Abstract
Objective:
To investigate the role of dietary patterns in prevention and management of type 2 diabetes mellitus.
Materials and Methods:
A systematic review of databases which were published in ISI, Cochrane Central Register of Controlled Trials databases, PubMed, Iran Medex, and MagIran was performed. “Diabetes” and “dietary pattern” were used as the keywords.
Results:
A total of 58 studies which aimed to focus on diabetes mellitus, insulin resistance, metabolic syndrome, dietary pattern, and other related key words were reviewed. More than 47,447 articles were found and 46,709 entries of the extracted studies were excluded on the basis of the title and abstracts. The major dietary patterns were: “Healthy”, “Western”, “Traditional”, “Prudent”, “Unhealthy”, “Mediterranean”, “Modern”, and “Dietary Approach to Stop Hypertension” (DASH) diets. Comparison of the effects of different diets revealed that dietary patterns containing fiber-rich foods have a protective role in managing diabetes mellitus. “Healthy”, “Mediterranean”, “Prudent”, and “DASH” dietary patterns were associated with lower risk of hyperglycemia.
Conclusions:
The adherence to the Mediterranean, Prudent, or DASH diets could control hyperglycemia. The higher intake of vegetables, fruits, nuts, whole grains, and lower intake of red meat could reduce the risk of type 2 diabetes mellitus.
Keywords: Dietary pattern, glycemic control, Healthy dietary pattern, Mediterranean dietary pattern, Prudent dietary pattern, type 2 diabetes mellitus, Western dietary pattern
INTRODUCTION
Diabetes mellitus (DM) is a popular lifelong metabolic disease, and probably will remain the most frequent cause of death in the following decades.[1] Diabetes as a concerned epidemic problem is increasing all over the world.[2–10] Statistical estimations show that the number of diabetic individuals will be 65% of the world population (380 millions) by 2025.[11] The prevalence of this disease will become about twofold in the coming 20 years.[12] The prevalence of DM is as much as nearly 5% of the world population[12] and it has doubled during the recent 20 years.[13] It is the fifth cause of death in the USA[14] and one of the four causes of non-communicable disorders in different age groups.[15] Asian countries also have high prevalence of diabetes. Incidence rate of 10.6 per 1000 persons was observed in an Iranian survey.[16] Data show that almost 15–20% of population in different areas may have either DM or impaired glucose tolerance (IGT) in 2025.[12] Lifestyle modification could reduce the risk of diabetes by 30–67%, and surprisingly, this reduction maintains even after removing the lifestyle modifications.[16,17] Lifestyle modification can decrease diabetes risk by about 58% among subjects with IGT. These modifications consist of physical activity and changes in dietary habits, which are 27% more useful than taking various medications. Most of the assessments revealed that broad preventive population-based strategies are critical to challenge the pandemic of DM.[18] DM is a multi-factorial disorder in which both genetic and environmental factors have major roles.[18,19] Besides urbanization and technology development, the rapid nutritional and lifestyle transition faced by us doubles the burden of diseases. Poor quality of diet and nutritional habits have potential effects on the obesity-based chronic diseases.[2,20–23] Diet has a major role in preventing and managing hyperglycemia and DM.[1,24,25] Previous focus of nutrition science was on the amount and distribution of nutrients and food components. However, this approach has been replaced by a focus on a combination of nutrients and considering foods and food components together. Different unknown components and various interactions of food components provide the idea of focusing on dietary patterns instead of food components or nutrients.[26,27] Dietary pattern approach helps in assessing the entire diet,[27] which is also more understandable compared to just focusing on nutrient- or food-based approach to make recommendation for population.[28] Dietary pattern as a new focus in nutritional epidemiology is a suitable approach that covers biological native interactions of nutrient components in different food groups in relation with various disorders. Dietary pattern reflects an individual's food consumption and its change during the life span,[29,30] so it provides comprehensive information about dietary habits and identifies more effective recommendations to manage different chronic diseases. The complex interactions are shown in numerous dietary patterns such as “Mediterranean,” Dietary Approaches to Stop Hypertension (DASH), “Prudent,” “Western,” “Traditional,” and “Healthy” dietary patterns.[26]
Therefore, we aimed to assess the relationship between different dietary pattern and the prevalence of type 2 DM and also assess the effect of different eating habits on managing type 2 DM in this review paper.
MATERIALS AND METHODS
We reviewed all the study designs (prospective cohort study, clinical trials, cross-sectional studies) and focused on the available sources between 1992 and 2011, including journals, electronic books, seminars, and symposium contexts. The search focused on databases published in Cochrane Central Register of Controlled Trials databases, PubMed, Iran Medex, and MagIran using the keywords: Diabetes mellitus, insulin resistance, metabolic syndrome, and dietary pattern. We also studied food, insulin resistance (IR), fasting blood glucose (FBG), and Homeostasis Model Assessment of Insulin Resistance (HOMA-IR) as the basic related features of DM[26] and metabolic syndrome.[27] The relevance of surveys was found with a hierarchical approach on the basis of titles, abstracts, and full text of articles. Our search was limited to English materials We excluded letters, and studies focusing on single nutrients and food items, children, adolescents, and animal studies. The information had been summarized based on fixed protocol: Lead author, country, year of publication, sample size, sex and age of subjects, assay method, follow-up duration, outcome measure, race/ethnic, dietary pattern, effect size measurements [odds ratio (OR)/relative risk], and confounding factors adjustments.
