Abstract
Iron deficiency anemia arises when the balance of iron intake, iron stores, and the body's loss of iron are insufficient to fully support production of erythrocytes. Iron deficiency anemia rarely causes death, but the impact on human health is significant. In the developed world, this disease is easily identified and treated, but frequently overlooked by physicians. In contrast, it is a health problem that affects major portions of the population in underdeveloped countries. Overall, the prevention and successful treatment for iron deficiency anemia remains woefully insufficient worldwide, especially among underprivileged women and children. Here, clinical and laboratory features of the disease are discussed, and then focus is placed on relevant economic, environmental, infectious, and genetic factors that converge among global populations.
Several hundred million people worldwide have iron deficiency anemia. Obstacles involving economics, cultural barriers, and infectious diseases have made it difficult to eradicate this disease.
Iron comprises 5% of the earth’s crust. Its redox states make iron useful for evolving biological processes. Growing lists of biomolecules that bind or incorporate iron are being catalogued according to their structural similarities. An excellent source of information is provided at http://metallo.scripps.edu/PROMISE/PROMISE_LIST.html.
Four general categories of proteins contain iron: (1) mononuclear iron proteins (e.g., superoxide dismutase), (2) diiron-carboxylate proteins (e.g., ribonucleotide reductase, ferritin), (3) iron-sulfur proteins (e.g., aconitase), and (4) heme proteins (e.g., hemoglobin). Among these four categories, the first three protein groups are detected at lower levels, but they are functionally important. Hemoglobin is the most abundant iron-containing protein in humans. More than one-half of total-body iron is contained within hemoglobin. Based on the location of hemoglobin in erythrocytes, anemia is a characteristic trait of iron deficiency.
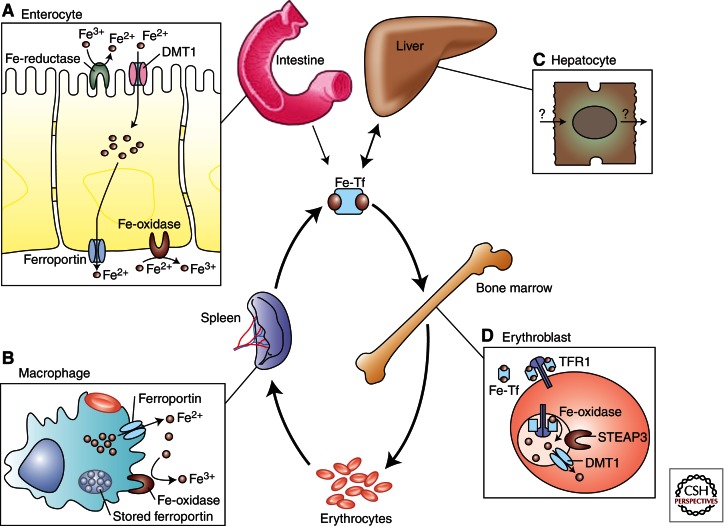
Despite iron’s plentifulness on earth, iron deficiency is extremely common in humans, and is the most prevalent cause of anemia worldwide. To more fully understand iron deficiency anemia, consideration must be directed toward concepts of iron supply and demand for the production of erythrocytes. Erythropoiesis-related demands for iron are created by three variables: tissue oxygenation, erythrocyte turnover, and erythrocyte loss from hemorrhage. Tissue oxygenation requirements and erythrocyte production generally remain stable during adulthood in the absence of hemorrhage, disease, or altered physical activity. As such, iron homeostasis (Fig. 1) also remains stable. Approximately 20 mL of senescent erythrocytes are cleared daily, and the 20 mg of iron in those cells is recycled for the production of new erythrocytes. Owing to a shorter half-life of circulating erythrocytes in iron deficiency anemia, iron is recovered sooner in those patients, but the amount of iron in each microcytic erythrocyte is reduced (Macdougall et al. 1970). In the event of hemorrhage, additional iron must be absorbed from the diet to meet the steady-state demands of the host.
Figure 1.
Iron homeostasis in humans. Each day, 20 mg of iron is recycled between circulating transferrin (Fe-Tf) and erythrocytes. This recycling pathway is supported by (A) intestinal iron absorption, (B) erythrophagocytosis, (C) hepatic iron stores, and (D) iron incorporation into hemoglobin. For more details, see Andrews 2008. (From Andrews 2008; reprinted, with permission, © American Society of Hematology.)
Erythrocytes and their precursors require large amounts of iron for the production of heme (Fig. 2) and hemoglobin. Iron is central to hemoglobin structure and function (Perutz 1982). The most immediate source of iron for erythroblasts is mono- or diferric transferrin, found in high concentrations in the plasma. Iron deficiency anemia is typically associated with low iron saturation of available transferrin. Iron is loaded onto diferric transferrin from three sources: the gut (diet), macrophages (recycled iron), and the liver (stored ferritin iron). In general, iron stores are reduced or lost before the host develops anemia. Therefore, dietary and erythrocyte-recycled iron must meet the demands for erythrocyte production. If iron losses continue, the newly produced erythrocytes will have decreased hemoglobin, causing the amount of iron provided by the same number of senescent erythrocytes to be reduced. Unlike thalassemia trait, increased numbers of erythrocytes are not produced in the iron-deficient state to compensate for the reduction in intracellular hemoglobin content. For this reason, reticulocytosis is usually not present. In the absence of major hemorrhage, iron deficiency anemia generally develops slowly over the course of months or years. Resolution of iron deficiency anemia may be equally slow depending on the availability of iron in the diet as well as the adequacy of gastrointestinal function.
Figure 2.
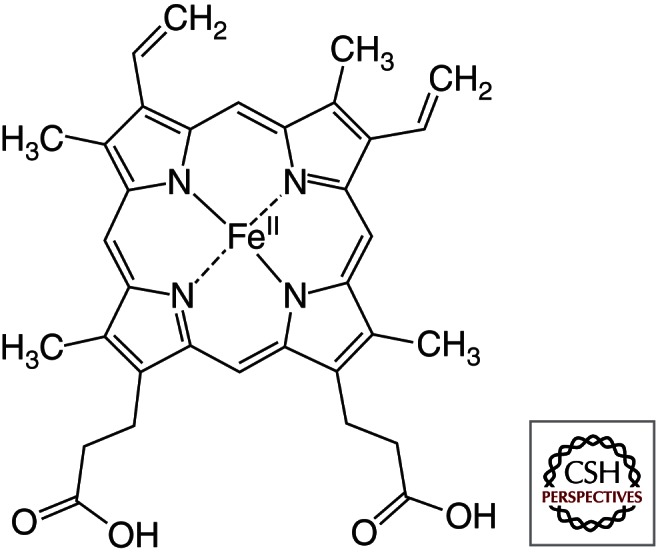
The heme B molecule. (The image is a public domain illustration from Wikipedia and can be found at http://commons.wikimedia.org/wiki/File:Heme_b.svg.)
For decades, it has been possible to diagnose and fully reverse the anemia of iron deficiency at a relatively low cost. Unfortunately, iron deficiency has maintained itself as the most common anemia and nutritional disorder worldwide. This seemingly inexplicable paradox of high prevalence despite effective treatment represents a major challenge to public health efforts. Multiple obstacles involving economics, cultural barriers, and infectious diseases converge and make eradication of this disease more difficult. The additional challenges that are encountered by certain human subpopulations in select geographies need to be overcome to achieve therapeutic success in the global community.
