Summary
The technique of nidus embolization with N-butyl-2-cyanoacrylate (NBCA) glue is presented. The microcatheter is navigated into the nidus and the tip is set in a wedged position. A diluted mixture of NBCA in ethiodized oil (a 25 % mixture is mainly used) is injected very slowly, using complete column technique. Using this technique, the progression of glues in the nidus can be seen easily, which leads to improve accuracy and effectiveness of embolization. The mean blood pressure is maintained 15% to 20% below baseline for several days after the embolization to prevent hemorrhage caused by normal pressure breakthrough. We believe this technique is very useful and effective method for the treatment of arteriovenous malformations. However; considerable experience in this technique should be required.
Key words: cerebral arteriovenous malformation, embolization, NBCA
Introduction
Transarterial embolization is one of the useful method for the treatment of brain arteriovenous malformations (AVMs). The rate of eradication is low after embolization alone (5% to 10%)1,2,3,4, however, reducing the size and diminishing the anomalous flow of vascular malformation contribute to increase the chance of cure by surgical intervention or radiosurgery.
Various kinds of embolic materials has been used for embolization of AVMs, however, only cyanoacrylate adhesives has a potentiality to get permanent obliteration of embolized region 5. Isobutyl-2-cyanoacrylate (IBCA) was initially used, then it has been replaced by N-butyl 2-cyanoacrylate (NBCA) in the mid 1980s. Although it is very difficult to handle pure form of NBCA, polymerization time of NBCA can be prolonged by addition of io-phenydylate or ethiodized oil (Ethidol, Savage Laboratories, Melville, NJ), both of which are oil-based radiographic contrast agent and/or glacial acetic acid6. Using these methods, polymerization times ranging between 0.2 and 5 seconds can be achieved 6. Relatively higher concentrated NBCA glue (50% to 75%) was used for embolization of AVM in our institute before 1997, but effective obliteration could not be obtained. Therefore we have used a diluted NBCA/Ethidol mixture (normally 25% NBCA (Histoacryl; Braun Melsungen, Germany), 75% Ethiodol) for embolization since 1997, and successful results have been obtained 7.
In this paper, we describe our technique of AVM embolization and discuss the usefulness and pitfall of embolization with diluted NBCA glue.
Technique
The embolization procedure was performed under general anesthesia and systemic heparinization (5000 units in an intravenous bolus, followed by 1000 units per hour throughout the procedure). A No. 6 Fr. thin-wall guiding catheter was navigated in the cervical portion of either the internal carotid or vertebral artery, and positioned as close as technically feasible to the skull base. The guiding catheter is continuously flushed with heparinized saline (4000 units per litter) via an infusion pump. Provocative test was performed during diagnostic angiography in another session before embolization. When the tip of the microcatheter is positioned within the nidus, a super-selective angiogram is performed to evaluated the flow characteristics, angioarchitecture and venous outflow of the AVMs. According to the results of this angiogram, the rate of the mixture of NBCA in ethiodized oil appropriate for the particular AVM is determined. The ideal position of the microcatheter tip for embolization is in a wedged position within the nidus of the AVMs without proximal reflux of contrast during the pre-embolization test injection. Using this technique, flow arrest can be achieved, and the NBCA distal to the tip of the microcatheter has a prolonged polymerization time because it is not in contact with proximally inflowing blood. This allows very prolonged and relatively large injection to be achieved, with extremely good permeation of a brain AVM nidus.