In the initial search, we found more than 569 articles in PubMed on DM and dietary pattern, 23,296 entries on DM and diet, 344 articles on dietary pattern and IR, 10,359 entries on diet and IR, and 12,879 articles on DM and food. After scanning the articles, 46,709 of the extracted studies were excluded on the basis of the title, abstract, and their major purposes which were limited to the single nutrients and food items.
RESULTS AND DISCUSSION
Mediterranean dietary pattern
This food habit emphasizes on good source of monoun-saturated fatty acids (MUFA) from olive oil, accompanied with intake of vegetables, nuts, seeds, fruits, and whole grains, and reduction in the consumption of red meat and unhealthy fats. High content of fiber, magnesium, polyphenol, and antioxidants makes this diet as a useful approach to control hyperglycemia and weight maintenance.[28,31,32]
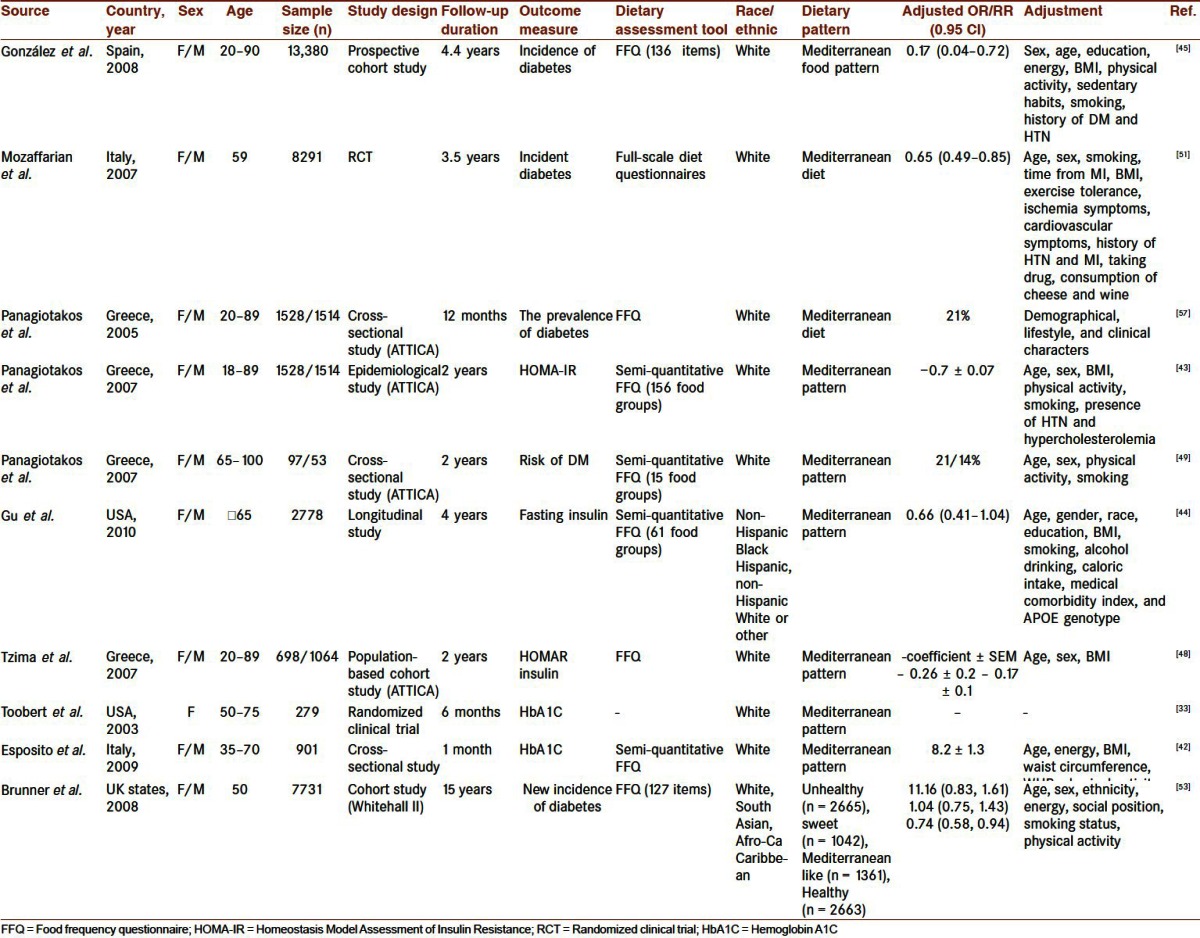
The results of a large Spanish cohort study among 13,380 men and women showed that adherence to the Mediterranean diet could decrease the risk of type 2 DM by 83%.[33] This inverse association between Mediterranean dietary pattern and the prevalence of type 2 DM was observed in various multiethnic studies. Several epidemiological studies explained lower odds of having DM[34] and inverse relation between glucose level,[35–37] insulin,[31–39] and HOMA-IR (as one of the basic features of metabolic syndrome and type 2 DM)[31,33,36,40–42] following adherence to the Mediterranean dietary pattern even after controlling different confounding agents.[43–48] Higher adherence to the Mediterranean dietary pattern score in normoglycemic persons decreased fasting glucose, insulin, and IR. However, this reduction was not significant after multiple adjustments were made for diabetic patients and subjects with impaired fasting glucose (IFG).[43] The aforementioned findings are observed in elderly group[49] and high-risk persons with cardiovascular risk factors and in also those with history of myocardial infarction.[31,50–52] Another cohort study on 7751 subjects in different ethnics compared four dietary patterns: 1. “Mediterranean-like diet” containing rice, pasta, vegetables, fruits, and wine; 2. “Healthy pattern” that includes whole bread, fruits, vegetables, low-fat dairies, and little alcohol; 3. “Sweet pattern” rich in white bread, processed meat, and high-fat dairy products; and 4. “Unhealthy eating pattern” high in white bread, processed meat, fries, and full-cream milk. Results showed that healthy diet is the best pattern in lowering the incidence of DM.[53] Panagiotakos et al. observed a lower OR of diabetes among Greek adults with high score of adherence to the Mediterranean dietary pattern.[54] The comparison of the effects of “Mediterranean hypocaloric” diet and “very-low-carbohydrate hypocaloric” diet on fasting plasma glucose, serum insulin level, and insulin 2 h post-load concentration and HOMA-IR did not show a significant difference even after 8 weeks weight loss in obese women.[55] A longitudinal clinical trial for 54 months revealed that consuming a Mediterranean diet could decrease HOMA-IR and serum glucose and serum insulin levels in persons with metabolic syndrome.[56] As patients with metabolic syndrome are at high risk for developing type 2 diabetes, following the Mediterranean diet can have a protective effect in this regard. Table 1 shows the different studies which evaluate the effects of “Mediterranean” dietary pattern on type 2 DM.
Table 1.
Characteristics of various studies that evaluated the effects of “Mediterranean” dietary pattern on diabetes mellitus type 2
Prudent and Western dietary pattern
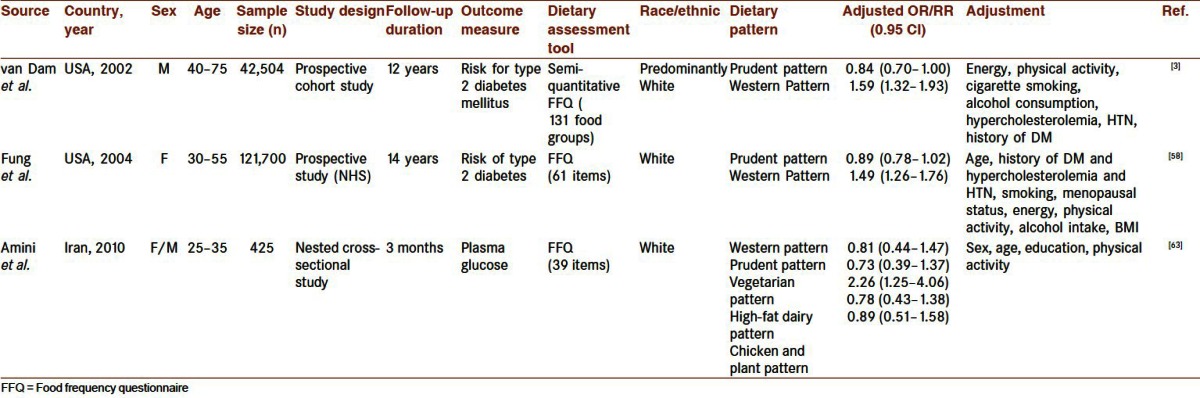
Several studies have focused on the association between lower risk of type 2 DM and adherence to the “Prudent pattern.” Prudent pattern is another dietary pattern which is characterized by higher consumption of whole grains, vegetables, fruits, poultry/sea foods, legumes, and coffee.[3,58,59] In an American prospective cohort study among 42,504 men, higher adherence to the Prudent pattern reduced the risk of DM by 16%, however, after 12 years of follow-up. However, “Western dietary pattern” increased the risk to almost 60%.[3] Western dietary pattern contains red and processed meat, butter, French fries, refined grains, deserts, potatoes, sweets, high-fat dairy, and soda.[3,58,59] The results were similar to the findings of the “Atherosclerosis Risk in Communities (ARIC)” study[60] and al so, the observations of Fung et al. in the Nurses’ Health Study (NHS) following 12 years.[58] In another study, the “Conservative” and “Prudent” patterns were compared. “Conservative” eating pattern, which contains butter, potatoes, and whole milk, has been correlated positively with the risk of diabetes by 50% while adherence to the “Prudent” dietary pattern reduced this risk by 28%.[59] Two cross-sectional studies of Villegas et al. defined usual dietary pattern of adults in three clusters, which correspond to “Traditional,” “Prudent,” and “Alcohol and convenience” diets. “Traditional” pattern had high percent of fat in total calorie intake; predominantly fat intake was in the forms of saturated fatty acids (SFA) and MUFA, in contrast to “Prudent” diet which was characterized as a pattern rich in polyunsaturated fatty acids (PUFA), high P/S ratio, fiber, and antioxidant vitamin sources. “Alcohol and convenience” diet included the highest intake of alcohol, protein, cholesterol, vitamin B-complex, iron, phosphorus, selenium, zinc, and the lowest amount of PUFA and antioxidant vitamins. Analysis showed the lowest IR and hemoglobin A1C (HbA1C) level in subjects adhering to the “Prudent dietary pattern.”[61,62] An Iranian nested cross-sectional study among 425 subjects with IGT (25–35 years old) showed the association between plasma glucose as one of the major features of metabolic syndrome and five eating patterns: 1. “Western” pattern (rich in sweets, butter, soda, mayonnaise, sugar, cookies, tail of a lamb, hydrogenated fat, and eggs); 2. “Prudent” pattern (contains fish, peas, honey, nuts, juice, dry fruits, vegetable oil, liver and organic meat, and coconuts); 3. “vegetarian” pattern (includes potatoes, legumes, fruits, rice, green leafy vegetables, and fruits); 4. “high-fat dairy” pattern (high in fatty dairies); and 5. “chicken and plant” pattern (rich in chicken, fruits, green leafy vegetables, and mayonnaise). After controlling various confounding factors, results revealed that “vegetarian” diet can reduce blood glucose level significantly.[63] Different studies that assessed the effects of “Prudent” and “Western” patterns among type 2 DM are shown in Table 2.