THE MAGNITUDE OF THE PROBLEM
30%–50% of anemia in children and other groups is caused by iron deficiency (World Health Organization 2007). Because 1.6 billion people are anemic (McLean et al. 2009), several hundred million manifest iron deficiency anemia. As such, iron deficiency is the most common cause of anemia worldwide. Iron deficiency anemia afflicts a subset of the two billion people worldwide who are nutritionally iron deficient (Viteri 1998). Therefore, the health burden of iron deficiency may be extrapolated from the global prevalence of anemia. Anemia is not distributed evenly throughout the world, as there is a fivefold increase in underdeveloped geographies. In some global regions, the prevalence of anemia among young children is >50% (Table 1) and even approaches 100% in some locales (Lutter 2008). In the same regions, 40%–50% of the population remains anemic at all ages with the exception of nonelderly men (McLean et al. 2009). By comparison, the disease burden is far less in developed nations. In the United States, the prevalence of anemia as a result of iron deficiency is reduced among all age and gender groups (Clark 2008). However, approximately 10 million people are iron deficient in the United States, including 5 million who have iron deficiency anemia.
Table 1.
Prevalence of anemia in infants and young children (birth to 5 years of age)
| Global region | Prevalence (%) |
|---|---|
| Africa | 64.6 |
| Asia | 47.7 |
| Europe | 16.7 |
| Latin America | 39.5 |
| North America | 3.4 |
| Oceania | 28.0 |
Data adapted from McLean et al. 2009.
RECOGNIZING IRON DEFICIENCY ANEMIA
The clinical constellation of signs and symptoms for this disease depends largely on the magnitude of the anemia. Hemoglobin values used for the definition of anemia vary according to age, sex, race, and whether the blood was sampled from the capillary (finger stick) or venous (phlebotomy) source (Newman 2006; Cable et al. 2011a). In the absence of automated testing, portable devices or visual matching of hemoglobin color have been proven to be 95% accurate for identifying the hemoglobin level within 1–2 g/dL of reference values (Ingram and Lewis 2000; Lewis and Emmanuel 2001). Patients may complain of poor mental performance or cold intolerance (Rosenzweig and Volpe 1999). Fatigue and exercise-associated dyspnea are regularly reported. Although rare, glossitis or dysphagia may be identified at presentation (Cook 2005; Novacek 2006). Recognition of these features may trigger appropriate laboratory tests and therapy.
Iron deficiency anemia is associated with some rather striking neurological sequelae. Some subjects possess the compulsion to move their lower extremities while at rest. The restless leg syndrome is now recognized as a reversible symptom of reduced brain iron levels that is particularly prevalent during pregnancy (Vivarelli et al. 1976; Goodman et al. 1988). Pica is another associated neurological comorbidity. Pica is defined as dietary compulsions for materials that may not usually be consumed in the diet of humans without iron deficiency. Pica, specifically geophagia, has been reported in a majority of pregnant African women living in regions where iron deficiency anemia is extremely common (Njiru et al. 2011). The molecular basis for this unusual behavior is unknown. Iron deficiency is also known to cause cognitive dysfunction. Neurological damage is particularly relevant during infancy brain development. Long-lasting cognitive challenges occur despite therapy later in life (Lozoff et al. 1991). Therefore, iron deficiency anemia during infancy should be aggressively treated to avoid the potential for cognitive problems.
Laboratory evaluation reveals characteristic changes in blood parameters for iron regulation storage, transport, and utilization. Hepcidin is the main regulator of iron in humans. Unfortunately, interlaboratory variation and lack of adequate standards have muted the advance of hepcidin assays in clinical care (Kroot et al. 2009). Research studies suggest that low or absent hepcidin levels may be diagnostic of simple iron deficiency (Tanno et al. 2010).
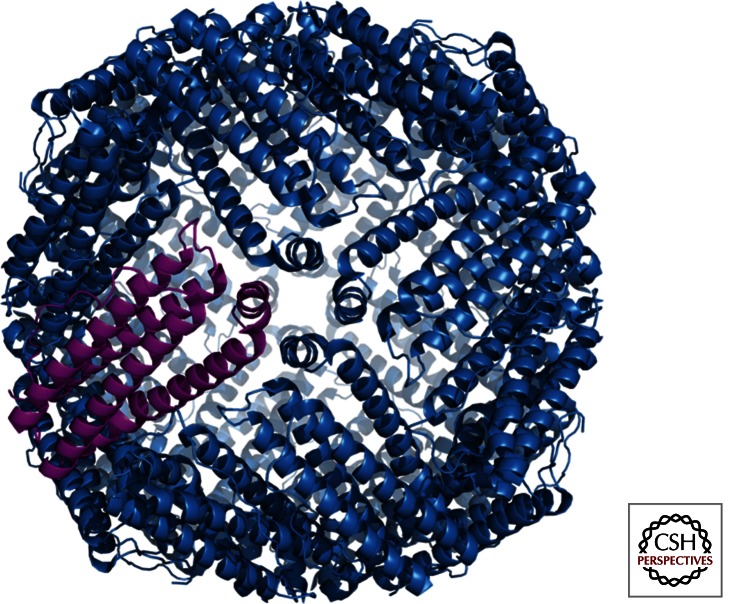
Currently, the central parameter for determination of significant iron deficiency as well as therapeutic response is ferritin (Mei et al. 2005; O’Meara et al. 2011). The ferritin protein complex structure acts as a cage to contain up to 4500 iron molecules (Fig. 3) (Harrison and Arosio 1996). A serum ferritin level of 15 μg/L or less is diagnostic of iron deficiency, and correlates specifically with the absence of stainable bone marrow iron (Baker 2000). Even at higher ferritin levels, ∼40 μg/L, erythropoiesis may be affected. Iron deficiency also causes increased release of soluble transferrin from erythroblasts. Therefore, ratios of soluble transferrin receptor and ferritin are used to detect iron-deficient erythropoiesis (Cable et al. 2011b). When significant inflammation is present, serum ferritin levels may not reflect accurate iron stores. In patients with chronic renal disease, ferritin levels of >400 μg/L are regularly detected in the absence of significant marrow iron stores (Rocha et al. 2009).
Figure 3.
Three-dimensional ribbon representation of the ferritin protein cage. (The image is a public domain illustration from Wikipedia and can be found at http://commons.wikimedia.org/wiki/File:Ferritin.png.)
As expected, serum iron levels are reduced in iron deficiency anemia. Transferrin protein expression increases in iron-deficient states, so the iron saturation on transferrin is reduced to values of <15%. Notably, apoferric and monoferric transferrin are the dominant species, and relatively minor amounts of diferric iron are present in the plasma (Finch and Huebers 1982). The reduction of diferric iron is pertinent for erythropoiesis owing to the relative levels and saturation kinetics of transferrin receptors on erythroblasts (Cazzola et al. 1987).
In addition to iron parameters, a lack of iron has measurable effects on erythropoiesis and erythroid cells. Low reticulocyte hemoglobin content is derived from reduced hemoglobin production, and may be useful for screening infants and children for iron deficiency (Brugnara et al. 1999; Ullrich et al. 2005). However, thalassemia mutations may confound the interpretation of reticulocyte hemoglobin quantitation (Mast et al. 2002). Iron deficiency accounts for increased production of zinc protoporphyrin in association with decreased heme production during erythroblast maturation. Ratios of these two parameters may be quantified using washed erythrocytes. Although values >40 moles of zinc protoporphyrin per mole heme denote an iron-deficient state (Hastka et al. 1992), the presence of a recent illness may reduce the sensitivity of this test (Crowell et al. 2006).
