Summary
The purpose of this study was to evaluate asymptomatic embolisms during cerebral endovascular surgery for cerebrovascular diseases with diffusion-weighted magnetic resonance imaging (DWI) which allowed sensitive and early detection of cerebral ischemic lesions. 71 patients who underwent a total of 74 cerebral endovascular procedures were subjected to DWI screening study. MR imaging was performed on a 1.5T system by using single-shot SE echo-planar imaging (EPI) with b value of 1100 seconds per mm2 in pre-and post-treatment periods (between day 2 and 5 after procedures).
In 38 (51.3%) of 74 procedures, new high intensity lesions, as recent infarctions related to procedures, were detected on post-procedural DWI. In 18 Ofthe patients (47.4%), symptomatic infarctions occurred and resulted in TIAs (n = 4), RINDs (n = 8), minor strokes (n = 6) and no major strokes and no death. 20 (52.6%) of the recent infarctions detected by DWI were asymptomatic lesions. Most of the asymptomatic ischemic lesions were likely to be distributed in watershed border areas. On the other hand, symptomatic lesions tended to be distributed in cortical and/or perforator regions and to be multiple.
Thus, DWI is a useful method that can detect neurologically silent and asymptomatic ischemic lesions. It can be used to help to evaluate the safety and efficacy of neurovascular intervention.
Key words: complication, diffusion-weighted imaging, endovascular surgery, microembolism
Introduction
Cerebral infarction caused by dislodging a microembolus is a major problem during endovascular surgery on supraaortic arteries. Although some studies have demonstrated there is a risk of microembolism during cerebral endovascular surgery1,2, other studies have reported good results in endovascular treatments for cerebrovascular lesions3,4.
Therefore, it is possible that most of the microemboli dislodged during endovascular surgery result in only ischemic lesions without apparent neurological signs. Experimental and clinical reports have revealed that diffusion-weighted magnetic resonance imaging (DWI) allows sensitive and early detection of cerebral ischemic lesions5,6,7.
The purpose of this study was to evaluate asymptomatic embolisms during cerebral endovascular surgery for cerebrovascular diseases with DWI.
Subject and Methods
Seventy-one patients who underwent a total of 74 cerebral endovascular procedures underwent the DWI screening study Of them, 24 procedures were endosaccular embolization with detachable coils for cerebral aneurysms (IC cavernous portion: 2, IC C3:10, IC C2/3: 7, BA top: 5), 8 were parent artery occlusion for cerebral aneurysms (IC: 6, PICA: 1, Al: 1), 26 were carotid stenting, 5 were percunateous transluminar angioplasty (PTA) and/or stenting for stenosis of subclavian arteries, 5 were PTA and/or stenting for stenosis of vertebral arteries, 5 were PTA for stenosis of the basilar artery, and one was stenting for carotid stenosis caused by aortitis. Only two of these groups, carotid stenting and parent artery occlusion for cerebral aneurysms, had consecutive cases.
MR imaging was performed on a 1.5T system (MAGNETOM Vision, Siemens) by using single-shot SE echo-planar imaging (EPI) with Stejskal-Tanner diffusion-encoding gradient pairs along the through-plane direction with b value of 1100 seconds per mm2. Imaging parameters included a TE of 123, a field of view of 23 cm, a matrix of 128 × 200, a section thickness of 4 mm, and an intersection gap of 2 mm. Conventional SE imaging was also performed at each examination in Tl-and T2-weighted conditions. MR studies were performed in pre-and post-procedural periods. Because some studies have reported that acute ischemic lesions on DWI tended to decrease in intensity from day 6-7 after an ischemic event6,7, post-operative DWI studies were done between day 2 and 5 after procedures. A high intensity lesion detected on post-procedural DWI in the ipsilateral hemisphere but not on pre-procedural DWI, was considered to be a procedure-related infarction.
Results
In 38 (51.3%) of 74 procedures, new bright lesions, as recent infarctions related to endovascular procedures, were detected on post-procedural DWI studies. Of them, 18 procedures (47.4%) were symptomatic infarctions and resulted in TIAs (n = 4) , RINDs (n = 8), minor strokes (n = 6) and no major strokes and no death. The morbidity and mortality rate related to procedures was 8.1% in this study. Twenty (52.6%) of the recent infarctions detected by DWI were asymptomatic lesions.
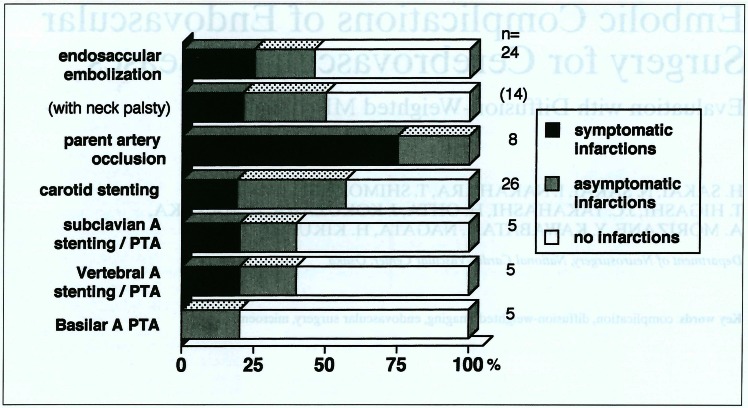
In the present study, the procedure with the highest incidence of procedure-related lesions detected on DWI was parent artery occlusion for cerebral aneurysm (100%, symptomatic: 75% and asyptomatic: 25%) (figure 1). In 15 (57.7%) of 26 carotid stentings, high intensity lesions were detected on post-procedural DWI. The incidence of ischemic lesions in endosaccular embolization for cerebral aneurysms was 45.8%, but there was no significant difference between those of aneurysmal coil embolization with or without neck plasty technique.