Table 2.
Characteristics of various studies that evaluated the effects of “Prudent” and “Western” dietary patterns on diabetes mellitus type 2
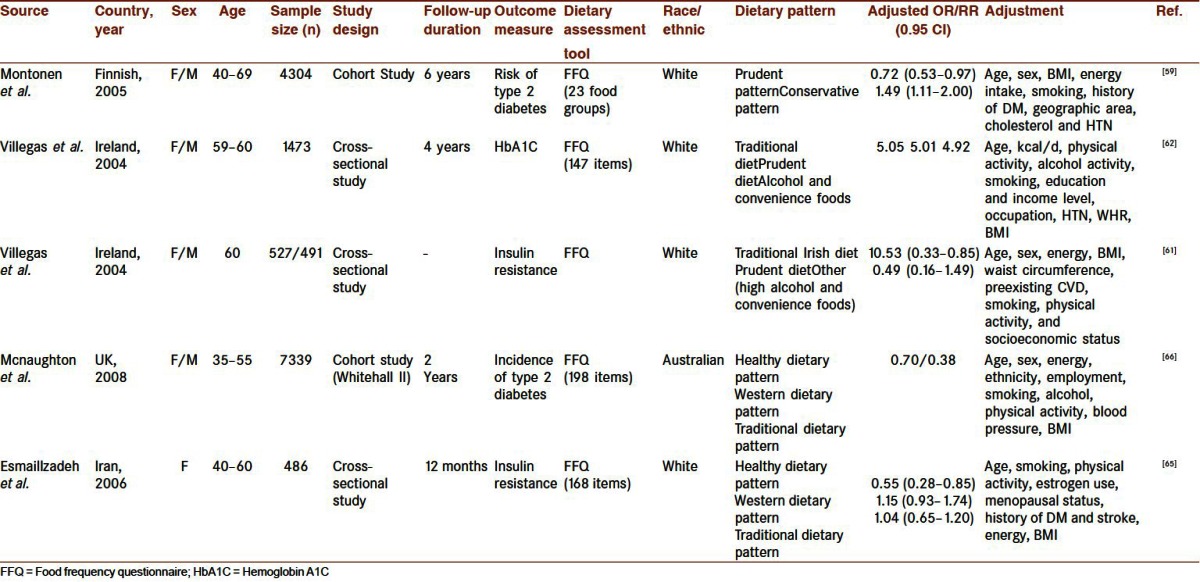
“Healthy,” “Western,” and “Traditional” dietary patterns
Food items of similar dietary patterns are different, based on geographic and ethnic characters. “Traditional” pattern is characterized by higher consumption of refined grains, potato, tea, whole grains, hydrogenated fats, legumes, and casserole,[64] or it can be defined as a pattern rich in high-fat sandwich spreads, red meat, potatoes, butter and lard, low-fat fish, sandwich meat, and sauces.[65] Healthy diet usually contains higher intake of whole meal bread, fruit and vegetables, and polyunsaturated margarine, besides lower consumption of red meat, sweet foods, and wine and beer,[53] or food rich in fruits, vegetables, tomato, poultry, legumes, tea, fruit juices, and whole grains.[66]
Pattern rich in red meat, processed meat, French fries, high-fat dairy products, refined grains, and sweets and desserts,[3] or sweets, butter, soda, mayonnaise, sugar, cookies, tail of a lamb, hydrogenated fat, and eggs,[63] and refined grains, red meat, butter, processed meat, high-fat dairy, sweets and desserts, pizza, potato, eggs, hydrogenated fats, and soft drinks[66] is called as a “Western” dietary pattern.
In a cross-sectional study of 486 Iranian women between 40 and 60 years of age, three dietary patterns were determined by using the factor analysis method: 1. “Healthy” pattern defined by frequent consumption of fruits, green leafy and cruciferous vegetables, tomatoes, legumes, tea, and poultry; 2. ready-to-use food items as the main footsteps of modernization or so-called as “Western” dietary pattern; and 3. “Iranian traditional” pattern consists of whole and refined grains, potatoes, legumes, tea, hydrogenated fats, and broth. The highest OR of IR and syndrome X was observed in people with the adherence to the highest quintile of “Western” diet. This result is similar to the result of Fung et al. who observed a positive association between “Western” pattern adherence and insulin level.[67] It should be mentioned that “Healthy” pattern can reduce risk of IR by 45%, while adherence to the “Western” dietary pattern increases this risk to 15%.[66]
Mcnaughton et al. in an Australian cohort study (Whitehall II) observed higher incidence of type 2 diabetes and higher value of HOMA-IR by adherence to the highest quartile of a diet rich in soft drinks, sugar-sweetened beverages, burgers and sausages, snacks, and white bread, and low intake of fiber food sources, by 2.95 times.[68] A multiethnic Hawaiian survey revealed that higher ORs for type 2 DM were associated with “animal” foods, “local ethnic” dishes, and “Western” dietary pattern. “Animal” and “local ethnic” dishes included high intake of cabbage, rice, shell fish, corned beef plus “Hawaiian and Filipino” dishes.[69] The study showed that people with “Modern” dietary pattern had a lower postprandial plasma glucose, after adjusting the confounding factors in the analysis in brief more consumptions of vegetables, vegetable oil/vinegar dressing, fruits, cereals, rice, pasta, and poultry against “Traditional” diet (contains red meat, high-fat meat sandwich, butter and lard, potatoes, low-fat fishes, and sauces). This study showed that eating pattern can affect 2 h plasma glucose independent of subject's tolerance.[65] Analysis of dietary intake among 1508 Samoan and American Samoan subjects derived two major diets as “Neo-traditional pattern” and “Modern pattern.” “Neo-traditional pattern” is rich in local dishes such as coconut products, lobster, starchy vegetables, crab, and low consumptions of soda and chips, while “Modern dietary pattern” contains processed and ready-to-use foods like cake, butter, eggs, and chips. In contrast with “Neo-traditional” pattern, “Modern” pattern represented lower serum glucose concentration and metabolic syndrome in Samoan men and women.[70] The effects of “Healthy,” “Western,” and “Traditional” dietary patterns among type 2 DM were evaluated in various studies whose characters are reflected in Table 3.
Table 3.
Characteristics of various studies that evaluated the effects of “Healthy” and “Western” and “Traditional” dietary patterns on diabetes mellitus type 2
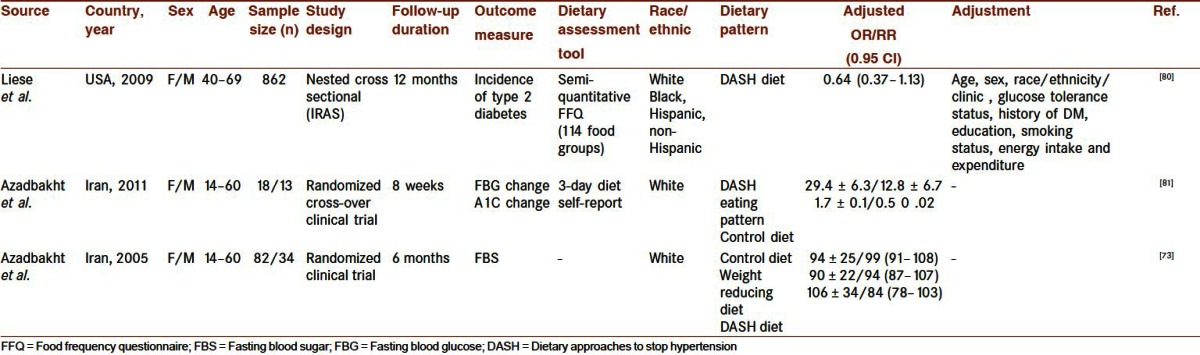
“DASH” dietary pattern
Besides the first known effect of DASH on blood pressure control,[71–77] the other useful potent roles of its main components, such as low-fat dairies and fiber-based foods, were observed on lipid profile[74,78] and features of metabolic syndrome.[74,79] DASH can also reduce the coronary heart disease.[80] In recent years, several surveys assessed DASH effects on blood glucose and incidence of type 2 DM. In the insulin resistance atherosclerosis study (IRAS) of 862 subjects from three different ethnics (Hispanic, non-Hispanic White and Black), “DASH” diet lowered the risk of diabetes incidence by as much as 36% in Whites against Black and Hispanic participants.[81] The effect of “DASH” diet on FBG was shown in two randomized clinical trial studies. In one study, three diets were prescribed for 116 men and women during 6 months. These diets consisted of “weight reducing” diet, “DASH” diet, and “control” diet. The “weight reducing” diet is defined as a diet with lower calorie contents and more “consumption of healthy food items” (such as vegetables, fruits, and low-fat Dairies) Subjects in the “control group” followed their usual eating habits. The significant reduction of FBG in both sexes with “DASH” diet emphasized on its safe effects to modify metabolic syndrome features.[74] The other cross-over randomized clinical trial (RCT) assessed the effects of “DASH” diet on HbA1C and fasting blood sugar (FBS) levels in diabetic patients. Reduction in FBG and HbA1C following adherence to the DASH diet showed that DASH eating pattern is a useful strategy in controlling blood glucose among type 2 diabetic patients.[57] Table 4 reflects the characters of related studies.