The manifestation of anemia or microcytosis is usually somewhat delayed relative to the loss of body iron stores. About 1% of erythrocytes are replaced daily, and the recycling of iron from the senescent cells continues to support the production of new cells. Eventually, the complete blood count (CBC) will reflect the effects on erythropoiesis. A combination of increased red cell distribution width (RDW), decreased red blood cell (RBC) count, decreased RBC hemoglobin, and decreased mean cell volume may be manifested. Unless the iron deficiency is reversed, the hemoglobin and hematocrit levels decrease to sufficiently low levels to be classified as anemia.
MAJOR CAUSES OF IRON DEFICIENCY ANEMIA
Blood Loss
Each milliliter of packed RBCs (∼2.5 mL of whole blood) contains ∼1.0 mg of iron. Each day, 1.0 mg of iron is absorbed from the diet and 20 mg of iron from senescent erythrocytes are available to support erythropoiesis. Once iron stores are depleted, dietary and recycled erythrocyte iron are not usually sufficient to compensate for acute blood loss.
In all cases of iron deficiency anemia, blood loss should be considered. Hemorrhage itself is by far the most common mechanism for acute iron loss and anemia. Hemorrhage decreases the host’s red cell mass, decreases the supply of iron for erythropoiesis, and increases the iron demand for erythropoiesis. Chronic blood loss from menstruation or hookworm infection (see below) has the greatest impact worldwide. Less than 2 mL of blood is lost daily in the stool of healthy adults (Ahlquist et al. 1985). Detection of occult blood losses of up to 60 mL/d may be difficult without specialized stool tests (Rockey 1999). Bleeding may occur from multiple sites along the intestinal tract, with an increased incidence of bleeding from the colon (Lanas et al. 2009). Sometimes overlooked causes of blood loss include blood donation and nosebleeds. Intravascular hemolysis with hemoglobinuria such as occurs in malaria results in iron loss in the absence of hemorrhage. After chronic physical exertion, significant iron is lost in sweat and may contribute to the deficient state (Reinke et al. 2010). A full history should be queried in all new cases of iron deficiency anemia.
The Maternal–Fetal Bridge of Iron Deficiency
Requirements for iron are greatest around the time of birth. Iron demand is high in menstruating as well as pregnant females. During pregnancy, it is estimated that ∼1200 mg of iron are required from conception through delivery (Lee and Okam 2011). Iron intake and stores in the mother must satisfy fetal development, and blood loss at delivery. Additionally, the maternal erythrocyte mass should increase from 350 to 450 mL. By comparison, pregnant women without iron supplements only increase their red cell mass by 180–250 mL (Pedersen and Milman 2003). One interpretation of this difference is that fetal iron demands are prioritized over the red cell mass of the mother. Postpartum, iron is lost as lactoferrin in breast milk. Those losses are balanced by the absence of menstruation in the lactating female.
Maternal iron deficiency anemia during pregnancy and the perinatal period have devastating effects on both the mother and child. In addition to the direct effects of anemia, reduced fetal brain maturation, pediatric cognitive defects, and maternal depression are associated with iron deficiency anemia (Black et al. 2011). The reversibility of cognitive defects caused at an early age by iron deficiency is unclear. Importantly, untreated iron deficiency in pregnant females will be passed to the infant. If left untreated during infancy, childhood, and adolescence, anemia and iron-associated cognitive defects may conceivably be passed between generations much like genetic traits. Unless the iron deficiency is treated at some stage of life, the cycle of iron deficiency from mother to child may remain unbroken for several generations.
In the fetus and during infancy, iron is required for the growth and development of all tissues. The human growth rate is almost logarithmic during this period (Anderson and Holford 2008). The hemoglobin and myoglobin requirements must be met before the accumulation of storage iron. Although serum ferritin levels are elevated in the fetus compared with the mother, the fetal iron stores correlate well with the iron stores of the mother (Milman et al. 1987). In anemic mothers with iron deficiency, the fetal ferritin levels remain 10 times higher than the maternal ferritin at the time of delivery (Erdem et al. 2002). At birth, the fetal red cell mass is ∼50 mL/kg (Phillips et al. 1986), compared with 25–30 mL/kg in adults (Fairbanks et al. 1996). During the first year of postnatal life, total-body iron increases by ∼240 mg (Oski 1993). Around 80% of that iron is used for expanded hemoglobin production (50%) and iron stores (30%). Beyond the first year, iron intake or stores must remain sufficient to support the ongoing growth and increased red cell mass (Moser et al. 2011). In children and young adults, iron deficiency remains one of the top three contributors to the overall disease burden in those populations (Gore et al. 2011).
Malaria
Iron deficiency anemia and malaria coexist in most tropical regions of the world. Malaria contributes to iron deficiency anemia by causing intravascular hemolysis with subsequent loss of hemoglobin iron in the urine. This clinical feature was described in 1898 as blackwater fever (Connolly 1898). Malaria also causes an immune response that suppresses erythropoietin (Burgmann et al. 1996) as well as direct effects on erythropoiesis (Skorokhod et al. 2010). The host may also increase hepcidin expression for protection from liver-stage malaria (Portugal et al. 2011). Of course, increased hepcidin restricts iron and might delay erythroid recovery.
It is essential to understand the complex interplay between iron, hepcidin, and malaria when considering efforts to eradicate iron deficiency in malaria-endemic regions. If iron redistribution by hepcidin is beneficial for malaria, restricted iron could benefit the infected host. This hypothesis may help explain the recent report of potential harm caused by iron supplementation among preschool children in malaria-endemic areas (Sazawal et al. 2006). In that study, iron and folic acid supplements were stopped owing to an increased risk for hospitalization or death from malaria in Zanzibar, Tanzania. Increased caution for iron supplementation in malaria-endemic regions was proposed (World Health Organization 2007). However, a recent Cochrane paper recommended, “iron supplementation should not be withheld from children living in malaria-endemic countries” (Okebe et al. 2011). Treatment of iron deficiency anemia is less clear in areas where access to proper malarial prevention and treatment are suboptimal. Further studies and resolution of this critical, but complex issue are awaited.