Figure 1.
The proportion of symptomatic and asymptomatic embolisms detected by diffusion-weighted imaging (DWI) in each procedure.
Most of the asymptomatic ischemic lesions on DWI were several small ones (< 5mm) located in subcortical white matter in watershed border areas (figure 2). Post-procedural X-ray CT scan rarely detected such small asymptomatic lesions. On the other hand, symptomatic lesions tended to be distributed in cortical and/or perforator regions and to be multiple. In 2 of 6 patients presenting minor strokes, their ischemic lesions were large territorial infarcts in ipsilateral hemispheres (figure 3), and the other 4 had multiple cortical and/or white matter infarcts.
Figure 2.
A case of asymptomatic embolism (59 year-old-male; right carotid stenting with a SMART stent). Post-procedural DWI (A) demonstrated bright intensity spots (indicated by arrows) in the watershed border zones of the right cerebral hemisphere. These lesions were not obviously distinguished from old infractions on FLAIR MR imaging (B) and not detected by X-ray CT (C).
Figure 3.
A representative case of symptomatic distal embolism (74 year-old-male; right carotid stenting with a Wallstent). Pre-treatment DWI (A) revealed no recent infarctions. DWI (B) two days after stenting demonstrated a large territorial infarction in the right frontal cortex.
Discussion
The most frequent and serious complications of endovascular treatments for cerebrovascular diseases are ischemic lesions caused by thromboembolic events. For safe neurointervention, it is necessary to evaluate their procedure-related embolic complications including not only symptomatic but asymptomatic ones. DWI appears to be the most sensitive modality for detecting early and small ischemic lesions5,6,7. In this study, DWI screening demonstrated that half of the ischemic lesions detected by DWI were neurologically silent or asymptomatic embolisms which could not be detected by CT. Recently, Bendszus et Al8 have reported that post-procedural DWI after routine diagnostic cerebral angiography and neurointerventions detected asymptomatic ischemic lesions in 25.8% and 17.6% of the patients, respectively. These findings differed from our results, because the intervention cases in their study included neither carotid stenting nor aneurysmal embolizations, whereas, unexpectedly the incidence of asymptomatic ischemic lesions in our study was high, compared with that of symptomatic infarctions. These results suggest that some countermeasures are required to prevent distal embolism in further endovascular treatments.
In the patients with insufficient cerebrovascular flow (CBF) such as parent artery occlusion and severe stenosis of bilateral carotid arteries, procedure-related cerebral infarctions were frequently detected on DWI after treatment. Moreover, asymptomatic embolisms also tended to be distributed in watershed border zones. These findings suggest that a distal embolus, when there was a corresponding global and/or regional decrease in CBF, was likely to occur in ischemic lesions, and so did not always result in infarctions. Therefore, for the reduction of embolic complications during neurointervention, it seems to be important to assess CBF in advance.
Conclusions
DWI was a useful method that can detect neurologically silent ischemic lesions during interventional procedures for cerebrovascular diseases. It can be used to help to evaluate the safety and efficacy of neurovascular intervention.
References
- 1.Crawley F, Clifton A, et al. Comparison of hemodynamic cerebral ischemia and microembolic signals detection during carotid endarterectomy and carotid angioplasty. Stroke. 1997;28:2460–2464. doi: 10.1161/01.str.28.12.2460. [DOI] [PubMed] [Google Scholar]
- 2.Fisher WS, Jordan WD. Carotid angioplasty. Surg Neurol. 1998;50:295–299. doi: 10.1016/s0090-3019(98)00005-6. [DOI] [PubMed] [Google Scholar]
- 3.Wholey MH, Wholey M, et al. Current global status of carotid artery stent placement. Cathet Cardiovasc Diagn. 1998;44:1–6. doi: 10.1002/(sici)1097-0304(199805)44:1<1::aid-ccd1>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 4.Murayama Y, Viñuela F, et al. Embolization of incidental cerebral aneurysms by using the Guglielmi detachable coil system. J Neurosurg. 1999;90:207–214. doi: 10.3171/jns.1999.90.2.0207. [DOI] [PubMed] [Google Scholar]
- 5.Warach S, Chien D, et al. Fast magnetic resonance diffusion-weighted imaging of acute human stroke. Neurology. 1992;17:1743–1748. doi: 10.1212/wnl.42.9.1717. [DOI] [PubMed] [Google Scholar]
- 6.Schlaug G, Siewert B, et al. Time course of the apparent diffusion coefficient (ADC) abnormality in human stroke. Neurology. 1997;49:113–119. doi: 10.1212/wnl.49.1.113. [DOI] [PubMed] [Google Scholar]
- 7.Yamada N, Imakita S, Sakuma T. Value of diffusion weighted image and apparent diffusion coefficient in recent cerebral infarction: a correlative study with gadolinium enhanced T1 weighted spine-echo. Am J Neuroradiol. 1999;20:193–198. [PMC free article] [PubMed] [Google Scholar]
- 8.Bendszus M, Koltzenburg M, et al. Silent embolism in diagnostic cerebral angiography and neurointerventional procedures: a prospective study. Lancet. 1999;354:1594–1597. doi: 10.1016/S0140-6736(99)07083-X. [DOI] [PubMed] [Google Scholar]