Summary
Stroke patients tend to stay longer in one hospital compared to patients with other neurological disease.
After the introduction of 3 types of critical pathway dedicated for various severity of acute ischemic stroke in 1995, the average length of in-hospital days declined from 30.0 days (1993) to 15.3 days (1998), ie 49% reduction.
This reduction was achieved by the use of critical pathway and the hospital-hospital cooperation.
Key words: acute stroke, brain infarction, hospital-hospital cooperation, critical pathway, rehabilitation
Introduction
Patients admitted to neurological ward, especially stroke patients have longer length of hospital stay Stroke patients treated in a specialized stroke unit have been reported to have better outcome1.
In our hospital, however, acute stroke care is taken place on general wards. To minimize the variety and improve the level of acute stroke care, we made critical pathways of acute brain infarction.
The aim of the present study was to test the hypothesis that the length of hospital stay could be reduced by the use of critical pathway.
Subject and Methods
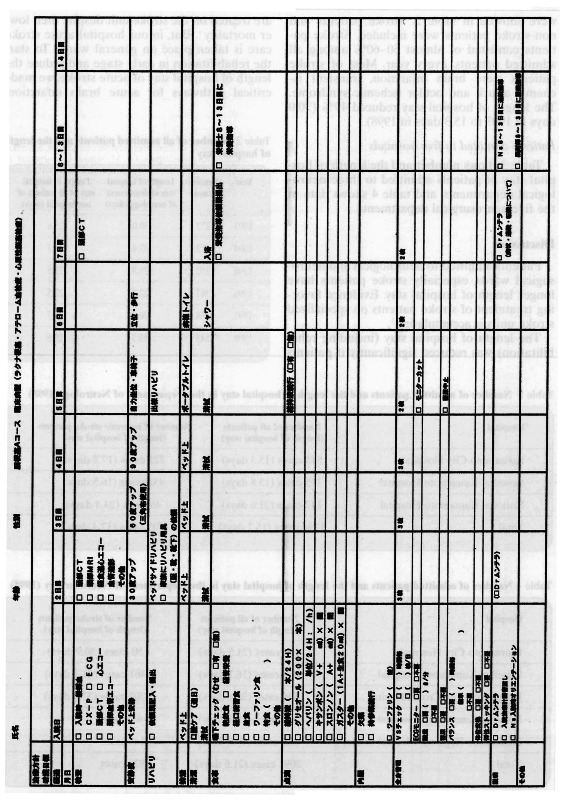
We obtained data from 2314 patients admitted to the departments of neurology and strokology, Kumamoto City Hospital from April 1993 to March 1998. We made three types of critical pathway of brain infarction which was composed of A, B and C courses, March 1995. We used these critical pathways to stroke, especially ischemic stroke, since April 1995. We evaluated the outcome, discharge rate to other hospitals, and length of hospital stay in 281 cases of acute brain infarction admitted within the first week of onset among 368 cases of ischemic stroke from April 1995 to March 1997. Figure shows an example of present critical pathway (A course for staff) .
We also evaluated the number, rate of stroke patients, and the average length of hospital stay of patients admitted to the departments of neurology and neurosurgery of five hospitals in Kumamoto City in 1998.
Results
Brain infarction (April 1995 to March 1997)2
Patients with acute brain infarction referred from other clinics and hospitals, consisted 65% of all patients in our hospital (table 1). The in-hospital mortality was 4%. The discharge rate to other hospitals (hospital-hospital cooperation) was 38%, and the discharge rate to the patient's own home was 58%. The discharge rate to other hospitals and length of hospital stay were, respectively, 21 % and 26 days in lacunar brain infarction, 42% and 30 days in atherothrombotic brain infarction, and 56% and 39 days in cardioembolic brain infarction. The proportion of patients with a length of hospital stay more than 60 days was 8%. The main cause of a long hospital stay was complications. The length of hospital stay was longer and the discharge rate to other hospital was higher in cardioembolic brain infarction than in other kinds of brain infarction.
Table 1.
Outcome of acute brain infarction (April 1995 to March 1997)
| Clinical Categories |
Lacunar brain infarction |
Atherothrombotic brain infarction |
Cardioembolic brain infarction |
Other and unclassified brain infarction |
Total |
|---|---|---|---|---|---|
| Number (%) | 104 (37%) | 71 (25%) | 86 (31%) | 20 (7%) | 281 |
| Age (mean±SD) | 70 ±11 | 71 ±10 | 73 ±13 | 61 ± 19 | 71 ±12 |
| Male : female | 69:35 | 46:25 | 57:29 | 14:6 | 186:95 |
| Introduction referred from other hospital(rate) |
73 (70%) | 43 (61%) | 57 (66%) | 10 (50%) | 183 (65%) |
| Outcome | |||||
| Independent | 83 (80%) | 42 (59%) | 39 (45%) | 15 (75%) | 179 (64%) |
| With cane | 2 (2%) | 7 (10%) | 3 (3%) | 2 (10%) | 14 (5%) |
| Wheel-chair | 16 (15%) | 13 (18%) | 19 (22%) | 1 (5%) | 49 (17%) |
| Bed-ridden | 1 (1%) | 7 (10%) | 18 (21%) | 1 (5%) | 27 (10%) |
| Dead | 2 (2%) | 2 (3%) | 7 (8%) | 1 (5%) | 12 ( 4%) |
| Discharge to other hospital | 22 (21%) | 30 (42%) | 48 (56%) | 7 (35%) | 106 (38%) |
| Discharge to own home | 80 (77%) | 39 (55%) | 31 (36%) | 12 (60%) | 163 (58%) |
| Length of hospital stay | |||||
| Patients of discharge to own home |
21 days | 22 days | 27 days | 24 days | 23 days |
| Patients of discharge to other hospital |
40 days | 40 days | 49 days | 34 days | 44 days |
| Dead patients | 107 days | 42 days | 20 days | 4 days | 37 days |
| Total | 26 days | 30 days | 39 days | 27 days | 31 days |
| Patients with hospital Stay over 60 days(rate) |
4 (4%) | 5 (7%) | 14 (16%) | 0 (0%) | 23 (8%) |
Length of hospital stay in our department (Kumamoto City Hospital)
The lengths of hospital stay of patients admitted to our departments and to our hospital were showed in table 2. Stroke patients and non-stroke patients were included. Stroke patients consisted of almost 50~60% among all admitted patients, every year. Most of stroke patients were brain infarction, transient ischemic attack and ocular ischemic syndrome. The length of hospital stay reduced 49% (30.0 days in 1993 to 15.3 days in 1998).