Table 4.
Characteristics of various studies that evaluated the effects of “DASH” dietary pattern on diabetes mellitus type 2
Other dietary habits
In Panagiotakos’ study, a positive correlation between red meat intake and Homeostasis Model Assessment of Insulin. Resistance and Insulin Secretory Capacity (HOMA-IR, HOMA-B), insulin, and blood glucose levels was observed among 2832 subjects without cardiovascular disorders.[43] However, there was no significant relationship between healthy food groups such as vegetables, legumes, and fruits consumption and glycemic control after controlling for potential confounders.[82] Reverse association between DM incidence and dietary pattern rich in “meat and milk” was observed in another study.[83] The “Traditional” pattern was compared with “meat and alcohol” and “Korean healthy” dietary patterns in a cross-sectional study. White rice was the dominant food item in all three diets. But noodle and dumpling in “Korean” pattern and processed meat products in “meat and alcohol” eating habit showed significantly different effect on FBG. “Meat and alcohol” dietary pattern increased the risk of high blood glucose by 33%.[84] Furthermore, data from the Puerto Rican elder inhabitants with rice and bean rich diet were studied in a longitudinal investigation among 1167 subjects. Analysis of their eating habits extracted three main patterns: “meat and French fries,” “Traditional pattern” (rice, beans, and oils), “sweets, sugary beverages, and dairy desserts.” After controlling the confounders, just “sweet” diet had a negative significant association with fasting serum sugar.[85] A cross-sectional study among 984 Iranian women revealed that the clusters of diet containing “fish, vegetables, legumes, cereals, and fruits,” and diet rich in “dairy products and eggs” could decrease FBS. However, diet rich in “red or white meat, meat products, and potatoes,” “pasta” and “sweet” patterns had unfavorable effects.[86] A reverse association of habitual diet with hyperglycemia and hyperinsulinemia was also observed in a nested cross-sectional survey of six dietary patterns among Sweden adults. Data showed lower hyperinsulinemia in women with higher milk-fat–based food habits against taking white bread items, in common.[87] He et al. derived four dietary patterns after analysis of semi-quantitative food frequency questionnaire among 20,210 Chinese adults: “Western Adopter”(Western-like pattern), “Green Water” (high vegetables and low animal food style in the southeast area), “New Affluence” (rich in animals and soy products which is used by well-to-do individuals), and “Yellow Earth” [high carbohydrate (CHO) and low fruits, vegetables, and animal dishes, which is common in the northwest area]. Comparing “Green Water consumer,” the prevalence of IGT in “Yellow Earth” and “New Affluence” escalated to ratios of 1.22 and 2.05, in sequence.[88] Risk of DM in Caucasian, Japanese, American, and Native Hawaiian participants in a 14-year follow-up survey showed a significant difference according to sex, and their three dietary designs included: “fat and meat,” “vegetables,” and “fruit and milk” dietary patterns. The hazard ratios for type 2 diabetes among women/men who adhered to the fifth quartiles of mentioned diets were 1.22/1.40, 1.02/0.86, and 0.85/0.92, respectively. These ratios were significant in all ethnics, except for “Native Hawaiian” subjects.[89] Another multiethnic population-based cohort study among 6814 White, Black, Hispanic, and Chinese subjects, which was conducted during 5 years, revealed two patterns which were defined as: 1. Beans, tomatoes, refined grains, high-fat dairy, red meat and 2. whole grain, fruit, nuts/seeds, green leafy vegetables, low-fat dairy, and low-risk food patterns as the common dietary habits. Adherence to the first diet was accompanied with 18% higher risk ratio, while the others reduced the risk by 15%.[90] The results of a study among 7500 Chinese revealed that “high dairy milk” dietary pattern had decreased diabetes incidence by almost 22%, in contrast to “meat, fruit, and vegetable rich pattern” which increased the relative risk to 1.05.[64]
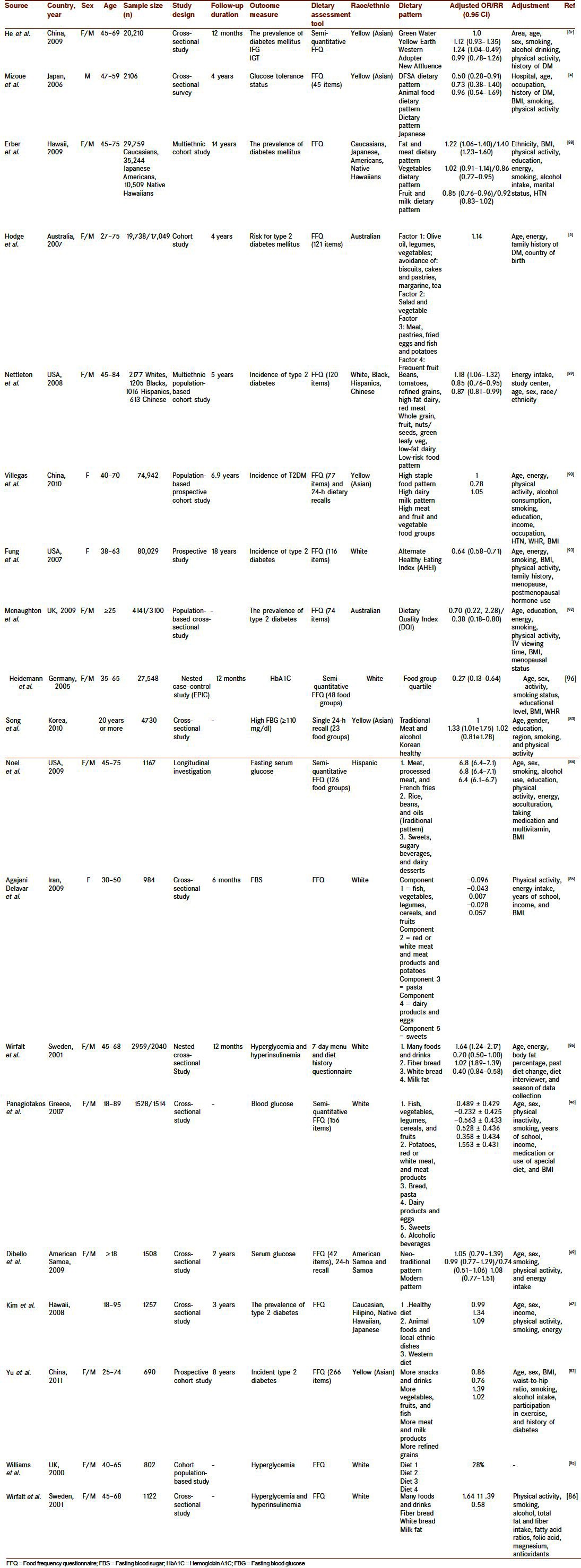
All the mentioned studies in this review paper had used factor analysis and cluster analysis. These analyses detect dietary patterns from the existing data with no any prior assumption of disease. Besides these posteriori methods, another method for evaluating the overall diet is based on our previous knowledge about the effects of dietary components on health and disease. which is a prior method. This method is based on scoring different components of a diet according to the scientific evidence regarding diet–disease relationship and dietary recommendations.[27] Healthy Eating Index (HEI) is an example of this prior method. This index shows how well a diet follows the US dietary guidelines.[91] High “diet quality index” which is defined based on dietary variety, and high intake of whole grain, lean protein, low-fat dairy, and high-fiber food items was associated with OR of type 2 DM by 0.38 in men and OR for pre-diabetes by 0.66 in women.[92] Alternative Healthy Eating index (AHEI) is defined based on its association with various disorders, which consists of nine chief components of diet quality such as intake of vegetables, nuts, fruits, soybean, the white-to-red meat ratio, trans fatty acids, polyunsaturated to saturated fatty acids ratio (P/S ratio), alcohol drinking, and taking multivitamin, and it is a suitable substitute for HEI. In a prospective study, Fung et al. assessed AHEI among 80,029 women. Data show that high index can lower the incidence of type 2 diabetes by 36% during 18 years.[93] The cluster analysis on dietary intake of 1052 Italians derived five main components which included: “common” (low in fat but rich in MUFA and CHO), “animal products” (high in animal protein, SFA, and cholesterol), “starch” (rich in vegetable protein and starch), “vegetal/fat”(high in olive oil and seeds), and “vitamin/fiber”(rich in fruits and vegetables). Leite et al. observed the lowest IGT prevalence by adherence to “starch” pattern, in contrast to “animal” food pattern.[94] In the four dietary patterns derived from population-based cohort study, a negative association between commonly consumed fiber-based foods and white meat in “Diet 1” and diet rich in cake, vegetable, and cheese pattern named as “Diet 2” with IGT was seen. There was also a 28% reduction in diabetes incidence following adherence to the diet containing fiber-based foods and white meat.[27,95] Sex difference in relation to dietary pattern and features of metabolic syndrome was reflected significantly in Malmo Diet and Cancer Study of Swedish adults. Risk of hyperglycemia accompanying dietary pattern rich in meat and dairies increased by 64% among men, while it was not significantly associated with hyperglycemia among women[27] However, Heidemann revealed that those in the highest quartiles of diet rich in fruits and poor in meat, beer, and soft drink had lower incidence of type 2 DM by 0.27.[96] In Framingham Offspring Study, “fruits, reduced fat dairy, and whole grains,” “refined grains and sweets,” “beer” and “soda” diets were extracted. Data revealed that adherence to “soda” pattern is accompanied by higher fasting insulin level. A pattern high in fruits, vegetables, whole grains, and reduced fat dairy protects against insulin resistance compared to sweet food pattern and soda pattern which are associated with insulin resistance.[97] Table 5 shows the different surveys that assess the effects of various dietary patterns among type 2 DM patients.