Hookworm
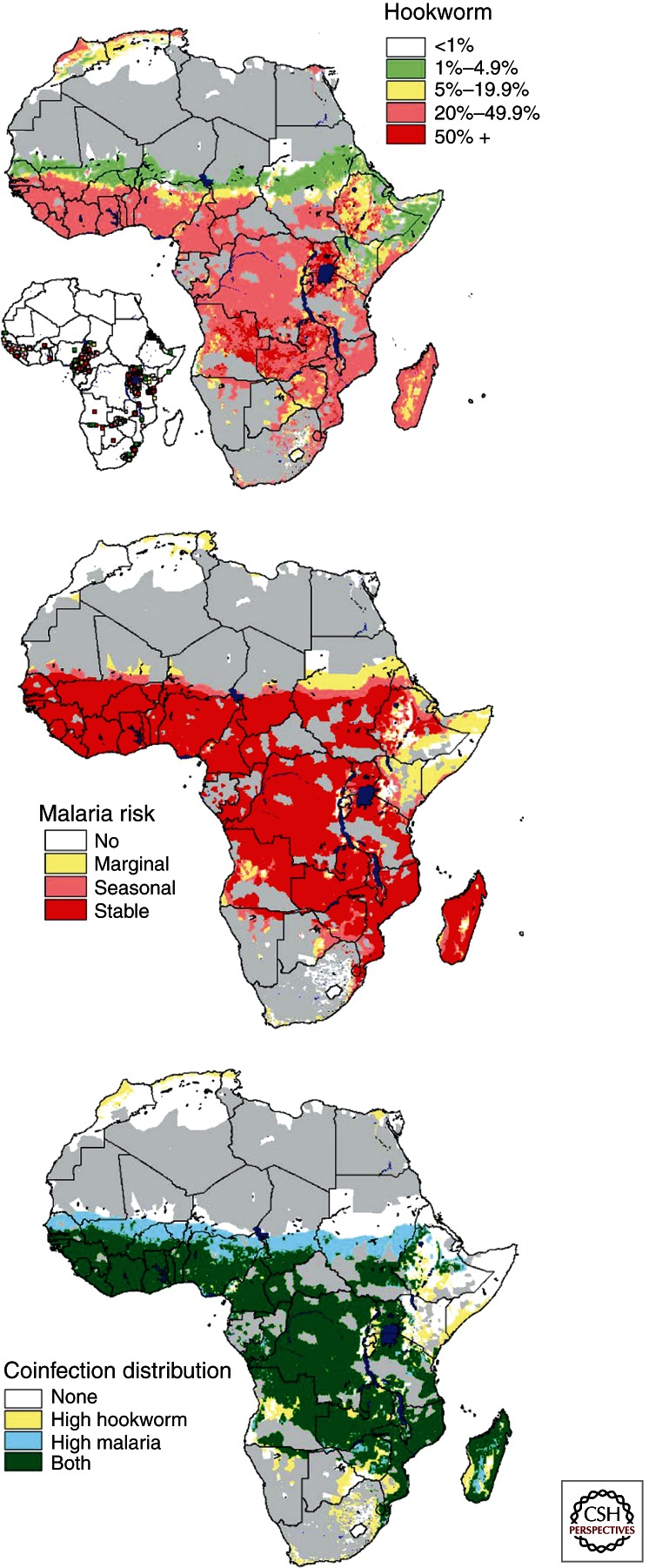
Like iron deficiency anemia, hookworm infection affects several hundred million humans worldwide (Bungiro and Cappello 2011). Amazingly, a recent study reported that there is a considerable overlap between malaria and hookworm in sub-Saharan Africa (Fig. 4) (Brooker et al. 2006). Worldwide, there are two hookworm species that infect humans. Both are found in tropical regions based on the requirement of moist soil for survival. The worm is introduced to the soil by fecal matter in regions where sanitation is not present. From the soil, the parasite accesses the duodenum of a new human host directly by mouth, or indirectly via the skin. Once in the gut, the worm may be retained for several years as it releases eggs in the stool. A hookworm infection should be suspected in cases of travel or habitation in the tropics, iron deficiency anemia, and mild eosinophilia. Owing to their location in the small bowel, capsule endoscopy is helpful for diagnosis if eggs are not present in the stool (Li et al. 2007). Hookworms live on 0.3–0.5 mL of blood extravasated daily from the intestinal mucosa. Heavily infected patients are simply unable to maintain adequate iron stores and become anemic (Smith and Brooker 2010). Even without additional iron supplements, antihelminthic drugs can cause reversal of iron deficiency anemia (Radhika et al. 2011). It is currently unknown whether hookworm infection causes increased production of hepcidin in the host.
Figure 4.
Map of hookworm (top), Plasmodium falciparum (middle), and overlapping (bottom) prevalence. (From Brooker et al. 2006; reprinted, with express permission, from BioMed Central Ltd., © 2006.)
Diet and Malabsorption of Iron
Local economics generally dictate the level of nutrition worldwide. The diet, by itself, infrequently causes iron deficiency anemia in the absence of severe malnourishment or a comorbidity. A vegan diet is usually sufficient to prevent anemia even though the iron stores of the host may be low (Craig 1994). The diet becomes far more relevant when the iron stores are lost, or anemia has already developed, and the host requires additional iron absorption from the gut for recovery. This occurs in the multiple settings described earlier in this work: blood loss, rapid growth during infancy, malaria, and hookworm. In these settings, the diet and iron supplements become critical for maintaining iron availability. Supplemental dietary iron may be needed, because the average Western diet is not sufficient to meet the needs of pregnancy (Lee and Okam 2011). In addition to the iron content itself, the bioavailability of iron for absorption depends largely on the dietary components (Sharp 2010). Iron in the form of heme is especially bioavailable, and meat-containing diets are also beneficial (López and Martos 2004). Vitamin C improves dietary availability of iron as well as avoidance of tea or other iron-chelating substances (Thankachan et al. 2008). Numerous approaches are being tried to improve iron availability in the diet with a goal of low-cost and culturally acceptable implementation among the underprivileged (Hurrell et al. 2004).
In addition to the dietary components, the gut must be able to absorb iron to prevent or treat iron deficiency anemia. Inorganic iron absorption requires multiple mechanisms for entry and exit from duodenal and jejunal epithelial cells (Fig. 1). In cases of suspected malabsorption, a simple oral iron absorption test may prevent or direct more invasive studies (Alleyne et al. 2008). If the host’s hepcidin expression is increased, inorganic iron from the diet will not be optimally absorbed into the blood from the intestine. Instead, that iron will be trapped in the intestinal epithelial cells, and then sloughed into the lumen and stool (Anderson et al. 2009). Therefore, infections, inflammation, or other hepcidin up-regulating mechanisms are likely to inhibit nonheme iron absorption despite a high bioavailability in the diet. Other diseases, including helicobacter infections (Vitale et al. 2011), bariatric surgery (Shankar et al. 2010), or decreased gastrin (Kovac et al. 2011) can inhibit iron absorption. Finally, celiac disease is a common cause of anemia owing to low iron absorption from the gut (Presutti et al. 2007). There is a high incidence (15%) of celiac sprue among the subjects who undergo endoscopy for evaluation of iron deficiency anemia (Oxentenko et al. 2002).
SOLVING THE GLOBAL PROBLEM
Iron Fortification
Iron fortification remains the mainstay of efforts aimed toward the treatment or prevention of iron deficiency anemia. As a general rule, menstruating and pregnant women along with their children clearly represent the largest at-risk population for this disease. In the underdeveloped world, iron may be provided with other micronutrients to reduce anemia in schoolchildren (Ahmed et al. 2010; Best et al. 2011; Lemaire et al. 2011). In-home food preparations with iron supplements present an alternate to industrial scale supplementation of grains or commercial food products (Lynch 2011). Numerous oral preparations and dosing regimens are available for menstruating and pregnant females (Fernández-Gaxiola and De-Regil 2011). Recently, intravenous iron preparations with improved toxicity profiles have been used for cases where rapid therapy was useful in reducing the need for transfusion (Gozzard 2011). Based on the large amount of iron that is provided with intravenous therapy, special care should be given toward dosing to prevent iatrogenic iron overload. As a general rule, therapy should be continued only until the anemia is resolved and iron stores are replenished. These goals are met with a normal hematocrit and serum ferritin level of 50–100 μg/L (corresponding to ∼400 –800 mg iron in stores for otherwise healthy adults) (Walters et al. 1973; Magnussen et al. 2008).