Table 2.
Number of all admitted patients and the length of hospital stay
| Year | Number (cases) |
Length of hospital stay of department of neurology (days) |
Length of hospital stay of all patients of our hospital (days) |
|---|---|---|---|
| 1993 | 272 | 30.0 | 25.6 |
| 1994 | 312 | 27.4 | 25.3 |
| 1995 | 352 | 23.3 | 23.5 |
| 1996 | 367 | 22.9 | 22.5 |
| 1997 | 468 | 20.4 | 21.7 |
| 1998 | 543 | 15.3 | 20.8 |
Patients admitted to five hospitals
Table 3 shows number and the length of hospital stay of patients admitted to three neurological departments, and table 4 shows data in the five neurosurgical departments.
Table 3.
Number of admitted patients and the length of hospital stay in the Department of Neurology(1998)
| Hospital | Number of all patients (length of hospital stay) |
Number of ischemic stroke patients (length of hospital stay) |
|---|---|---|
| Kumamoto City Hospital | 543 cases (15.3 days) | 225 cases (17.8 days) |
| Saiseikai Kumamoto Hospital | 705 cases (13.8 days) | 432 cases (16.5 days) |
| National Kumamoto Hospital | 147 cases (21.6 days) | 46 cases (24.4 days) |
| Total | 1394 cases (15.2 days) | 703 cases (17.4 days) |
Table 4.
Number of admitted patients and the length of hospital stay in the Department of Neurosurgery (1998)
| Hospital | Number of all patients (length of hospital stay) |
Number of stroke patients (length of hospital stay) |
|---|---|---|
| Kumamoto City Hospital | 164 cases (21.5 days) | 50 cases (30.9 days) |
| Saiseikai Kumamoto Hospital | 868 cases (18.7 days) | 461 cases (21.7 days) |
| Kumamoto Red Cross Hospital | 536 cases (26.4 days) | 202 cases (37.0 days) |
| National Kumamoto Hospital | 201 cases (25.1 days) | 63 cases |
| Kumamoto Regional Medical Center | 322 cases (19.0 days) | 144 cases |
| Total | 2091 cases (21.6 days) | 920 cases |
 |
Discussion
Patients admitted to neurological and neurosugical wards, especially stroke patients have longer length of hospital stay. Evidence favoring treatment of stroke patients on specialized stroke units is accumulating1.
The length of hospital stay (including rehabilitation) was reduced significantly if patients are treated on the stroke unit despite their lower mortality1. But, in our hospital acute stroke care is taken place on general wards. To start the rehabilitation in early stage and reduce the length of hospital stay of acute stroke, we made critical pathways for acute brain infarction. Acute stroke including brain infarction varies in symptoms and sings, clinical category, mechanism, distribution, and severity.
Therefore we made three types of critical pathway (A, B, and C courses) in March 1995. The length of hospital stay in our department was 30.0 days in 1993, 27.4 days 1994 in which exceeded the mean length of hospital stay in our hospital. We used critical pathway of brain infarction from April 1995. The length of hospital stay was reduced 49% (30.0 days in 1993 to 15.3 days in 1998) by the introduction of critical pathway.
Hospital-clinic and hospital-hospital cooperation were also contributed to reduction of the length of hospital stay. Rehabilitation in the recovery stage (2~3 weeks to about 6 months from the stroke onset) could be done in the specialized rehabilitation hospitals within the Kumamoto City area due to hospital-hospital cooperation. Now our acute stroke team can concentrate on the treatment of stroke including early rehabilitation in the acute stage (within 2~3 week from the onset). And rehabilitation team makes rehabilitation in the recovery stage.
Conclusions
The length of hospital stay of neurological patients, especially stroke was reduced by the introduction of critical pathway.
Acknowledgment
The authors thank Dr T. Marubayashi, Department of Neurosurgery, Kumamoto Red Cross Hospital, Japan, Dr S. Fujioka, Department of Neurosurgery, Stroke Center, Saiseikai Kumamoto Hospital, Japan, Dr M. Miura, Department of Neurosurgery, Kumamoto City Hospital, Kumamoto, Japan, Dr T. Ohtsuka, Department of Neurosurgery, National Kumamoto Hospital, Japan, Dr Y. Itoyama, Department of Neurosurgery, Kumamoto Regional Medical Center, Japan, for collecting data.
References
- 1.Joergensen HS, Nakayama H, et al. The effect of a stroke unit: reduction in mortality, discharge rate to nursing home, length of hospital stay, and cost. A community-based study. Stroke. 1995;26:1178–1182. doi: 10.1161/01.str.26.7.1178. [DOI] [PubMed] [Google Scholar]
- 2.Hashimoto Y, Terasaki T, et al. Outcome and hospital-clinic cooperation in acute brain infarction. Jpn J Stroke. 1999;21:200–204. [Google Scholar]