Table 5.
Characteristics of various studies that evaluated the effects of different dietary patterns on diabetes mellitus type 2
CONCLUSION
Dietary intakes have important roles against insulin resistance, and in the prevention and management of hyperglycemia.[31] Epidemiological studies revealed that dietary patterns high in fiber-rich food items such as vegetables, fruits, whole grains, seeds and nuts, plus white meat sources like poultry and fish could have protective effects against the incidence of DM. However, dietary patterns rich in processed meat and red meat, refined cereals, and SFAs are associated with higher risk of DM.[28] Healthy patterns, Mediterranean, and Prudent dietary patterns also are protective dietary patterns against DM. However, adherence to Western dietary pattern is associated with higher risk of diabetes.[86,98,99] These results are in line with Iranian dietary pattern surveys which emphasize on adherence to Healthy pattern to manage abnormal glucose homeostasis.[66] It is suggested to see the relationship of different dietary patterns and the incidence of type 2 diabetes in cohort studies among different populations in future studies.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Sharifirad G, Entezari MH, Kamran A, Azadbakht L. The effectiveness of nutritional education on the knowledge of diabetic pa-tients using the health belief model. J Res Med Sci. 2009;14:1–6. [PMC free article] [PubMed] [Google Scholar]
- 2.Thanopoulou AC, Karamanos BG, Angelico FV, Assaad-Khalil SH, Barbato AF, Del Ben MP, et al. Dietary fat intake as risk factor for the development of diabetes. Diabetes care. 2003;26:302–7. doi: 10.2337/diacare.26.2.302. [DOI] [PubMed] [Google Scholar]
- 3.van Dam RM, Rimm EB, Willett EB, Stampfer MJ, Hu FB. Dietary patterns and risk for type 2 diabetes mellitus in US men. Ann Intern Med. 2002;136:201–9. doi: 10.7326/0003-4819-136-3-200202050-00008. [DOI] [PubMed] [Google Scholar]
- 4.Mizoue T, Yamaji T, Tabata S, Yamaguchi S, Ogawa S, Mineshita M, et al. Dietary patterns and glucose tolerance abnormalities in Japanese men. J Nutr. 2006;136:1352–8. doi: 10.1093/jn/136.5.1352. [DOI] [PubMed] [Google Scholar]
- 5.Hodge AM, English DR, O’Dea K, Giles GG. Dietary patterns and diabetes incidence in the melbourne collaborative cohort study. Am J Epidemiol. 2007;165:603–10. doi: 10.1093/aje/kwk061. [DOI] [PubMed] [Google Scholar]
- 6.Mosdøl A, Witte DR, Frost G, Marmot MG, Brunner EJ. Dietary glycemic index and glycemic load are associated with high-density-lipoprotein cholesterol at baseline but not with increased risk of diabetes in the Whitehall II study. Am J Clin Nutr. 86:988–94. doi: 10.1093/ajcn/86.4.988. [DOI] [PubMed] [Google Scholar]
- 7.Duc Son NT, Hanh TT, Kusama K, Kunii D, Sakai T, Hung NT, et al. Anthropometric characteristics, dietary patterns and risk of type 2 diabetes mellitus in Vietnam. J Am Coll Nutr. 2005;24:229–34. doi: 10.1080/07315724.2005.10719469. [DOI] [PubMed] [Google Scholar]
- 8.Sartorelli DS, Cardoso MA. Association between dietary carbohydrates and type 2 diabetes mellitus: epidemiological evidences. Arq Bras Endocrinol Metabol. 2006;50:415–26. doi: 10.1590/s0004-27302006000300003. [DOI] [PubMed] [Google Scholar]
- 9.Venn BJ, Mann JI. Cereal grains, legumes and diabetes. Eur J Clin Nutr. 2004;58:1443–61. doi: 10.1038/sj.ejcn.1601995. [DOI] [PubMed] [Google Scholar]
- 10.Keegan MT, Goldberg ME, Torjman MC, Coursin DB. Challenges in Glycemic Control in perioperative and critically ill patients: Perioperative and critical illness dysglycemia-controlling the iceberg”. J Diabetes Sci Technol. 2009;3:1288–91. doi: 10.1177/193229680900300608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huxley R, Lee CM, Barzi F, Timmermeister L, Czernichow S, Perkovic V, et al. Coffee, decaffeinated coffee, and tea consumption in relation to incident type 2 diabetes mellitus: A systematic review with meta-analysis. Arch Intern Med. 2009;169:2053–63. doi: 10.1001/archinternmed.2009.439. [DOI] [PubMed] [Google Scholar]
- 12.Goldstein BJ, Wieland DM. Type 2 diabetes mellitus: principle and practice: Informa Healthcare. 2008 [Google Scholar]
- 13.Sahyoun NR, Anderson AL, Tylavsky FA, Lee JS, Sellmeyer DE, Harris TB. Health, Aging, and Body Composition Study. Dietary glycemic index and glycemic load and the risk of type 2 diabetes in older adults. Am J Clin Nutr. 2008;87:126–31. doi: 10.1093/ajcn/87.1.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pittas AG, Lau J, Hu FB, Dawson-Hughes B. The role of vitamin D and calcium in type 2 diabetes. A systematic review and meta-analysis. J Clin Endocrinol Metab. 2007;92:2017–29. doi: 10.1210/jc.2007-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naghavi M, Abolhassani F, Pourmalek F, Lakeh M, Jafari N, Vaseghi S, et al. The burden of disease and injury in Iran 2003”. Popul Health Metr. 2009;7:9. doi: 10.1186/1478-7954-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lindström J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson JG, Hemiö K, et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow up of the Finnish Disease prevention Study. Lancet. 2006;368:1673–9. doi: 10.1016/S0140-6736(06)69701-8. [DOI] [PubMed] [Google Scholar]
- 17.Li G, Zhang P, Wang J, Gregg EW, Yang W, Gong Q, et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Quin Diabetes Prevention Study: A 20-year follow up study. Lancet. 2008;371:1783–9. doi: 10.1016/S0140-6736(08)60766-7. [DOI] [PubMed] [Google Scholar]
- 18.Colditz GA, Manson JE, Stampfer MJ, Rosner B, Willett WC, Speizer FE. Diet and risk of clinical diabetes in women”. Am J Clin Nutr. 1992;55:1018–23. doi: 10.1093/ajcn/55.5.1018. [DOI] [PubMed] [Google Scholar]
- 19.Staiger H, Machicao F, Fritsche A, Häring HU. Pathomechanisms of type 2 diabetes genes. Endocr Rev. 2009;30:557–85. doi: 10.1210/er.2009-0017. [DOI] [PubMed] [Google Scholar]
- 20.Mirmiran P, Azadbakht L, Azizi F. Dietary behaviour of Tehranian adolescents does not accord with their nutritional knowledge”. Public Health Nutr. 2007;10:897–901. doi: 10.1017/S1368980007246701. [DOI] [PubMed] [Google Scholar]
- 21.Ylönen K, Saloranta C, Kronberg-Kippilä C, Groop L, Aro A, Virtanen SM ; Botnia Dietary Study. Associations of dietary fiber with glucose metabolism in nondiabetic relatives of subjects with type 2 diabetes. Diabetes Care. 2003;26:1979–85. doi: 10.2337/diacare.26.7.1979. [DOI] [PubMed] [Google Scholar]
- 22.Cruz AF, Calle-Pascual AL ; Diabetes and Nutrition Study Group, Spanish Diabetes Association. Diabetes nutrition and complications trial: Trends in nutritional pattern between 1993 and 2000 and targets of diabetes treatment in a sample of Spanish people with diabetes. Diabetes Care. 2004;27:984–7. doi: 10.2337/diacare.27.4.984. [DOI] [PubMed] [Google Scholar]