Delayed Clamping of the Umbilical Cord
Special attention must be given toward preventing iron deficiency in the newborn. In addition to maternal iron supplements, the simple maneuver of delayed umbilical cord clamping might help achieve this goal. In 1954, delayed umbilical cord clamping was found to be a relatively benign procedure (Colozzi 1954). The potential benefit of placental transfusion as an iron source was not initially considered. By the 1960s it was shown that placental transfusion causes a significant increase in the red cell volume when clamping is delayed for several minutes. A delay of 5 min results in 166 mL of added blood volume for a 3.5 kg infant (Usher et al. 1963). Placental transfusion is also achieved by placing the newborn on the mother’s abdomen after vaginal delivery, and clamping the cord once it stops pulsating (Nelle et al. 1995). In cases of cesarean section or other clinical setting that may preclude delayed clamping, clamping near the placenta should increase the volume of blood delivered to the newborn (Daniel and Weerakkody 1996). In the 1990s, the benefit of delayed clamping for the purpose of preventing iron deficiency during the first 6 months of life was more clearly appreciated (Pisacane 1996). Widespread adaptation placental transfusion may have been prevented to date by unsupported concerns for polycythemia, hyperbilirubinemia, and increased blood viscosity (van Rheenen and Brabin 2004). Importantly, none of those concerns were realized by a 3 min delay in umbilical cord clamping at the time of delivery among 400 low-risk pregnancies (Andersson et al. 2011). Instead, neonatal anemia and iron parameters by 4 months of age were improved. None of the infants who had undergone delayed (>3 min) clamping had ferritin levels below 20 μg/L, versus decreased ferritin levels in 7.4% of subjects who had undergone clamping almost immediately after delivery. Overall, these studies suggest that some level of placental transfusion may be beneficial in most deliveries. Large, prospective multinational studies of this simple maneuver are needed to confirm these results. If those studies show a generic benefit toward preventing iron deficiency or anemia, then appropriate efforts should be made to widely institute placental transfusion via delayed umbilical cord clamping. This procedure may be particularly useful in underdeveloped communities, as it incurs little, if any, additional expense.
Understand Fundamental Iron Biology
It is predicted that advances in global therapy for iron deficiency anemia will be greatly assisted by basic research efforts. Perhaps the most significant advance in this regard is the discovery and development of hepcidin biology over the last decade (Ganz 2011). Hepcidin biology will undoubtedly evolve into applications for iron deficiency anemia among all world populations. For instance, the recognition that hepcidin expression is highly variable and influenced by a circadian rhythm should be advantageous in improving dosing regimens (Kemna et al. 2007). The kinetics of hepcidin expression in response to iron supplementation for iron deficiency remain largely unexplored as another research avenue aimed toward the optimization of therapy. Clinical comparisons of oral versus intravenous therapies will help determine if a rapid pulse of therapy can improve the chances of success for certain individuals or groups of patients.
Certain populations do not benefit from universal iron supplementation (Ghio 2011). With inherited hemochromatosis, the absorption of dietary iron increases. Some genetic variants are quite common, especially in northern Europeans (van Bokhoven et al. 2011). Although the clinical penetrance is quite variable in the most common forms of hereditary hemochromatosis, communal iron fortification for this group is generally not recommended. Another genetic disorder named thalassemia (see Fucharoen and Weatherall 2012; Gibbons 2012; Musallam et al. 2012; Nienhuis and Nathan 2012; Cao and Kan 2013; Higgs 2013; Thein 2013; Vichinsky 2013) has a more direct relationship with iron deficiency anemia, because both diseases are concentrated within malaria and hookworm-endemic regions of the world. Thalassemia is caused by mutations in the globin genes that lead to decreased production of hemoglobin. Interestingly, iron deficiency itself may affect the production of hemoglobin in α- thalassemia (O’Brien 1973). Thalassemia trait patients present with microcytosis similar to iron deficiency. Homozygous thalassemia mutations lead to iron overload in the host by mechanisms that are not fully understood. As such, it is essential to recognize thalassemia and avoid iron supplements in that population.
Recent basic discoveries of several important genes or mutations that modify iron metabolism should also be mentioned. Iron is regulated, in part, by a recently discovered gene named TMPRSS6 (Du et al. 2008). Mutations in that gene cause iron deficiency that is refractory to iron supplements (Cau et al. 2010). If patients with malaria or hookworm benefit from iron deficiency, then some populations may have evolved by incorporating mutations into this gene. Population-based studies will help determine if mutations in the TMPRSS6 gene could be confounding efforts to reverse iron deficiency in some global populations including those in sub-Saharan Africa.
As evidenced by the importance of iron for malarial pathogenesis, further research into the complex relationships between deprivation of iron for this pathogen and iron deficiency anemia are needed to determine the best course of therapy. Determination of hookworm effects on hepcidin expression should also be pursued. In populations afflicted with one or both of these parasites, efforts to supplement iron can be confounded by the host’s inflammatory response. Relationships between hookworm and intestinal iron absorption should be studied further, understood, and incorporated into eradication efforts. Ideally, strategies will be tested that incorporate vaccination, sanitation, malarial treatment, deworming, and iron supplements into the same research plan. Although such strategies seem ambitious in a world of limited resources, it is crucial to remember that hundreds of millions stand to benefit worldwide.
CONCLUDING REMARKS
Unlike other prevalent anemias and hemoglobinopathies, the diagnosis and treatment of iron deficiency anemia is achievable in most, if not all individuals. However, consideration of iron deficiency anemia must include the possible convergence of several causative factors. If resources are adequate, care must be given toward individualized approaches to therapy (Alleyne et al. 2008). In the underdeveloped world, more communal approaches are being taken to overcome the overlapping causes of iron deficiency anemia that affect hundreds of millions worldwide. Ultimately, it is predicted that increased research and understanding of fundamental iron biology will assist in devising new strategies aimed toward the global elimination of this disease.
ACKNOWLEDGMENTS
J.L.M. thanks his mentors, colleagues, and all members of his section at National Institutes of Health for their inspiration over the last 20 years.
Footnotes
Editors: David Weatherall, Alan N. Schechter, and David G. Nathan
Additional Perspectives on Hemoglobin and Its Diseases available at www.perspectivesinmedicine.org
REFERENCES
*Reference is also in this collection.