Except the treatment of true fistula, a diluted mixture of Histoacryl in Ethidol (a 25% mixture is mainly used, varied from 20% to 33%) is prepared. Injection is performed very slowly, using complete column technique, filling the interstices of the nidus up to the draining vein. If glue pass through the nidus and into the draining vein, the injection is halted for 2 to 3 seconds and then resumed8,9. This technique stops when no further progression of glue into the nidus can be detected or reflux of glue proximal to the tip of the microcatheter is observed. At this point, the syringe is aspirated, and the microcatheter and guiding catheter are quickly removed as a unit. Depending on the size of the vascular malformation, a staged embolization is performed in most large or giant AVMs to reduce the risk of normal pressure breakthrough. After the embolization procedure is finished, systemic heparinization is reversed with protamine sulfate. The mean arterial blood pressure is maintained approximately 15% to 20% below baseline after embolization for several days. If there is angiographic evidence of untoward occlusion or marked strategy of a partially embolized AVM, then surgical resection of the residual AVM is performed as soon as possible. Systemic steroid therapy was performed, typically with dexamethasone, in an effort to minimize the expected inflammatory response to cyanoacrylate injection for a short while after embolization. Subsequent embolization is performed at approximately two to four weeks later, expecting the stabilization of the altered cerebral hemodynamics that occur for a while after embolization.
Illustrative cases
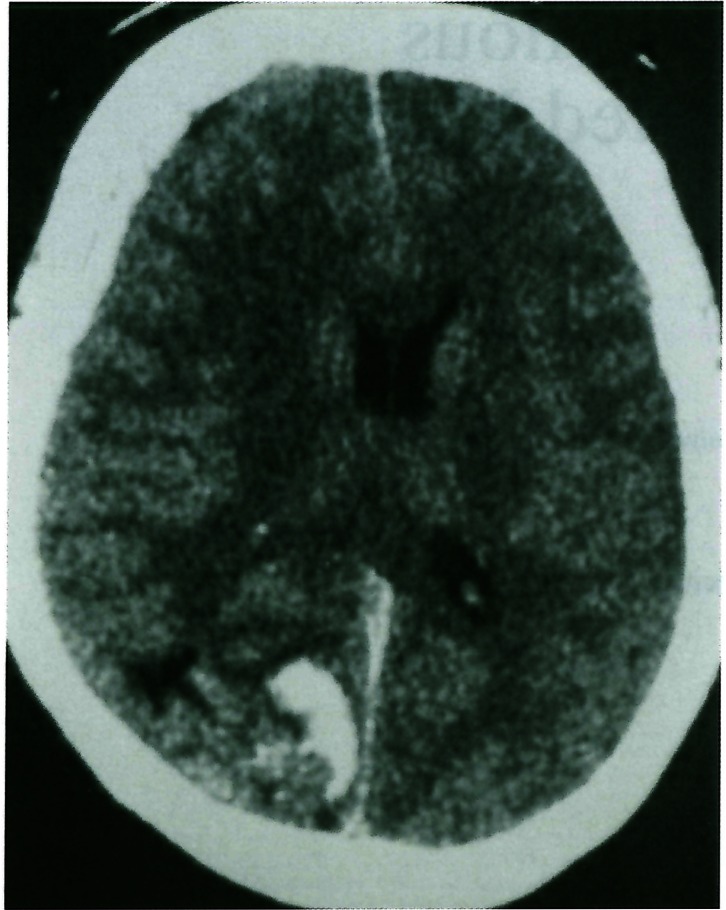
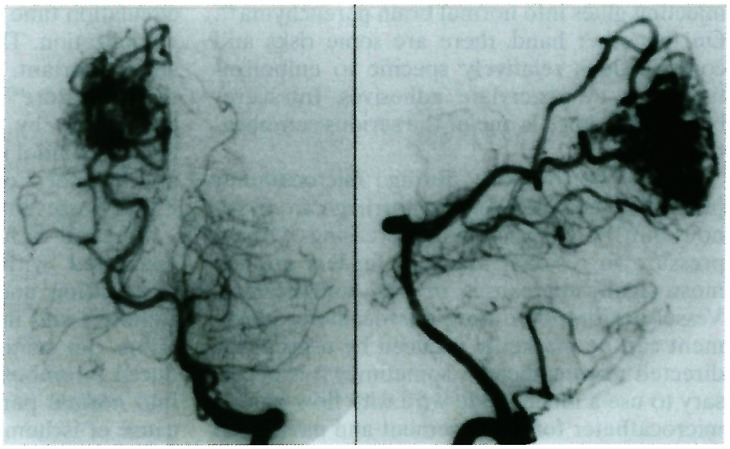
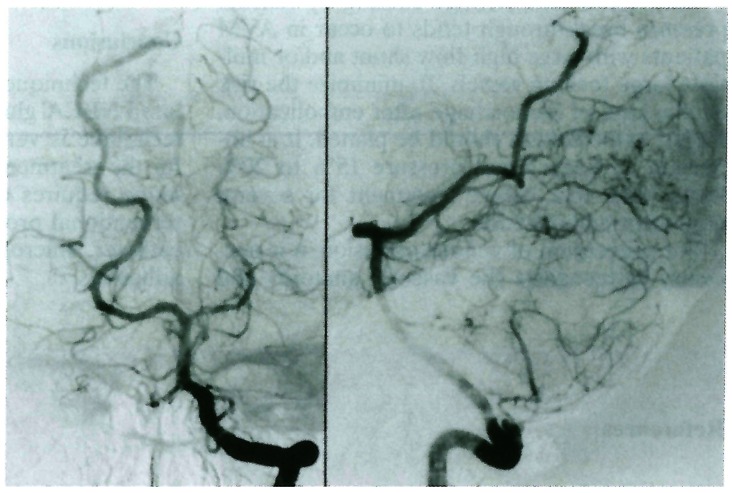
A 33-year-old woman was found to have a right occipital AVM. She suddenly presented disturbance of consciousness and was transferred to our hospital urgently. Initial CT scan demonstrated right occipital subcortical hematoma with subdural hematoma (figure 1).Tʼne diagnostic angiogram showed a Spetzler grade III AVM of right occipital lobe (figure 2). Embolization with 25% Histoacryl / Ethiodol mixture was performed and 99% obliteration of nidus was obtained (figure 3). Surgical intervention was performed after embolization and complete cure was obtained.
Figure 1.
Initial CT scan showing right occipital subcortical hematoma with acute subdural hematoma.
Figure 2.
Preembolization angiogram showing right occipital AVM.
Figure 3.
Postembolization angiogram showing slightly remained nidus with markedly reduced shunt flow.