- 23.Kant AK. Dietary patterns and health outcomes. J Am Diet Assoc. 2004;104:615–35. doi: 10.1016/j.jada.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 24.Van Dam RM, Hu FB, Rosenberg L, Krishnan S, Palmer JR. Dietary calcium and magnesium, major food sources, and risk of type 2 diabetes in US black women. Diabetes Care. 2006;29:2238–43. doi: 10.2337/dc06-1014. [DOI] [PubMed] [Google Scholar]
- 25.Hu FB, van Dam RM, Liu S. Diet and risk of type II diabetes: the role of types of fat and carbohydrate. Diabetologia. 2001;44:805–17. doi: 10.1007/s001250100547. [DOI] [PubMed] [Google Scholar]
- 26.Isharwal S, Misra A, Wasir JS, Nigam P. Diet & insulin resistance: A review & Asian Indian perspective. Indian J Med Res. 2009;129:485–99. [PubMed] [Google Scholar]
- 27.Baxter AJ, Coyne T, McClintock C. Dietary patterns and metabolic syndrome-A review of epidemiologic evidence. Asia Pac J Clin Nutr. 2006;15:134–42. [PubMed] [Google Scholar]
- 28.Kastorini CM, Panagiotakos DB. Mediterranean diet and diabetes prevention: Myth or fact? World J Diabetes. 2010;1:65–7. doi: 10.4239/wjd.v1.i3.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Newby PK, Weismayer C, Akesson A, Tucker KL, Wolk A. Long-term stability of food patterns identified by use of factor analysis among Swedish women. J Nutr. 2006;136:626–33. doi: 10.1093/jn/136.3.626. [DOI] [PubMed] [Google Scholar]
- 30.Weismayer C, Anderson JG, Wolk A. Changes in the stability of dietary patterns in a study of middle-aged Swedish women. J Nutr. 2006;136:1582–7. doi: 10.1093/jn/136.6.1582. [DOI] [PubMed] [Google Scholar]
- 31.Kastorini CM, Panagiotakos DB. Dietary patterns and prevention of type 2 diabetes: from research to clinical practice, a systematic review. Curr Diabetes Rev. 2009;5:221–7. doi: 10.2174/157339909789804341. [DOI] [PubMed] [Google Scholar]
- 32.Schroder H. Protective mechanisms of the mediterranean diet in obesity and type 2 diabetes. J Nutr Biochem. 2007;18:149–60. doi: 10.1016/j.jnutbio.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 33.Toobert DJ, Glasgow RE, Strycker LA, Barrera M, Jr, Radcliffe JL, Wander RC, et al. Biologic and quality-of-life outcomes from the Mediterranean lifestyle program: A randomized clinical trial. Diabetes Care. 2003;26:2288–93. doi: 10.2337/diacare.26.8.2288. [DOI] [PubMed] [Google Scholar]
- 34.Ciccarone E, Di Castelnuovo A, Salcuni M, Siani A, Giacco A, Donati MB, et al. A high-score Mediterranean dietary pattern is associated with a reduced risk of peripheral arterial disease in Italian patients with Type 2 diabetes”. J Thromb Haemost. 2003;1:1744–52. doi: 10.1046/j.1538-7836.2003.00323.x. [DOI] [PubMed] [Google Scholar]
- 35.Paletas K, Athanasiadou E, Sarigianni M, Paschos P, Kalogirou A, Hassapidou M, et al. The protective role of the Mediterranean diet on the prevalence of metabolic syndrome in a population of Greek obese subjects. J Am Coll Nutr. 2010;29:41–5. doi: 10.1080/07315724.2010.10719815. [DOI] [PubMed] [Google Scholar]
- 36.Rumawas ME, Meigs JB, Dwyer JT, McKeown NM, Jacques PF. Mediterranean-style dietary pattern, reduced risk of metabolic syndrome traits, and incidence in the framingham offspring cohort. Am J Clin Nutr. 2009;90:1608–14. doi: 10.3945/ajcn.2009.27908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, Greenberg I, et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med. 2008;359:229–41. doi: 10.1056/NEJMoa0708681. [DOI] [PubMed] [Google Scholar]
- 38.Fragopoulou E, Panagiotakos DB, Pitsavos C, Tampourlou M, Chrysohoou C, Nomikos T, et al. The association between adherence to the Mediterranean diet and adiponectin levels among healthy adults: The ATTICA study. J Nutr Biochem. 2010;21:285–9. doi: 10.1016/j.jnutbio.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 39.Michalsen A, Lehmann N, Pithan C, Knoblauch NT, Moebus S, Kannenberg F, et al. Mediterranean diet has no effect on markers of infl ammation and metabolic risk factors in patients with coronary artery disease. Eur J Clin Nutr. 2006;60:478–85. doi: 10.1038/sj.ejcn.1602340. [DOI] [PubMed] [Google Scholar]
- 40.Giugliano D, Esposito K. Mediterranean diet and metabolic diseases. Curr Opin Lipidol. 2008;19:63–8. doi: 10.1097/MOL.0b013e3282f2fa4d. [DOI] [PubMed] [Google Scholar]
- 41.Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Covas MI, et al. Effects of a Mediterranean-style diet on cardiovascular risk factors. Ann Intern Med. 2006;145:1–11. doi: 10.7326/0003-4819-145-1-200607040-00004. [DOI] [PubMed] [Google Scholar]
- 42.Esposito K, Maiorino MI, Di Palo C, Giugliano D Campanian Postprandial Hyperglycemia Study Group. Adherence to a Mediterranean diet and glycaemic control in Type 2 diabetes mellitus. Diabet Med. 2009;26:900–7. doi: 10.1111/j.1464-5491.2009.02798.x. [DOI] [PubMed] [Google Scholar]
- 43.Panagiotakos DB, Tzima N, Pitsavos C, Chrysohoou C, Zampelas A, Toussoulis D, et al. The association between adherence to the Mediterranean diet and fasting indices of glucose homoeostasis: The ATTICA study. J Am Coll Nutr. 2007;26:32–8. doi: 10.1080/07315724.2007.10719583. [DOI] [PubMed] [Google Scholar]
- 44.Gu Y, Luchsinger JA, Stern Y, Scarmeas N. Mediterranean diet, inflammatory and metabolic biomarkers, and risk of alzheimer's disease. J Alzheimers Dis. 2010;22:483–92. doi: 10.3233/JAD-2010-100897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Martínez-González MA, de la Fuente-Arrillaga C, Nunez-Cordoba JM, Basterra-Gortari FJ, Beunza JJ, Vazquez Z, et al. Adherence to Mediterranean diet and risk of developing diabetes: Prospective cohort study. BMJ. 2008;336:1348–51. doi: 10.1136/bmj.39561.501007.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Panagiotakos DB, Pitsavos C, Skoumas Y, Stefanadis C. The association between food patterns and the metabolic syndrome using principal components analysis: The ATTICA study. J Am Diet Assoc. 2007;107:979–87. doi: 10.1016/j.jada.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 47.Tortosa A, Bes-Rastrollo M, Sanchez-Villegas A, Basterra-Gortari FJ, Nuñez-Cordoba JM, Martinez-Gonzalez MA. Mediterranean diet inversely associated with the incidence of metabolic syndrome: The SUN prospective cohort. Diabetes Care. 2007;30:2957–9. doi: 10.2337/dc07-1231. [DOI] [PubMed] [Google Scholar]