- Ahlquist DA, McGill DB, Schwartz S, Taylor WF, Owen RA 1985. Fecal blood levels in health and disease. A study using HemoQuant. N Engl J Med 312: 1422–1428 [DOI] [PubMed] [Google Scholar]
- Ahmed F, Khan MR, Akhtaruzzaman M, Karim R, Williams G, Torlesse H, Darnton-Hill I, Dalmiya N, Banu CP, Nahar B 2010. Long-term intermittent multiple micronutrient supplementation enhances hemoglobin and micronutrient status more than iron + folic acid supplementation in Bangladeshi rural adolescent girls with nutritional anemia. J Nutr 140: 1879–1886 [DOI] [PubMed] [Google Scholar]
- Alleyne M, Horne MK, Miller JL 2008. Individualized treatment for iron-deficiency anemia in adults. Am J Med 121: 943–948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson BJ, Holford NH 2008. Mechanism-based concepts of size and maturity in pharmacokinetics. Annu Rev Pharmacol Toxicol 48: 303–332 [DOI] [PubMed] [Google Scholar]
- Anderson GJ, Frazer DM, McLaren GD 2009. Iron absorption and metabolism. Curr Opin Gastroenterol 25: 129–135 [DOI] [PubMed] [Google Scholar]
- Andersson O, Hellström-Westas L, Andersson D, Domellöf M 2011. Effect of delayed versus early umbilical cord clamping on neonatal outcomes and iron status at 4 months: A randomised controlled trial. BMJ 343: d7157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews NC 2008. Forging a field: The golden age of iron biology. Blood 112: 219–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker WF Jr 2000. Iron deficiency in pregnancy, obstetrics, and gynecology. Hematol Oncol Clin North Am 14: 1061–1077 [DOI] [PubMed] [Google Scholar]
- Best C, Neufingerl N, Del Rosso JM, Transler C, van den Briel T, Osendarp S 2011. Can multi-micronutrient food fortification improve the micronutrient status, growth, health, and cognition of schoolchildren? A systematic review. Nutr Rev 69: 186–204 [DOI] [PubMed] [Google Scholar]
- Black MM, Quigg AM, Hurley KM, Pepper MR 2011. Iron deficiency and iron-deficiency anemia in the first two years of life: Strategies to prevent loss of developmental potential. Nutr Rev 69: S64–S70 [DOI] [PubMed] [Google Scholar]
- Brooker S, Clements AC, Hotez PJ, Hay SI, Tatem AJ, Bundy DA, Snow RW 2006. The co-distribution of Plasmodium falciparum and hookworm among African schoolchildren. Malar J 5: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brugnara C, Zurakowski D, DiCanzio J, Boyd T, Platt O 1999. Reticulocyte hemoglobin content to diagnose iron deficiency in children. JAMA 281: 2225–2230 [DOI] [PubMed] [Google Scholar]
- Bungiro R, Cappello M 2011. Twenty-first century progress toward the global control of human hookworm infection. Curr Infect Dis Rep 13: 210–217 [DOI] [PubMed] [Google Scholar]
- Burgmann H, Looareesuwan S, Kapiotis S, Viravan C, Vanijanonta S, Hollenstein U, Wiesinger E, Presterl E, Winkler S, Graninger W 1996. Serum levels of erythropoietin in acute Plasmodium falciparum malaria. Am J Trop Med Hyg 54: 280–283 [DOI] [PubMed] [Google Scholar]
- Cable RG, Steele WR, Melmed RS, Johnson B, Mast AE, Carey PM, Kiss JE, Kleinman SH, Wright DJ, for the NHLBI Retrovirus Epidemiology Donor Study-II (REDS-II) 2011a. The difference between fingerstick and venous hemoglobin and hematocrit varies by sex and iron stores. Transfusion 52: 1031–1040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cable RG, Glynn SA, Kiss JE, Mast AE, Steele WR, Murphy EL, Wright DJ, Sacher RA, Gottschall JL, Tobler LH, et al. 2011b. Iron deficiency in blood donors: The REDS-II Donor Iron Status Evaluation (RISE) study. Transfusion 52: 702–711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Cao A, Kan YW 2013. The prevention of thalassemia. Cold Spring Harb Perspect Med 3: a011775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cau M, Melis MA, Congiu R, Galanello R 2010. Iron-deficiency anemia secondary to mutations in genes controlling hepcidin. Expert Rev Hematol 3: 205–216 [DOI] [PubMed] [Google Scholar]
- Cazzola M, Pootrakul P, Bergamaschi G, Huebers HA, Eng M, Finch CA 1987. Adequacy of iron supply for erythropoiesis: In vivo observations in humans. J Lab Clin Med 110: 734–739 [PubMed] [Google Scholar]
- Clark SF 2008. Iron deficiency anemia. Nutr Clin Pract 23: 128–141 [DOI] [PubMed] [Google Scholar]
- Colozzi AE 1954. Clamping of the umbilical cord; its effect on the placental transfusion. N Engl J Med 250: 629–632 [DOI] [PubMed] [Google Scholar]
- Connolly RM 1898. African Haemoglobinuric fever, commonly called Blackwater Fever. Br Med J 2: 882–885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook JD 2005. Diagnosis and management of iron-deficiency anaemia. Best Pract Res Clin Haematol 18: 319–332 [DOI] [PubMed] [Google Scholar]
- Craig WJ 1994. Iron status of vegetarians. Am J Clin Nutr 59: 1233S–1237S [DOI] [PubMed] [Google Scholar]
- Crowell R, Ferris AM, Wood RJ, Joyce P, Slivka H 2006. Comparative effectiveness of zinc protoporphyrin and hemoglobin concentrations in identifying iron deficiency in a group of low-income, preschool-aged children: Practical implications of recent illness. Pediatrics 118: 224–232 [DOI] [PubMed] [Google Scholar]
- Daniel DG, Weerakkody AN 1996. Neonatal prevention of iron deficiency. Blood can be transfused from cord clamped at placental end. BMJ 312: 1102–1103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du X, She E, Gelbart T, Truksa J, Lee P, Xia Y, Khovananth K, Mudd S, Mann N, Moresco EM, et al. 2008. The serine protease TMPRSS6 is required to sense iron deficiency. Science 320: 1088–1092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erdem A, Erdem M, Arslan M, Yazici G, Eskandari R, Himmetoglu O 2002. The effect of maternal anemia and iron deficiency on fetal erythropoiesis: Comparison between serum erythropoietin, hemoglobin and ferritin levels in mothers and newborns. J Matern Fetal Neonatal Med 11: 329–332 [DOI] [PubMed] [Google Scholar]
- Fairbanks VF, Klee GG, Wiseman GA, Hoyer JD, Tefferi A, Petitt RM, Silverstein MN 1996. Measurement of blood volume and red cell mass: Re-examination of 51Cr and 125I methods. Blood Cells Mol Dis 22: 169–186 [DOI] [PubMed] [Google Scholar]
- Fernández-Gaxiola AC, De-Regil LM 2011. Intermittent iron supplementation for reducing anaemia and its associated impairments in menstruating women. Cochrane Database Syst Rev 12: CD009218. [DOI] [PubMed] [Google Scholar]
- Finch CA, Huebers H 1982. Perspectives in iron metabolism. N Engl J Med 306: 1520–1528 [DOI] [PubMed] [Google Scholar]
- *.Fucharoen S, Weatherall DJ 2012. The hemoglobin E thalassemias. Cold Spring Harb Perspect Med 2: a011734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganz T 2011. Hepcidin and iron regulation, 10 years later. Blood 117: 4425–4433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghio AJ 2011. Anemia and global iron fortification and supplementation. Ann Hematol 91: 957–958 [DOI] [PubMed] [Google Scholar]