Discussion
The goal of AVM treatment is to obtain complete obliteration or removal of the anomalous arterial-venous connection and to restore normal cerebral blood flow. Although surgical resection is the gold standard technique in treating AVMs, it may not be suitable for some patients because of anatomical factor or poor medical condition, and alternative methods of treatment may be indicated. Embolization is one of the alternative. Various embolic materials are available for the endovascular treatment of AVM, however, cyanoacrylate glue (NBCA) has several advantages over embolization with solid particle. NBCA is a vinyl monomer of alkyl 2-cyanoacrylate family that has been used as a tissue adhesive. It polymerizes on contact with ionic solutions such as contrast medium, saline or blood. Polymerization time of NBCA can be varied from almost immediate, when used in pure form, to a few seconds when mixed with Ethiodol or Pantopaque. The polymerization time is decided by several factors, such as the type of lesion, the transit time from the tip of catheter to the target, and the flow characteristics within the vessel to be embolized. In our institute, diluted mixture of Histoacryl (normally 25% Histoacryl, 75% Ethiodol) is mainly used for the majority of AVM cases, except for the marked fistulous lesion. Dilute mixture of Histoacryl has several advantages for the embolization of AVMs: 1) it is possible to inject glues extremely slowly and this leads to improve control and accuracy of the injection; 2) it is much easier to see the progression of glues in the nidus and visualize reflux along the microcatheter tip when it occurs, which can reduce the risk of permanently gluing the tip of the microcatheter and injecting glues into normal brain parenchyma8,9. On the other hand, there are some risks and complications relatively specific to embolization with cyanoacrylate adhesives. Intracerebral hemorrhage is one of the serious complications.
Vessel perforation during microcatheter placement and delayed hemorrhage from venous outflow obstruction or increasing of blood pressure in residual nidus or feeders are the most significant causes of this complication. Vessel perforation during microcatheter placement can be markedly reduced by using flow-directed microcatheters. Sometimes it is necessary to use a metal guide wire with flow-guided microcatheter for advancement and navigation in the feeder of an AVM. However, it is important that the guidewire is not extended beyond the tip of the microcatheter8,9.