- 48.Tzima N, Pitsavos C, Panagiotakos DB, Skoumas J, Zampelas A, Chrysohoou C, et al. Mediterranean diet and insulin sensitivity, lipid profile and blood pressure levels, in overweight and obese people, the Attica study”. Lipids Health Dis. 2007;6:22. doi: 10.1186/1476-511X-6-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Panagiotakos DB, Polystipioti A, Papairakleous N, Polychronopoulos E. Long-term adoption of a Mediterranean diet is associated with a better health status in elderly people, a cross-sectional survey in Cyprus. Asia Pac J Clin Nutr. 2007;16:331–7. [PubMed] [Google Scholar]
- 50.Lindeberg S, Jönsson T, Granfeldt Y, Borgstrand E, Soffman J, Sjöström K, et al. A Palaeolithic diet improves glucose tolerance more than a Mediterranean-like diet in individuals with ischaemic heart disease”. Diabetologia. 2007;50:1795–807. doi: 10.1007/s00125-007-0716-y. [DOI] [PubMed] [Google Scholar]
- 51.Mozaffarian D, Marfisi R, Levantesi G, Silletta MG, Tavazzi L, Tognoni G, et al. Incidence of new-onset diabetes and impaired fasting glucose in patients with recent myocardial infarction and the effect of clinical and lifestyle risk factors. Lancet. 2007;370:667–75. doi: 10.1016/S0140-6736(07)61343-9. [DOI] [PubMed] [Google Scholar]
- 52.Sánchez-Taínta A, Estruch R, Bulló M, Corella D, Gómez-Gracia E, Fiol M, Algorta J, et al. Adherence to a Mediterranean-type diet and reduced prevalence of clustered cardiovascular risk factors in a cohort of 3204 high-risk patients. Eur J Cardiovasc Prev Rehabil. 2008;15:589–93. doi: 10.1097/HJR.0b013e328308ba61. [DOI] [PubMed] [Google Scholar]
- 53.Brunner EJ, Mosdøl A, Witte DR, Martikainen P, Stafford M, Shipley MJ. Dietary patterns and 15-y risks of major coronary events, diabetes, and mortality. Am J Clin Nutr. 2008;87:1414–21. doi: 10.1093/ajcn/87.5.1414. [DOI] [PubMed] [Google Scholar]
- 54.Panagiotakos DB, Pitsavos C, Chrysohoou C, Stefanadis C. The epidemiology of type 2 diabetes mellitus in Greek adults: The ATTICA study. Diabet Med. 2005;22:1581–8. doi: 10.1111/j.1464-5491.2005.01731.x. [DOI] [PubMed] [Google Scholar]
- 55.Buscemi S, Verga S, Tranchina MR, Cottone S, Cerasola G. Effects of hypocaloric very low carbohydrate diet vs. Mediterranean diet on endothelial function in obese women. Eur J Clin Invest. 2009;39:339–47. doi: 10.1111/j.1365-2362.2009.02091.x. [DOI] [PubMed] [Google Scholar]
- 56.Esposito K, Marfella R, Ciotola M, Di Palo C, Giugliano F, Giugliano G, et al. Effect of a Meditarranean style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: A randomized trial. JAMA. 2004;292:1440–6. doi: 10.1001/jama.292.12.1440. [DOI] [PubMed] [Google Scholar]
- 57.Azadbakht L, Fard NRP, Karimi M, Baghaei MH, Surkan PJ, Rahimi M, et al. Effects of the dietary approaches to stop hypertension (DASH) eating plan on cardiovascular risks among type 2 diabetic patients. Diabetes care. 2011;34(1):55. doi: 10.2337/dc10-0676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fung TT, Schulze M, Manson JE, Willett WC, Hu FB. Dietary patterns, meat intake, and the risk of type 2 diabetes in women. Arch Intern Med. 2004;164:2235–40. doi: 10.1001/archinte.164.20.2235. [DOI] [PubMed] [Google Scholar]
- 59.Montonen J, Knekt P, Härkänen T, Järvinen R, Heliövaara M, Aromaa A, et al. Dietary patterns and the incidence of type 2 diabetes. Am J Epidemiol. 2005;161:219–27. doi: 10.1093/aje/kwi039. [DOI] [PubMed] [Google Scholar]
- 60.Lutsey PL, Steffen LM, Stevens J. Dietary intake and the development of the metabolic syndrome: The atherosclerosis risk in communities study. Circulation. 2008;117:754–61. doi: 10.1161/CIRCULATIONAHA.107.716159. [DOI] [PubMed] [Google Scholar]
- 61.Villegas R, Salim A, Collins MM, Flynn A, Perry IJ. Dietary patterns in middle-aged Irish men and women defined by cluster analysis. Public Health Nutr. 2004;7:1017–24. doi: 10.1079/PHN2004638. [DOI] [PubMed] [Google Scholar]
- 62.Villegas R, Salim A, Flynn A, Perry IJ. Prudent diet and the risk of insulin resistance. Nutr Metab Cardiovasc Dis. 2004;14:334–43. doi: 10.1016/s0939-4753(04)80023-1. [DOI] [PubMed] [Google Scholar]
- 63.Amini M, Esmaillzadeh A, Shafaeizadeh S, Behrooz J, Zare M. Relationship between major dietary patterns and metabolic syndrome among individuals with impaired glucose tolerance”. Nutrition. 2010;26:986–92. doi: 10.1016/j.nut.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 64.Villegas R, Yang G, Gao YT, Cai H, Li H, Zheng W, et al. Dietary patterns are associated with lower incidence of type 2 diabetes in middle-aged women: The shanghai women's health study. Int J Epidemiol. 2010;39:889–99. doi: 10.1093/ije/dyq008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lau C, Toft U, Tetens I, Carstensen B, Jørgensen T, Pedersen O, et al. Dietary patterns predict changes in two-hour post-oral glucose tolerance test plasma glucose concentrations in middle-aged adults. J Nutr. 2009;139:588–93. doi: 10.3945/jn.108.100339. [DOI] [PubMed] [Google Scholar]
- 66.Esmaillzadeh A, Kimiagar M, Mehrabi Y, Azadbakht L, Hu FB, Willett WC. Dietary patterns, insulin resistance, and prevalence of the metabolic syndrome in women”. Am J Clin Nutr. 2007;85:910–8. doi: 10.1093/ajcn/85.3.910. [DOI] [PubMed] [Google Scholar]
- 67.Fung TT, Rimm EB, Spiegelman D, Rifai N, Tofler GH, Willett WC, et al. Association between dietary patterns and plasma biomarkers of obesity and cardiovascular disease risk. Am J Clin Nutr. 2001;73:61–7. doi: 10.1093/ajcn/73.1.61. [DOI] [PubMed] [Google Scholar]
- 68.McNaughton SA, Mishra GD, Brunner EJ. Dietary patterns, insulin resistance, and incidence of type 2 diabetes in the Whitehall II Study. Diabetes care. 2008;31:1343–8. doi: 10.2337/dc07-1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kim HS, Park SY, Grandinetti A, Holck PS, Waslien C. Major dietary patterns, ethnicity, and prevalence of type 2 diabetes in rural Hawaii. Nutrition. 2008;24:1065–72. doi: 10.1016/j.nut.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.DiBello JR, McGarvey ST, Kraft P, Goldberg R, Campos H, Quested C, et al. Dietary patterns are associated with metabolic syndrome in adult Samoans. J Nutr. 2009;139:1933–43. doi: 10.3945/jn.109.107888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ard JD, Coffman CJ, Lin PH, Svetkey LP. One-year follow-up study of blood pressure and dietary patterns in dietary approaches to stop hypertension (DASH)-sodium participants. Am J Hypertens. 2004;17:1156–62. doi: 10.1016/j.amjhyper.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 72.Vollmer WM, Sacks FM, Svetkey LP. New insights into the effects on blood pressure of diets low in salt and high in fruits and vegetables and low-fat dairy products. Curr Control Trials Cardiovasc Med. 2001;2:71–74. doi: 10.1186/cvm-2-2-071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Obarzanek E, Sacks FM, Vollmer WM, Bray GA, Miller ER, 3rd, Lin PH, et al. Effects on blood lipids of a blood pressure#x2013;lowering diet: The dietary approaches to stop hypertension (DASH) Trial. Am J Clin Nutr. 2001;74:80–9. doi: 10.1093/ajcn/74.1.80. [DOI] [PubMed] [Google Scholar]
