors. Campbell-Walsh Urology. 10th ed. Philadelphia: Elsevier Saunders; 2012. pp. 1357–1410. [Google Scholar]
- 13.Wu CF, Shee JJ, Lin WY, Lin CL, Chen CS. Comparison between extracorporeal shock wave lithotripsy and semirigid ureterorenoscope with holmium: YAG laser lithotripsy for treating large proximal ureteral stones. J Urol. 2004;172:1899–902. doi: 10.1097/01.ju.0000142848.43880.b3. [DOI] [PubMed] [Google Scholar]
- 14.Karlsen SJ, Renkel J, Tahir AR, Angelsen A, Diep LM. Extracorporeal shockwave lithotripsy versus ureteroscopy for 5- to 10-mm stones in the proximal ureter: Prospective effectiveness patient-preference trial. J Endourol. 2007;21:28–33. doi: 10.1089/end.2006.0153. [DOI] [PubMed] [Google Scholar]
- 15.Ziaee SA, Halimiasl P, Aminsharifi A, Shafi H, Beigi FM, Basiri A. Management of 10-15-mm proximal ureteral stones: Ureteroscopy or extracorporeal shockwave lithotripsy? Urology. 2008;71:28–31. doi: 10.1016/j.urology.2007.08.025. [DOI] [PubMed] [Google Scholar]
- 16.Ghoneim IA, El-Ghoneimy MN, El-Naggar AE, Hammoud KM, El-Gammal MY, Morsi AA. Extracorporeal shock wave lithotripsy in impacted upper ureteral stones: A prospective randomized comparison between stented and non-stented techniques. Urology. 2010;75:45–50. doi: 10.1016/j.urology.2009.06.071. [DOI] [PubMed] [Google Scholar]
- 17.Fong YK, Ho SH, Peh OH, Ng FC, Lim PH, Quek PL, et al. Extracorporeal shockwave lithotripsy and intracorporeal lithotripsy for proximal ureteric calculi-a comparative assessment of efficacy and safety. Ann Acad Med Singapore. 2004;33:80–3. [PubMed] [Google Scholar]
- 18.Yu W, Cheng F, Zhang X, Yang S, Ruan Y, Xia Y, et al. Retrograde ureteroscopic treatment for upper ureteral stones: A 5-year retrospective study. J Endourol. 2010;24:1753–7. doi: 10.1089/end.2009.0611. [DOI] [PubMed] [Google Scholar]
- 19.Chen CS, Wu CF, Shee JJ, Lin WY. Holmium: YAG Lasertripsy with semirigid ureterorenoscope for upper-ureteral stones >2 cm. J Endourol. 2005;19:780–4. doi: 10.1089/end.2005.19.780. [DOI] [PubMed] [Google Scholar]
- 20.Papadoukakis S, Stolzenburg JU, Truss MC. Treatment strategies of ureteral stones. Eur Urol Supplements. 2006;4:184–190. http://www.journals.elsevierhealth.com/periodicals/eeus/article/S1871.2592 (06)00045-1 . [Google Scholar]
- 21.Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck C, Gallucci M, et al. 2007 guideline for the management of ureteral calculi. J Urol. 2007;178:2418–34. doi: 10.1016/j.juro.2007.09.107. [DOI] [PubMed] [Google Scholar]
- 22.Nuttall MC, Abbaraju J, Dickinson IK, Sriprasad S. A review of studies reporting on complications of upper urinary tract stone ablation using the holmium: YAG laser. Br J Med and Surg Urol. 2010. pp. 3151–159. http://www.bjmsu.com/article/S1875-9742%2810%2900026-1 .
- 23.Jiang H, Wu Z, Ding Q, Zhang Y. Ureteroscopic treatment of ureteral calculi with holmium: YAG laser lithotripsy. J Endourol. 2007;21:151–4. doi: 10.1089/end.2006.0209. [DOI] [PubMed] [Google Scholar]
- 24.Lam JS, Greene TD, Gupta M. Treatment of proximal ureteral calculi: Holmium: YAG laser ureterolithotripsy versus extracorporeal shock wave lithotripsy. J Urol. 2002;167:1972–6. [PubMed] [Google Scholar]