- *.Gibbons RJ 2012. α-Thalassemia, mental retardation, and myelodysplastic syndrome. Cold Spring Harb Perspect Med 2: a011759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman JD, Brodie C, Ayida GA 1988. Restless leg syndrome in pregnancy. BMJ 297: 1101–1102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gore FM, Bloem PJ, Patton GC, Ferguson J, Joseph V, Coffey C, Sawyer SM, Mathers CD 2011. Global burden of disease in young people aged 10–24 years: A systematic analysis. Lancet 377: 2093–2102 [DOI] [PubMed] [Google Scholar]
- Gozzard D 2011. When is high-dose intravenous iron repletion needed? Assessing new treatment options. Drug Des Devel Ther 5: 51–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison PM, Arosio P 1996. The ferritins: Molecular properties, iron storage function and cellular regulation. Biochim Biophys Acta 1275: 161–203 [DOI] [PubMed] [Google Scholar]
- Hastka J, Lasserre JJ, Schwarzbeck A, Strauch M, Hehlmann R 1992. Washing erythrocytes to remove interferents in measurements of zinc protoporphyrin by front-face hematofluorometry. Clin Chem 38: 2184–2189 [PubMed] [Google Scholar]
- *.Higgs DR 2013. The molecular basis of α-thalassemia. Cold Spring Harb Perspect Med 3: a011718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurrell RF, Lynch S, Bothwell T, Cori H, Glahn R, Hertrampf E, Kratky Z, Miller D, Rodenstein M, Streekstra H, et al. 2004. Enhancing the absorption of fortification iron. A SUSTAIN Task Force report. Int J Vitam Nutr Res 74: 387–401 [DOI] [PubMed] [Google Scholar]
- Ingram CF, Lewis SM 2000. Clinical use of WHO haemoglobin colour scale: Validation and critique. J Clin Pathol 53: 933–937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemna EH, Tjalsma H, Podust VN, Swinkels DW 2007. Mass spectrometry-based hepcidin measurements in serum and urine: Analytical aspects and clinical implications. Clin Chem 53: 620–628 [DOI] [PubMed] [Google Scholar]
- Kovac S, Anderson GJ, Alexander WS, Shulkes A, Baldwin GS 2011. Gastrin-deficient mice have disturbed hematopoiesis in response to iron deficiency. Endocrinology 152: 3062–3073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroot JJ, Kemna EH, Bansal SS, Busbridge M, Campostrini N, Girelli D, Hider RC, Koliaraki V, Mamalaki A, Olbina G, et al. 2009. Results of the first international round robin for the quantification of urinary and plasma hepcidin assays: Need for standardization. Haematologica 94: 1748–1752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanas A, García-Rodríguez LA, Polo-Tomás M, Ponce M, Alonso-Abreu I, Perez-Aisa MA, Perez-Gisbert J, Bujanda L, Castro M, Muñoz M, et al. 2009. Time trends and impact of upper and lower gastrointestinal bleeding and perforation in clinical practice. Am J Gastroenterol 104: 1633–1641 [DOI] [PubMed] [Google Scholar]
- Lee AI, Okam MM 2011. Anemia in pregnancy. Hematol Oncol Clin North Am 25: 241–259, vii [DOI] [PubMed] [Google Scholar]
- Lemaire M, Islam QS, Shen H, Khan MA, Parveen M, Abedin F, Haseen F, Hyder Z, Cook RJ, Zlotkin SH 2011. Iron-containing micronutrient powder provided to children with moderate-to-severe malnutrition increases hemoglobin concentrations but not the risk of infectious morbidity: A randomized, double-blind, placebo-controlled, noninferiority safety trial. Am J Clin Nutr 94: 585–593 [DOI] [PubMed] [Google Scholar]
- Lewis SM, Emmanuel J 2001. Validity of the haemoglobin colour scale in blood donor screening. Vox Sang 80: 28–33 [DOI] [PubMed] [Google Scholar]
- Li ZS, Liao Z, Ye P, Wu RP 2007. Dancing hookworm in the small bowel detected by capsule endoscopy: A synthesized video. Endoscopy 39: E97. [DOI] [PubMed] [Google Scholar]
- López MA, Martos FC 2004. Iron availability: An updated review. Int J Food Sci Nutr 55: 597–606 [DOI] [PubMed] [Google Scholar]
- Lozoff B, Jimenez E, Wolf AW 1991. Long-term developmental outcome of infants with iron deficiency. N Engl J Med 325: 687–694 [DOI] [PubMed] [Google Scholar]
- Lutter CK 2008. Iron deficiency in young children in low-income countries and new approaches for its prevention. J Nutr 138: 2523–2528 [DOI] [PubMed] [Google Scholar]
- Lynch SR 2011. Why nutritional iron deficiency persists as a worldwide problem. J Nutr 141: 763S–768S [DOI] [PubMed] [Google Scholar]
- Macdougall LG, Judisch JM, Mistry SB 1970. Red cell metabolism in iron deficiency anemia. II. The relationship between red cell survival and alterations in red cell metabolism. J Pediatr 76: 660–665 [DOI] [PubMed] [Google Scholar]
- Magnussen K, Bork N, Asmussen L 2008. The effect of a standardized protocol for iron supplementation to blood donors low in hemoglobin concentration. Transfusion 48: 749–754 [DOI] [PubMed] [Google Scholar]
- Mast AE, Blinder MA, Lu Q, Flax S, Dietzen DJ 2002. Clinical utility of the reticulocyte hemoglobin content in the diagnosis of iron deficiency. Blood 99: 1489–1491 [DOI] [PubMed] [Google Scholar]
- McLean E, Cogswell M, Egli I, Wojdyla D, de Benoist B 2009. Worldwide prevalence of anaemia, WHO Vitamin and Mineral Nutrition Information System, 1993–2005. Public Health Nutr 12: 444–454 [DOI] [PubMed] [Google Scholar]
- Mei Z, Cogswell ME, Parvanta I, Lynch S, Beard JL, Stoltzfus RJ, Grummer-Strawn LM 2005. Hemoglobin and ferritin are currently the most efficient indicators of population response to iron interventions: An analysis of nine randomized controlled trials. J Nutr 135: 1974–1980 [DOI] [PubMed] [Google Scholar]
- Milman N, Ibsen KK, Christensen JM 1987. Serum ferritin and iron status in mothers and newborn infants. Acta Obstet Gynecol Scand 66: 205–211 [DOI] [PubMed] [Google Scholar]
- Moser AM, Urkin J, Shalev H 2011. Normal hemoglobin at the age of 1 year does not protect infants from developing iron deficiency anemia in the second year of life. J Pediatr Hematol Oncol 33: 467–469 [DOI] [PubMed] [Google Scholar]
- *.Musallam KM, Taher AT, Rachmilewitz EA 2012. β-Thalassemia intermedia: A clinical perspective. Cold Spring Harb Perspect Med 2: a013482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelle M, Zilow EP, Bastert G, Linderkamp O 1995. Effect of Leboyer childbirth on cardiac output, cerebral and gastrointestinal blood flow velocities in full-term neonates. Am J Perinatol 12: 212–216 [DOI] [PubMed] [Google Scholar]
- Newman B 2006. Iron depletion by whole-blood donation harms menstruating females: The current whole-blood-collection paradigm needs to be changed. Transfusion 46: 1667–1681 [DOI] [PubMed] [Google Scholar]
- *.Nienhuis AW, Nathan DG 2012. Pathophysiology and clinical manifestations of the β-thalassemias. Cold Spring Harb Perspect Med 2: a011726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Njiru H, Elchalal U, Paltiel O 2011. Geophagy during pregnancy in Africa: A literature review. Obstet Gynecol Surv 66: 452–459 [DOI] [PubMed] [Google Scholar]
- Novacek G 2006. Plummer-Vinson syndrome. Orphanet J Rare Dis 1: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien RT 1973. The effect of iron deficiency on the expression of hemoglobin H. Blood 41: 853–856 [PubMed] [Google Scholar]