- 74.Azadbakht L, Mirmiran P, Esmaillzadeh A, Azizi T, Azizi F. Beneficial effects of a dietary approaches to stop hypertension eating plan on features of the metabolic syndrome. Diabetes Care. 2005;28:2823–31. doi: 10.2337/diacare.28.12.2823. [DOI] [PubMed] [Google Scholar]
- 75.Pitsavos C, Panagiotakos D, Weinem M, Stefanadis C. Diet, exercise and the metabolic syndrome”. Rev Diabet Stud. 2006;3:118–26. doi: 10.1900/RDS.2006.3.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hu FB, Willett WC. Optimal diets for prevention of coronary heart disease. JAMA. 2002;288:2569–78. doi: 10.1001/jama.288.20.2569. [DOI] [PubMed] [Google Scholar]
- 77.Kastorini CM, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB. The effect of mediterranean diet on metabolic syndrome and its components: a meta-analysis of 50 studies and 534,906 individuals”. J Am Coll Cardiol. 2011;57:1299–313. doi: 10.1016/j.jacc.2010.09.073. [DOI] [PubMed] [Google Scholar]
- 78.Azizi F, Salehi P, Etemadi A, Zahedi-Asl S. Prevalence of metabolic syndrome in an urban population: Tehran lipid and glucose study. Diabetes Res Clin Pract. 2003;61:29–37. doi: 10.1016/s0168-8227(03)00066-4. [DOI] [PubMed] [Google Scholar]
- 79.Young-Hyman D, Schlundt DG, Herman L, De Luca F, Counts D. Evaluation of the insulin resistance syndrome in 5-to 10-year-old overweight/obese African-American children. Diabetes Care. 2001;24:1359–64. doi: 10.2337/diacare.24.8.1359. [DOI] [PubMed] [Google Scholar]
- 80.Azadbakht L, Surkan PJ, Esmaillzadeh A, Willett WC. The dietary approaches to stop hypertension eating plan affects c-reactive protein, coagulation abnormalities, and hepatic function tests among type 2 diabetic patients. J Nutr. 2011;141:1083–8. doi: 10.3945/jn.110.136739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liese AD, Nichols M, Sun X, D’Agostino RB, Jr, Haffner SM. Adherence to the DASH Diet is inversely associated with incidence of type 2 diabetes: the insulin resistance atherosclerosis study. Diabetes Care. 2009;32:1434–6. doi: 10.2337/dc09-0228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Azadbakht L, Fard NRP, Karimi M, Baghaei MH, Surkan PJ, Rahimi M, et al. Effects of the dietary approaches to stop hypertension (DASH) eating plan on cardiovascular risks among type 2 diabetic patients. Diabetes care. 2011;34(1):55. doi: 10.2337/dc10-0676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yu R, Woo J, Chan R, Sham A, Ho S, Tso A, et al. Relation between dietary intake and the development of type 2 diabetes in a Chinese population: The Hong Kong Dietary Survey”. Public Health Nutr. 2011;14:1133–41. doi: 10.1017/S136898001100053X. [DOI] [PubMed] [Google Scholar]
- 84.Song Y, Joung H. A traditional Korean dietary pattern and metabolic syndrome abnormalities. Nutr Metab Cardiovasc Dis. 2012;22:456–62. doi: 10.1016/j.numecd.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 85.Noel SE, Newby PK, Ordovas JM, Tucker KL. A traditional rice and beans pattern is associated with metabolic syndrome in Puerto Rican older adults”. J Nutr. 2009;139:1360–7. doi: 10.3945/jn.109.105874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Delavar MA, Lye MS, Khor GL, Hassan ST, Hanachi P. Dietary patterns and the metabolic syndrome in middle aged women, Babol, Iran. Asia Pac J Clin Nutr. 2009;18:285–92. [PubMed] [Google Scholar]
- 87.Wirfält E, Hedblad B, Gullberg B, Mattisson I, Andrén C, Rosander U, et al. Food patterns and components of the metabolic syndrome in men and women: a cross-sectional study within the Malmö Diet and Cancer cohort. Am J Epidemiol. 2001;154:1150–9. doi: 10.1093/aje/154.12.1150. [DOI] [PubMed] [Google Scholar]
- 88.He Y, Ma G, Zhai F, Li Y, Hu Y, Feskens EJ, et al. Dietary patterns and glucose tolerance abnormalities in Chinese adults. Diabetes Care. 2009;32:1972–6. doi: 10.2337/dc09-0714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Erber E, Hopping BN, Grandinetti A, Park SY, Kolonel LN, Maskarinec G. Dietary patterns and risk for diabetes”. Diabetes Care. 2010;33:532–8. doi: 10.2337/dc09-1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nettleton JA, Steffen LM, Ni H, Liu K, Jacobs DR., Jr Dietary patterns and risk of incident type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA) Diabetes Care. 2008;31:1777–82. doi: 10.2337/dc08-0760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kennedy ET, Ohls J, Carlson S, Fleming K. The healthy eating index: Design and applications. J Am Diet Assoc. 1995;95:1103–8. doi: 10.1016/S0002-8223(95)00300-2. [DOI] [PubMed] [Google Scholar]
- 92.McNaughton SA, Dunstan DW, Ball K, Shaw J, Crawford D. Dietary quality is associated with diabetes and cardio-metabolic risk factors. J Nutr. 2009;139:734–42. doi: 10.3945/jn.108.096784. [DOI] [PubMed] [Google Scholar]
- 93.Fung TT, McCullough M, van Dam RM, Hu FB. A prospective study of overall diet quality and risk of type 2 diabetes in women. Diabetes Care. 2007;30:1753–7. doi: 10.2337/dc06-2581. [DOI] [PubMed] [Google Scholar]
- 94.Leite ML, Nicolosi A. Dietary patterns and metabolic syndrome factors in a non-diabetic Italian population”. Public Health Nutr. 2009;12:1494–503. doi: 10.1017/S1368980008004539. [DOI] [PubMed] [Google Scholar]
- 95.Williams DE, Prevost AT, Whichelow MJ, Cox BD, Day NE, Wareham NJ. A cross sectional study of dietary patterns with glucose intolerance and other features of metabolic syndrome. Br J Nutr. 2000;83:257–66. doi: 10.1017/s0007114500000337. [DOI] [PubMed] [Google Scholar]
- 96.Heidemann C, Hoffmann K, Spranger J, Klipstein-Grobusch K, Möhlig M, Pfeiffer AF, et al. A dietary pattern protective against type 2 diabetes in the european prospective investigation into cancer and nutrition (EPIC)-Potsdam study cohort. Diabetologia. 2005;48:1126–34. doi: 10.1007/s00125-005-1743-1. [DOI] [PubMed] [Google Scholar]
- 97.Liu E, McKeown NM, Newby PK, Meigs JB, Vasan RS, Quatromoni PA, et al. Cross-sectional association of dietary patterns with insulin-resistant phenotypes among adults without diabetes in the Framingham Offspring Study. Br J Nutr. 2009;102:576–83. doi: 10.1017/S0007114509220836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Esposito K, Giugliano D. Diet and inflammation: a link to metabolic and cardiovascular diseases. Eur Heart J. 2006;27:15–20. doi: 10.1093/eurheartj/ehi605. [DOI] [PubMed] [Google Scholar]
- 99.ernandez Maria FL. Metabolic syndrome and the components of the mediterranean functional foods in health and disease. Functional Foods In Health And Disease. 2011;2:25–37. [Google Scholar]