Intracranial hemorrhage causing by normal pressure breakthrough tends to occur in AVM patients with large high-flow shunt and/or multiple large feeding vessels. To minimize the risk of this kind of hemorrhage after embolization, staged embolization should be planed. It is important to keep blood pressure 15% to 20% lower than that before treatment for several days after embolization.
For prevention of venous occlusion, it is necessary to recognize the vascular anatomy and circulation time through the AVM nidus before embolization. The method of injecting glue is also important. As Debrun et al described in their literature8,9, the risk of venous occlusion is minimized by injecting the diluted Histoacryl/Ethidol mixture slowly, and pausing the injection for 2 or 3 seconds and then resuming if glue passes into the draining vein.
Cerebral ischemia is another complication associated with embolization. Systemic heparinization and continuous flush of guiding catheters and microcatheters with heparinized saline can minimized the risk of catheter-induced thrombosis. Reflux of embolic materials into normal parenchymal branches is another cause of ischemic complication. It is necessary for minimizing this kind of risk to set the tip of the microcatheter in wedged position and to perform very slow injection of the dilute glue.
Conclusions
The technique of nidus embolization with diluted NBCA glue is presented. We believe this technique is very useful and effective method for the treatment of AVM. However, this technique requires considerable experience in interventional procedure, familiarity with microcatheter, microguidewires and cyanoacrylate adhesives.
References
- 1.Deruty R, Pelissou-Guyotat I, et al. The combined management of cerebral arteriovenous malformations. Experience with 100 cases and review of the literature. Acta Neurochir (Wien) 1993;123:101–112. doi: 10.1007/BF01401864. [DOI] [PubMed] [Google Scholar]
- 2.Fournier D, TerBrugge KG, et al. Endovascular treatment of intracranial arteriovenous malformations: Experience in 49 cases. J Neurosurg. 1991;75:228–233. doi: 10.3171/jns.1991.75.2.0228. [DOI] [PubMed] [Google Scholar]
- 3.Gobin YP, Laurent A, et al. Treatment of brain arteriovenous malformations by embolization and radiosurgery. J Neurosurg. 1996;85:19–28. doi: 10.3171/jns.1996.85.1.0019. [DOI] [PubMed] [Google Scholar]
- 4.Hurst RW, Berenstein A, et al. Deep central arteriovenous malformations of the brain: The role of endovascular treatment. J Neurosurg. 1995;82:190–195. doi: 10.3171/jns.1995.82.2.0190. [DOI] [PubMed] [Google Scholar]
- 5.Berenstein A, Lasjaunias P. Surgical Neuroangiography. Endovascular treatment of cerebral lesions. Vol. 4. Heidelberg: Springer Verlag; 1992. Technical aspects of surgical neuroangiography; pp. 189–266. Chapter 4. [Google Scholar]
- 6.Dion JE, Mathis JM. Polymerizing acrylic adhesive agents in interventional neuroradiology. In: Macinnas RJ, editor. Endovascular Neurological Intervention. Illinois: The American Association of Neurological Surgeons; 1995. pp. 139–158. [Google Scholar]
- 7.Tamatani S, Ito Y, et al. Efficacy of diluted NBCA mixture for embolization of arteriovenous malformations. Interventional Neuroradiology. 1999;5(Suppl 1):161–165. doi: 10.1177/15910199990050S129. [DOI] [PubMed] [Google Scholar]
- 8.Debrun GM, Aletich V, et al. Embolization of the nidus of brain arteriovenous malformations with n-butyl cyanoacrylate. Neurosurgery. 1997;40:112–121. [PubMed] [Google Scholar]
- 9.Aletich VM, Debrun GM. Intracranial arteriovenous malformation: The approach and technique of cyanoacrylate embolization. In: Connors III J J, Wajok JC, editors. Interventional Neuroradiology. Philadelphia: W.B. Saunders Company; 1999. pp. 240–258. [Google Scholar]