- Okebe JU, Yahav D, Shbita R, Paul M 2011. Oral iron supplements for children in malaria-endemic areas. Cochrane Database Syst Rev CD006589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Meara A, Infanti L, Stebler C, Ruesch M, Sigle JP, Stern M, Buser A 2011. The value of routine ferritin measurement in blood donors. Transfusion 51: 2183–2188 [DOI] [PubMed] [Google Scholar]
- Oski FA 1993. Iron deficiency in infancy and childhood. N Engl J Med 329: 190–193 [DOI] [PubMed] [Google Scholar]
- Oxentenko AS, Grisolano SW, Murray JA, Burgart LJ, Dierkhising RA, Alexander JA 2002. The insensitivity of endoscopic markers in celiac disease. Am J Gastroenterol 97: 933–938 [DOI] [PubMed] [Google Scholar]
- Pedersen LM, Milman N 2003. Diagnostic significance of platelet count and other blood analyses in patients with lung cancer. Oncol Rep 10: 213–216 [PubMed] [Google Scholar]
- Perutz MF 1982. Nature of the iron-oxygen bond and control of oxygen affinity of the haem by the structure of the globin in haemoglobin. Adv Exp Med Biol 148: 31–48 [DOI] [PubMed] [Google Scholar]
- Phillips HM, Holland BM, Abdel-Moiz A, Fayed S, Jones JG, Turner TL, Wardrop CA, Cockburn F 1986. Determination of red-cell mass in assessment and management of anaemia in babies needing blood transfusion. Lancet 1: 882–884 [DOI] [PubMed] [Google Scholar]
- Pisacane A 1996. Neonatal prevention of iron deficiency. BMJ 312: 136–137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portugal S, Carret C, Recker M, Armitage AE, Gonçalves LA, Epiphanio S, Sullivan D, Roy C, Newbold CI, Drakesmith H, et al. 2011. Host-mediated regulation of superinfection in malaria. Nat Med 17: 732–737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Presutti RJ, Cangemi JR, Cassidy HD, Hill DA 2007. Celiac disease. Am Fam Physician 76: 1795–1802 [PubMed] [Google Scholar]
- Radhika MS, Nair KM, Kumar RH, Rao MV, Ravinder P, Reddy CG, Brahmam GN 2011. Micronized ferric pyrophosphate supplied through extruded rice kernels improves body iron stores in children: A double-blind, randomized, placebo-controlled midday meal feeding trial in Indian schoolchildren. Am J Clin Nutr 94: 1202–1210 [DOI] [PubMed] [Google Scholar]
- Reinke S, Taylor WR, Duda GN, von Haehling S, Reinke P, Volk HD, Anker SD, Doehner W 2010. Absolute and functional iron deficiency in professional athletes during training and recovery. Int J Cardiol 156: 186–191 [DOI] [PubMed] [Google Scholar]
- Rocha LA, Barreto DV, Barreto FC, Dias CB, Moysés R, Silva MR, Moura LA, Draibe SA, Jorgetti V, Carvalho AB, et al. 2009. Serum ferritin level remains a reliable marker of bone marrow iron stores evaluated by histomorphometry in hemodialysis patients. Clin J Am Soc Nephrol 4: 105–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockey DC 1999. Occult gastrointestinal bleeding. N Engl J Med 341: 38–46 [DOI] [PubMed] [Google Scholar]
- Rosenzweig PH, Volpe SL 1999. Iron, thermoregulation, and metabolic rate. Crit Rev Food Sci Nutr 39: 131–148 [DOI] [PubMed] [Google Scholar]
- Sazawal S, Black RE, Ramsan M, Chwaya HM, Stoltzfus RJ, Dutta A, Dhingra U, Kabole I, Deb S, Othman MK, et al. 2006. Effects of routine prophylactic supplementation with iron and folic acid on admission to hospital and mortality in preschool children in a high malaria transmission setting: Community-based, randomised, placebo-controlled trial. Lancet 367: 133–143 [DOI] [PubMed] [Google Scholar]
- Shankar P, Boylan M, Sriram K 2010. Micronutrient deficiencies after bariatric surgery. Nutrition 26: 1031–1037 [DOI] [PubMed] [Google Scholar]
- Sharp PA 2010. Intestinal iron absorption: Regulation by dietary and systemic factors. Int J Vitam Nutr Res 80: 231–242 [DOI] [PubMed] [Google Scholar]
- Skorokhod OA, Caione L, Marrocco T, Migliardi G, Barrera V, Arese P, Piacibello W, Schwarzer E 2010. Inhibition of erythropoiesis in malaria anemia: Role of hemozoin and hemozoin-generated 4-hydroxynonenal. Blood 116: 4328–4337 [DOI] [PubMed] [Google Scholar]
- Smith JL, Brooker S 2010. Impact of hookworm infection and deworming on anaemia in non-pregnant populations: A systematic review. Trop Med Int Health 15: 776–795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanno T, Rabel A, Lee YT, Yau YY, Leitman SF, Miller JL 2010. Expression of growth differentiation factor 15 is not elevated in individuals with iron deficiency secondary to volunteer blood donation. Transfusion 50: 1532–1535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thankachan P, Walczyk T, Muthayya S, Kurpad AV, Hurrell RF 2008. Iron absorption in young Indian women: The interaction of iron status with the influence of tea and ascorbic acid. Am J Clin Nutr 87: 881–886 [DOI] [PubMed] [Google Scholar]
- *.Thein SL 2013. The molecular basis of β-thalassemia. Cold Spring Harb Perspect Med 3: a011700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullrich C, Wu A, Armsby C, Rieber S, Wingerter S, Brugnara C, Shapiro D, Bernstein H 2005. Screening healthy infants for iron deficiency using reticulocyte hemoglobin content. JAMA 294: 924–930 [DOI] [PubMed] [Google Scholar]
- Usher R, Shepard M, Lind J 1963. The blood volume of the newborn infant and placental transfusion. Acta Paediatr 52: 497–512 [DOI] [PubMed] [Google Scholar]
- van Bokhoven MA, van Deursen CT, Swinkels DW 2011. Diagnosis and management of hereditary haemochromatosis. BMJ 342: c7251. [DOI] [PubMed] [Google Scholar]
- van Rheenen P, Brabin BJ 2004. Late umbilical cord-clamping as an intervention for reducing iron deficiency anaemia in term infants in developing and industrialised countries: A systematic review. Ann Trop Paediatr 24: 3–16 [DOI] [PubMed] [Google Scholar]
- *.Vichinsky EP 2013. Clinical manifestations of α-thalassemia. Cold Spring Harb Perspect Med 3: a011742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitale G, Barbaro F, Ianiro G, Cesario V, Gasbarrini G, Franceschi F, Gasbarrini A 2011. Nutritional aspects of Helicobacter pylori infection. Minerva Gastroenterol Dietol 57: 369–377 [PubMed] [Google Scholar]
- Viteri FE 1998. A new concept in the control of iron deficiency: Community-based preventive supplementation of at-risk groups by the weekly intake of iron supplements. Biomed Environ Sci 11: 46–60 [PubMed] [Google Scholar]
- Vivarelli E, Siracusa G, Mangia F 1976. A histochemical study of succinate dehydrogenase in mouse oocytes and early embryos. J Reprod Fertil 47: 149–150 [DOI] [PubMed] [Google Scholar]
- Walters GO, Miller FM, Worwood M 1973. Serum ferritin concentration and iron stores in normal subjects. J Clin Pathol 26: 770–772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization 2007. Conclusions and recommendations of the WHO consultation on prevention and control of iron deficiency in infants and young children in malaria-endemic areas. Food Nutr Bull 28: S621–S627 [DOI] [PubMed] [Google Scholar]